Abstract
Background
According to the Response Evaluation Criteria in Solid Tumors (RECIST) classification, progressive disease (PD) is defined as target lesion growth (TLG), unequivocal non-target lesion growth (NTLG), or new lesion appearance (NLA). The prognostic impact of the components of PD in tyrosine kinase inhibitor (TKI) therapy for metastatic renal cell carcinoma (mRCC) remains unknown.
Objective
We retrospectively evaluated the prognostic impact of these PD components on survival in patients with mRCC after first-line TKI therapy.
Patients and Methods
Patients were divided into three groups (TLG, NTLG, and NLA) based on the components of PD. Progression-free survival (PFS) and overall survival (OS) after first-line TKI therapy were compared between groups using the Kaplan-Meier method and log-rank test. The predictive impact of the PD components was evaluated using multivariate analyses.
Results
Among the 116 patients included, 80 (69.0%) had TLG, 18 (15.5%) NTLG, and 69 (58.6%) NLA. The mean PFS and OS were shorter for patients with TLG than those without TLG (PFS, 7.1 vs. 11.6 months, p = 0.0071; OS, 18.2 vs. 25.5 months, p = 0.0091). TLG was an independent predictor of PFS (hazard ratio [HR], 1.59; 95% confidence interval [CI], 1.02–2.51; p = 0.0395) and OS (HR, 1.67; 95% CI, 1.02–2.83; p = 0.040). NTLG and NLA were not associated with survival.
Conclusions
In this retrospective single-center study, patients with TLG had poor survival after first-line TKI therapy for mRCC. Thus, individual components of PD influence patient prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

1 Introduction
The advent of molecularly targeted therapies has led to a significant change in the treatment strategy for metastatic renal cell carcinoma (mRCC) [1,2,3]. According to current guidelines, tyrosine kinase inhibitor (TKI) therapy is preferred for most patients with mRCC [2, 4, 5]. The Response Evaluation Criteria in Solid Tumors (RECIST) is the gold standard for assessing the therapeutic efficacy of cancer treatments, including TKI therapy [6]. Several prognostic factors based on RECIST have been proposed for TKI therapy in mRCC [7,8,9,10,11].
According to the RECIST version 1.1, progressive disease (PD) is defined as target lesion growth (TLG), unequivocal non-target lesion growth (NTLG), or new lesion appearance (NLA). Several studies have reported that oncological outcomes were significantly different among the three components of PD. Litiere et al. suggested that NTLG and NLA were worse prognostic factors in patients with breast, colon, and lung cancers [12]. Twelves et al. reported that NLA was significantly associated with a poor prognosis in metastatic breast cancer treated with chemotherapy [13]. It is important to understand the impacts of individual PD components on survival, as these can contribute to better prognostication and treatment planning. However, the prognostic impact of the components of PD in TKI therapy for mRCC remains unknown. Therefore, we retrospectively evaluated the prognostic impact of the components of PD in patients who received first-line TKI therapy for mRCC.
2 Materials and Methods
2.1 Patients
In our department, 188 patients received first-line TKI therapy (106, sunitinib; 69, sorafenib; 13, pazopanib) between January 2007 and March 2017. Among these, we excluded 29 patients who were still receiving first-line TKI at the end of follow-up, after continuous observation of their tumor response, and another 21 patients in whom TKI therapy was discontinued due to adverse events. Of the remaining 138 patients who had PD after TKI therapy, one patient who had received prior cytokine therapy, four patients who received TKIs for only a short duration (< 4 weeks), and 17 patients who received hemodialysis or kidney transplantation were excluded. Ultimately, 116 patients were retrospectively evaluated (Electronic Supplementary Material 1). All patients experienced PD based on RECIST v1.1 after initiation of first-line TKI therapy.
The internal ethics review board of Tokyo Women’s Medical University approved this retrospective study (ID: 4518). For this type of study, formal consent is not required.
2.2 Response Criteria
According to the RECIST v1.1, we evaluated the tumor response of target lesions, non-target lesions, and new lesions, with each classification defined as follows [6]. TLG was defined as an increase of ≥ 20% in the sum of diameters of the target lesions, taking as the reference the smallest sum observed in the study. In addition to a relative increase of 20%, the sum had to demonstrate an absolute increase of at least 5 mm. The unequivocal progression of existing non-target lesions (NTLG) and the appearance of new malignant lesions (NLA) were defined as disease progression.
