Abstract
HIV infection and aging are each associated with neurocognitive impairment (NCI). This study examined the combined effects of HIV infection and aging on NCI. We performed a cross-sectional survey among 345 HIV-infected and 345 HIV-uninfected participants aged at least 40 years. The International HIV Dementia Scale (IHDS) and Chinese version of Mini-mental State Examination (MMSE) were administered to screen for NCI. HIV-infected individuals had higher prevalence of NCI than uninfected individuals (46.7% vs 15.1% for IHDS using cut-off of ≤ 10; 17.1% vs 2.6% for MMSE). Significant main effects of HIV and age were observed on IHDS and MMSE composite scores and all domains except for HIV on attention and calculation. Significant interaction effects between HIV and age were observed on motor speed, orientation, registration and recall, and mainly attributed to the inferior performance of HIV-infected patients aged over 60 years. Among HIV-infected individuals, in multivariable logistic models, older age, depressive symptoms and history of nevirapine treatment were associated with NCI using both IHDS and MMSE, whereas lower education current smoker and current CD4 ≥ 800 cells/μL were associated only with NCI using IHDS, and hypertension was associated only with NCI using MMSE. Findings suggest that HIV and older age may confer interactive effects on cognitive function in several domains with older HIV-infected adults experiencing greater NCI, which requires further longitudinal investigation. Furthermore, HIV early diagnosis and treatment may prevent or reverse NCI, but extra attention should be given to adverse effects including metabolic changes associated with long-term treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People living with HIV often experience neurocognitive impairment (NCI), referred to as HIV-associated neurocognitive disorders (HAND) (Heaton et al. 2010). Combination antiretroviral therapy (cART) has led to significant reduction in severe forms of HAND. Yet, mild to moderate forms of HAND are still highly prevalent and may even have increased (Cysique et al. 2004; Heaton et al. 2010; Sacktor et al. 2016; Tozzi et al. 2007), partly due to the aging of HIV population. Globally, an estimated 3.6 million people older than 50 years are living with HIV including 2.9 million in low- and middle-income countries, and the number continues to increase in all regions (United Nations Programme on HIV/AIDS 2013). The other possible reasons for sustained prevalence of HAND include irreversible HIV-related brain injury and neurotoxicity of specific antiretroviral drugs (ARVs) (Ciccarelli et al. 2011; Heaton et al. 2010).
It is also suggested that HIV may accelerate cognitive aging which is possibly caused by direct damage from the virus as well as indirectly through increased risk of other comorbidities such as cardiovascular diseases or chronic immune activation, and thereby facilitates the early expression of age-related cognitive disorders (Cohen et al. 2015; Hellmuth et al. 2014; Imp et al. 2017; McCutchan et al. 2012; Wright et al. 2010). However, studies on the synergistic (interaction) effects of HIV and aging on neurocognitive performance showed mixed results. Most neuropsychological studies found the main effects of aging and HIV on cognitive abilities but didn’t identify the interaction effect (Ciccarelli et al. 2012; Valcour et al. 2011). Only a limited number of neuropsychological studies identified interaction effect of HIV and aging on verbal memory (Scott et al. 2011; Seider et al. 2014) but several neuroimaging studies found the interaction effects between HIV and aging in selected brain structures (Chang et al. 2013; Cysique et al. 2013; Kuhn et al. 2017; Pfefferbaum et al. 2014). It has to be noted that most of the neuropsychological studies either included no well-matched HIV-uninfected individuals for comparison or included only a small number of HIV-infected cases over 60 (Ciccarelli et al. 2012; Scott et al. 2011; Seider et al. 2014; Valcour et al. 2011), which may limit the ability to fully evaluate the interaction effect.
Thereby, this cross-sectional study was undertaken to determine if there is an interaction effect between HIV infection and aging on neurocognitive performance. HIV-infected individuals aged over 40 years and age-, gender-, education-matched HIV-negative individuals were recruited to participate in the study in China. Factors that might contribute to the high prevalence of NCI in HIV-infected adults were also explored.
