Abstract
Spectral analysis of atrial signals has been used to identify regions of interest in atrial fibrillation (AF). However, the relationship to the atrial substrate is unclear. In this study, we compare regions with dominant frequency (DF), simultaneously determined in the left atrium (LA) by a novel noncontact mapping system using unipolar charge density signals, to the zones of slow conduction (SZ) during AF.
In 19 AF patients the conduction during AF was assessed by a validated algorithm and SZ compared to the DF and the DF ratio between the DF peak and the area under the total spectrum (DFR). The results were compared in five different regions of the LA. The reproducibility of SZ location at different time measurements was higher than for DF or DFR. The SZs are mainly confined at the anterior and posterior wall of the LA. There was no statistically significant correlation between SZ and DF or DFR across the atrium.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Spectral analysis of atrial fibrillation (AF) signals has been used to identify regions of interest in patients with persistent atrial fibrillation after pulmonary vein isolation and areas with dominant frequency (DF) were thought to be drivers of persistent AF [1]. However, initial studies were done with sequential contact mapping, which does not allow simultaneous DF mapping in the entire atrium. In addition, the correlation of DF to other physiologic measures of atrial disease, such as conduction velocity in AF is unknown.
Noncontact potentials have been recorded by noncontact multielectrode catheters (the EnSite™ Array™) for simultaneous frequency analysis in the entire atrium [2]. However, the results have not been reproducible, which might be related to the fact that unipolar voltage signals include the electrical far field signal [3].
Therefore, in order to decrease the far field component during DF analysis with noncontact mapping, we used a newly developed noncontact mapping system (AcQMap®, Actus Medical, Inc.). This system computes the source of the electrical field (potential), which is the charge density (CD = Coulomb/cm2) at the heart wall[4,5,6]. This is the first study reporting results of DF analysis from simultaneously obtained charge signals of the entire atrium.
First studies have been published reporting patterns of AF propagation waves in the entire atrium including automatic detection of areas with repeated focal discharges, rotational activities and local irregular conduction characteristics [7,8,9]. In addition, recently a new algorithm computing conduction velocity has been implemented in the system in order to determine the zones of slow conduction (SZ, slow zones, [10]). This is the first study to report the localization and reproducibility of SZ in the human atrium during AF.
Previous studies suggest that conduction velocity disturbances might play a role in arrhythmogenic substrate [11, 12]. The study from Grossi et al. shows correlation between bipolar signals and frequency during sinus rhythm and incremental pacing [13].
This study was conducted to test the hypothesis that high frequency areas might be correlated to zones of SZ. In addition, the reproducibility of DF and SZ analysis in the human atrium was assessed during AF.
2 Methods
2.1 Electrophysiologic study and recording
Signal recordings from 19 patients during AF mapping under general anesthesia were used for offline analysis. All patients have given informed written consent for the study. Patient characteristics are summarized in Table 1. Antiarrhythmic drug treatment was stopped at least 2 days before the procedure except for Amiodarone. After transseptal access, Heparin was administered until ACT was > 350 s. The AcQmap® catheter (Acutus Medical, Carlsbad, CA, USA) was deployed for anatomy reconstruction and unipolar electrogram recordings. The left atrium (LA) surface was meshed with triangular elements (> 3000 vertices, with a spatial resolution of ≈ 2 mm). Two baseline AF recordings of 30 s duration, which were at least 5 min apart, were used for analysis. In the patients with sinus rhythm, AF was induced by burst pacing. The unipolar voltage signals were filtered between 1 and 100 Hz for further processing.
2.2 Signal processing and data analysis
-
A)
Localization of slow conduction zones
AF propagation history maps [14] of 10 s were computed for two segments at different recording times and were computed as previously described [15]. Then, propagation data were analyzed by the software algorithm for automatic location of slow conduction zones (SlowZone™ Locator (SZ), Acutus Medical, Carlsbad, CA, USA) (Fig. 1). Briefly, noncontact local activation times (LAT) are determined from the CD signals of the Acutus mapping system (Fig. 1a). At each vertex of the anatomical surface, a neighborhood (radius ~ = 5 mm) is defined and projected to a 2D surface (Fig. 1b) using the two first principal components (u,v) determined using a singular value decomposition. The conduction velocity is estimated using a 3rd order polynomial surface fit [10, 16] to estimate the gradient of activation and inverted to estimate velocity on the mesh vertex (Fig. 1c). This estimation approach is similar to those implemented previously [10, 17, 18]. Single or multiple velocity maps can be combined to find regions of consistent slow conduction velocity (Fig. 1d). Zones of slow conduction were defined as having a conduction velocity magnitude < 0.3 m/s evaluated on a vertex basis, which is consistent with the literature [19,20,21].