2.3 Study Design and Endpoint
The patients were divided into three groups according to PD components, namely TLG, NTLG, and NLA. The different components of PD were not mutually exclusive and categories could overlap.
The endpoints of this study were progression-free survival (PFS) and overall survival (OS) after initiation of first-line TKI therapy. PFS was defined as the time from the start of first-line TKI to the date of progression. OS was defined as the time from the initiation of first-line TKI to death from any cause.
2.4 Imaging Methods and Assessment
Baseline imaging examinations, including plain or contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) of the chest, abdomen and pelvis, were performed within 28 days before the start of TKI therapy. Regular scans were performed every 8–12 weeks of therapy, according to the patient’s condition. One of the investigators (T.I.), who was blinded to all other clinical parameters and the patient outcomes, reviewed all images for analysis.
2.5 Protocols for Tyrosine Kinase Inhibitor Regimens
The TKI regimens used in our department have been described previously [14, 15]. The main agent for first-line TKI therapy is sunitinib. In the sunitinib regimen, we currently employ a 2-weeks-on/1-week-off schedule, based on findings from our previous study [16]. Sunitinib is administered orally at a dose of 50 mg daily and modified according to the patient’s condition. Based on previous research, for patients with a poor performance status or > 80 years of age, either sorafenib or pazopanib is selected, as these TKIs have better tolerability than sunitinib [17,18,19,20]. In the sorafenib regimen, 200 mg sorafenib is administered orally twice daily and increased to 800 mg within 2–4 weeks to reduce any acute dermatological reactions, with a continuous dosing schedule. In the pazopanib regimen, the drug is administered orally once daily at a dose of 800 mg, with continuous dosing. The dose is reduced to 600 mg and then to 400 mg according to the severity of adverse events. In all the regimens, the drugs are administered until PD is observed or intolerable adverse events occur.
2.6 Statistical Analysis
Distributions of PFS and OS were calculated using the Kaplan-Meier method and compared using the log-rank test. The median PFS and OS are reported along with 95% confidence intervals (CI). Univariate and multivariate analyses were performed using Cox proportional hazards regression models to identify predictors of survival. All analyses were performed using JMP software (version 12.1; SAS Institute, Cary, NC, USA), and differences were considered statistically significant at p values <0.05.
3 Results
3.1 Patient Characteristics
Eighty-two patients (70.7%) were men, and the median patient age was 66.0 years. The most frequent pathological type was clear cell carcinoma (CCC; n = 84, 72.4%). Sorafenib, sunitinib, and pazopanib were administered as first-line TKI agents in 35 (30.2%), 73 (62.9%), and 8 (6.9%) patients, respectively. Among the 116 patients, 80 (69.0%) showed TLG, 18 (15.5%) NTLG, and 68 (58.6%) NLA. Additionally, 43 and 36 patients had TLG alone and NLA alone, respectively, whereas no patients had NTLG alone. In 35 patients, overlapping components of PD were observed. Among these 35 patients, two patients (1.7%) had TLG and NTLG, 17 patients (14.7%) TLG and NLA, and 16 patients (13.8%) all three components. No patient had NTLG and NLA (Table 1).
3.2 Progression-Free Survival According to the Individual Components of Progressive Disease
Electronic Supplementary Material 2A shows the PFS of the entire study group, with a median PFS of 8.7 months.
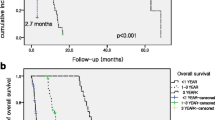
Figure 1 shows the Kaplan-Meier curves for PFS after first-line TKI therapy according to the individual components of PD. Patients with TLG had significantly shorter PFS than those without TLG (7.1 [95% CI: 5.6–9.1] vs. 11.6 [95% CI: 6.3–15.1] months, p = 0.0071). Patients with NTLG had significantly shorter PFS than those without NTLG (5.7 [95% CI: 2.9–9.2] vs. 9.0 [95% CI: 6.4–11.4] months, p = 0.0361). There was no significant difference in PFS between patients without and with NLA (7.1 [95% CI: 5.4–11.0] 9.1 [95% CI: 6.1–11.5] months, p = 0.225).
Progression-free survival according to the components of progressive disease. Progression-free survival was compared between patients a with TLG and without TLG, b with NTLG and without NTLG, and c with NLA and without NLA. CI, confidence interval; TLG, target lesion growth; NTLG, non-target lesion growth; NLA, new lesion appearance
3.3 Overall Survival According to Individual Components of Progressive Disease
Electronic Supplementary Material 2B shows the OS of the entire study group, with a median OS of 20.6 months.
Figure 2 shows the Kaplan-Meier curves for OS after first-line TKI therapy according to individual components of PD. Patients with TLG had significantly shorter OS than patients without TLG (18.2 [95% CI: 13.3–23.1] vs. 25.5 [95% CI: 20.3–not reached] months, p = 0.0091). No significant difference in OS was demonstrated between patients with and without NTLG (14.0 [95% CI: 8.5–31.7] vs. 21.7 [95% CI: 18.2–27.4] months, p = 0.113). Patients with and without NLA also showed no significant difference in OS (21.7 [95% CI: 14.5–30.6] vs. 19.3 [95% CI: 13.7–25.6] months, p = 0.381).
Overall survival according to components of progressive disease. Overall survival was compared between patients a with TLG and without TLG, b with NTLG and without NTLG, and c with NLA and without NLA. CI, confidence interval; TLG, target lesion growth; NTLG, non-target lesion growth; NLA, new lesion appearance
3.4 Progression-Free Survival and Overall Survival in Patients with Target Lesion Growth Alone, New Lesion Appearance Alone, and Multiple Components of Progressive Disease
To exclude the potential influence of overlapping PD components, we also compared survival among patients who had only a single PD component. Figure 3a reveals a trend for shorter PFS in patients with TLG alone compared to patients with NLA alone (7.3 [95% CI: 5.0–11.4] vs. 10.5 [95% CI: 6.1–15.1] months, p = 0.0759). Figure 3b shows that patients who had TLG alone had significantly shorter OS than those with NLA alone (20.4 [95% CI: 13.7–27.4] vs. 29.9 [95% CI: 21.0–not reached] months, p = 0.0212).
3.5 Predictors of Progression-Free Survival and Overall Survival
As shown in Table 2, univariate analysis for PFS showed that TLG, compared to no TLG, was a significant predictor of shorter PFS (p = 0.0061). Additionally, female sex, non-CCC pathological type, absence of a prior nephrectomy, and poor risk based on MSKCC risk classification were significant predictors for shorter PFS (p < 0.05 for all). Multivariate analysis for PFS identified TLG as an independent predictor of shorter PFS (hazard ratio [HR]: 1.59, 95% CI: 1.02–2.51, p = 0.0395), in addition to the absence of a prior nephrectomy (HR: 2.07, 95% CI: 1.13–3.61, p = 0.0182) and poor risk based on MSKCC risk classification (HR: 3.22, 95% CI: 1.83–5.39, p = 0.0001).
As shown in Table 3, univariate analyses identified TLG as a significant predictor of OS (HR: 1.90, 95% CI: 1.18–3.16, p = 0.0073). Additionally, female sex, non-CCC pathological type, the absence of a previous nephrectomy, poor risk based on MSKCC risk classification, and multiple metastases were also significant predictors of OS (p < 0.05 for all). Multivariate analyses identified TLG as an independent predictor of OS (HR: 1.67, 95% CI: 1.02–2.83, p = 0.04), in addition to female sex (HR: 1.73, 95% CI: 1.06–2.78, p = 0.0299), non-CCC pathological type (HR: 1.99, 95% CI: 1.15–3.38, p = 0.0144), poor risk based on MSKCC risk classification (HR: 2.74, 95% CI: 1.48–4.80, p = 0.0019), and multiple metastases (HR: 2.19, 95% CI: 1.36–3.66, p = 0.0012).
3.6 Overall Survival After First-Line Therapy Failure According to the Components of Progressive Disease
Further, to investigate whether TLG could affect prognosis after failure of first-line therapy, we compared OS after first-line therapy failure between patients with and without TLG, as well as between patients with TLG alone and NLA alone. Patients with TLG had significantly shorter OS after first-line therapy failure than those without TLG (8.3 [95% CI: 5.0–9.9] vs. 16.8 [95% CI: 5.7–29.5] months, p = 0.0142; Electronic Supplementary Material 3A). However, only a trend toward shorter OS was identified in patients with TLG alone compared to NLA alone (8.3 [95% CI: 4.9–13.1] vs. 16.8 [95% CI: 5.7–29.5] months, p = 0.0773; Electronic Supplementary Material 3B).