-
B)
Frequency analysis
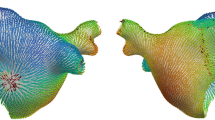
At each vertex of the meshed surface, the unipolar CD signals during baseline AF were computed for the entire LA surface a sampling rate of 3125 Hz. The ventricular component of the unipolar raw signal was subtracted by the Acutus Mapping System, using a template-based method [22]. All data were exported for further analysis with MATLAB (Mathworks, Natick, MA, USA). A band-pass filter between 3 and 20 Hz was applied and the power spectrum estimation was performed using a smoothed periodogram (Hamming window) with a frequency resolution of 0.1 Hz [2]. For each individual vertex, the frequency spectrum was computed and the frequency with the highest power was taken as the dominant frequency (DF). Then, the DF values of each vertex were displayed in a color 3D map (Fig. 2a, b). As higher frequencies were not considered physiologic, the algorithm looks for DF below 20 Hz. All maps were visually inspected, especially in regions with abrupt change in frequencies and if harmonics were found, the fundamental frequency was used as DF. The region of high frequency activity was defined by a DF larger than 90% of maximum DF in the entire LA (DFMaxDFMap), (Fig. 2c) [23].
In addition, the relationship between the DF and the entire frequency spectrum was assessed for each vertex. The DF peak value was divided by the integral of the entire frequency spectrum, resulting DF Ratio, which is a measure for the dispersion of the frequency spectrum and was visualized by a RF ratio Map (DFR), (Fig. 3a) as described previously[24, 25]. High DFR regions were defined by highest DFR, larger than 90% of DFRMaxDFRMap, where DFRMaxDFRMap was the maximum DFR value of the entire map (Fig. 3b).
-
C)
Distribution of SZ, DF and DFR on the LA surface
SlowZone Locator Map (SZ Map). a Local activation time computed from CD. b 3D to 2D projection. For each vertex on the surface, define a neighborhood and project them to the 2 first principal components (u and v). c Compute conduction velocity with polynomial fit and project back to 3D anatomy. d SZ Map, regions with consistent slow conduction (in blue)
Two SZ, DF, and DFR maps of 10 s recording each were constructed during baseline AF for each patient. The left atrium was arbitrarily divided into five regions (R1 to R5): 1. Anterior Wall, 2. Posterior Wall, 3. Septum, 4. Roof, 5. Lateral Wall (Fig. 4). The presence or absence of SZ, DF, and DFR was reported as a binary variable for each anatomical region.
2.3 Statistical analysis
Continuous data are reported as mean ± SD. Cohen’s Kappa coefficient was calculated to compare the agreement between the two maps and assess the relationship between the methods SZ and DF as well as SZ and DFR. The comparison between baseline recordings was computed using Fisher-exact test. Spearman’s Rho Coefficient was used to compare the temporal correlation between the two baseline recordings. Statistical analysis was performed using R Foundation.
3 Results
In each of the 19 patients, 2 recordings of baseline AF for 10 s have been used to compute the SZ, DF, and DFR maps, leading to a total of 114 maps.
The clinical characteristics of the patients are summarized in Table 1. The findings of the study are visualized in one patient as an example (Fig. 5): the SZ is predominant at septum and anterior part of the LA, the DF regions are located at the anterior, posterior and roof of the LA, while DFR are only located at the posterior wall.
3.1 Temporal reproducibility
The temporal reproducibility between the two recordings (Table 2) was better for the location of the SZ (best value Rho = 0.58, at the anterior wall) than for the DF analysis (Rho = 0.3, at the roof) between the two maps. For the DFR analysis, the highest agreement was found on the lateral wall (Rho = 0.32).
3.2 Slow conduction zones
The occurrence of SZ for each region is reported in Table 3 as percentage of the total 38 maps. Zones of slow conduction < 0.3 m/s were found all but one map, they were more frequently in the anterior wall of patients and posterior wall in 76.3% of the maps than on the septum or posteriorly. Interestingly the roof showed never zones of slow conduction. DF analysis does not show a clear localization of high frequency, while DFR method is mainly located at the posterior wall (60.5%).
3.3 Spectral analysis
In contrast, the DF was distributed all over the atrial regions (Table 3), as well as the highest DF ratio. The mean DF value of all LA sites did not differ between paroxysmal and persistent AF patients (5.2 ± 0.4 Hz versus 5.5 ± 0.8 Hz, p = 0.34). While a significant mean DF value was observed between paroxysmal and long-standing AF patients (5.2 ± 0.4 Hz versus 6.1 ± 0.1 Hz, p = 0.0007).
3.4 Agreement between slow conduction and frequency analysis
There was no significant agreement between the location of SZ and the location of DF or DFR, for both baseline recordings. Cohen’s Kappa, Κ between − 0.37 and 0.17 for SZ vs DF and K between − 0.13 and 0.13 for SZ vs DFR (Fig. 6a for DF and Fig. 6b for DFR). Using a mixed model regression analysis to compare the SZ vs DF and SZ vs DFR, not significant correlation was obtained (p > 0.21).
4 Discussion
This is the first study to report frequency analysis of CD signals simultaneously recorded in the entire atrium and to compare results to SZ during AF in humans.
4.1 Frequency analysis
This study shows that DF and DFR were not reproducible over time. For the five regions of the LA analyzed, no correlation has been observed between the first and second recordings (p > > 0.05) (Table 2). This result agrees with previous findings [2, 3], where mappings were performed using unipolar noncontact voltage and bipolar contact electrograms. The DF analysis also shows a quasi-uniform distribution of the DF over the entire atrium. Only on the posterior wall that a higher occurrence of DF location was observed (Table 2). There was no significant difference in the mean DF values of all LA sites between paroxysmal and persistent AF patients (5.2 ± 0.4 Hz versus 5.5 ± 0.8 Hz, p = 0.34), as observed by Jarman et al. [2] and no significant correlation has been found between locations of DF and DFR. Frequency analysis has been performed widely. For bipolar voltage signals, hopeful results have been published initially [1], however the clinical value has been low because of poor reproducibility of sequential measurements of bipolar contact signals. Also, for noncontact unipolar voltage signals, several studies report mixed results, which were obtained by using a definition for frequency regions by 20% higher frequency than neighborhood points [2]. However, with that definition, we would only obtain the border of high frequency regions but not identify the spots with the DF itself.
Frequency analysis has not gained widespread clinical application because of inherent limitations of reproducibility [3, 26, 27] and lack of pathophysiological correlation to clinical characterizations to the atrial substrate.
4.2 Location of slow zones
There are no previous studies identifying zones of slow conduction in the human atrium during AF, because the technology was not available in other mapping systems. First, the reproducibility of the methods was tested, which showed that only the localization of SZ areas is somewhat reproducible in the anterior and posterior wall with moderate but significant correlation values (Rho = 0.58, p = 0.01 and Rho = 0.47, p = 0.04, respectively) (Table 2). Previous studies have shown that atrial conduction velocity has been correlated to arrhythmogenic substrate [28,29,30,31]. In Heida et al. [29], patients with a history of AF had slower conduction velocity (CV) at the Bachmann’s bundle region compared to a control group, and Zhen et al. study [28] shows slow CV at the septum and anterior wall. This study also confirmed that SZ region are mainly confined at the anterior wall of the LA as reported by Kurato et al. [30]. For each of the 19 patients, 2 maps of SZ have been computed. Among these 38 maps, 29 maps were found having SZ at the anterior wall (76.3%) and 21 maps with SZ at the posterior wall (55.3%) (Table 3). Interestingly, no SZ have been found on the roof, this might be due to the small population included in this study.
The analysis of atrial CV is a new tool and might be more representative for the atrial substrate, because it is more reproducible, has been validated against contact measurements of CV [10] and represents a clinical meaningful value of atrial electrical properties. Whether the cutoff value of 3 m/s as used in the literature translates into prognostic information has to be determined by future studies. Also, the correlation of CV during various rhythms (sinus rhythm, pacing, flutter, fibrillation) has to be determined to further characterize the impact of functional alterations of the atrial substrate.
4.3 Relationship between frequency analysis, slow zones and complex fractionated atrial electrograms
This is the first study to compare DF and SZ. Our results did not show agreements between location of DF and SZ or DFR and SZ. This is not surprising since results of DF and DFR were not stable over time. One study reports a strong correlation between CV and the barycenter of the frequency spectrum Grossi et al. [13]. The study was performed during incremental pacing, and CV was computed along the catheter inserted along the coronary sinus. So, a comparison to our current study would not be relevant, since they used different technology and spectrum analysis during pacing.