4 Discussion
This study reveals that patients with TLG after first-line TKI therapy for mRCC had significantly poorer PFS and OS than patients experiencing PD without TLG. However, NLA was not significantly associated with PFS or OS. Multivariate analyses identified TLG as an independent predictive factor of PFS and OS. To the best of our knowledge, this is the first study evaluating the prognostic impact of components of PD after first-line TKI therapy for mRCC.
Previous studies have reported that NLA or NTLG was associated with poor patient survival after cytotoxic chemotherapy or targeted therapy for non-urological cancer [12, 13, 21, 22]. Nevertheless, in our analysis, TLG was a significant factor for oncological outcomes. This difference may have been caused by different types of cancers or corresponding treatments between molecularly targeted therapies and cytotoxic chemotherapy. That is, in some patients, it is difficult to evaluate the tumor response to targeted therapy for mRCC according to the RECIST, because specific morphological changes, such as necrosis, cannot be accurately reflected [23,24,25]. Therefore, a difference in PD interpretation may affect the analyses of outcomes according to types of treatment.
Regarding mRCC, Stein et al. showed that NTLG and NLA, and not TLG, were significant predictors of survival using data from RECORD-1 [26]. However, no significant association was observed for NTLG or NLA in the intermediate term after treatment initiation (i.e., 14–18 weeks) in their study. Therefore, the prognostic impact of the PD components may be strongly affected by the timing of PD. Stein et al. demonstrated that poor OS could be predicted by the fastest-growing target lesion [26]. Other studies have also reported that early treatment failure was significantly associated with poor oncological outcomes [26,27,28]. Similarly, our previous data showed that slow tumor growth mediated by TKI therapy was associated with a favorable prognosis [14, 15]. Indeed, in the present study, 18 patients experienced PD within the first 3 months after therapy initiation, and their OS was significantly poorer than that of the other patients. Further, TLG was observed in 15 of these patients. In summary, TLG was associated with early treatment failure and resulted in poor survival compared to the other PD components.
Importantly, patients with TLG had significantly shorter OS after first-line TKI therapy failure (Electronic Supplementary Material 3). Either a second TKI or a mammalian target of rapamycin inhibitor was administered to most patients (66 of 69 patients who received second-line therapy). Therefore, a novel treatment approach, such as the use of nivolumab and not conventional targeted therapy, may be an effective treatment option for patients who have TLG as a component of PD after first-line TKI therapy failure.
Our study has several limitations. First, the study was retrospectively conducted in a single center with a small cohort. Thus, our results were affected by unavoidable biases of patient and treatment selection. Second, our own TKI protocol may have influenced outcomes. That is, with regard to our use of sunitinib, a majority of patients received an alternative 2-weeks-on/1-week-off schedule. Although our previous study showed no significant difference in oncological outcome between this alternative schedule and the standard 4-weeks-on/1-week-off schedule [16], we cannot deny that a possible influence on outcomes by the difference in regimens might exist. Also, we selected either sorafenib or pazopanib for patients with a poor general condition, and therefore a corresponding selection bias may exist in some cases. Third, RECIST criteria can assess only the change in tumor diameter and not any intratumor activity, such as necrosis, which is considered to be an important morphologic change [25]. Therefore, the efficacy of TKI therapy might not be accurately reflected in some cases using the RECIST criteria. Finally, there might be diagnostic bias among the components of PD. In particular, the definition of non-target lesion growth was likely to be less strict (unequivocal progression of existing non-target lesions) than the other components. Thus, TLG or NLA might be over-diagnosed compared to NTLG, and this unbalanced priority of definition could affect the analyses.
5 Conclusions
This retrospective single-center study identified TLG as an independent predictor of survival in patients with mRCC who received first-line TKI therapy. This finding is valuable for physicians with regard to predicting patient survival after first-line TKI therapy.
References
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. New Engl J Med. 2007;356(2):115–24. https://doi.org/10.1056/NEJMoa065044.
Escudier B, Porta C, Schmidinger M, Rioux-Leclercq N, Bex A, Khoo V, et al. Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v58–68. https://doi.org/10.1093/annonc/mdw328.