Previous studies have investigated the relationship between DF and comoplex fractionated electrograms (CAFÉ) using bipolar signals [32, 33] in patient presenting for AF ablation. Habel et al. mapped the left atrium using a 64-electrode basket catheter while Vermal et al. [33] used a circular mapping catheter during persistent AF patient. These studies did not show a significant correlation between sites of high frequency and CAFEs, as well as their stability over time. From these studies, no conclusion to guide RFA could be drawn.
4.4 Methodological discussion
In the current study, the time segment used to compute DF and map of SZ was arbitrarily chosen at 10 s. The choice was made based on the processing capacity of the software to compute larger map duration. The AcQMap® allows to compute the SZ in different manners: (a) using Supermap recording, which is a specific mode to acquire data by rowing the AcQMap® catheter in the atrium, resulting in a single map based on a large set of non-contact electrogram recordings, (b) using a combination of several propagation maps recorded, and (c) using a single map recording. Since we had 10 s of recording for each map, we used only one map of 10 s to compute the SZ map. During 10 s of AF, at each vertex, CVs were computed for each activation detected. Atrial region with > 75% of the CVs below 0.3 m/s were displayed as SZ, which are standard settings of the AcQMap® algorithm. The size of the SZ was also not reported in this study, only their localization. The time interval between each map was approximatively 5 min, the effect of this parameter on the map was not accessed in this study. The current AcQmap® software was not also considering the magnitude of the signal to compute the zone of slow conduction, which might also play a role.
5 Limitations
The present study includes a small patient group; however, the amount of data collected are considerable. Two baselines AF recordings of 10 s each and data are analyzed over 3000 vertices for each anatomy. Novel and meaningful findings of statistical significance were obtained. Therefore, it is doubtful that different results would appear with larger patient numbers. Another limitation is that the size of LA was not computed, and inaccuracy can be introduced if the distance from the center of the noncontact catheter to the wall is > 4 cm. However, the mean value of left atrial diameter was 4.3 cm and the largest diameter 5.9 cm. Finally, further follow-up studies are necessary to address the clinical impact of our findings.
6 Conclusion
In this study, the locations of SZ and DF do not match in AF patients. The SZ are mainly confined at the anterior and posterior wall of the LA. The consistency of the results over time is only given for SZ and not for the spectral analysis. These findings suggest that the SZ, but not the DF could be used for comparison to measures of the atrial substrate.
Abbreviations
- AF:
-
Atrial fibrillation
- CAFE:
-
Complex fractionated electrogram
- CD:
-
Charge density (C·cm−2)
- CV:
-
Conduction velocity (m·s−1)
- SZ:
-
Slow zone
- LAT:
-
Local activation time (ms)
- FFT:
-
Fast Fourrier transform
- DF:
-
Dominant frequency (Hz)
- DFR:
-
Dominant frequency ratio, the ratio between the DF peak and the area under the total spectrum
- LA:
-
Left atrium
- MV:
-
Mitral valve
- LSPV:
-
Left pulmonary vein
- LIPV:
-
Left inferior pulmonary vein
- RSPV:
-
Right superior pulmonary vein
- RIPV:
-
Right inferior pulmonary vein
- LAA:
-
Left atrial appendage
References
Sanders P, Berenfeld O, Hocini M, Jaïs P, Vaidyanathan R, Hsu L-F, Garrigue S, Takahashi Y, Rotter M, Sacher F, Scavée C, Ploutz-Snyder R, Jalife J, Haïssaguerre M (2005) Spectral analysis identifies sites of high-frequency activity maintaining atrial fibrillation in humans. Circulation 112(6):789–797
Jarman JWE, Wong T, Kojodjojo P, Spohr H, Davies JE, Roughton M, Francis DP, Kanagaratnam P, Markides V, Davies DW, Peters NS (2012) Spatiotemporal behavior of high dominant frequency during paroxysmal and persistent atrial fibrillation in the human left atrium. Circ Arrhythmia electrophysiol 5(4):650–658
Schuessler RB, Kay MW, Melby SJ, Branham BH, Boineau JP, Damiano RJ (2006) Spatial and temporal stability of the dominant frequency of activation in human atrial fibrillation. J Electrocardiol 39:S7–S12
Grace A, Willems S, Meyer C, Verma A, Heck P, Zhu M, Shi X, Chou D, Dang L, Scharf C, Scharf G, Beatty G (2019) High-resolution noncontact charge-density mapping of endocardial activation. JCI insight 4(6)
Shi R, Parikh P, Chen Z, Angel N, Norman M, Hussain W, Butcher C, Haldar S, Jones DG, Riad O, Markides V, Wong T (2020) Validation of dipole density mapping during atrial fibrillation and sinus rhythm in human left atriumJACC. Clinical electrophysiology 6(2):171–181
Gagyi RB, Noten AME, Lesina K, Mahmoodi BK, Yap S-C, Hoogendijk MG, Wijchers S, Bhagwandien RE, Szili-Torok T (2021) New possibilities in the treatment of brief episodes of highly symptomatic atrial Tachycardia: the usefulness of single-position single-beat charge density mapping. Circ Arrhythmia and electrophysiol 14(11):e010340
Pope MTB, Kuklik P, Gala ABE, Leo M, Mahmoudi M, Paisey J, Betts TR (2021) Spatial and temporal variability of rotational, focal, and irregular activity: practical implications for mapping of atrial fibrillation. J Cardiovasc Electrophysiol 32:2393–2403
Pope MTB, Kuklik P, Gala ABE, Leo M, Mahmoudi M, Paisey J, Betts TR (2022) Impact of adenosine on wavefront propagation in persistent atrial fibrillation: insights from global noncontact charge density mapping of the left atrium. J Am Heart Assoc: Cardiovasc Cerebrovasc Dis 11
Shi R, Chen Z, Butcher C, Zaman JA, Boyalla V, Wang YK, Riad O, Sathishkumar A, Norman M, Haldar S, Jones DG, Hussain W, Markides V, Wong T (2020) Diverse activation patterns during persistent atrial fibrillation by noncontact charge-density mapping of human atrium. J arrhythmia 36(4):692–702
Mickelsen SR, Angel N, Shah P, Shi X, Chou D (2021) B-PO05-085 Regional conduction velocity measurements: comparing contact and non-contact activation techniques. Heart Rhythm 18:S406
Pytkowski M, Jankowska A, Maciag A, Kowalik I, Sterlinski M, Szwed H, Saumarez RC (2008) Paroxysmal atrial fibrillation is associated with increased intra-atrial conduction delay. Europace 10:1415–1420
Zheng Y, Xia Y, Carlson J, Kongstad O, Yuan S (2017) Atrial average conduction velocity in patients with and without paroxysmal atrial fibrillation. Clin Physiol Funct Imaging 37:596–601
Grossi S, Grassi F, Galleani L, Bianchi F, SibonaMasi A, Conte MR (2016) Atrial conduction velocity correlates with frequency content of bipolar signal. Pacing clin electrophysiol : PACE 39(8):814–821
Grace A, Verma A, Willems S (2017) Dipole density mapping of atrial fibrillation. Eur heart j 38(1):5–9
Willems S, Verma A, Betts TR, Murray S, Neuzil P, Ince H, Steven D, Sultan A, Heck PM, Hall MC, Tondo C, Pison L, Wong T, Boersma LV, Meyer C, Grace A (2019) Targeting nonpulmonary vein sources in persistent atrial fibrillation identified by noncontact charge density mapping: UNCOVER AF Trial. Circulation. Arrhythmia electrophysiol 12(7):e007233
Bayly PV, KenKnight BH, Rogers JM, Hillsley RE, Ideker RE, Smith WM (1998) Estimation of conduction velocity vector fields from epicardial mapping data. IEEE trans bio-med eng 45(5):563–571
Barnette AR, Bayly PV, Zhang S, Walcott GP, Ideker RE, Smith WM (2000) Estimation of 3-D conduction velocity vector fields from cardiac mapping data. IEEE Trans Biomed Eng 47(8):1027–1035
Good WW, Gillette KK, Zenger B, Bergquist JA, Rupp LC, Tate J, Anderson D, Gsell MAF, Plank G, MacLeod RS (2021) Estimation and validation of cardiac conduction velocity and wavefront reconstruction using epicardial and volumetric data. IEEE Trans Biomed Eng 68(11):3290–3300
Wong GR, Nalliah CJ, Lee G, Voskoboinik A, Prabhu S, Parameswaran R, Sugumar H, Anderson RD, McLellan A, Ling L-H, Morton JB, Sanders P, Kistler PM, Kalman JM (2019) Dynamic atrial substrate during high-density mapping of paroxysmal and persistent AF. JACC: Clin Electrophysiol 5:1265–1277