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Oudard S, et al. Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol. 2009;27(22):3584–90. https://doi.org/10.1200/jco.2008.20.1293.
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol. 2015;67(5):913–24. https://doi.org/10.1016/j.eururo.2015.01.005.
Motzer RJ, Jonasch E, Agarwal N, Bhayani S, Bro WP, Chang SS, et al. Kidney Cancer, version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw: JNCCN. 2017;15(6):804–34. https://doi.org/10.6004/jnccn.2017.0100.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Grunwald V, Lin X, Kalanovic D, Simantov R. Early tumour shrinkage: a tool for the detection of early clinical activity in metastatic renal cell carcinoma. Eur Urol. 2016;70(6):1006–15. https://doi.org/10.1016/j.eururo.2016.05.010.
Miyake H, Miyazaki A, Imai S, Harada K, Fujisawa M. Early tumor shrinkage under treatment with first-line tyrosine kinase inhibitors as a predictor of overall survival in patients with metastatic renal cell carcinoma: a retrospective multi-institutional study in Japan. Target Oncol. 2016;11(2):175–82. https://doi.org/10.1007/s11523-015-0385-6.
Grunwald V, McKay RR, Krajewski KM, Kalanovic D, Lin X, Perkins JJ, et al. Depth of remission is a prognostic factor for survival in patients with metastatic renal cell carcinoma. Eur Urol. 2015;67(5):952–8. https://doi.org/10.1016/j.eururo.2014.12.036.
Iacovelli R, Lanoy E, Albiges L, Escudier B. Tumour burden is an independent prognostic factor in metastatic renal cell carcinoma. BJU Int. 2012;110(11):1747–53. https://doi.org/10.1111/j.1464-410X.2012.11518.x.
Ishihara H, Kondo T, Omae K, Takagi T, Izuka J, Kobayashi H, et al. The magnitude of best tumor shrinkage during second-line targeted therapy affects progression-free survival but not overall survival in patients with metastatic renal cell carcinoma. Jpn J Clin Oncol. 2016;46(6):568–74. https://doi.org/10.1093/jjco/hyw024.
Litiere S, de Vries EG, Seymour L, Sargent D, Shankar L, Bogaerts J. The components of progression as explanatory variables for overall survival in the response evaluation criteria in solid tumours 1.1 database. Eur J Cancer. 2014;50(10):1847–53. https://doi.org/10.1016/j.ejca.2014.03.014.
Twelves C, Cortes J, Kaufman PA, Yelle L, Awada A, Binder TA, et al. “New” metastases are associated with a poorer prognosis than growth of pre-existing metastases in patients with metastatic breast cancer treated with chemotherapy. Breast Cancer Research : BCR. 2015;17(1):150. https://doi.org/10.1186/s13058-015-0657-1.
Ishihara H, Kondo T, Yoshida K, Omae K, Takagi T, Iizuka J, et al. Time to progression after first-line tyrosine kinase inhibitor predicts survival in patients with metastatic renal cell carcinoma receiving second-line molecular-targeted therapy. Urol Oncol. 2017; https://doi.org/10.1016/j.urolonc.2017.05.014.
Ishihara H, Yagisawa T, Kondo T, Omae K, Takagi T, Iizuka J, et al. Effect of the timing of best tumor shrinkage on survival of patients with metastatic renal cell carcinoma who received first-line tyrosine kinase inhibitor therapy. Int J Clin Oncol. 2017;22(1):126–35. https://doi.org/10.1007/s10147-016-1032-7.
Kondo T, Takagi T, Kobayashi H, Iizuka J, Nozaki T, Hashimoto Y, et al. Superior tolerability of altered dosing schedule of sunitinib with 2-weeks-on and 1-week-off in patients with metastatic renal cell carcinoma--comparison to standard dosing schedule of 4-weeks-on and 2-weeks-off. Jpn J Clin Oncol. 2014;44(3):270–7. https://doi.org/10.1093/jjco/hyt232.
Omae K, Kondo T, Kennoki T, Takagi T, Iizuka J, Kobayashi H, et al. Efficacy and safety of sorafenib for treatment of Japanese metastatic renal cell carcinoma patients undergoing hemodialysis. Int J Clin Oncol. 2016;21(1):126–32. https://doi.org/10.1007/s10147-015-0871-y.