Honarbakhsh S, Schilling RJ, Orini M, Providencia R, Keating E, Finlay M, Sporton S, Chow A, Earley MJ, Lambiase PD, Hunter RJ (2019) Structural remodeling and conduction velocity dynamics in the human left atrium: relationship with reentrant mechanisms sustaining atrial fibrillation. Heart Rhythm 16:18–25
Konings KTS, Kirchhof CJHJ, Smeets JRLM, Wellens HJJ, Penn OC, Allessie MA (2000) High-density mapping of electrically induced atrial fibrillation in humans. Springer, Netherlands, pp 549–567
Ng J, Kadish AH, Goldberger JJ (2007) Technical considerations for dominant frequency analysis. J cardiovasc electrophysiol 18(7):757–764
Li X, Chu GS, Almeida TP, Vanheusden FJ, Salinet J, Dastagir N, Mistry AR, Vali Z, Sidhu B, Stafford PJ, Schlindwein FS, Ng GA (2021) Automatic extraction of recurrent patterns of high dominant frequency mapping during human persistent atrial fibrillation. Front physiol 12:649486
Everett TH, Kok LC, Vaughn RH, Moorman JR, Haines DE (2001) Frequency domain algorithm for quantifying atrial fibrillation organization to increase defibrillation efficacy. IEEE trans bio-med eng 48(9):969–978
Everett TH, Moorman JR, Kok LC, Akar JG, Haines DE (2001) Assessment of global atrial fibrillation organization to optimize timing of atrial defibrillation. Circulation 103(23):2857–2861
Kogawa R, Okumura Y, Watanabe I, Kofune M, Nagashima K, Mano H, Sonoda K, Sasaki N, Ohkubo K, Nakai T, Hirayama A (2015) Spatial and temporal variability of the complex fractionated atrial electrogram activity and dominant frequency in human atrial fibrillation. J Arrhythmia 31:101–107
Li X, Chu GS, de Almeida TP, Salinet J, Mistry AR, Vali Z, Stafford PJ, Schlindwein FS, Ng GA (2018) Dominant frequency variability mapping for identifying stable drivers during persistent atrial fibrillation using noncontact mapping, Comput Cardiol
Zheng Y, Xia Y, Carlson J, Kongstad O, Yuan S (2017) Atrial average conduction velocity in patients with and without paroxysmal atrial fibrillation. Clin physiol funct imaging 37(6):596–601
Heida A, van Schie MS, van der Does WFB, Taverne YJHJ, Bogers AJJC, de Groot NMS (2021) Reduction of conduction velocity in patients with atrial fibrillation. J Clin Med 10:2614
Kurata N, Masuda M, Kanda T, Asai M, Iida O, Okamoto S, Ishihara T, Nanto K, Tsujimura T, Matsuda Y, Hata Y, Mano T (2020) Slow whole left atrial conduction velocity after pulmonary vein isolation predicts atrial fibrillation recurrence. J Cardiovasc Electrophysiol 31:1942–1949
Frontera A, Pagani S, Limite LR, Peirone A, Fioravanti F, Enache B, Cuellar Silva J, Vlachos K, Meyer C, Montesano G, Manzoni A, Dedé L, Quarteroni A, Lațcu DG, Rossi P, Della Bella P (2022) Slow conduction corridors and pivot sites characterize the electrical remodeling in atrial fibrillation. JACC Clin electrophysiol 8(5):561–577
Verma A, Lakkireddy D, Wulffhart Z, Pillarisetti J, Farina D, Beardsall M, Whaley B, Giewercer D, Tsang B, Khaykin Y (2011) Relationship between complex fractionated electrograms (CFE) and dominant frequency (DF) sites and prospective assessment of adding DF-guided ablation to pulmonary vein isolation in persistent atrial fibrillation (AF). J Cardiovasc Electrophysiol 22(12):1309–1316
Habel N, Znojkiewicz P, Thompson N, Müller JG, Mason B, Calame J, Calame S, Sharma S, Mirchandani G, Janks D, Bates J, Noori A, Karnbach A, Lustgarten DL, Sobel BE, Spector P (2010) The temporal variability of dominant frequency and complex fractionated atrial electrograms constrains the validity of sequential mapping in human atrial fibrillation. Heart Rhythm 7:586–593
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Drs Dang and Scharf are co-founder and shareholders of Acutus Meical Inc.
Drs Angel and Zhu were previously employees and shareholders of Acutus Medical Inc.
Dr Vesin has no disclosure.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dang, L., Angel, N., Zhu, M. et al. Correlation between conduction velocity and frequency analysis in patients with atrial fibrillation using high-density charge mapping. Med Biol Eng Comput 60, 3081–3090 (2022). https://doi.org/10.1007/s11517-022-02659-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02659-0