Akaza H, Tsukamoto T, Murai M, Nakajima K, Naito S. Phase II study to investigate the efficacy, safety, and pharmacokinetics of sorafenib in Japanese patients with advanced renal cell carcinoma. Jpn J Clin Oncol. 2007;37(10):755–62. https://doi.org/10.1093/jjco/hym095.
Procopio G, Bellmunt J, Dutcher J, Bracarda S, Knox J, Brueckner A, et al. Sorafenib tolerability in elderly patients with advanced renal cell carcinoma: results from a large pooled analysis. Br J Cancer. 2013;108(2):311–8. https://doi.org/10.1038/bjc.2012.543.
Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med. 2013;369(8):722–31. https://doi.org/10.1056/NEJMoa1303989.
Litière S, Isaac G, Vries ED, Bogaerts J, Chen AP, Dancey J, et al. Validation of RECIST 1.1 for use with cytotoxic agents and targeted cancer agents (TCA): results of a RECIST Working Group analysis of a 50 clinical trials pooled individual patient database. J Clin Oncol. 2017;35(15_suppl):2534. https://doi.org/10.1200/JCO.2017.35.15_suppl.2534.
Mietlowski WL, Bao W, Wood PA, Williams DE, El-Hashimy M, Sarr C, et al. Clinical importance of including new and nontarget lesion assessment of disease progression (PD) to predict overall survival (OS): implications for randomized phase II study design. J Clin Oncol. 2012;30(15_suppl):2543. https://doi.org/10.1200/jco.2012.30.15_suppl.2543.
Thian Y, Gutzeit A, Koh DM, Fisher R, Lote H, Larkin J, et al. Revised Choi imaging criteria correlate with clinical outcomes in patients with metastatic renal cell carcinoma treated with sunitinib. Radiology. 2014;273(2):452–61. https://doi.org/10.1148/radiol.14132702.
Brufau BP, Cerqueda CS, Villalba LB, Izquierdo RS, Gonzalez BM, Molina CN. Metastatic renal cell carcinoma: radiologic findings and assessment of response to targeted antiangiogenic therapy by using multidetector CT. Radiographics. 2013;33(6):1691–716. https://doi.org/10.1148/rg.336125110.
Choi H, Charnsangavej C, Faria SC, Macapinlac HA, Burgess MA, Patel SR, et al. Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol. 2007;25(13):1753–9. https://doi.org/10.1200/jco.2006.07.3049.
Stein A, Bellmunt J, Escudier B, Kim D, Stergiopoulos SG, Mietlowski W, et al. Survival prediction in everolimus-treated patients with metastatic renal cell carcinoma incorporating tumor burden response in the RECORD-1 trial. Eur Urol. 2013;64(6):994–1002. https://doi.org/10.1016/j.eururo.2012.11.032.
Suzuki C, Blomqvist L, Sundin A, Jacobsson H, Bystrom P, Berglund A, et al. The initial change in tumor size predicts response and survival in patients with metastatic colorectal cancer treated with combination chemotherapy. Ann Oncol. 2012;23(4):948–54. https://doi.org/10.1093/annonc/mdr350.
Krajewski KM, Fougeray R, Bellmunt J, Pons F, Schutz FA, Rosenberg JE, et al. Optimisation of the size variation threshold for imaging evaluation of response in patients with platinum-refractory advanced transitional cell carcinoma of the urothelium treated with vinflunine. Eur J Cancer. 2012;48(10):1495–502. https://doi.org/10.1016/j.ejca.2011.11.018.
Acknowledgments
The authors thank Editage for English language editing and Nobuko Hata for secretarial work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of Interest
Tsunenori Kondo received honoraria from Pfizer, Bayer, and Novartis. Takashi Ikeda, Hiroki Ishihara, Toshio Takagi, Kazuhiko Yoshida, Junpei Iizuka, and Kazunari Tanabe declare that they have no conflict of interest that might be relevant to the contents of this manuscript.
Electronic supplementary material
ESM 1
(PDF 490 kb)
Rights and permissions
About this article
Cite this article
Ikeda, T., Ishihara, H., Takagi, T. et al. Prognostic Impact of the Components of Progressive Disease on Survival After First-Line Tyrosine Kinase Inhibitor Therapy for Metastatic Renal Cell Carcinoma. Targ Oncol 13, 379–387 (2018). https://doi.org/10.1007/s11523-018-0569-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-018-0569-y