Methods
Participants and Procedures
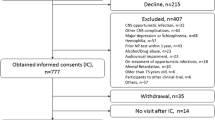
This study was conducted in Taizhou prefecture of Zhejiang province, China, as described elsewhere (Ding et al. 2017). HIV-infected individuals in Taizhou registered with the Chinese National Information System for AIDS Prevention and Control (CNISAPC) were consecutively enrolled in this special survey between June 2014 and May 2015, and were eligible if they were 40 years and above. HIV-uninfected participants were frequency matched in 1:1 ratio by sex, education and 5-year age categories to HIV cases, who were randomly selected from a sample of 1216 HIV-uninfected individuals recruited either from persons receiving HIV voluntary counseling and testing or routine physical examination at local Center for Disease Prevention and Control during the same study period, and were eligible if they were 40 years and above and also HIV-seronegative at the time of enrollment. The study was approved by the Institutional Review Board of Fudan University, Shanghai, China. All subjects provided informed consent prior to enrollment.
Data Collection
A standardized structured questionnaire was administered face-to-face by trained health staff to collect information on demographics, smoking, illicit drug use, and medical history regarding hypertension, diabetes and cardiovascular events (e.g., coronary artery disease). Physical examinations of height, weight, and blood pressure (BP) were carried out after the questionnaire has been completed. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Hypertension was defined as systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg, or current use of antihypertensive therapy.
All HIV-related characteristics were extracted from CNISAPC. Nadir CD4 count was defined as the lowest ever measured CD4 count between HIV diagnosis and the present survey. Current CD4 count was defined as the most recent CD4 count (within 2 months prior to the survey or within 1 month after the survey).
Depression and Insomnia Assessment
Depressive symptoms were measured by the 10-item version of Zung Self-Rating Depression Scale (Li et al. 2011; Zung 1973). Insomnia symptoms were measured based on Jenkins’s 4-item sleep questionnaire (Jenkins et al. 1988). Presence of insomnia symptoms was based on answers with “on most nights” or “on every night” to 1 or more questions.
Neurocognitive Assessment
All participants underwent face-to-face neurocognitive testing conducted by trained health staff using both the International HIV Dementia Scale (IHDS) and the Chinese version of Mini-mental State Examination (MMSE) in each participant. The two scales were chosen for three primary reasons: first, both are brief, easy to administer and highly applicable to resource-limited countries (Kamminga et al. 2013); second, IHDS is designed to identify HIV-associated dementia which is a subcortical dementia and has been confirmed to have high sensitivity to detect HAND among HIV-positive patients (Dang et al. 2015; Sacktor et al. 2005), and MMSE is originally developed to screen for cortical dementia and is the most widely used cognitive impairment screening instrument (Oshinaike et al. 2012); third, the pattern of NCI in the aged HIV-infected population is complex and includes symptoms of both cortical and subcortical dysfunctions (Cohen et al. 2015; Scott et al. 2011).
IHDS covers 3 domains: memory registration and recall, motor speed; psychomotor speed; each of these subtests is rated on a scale of 0–4. The cutoff score for defining NCI is 10 (Sacktor et al. 2005). Chinese version of MMSE takes the subjects’ education into account to define NCI if MMSE ≤ 19 for those with no formal education; MMSE ≤ 22 for those with primary school education (≤ 6 years); MMSE ≤ 26 for those with junior school education or above (≥ 7 years) (Zhang et al. 2006). It has a high sensitivity (90.8%) and specificity (93%) in the detection of dementia in the Chinese populations (Zhang et al. 2006). It covers the five domains: orientation of place and time, registration, attention and calculation, recall, language and visual construction.
Statistical Analysis
Analyses were performed using SAS software (version 9.11). Differences between groups were assessed by χ2 test, Fisher’s exact test, Student’s t-test, ANOVA or Kruskal-Wallis test as appropriate. A series of ANCOVA were run to test for main effects of age (40–49, 50–59 vs ≥ 60 years) and HIV serostatus (yes vs no) and the potential interaction between two variables on the neurocognitive scores of interest, controlling for education, depressive symptoms and hypertension which were associated with age or/and HIV infection as well as NCI based on bivariate analysis. Tukey post-hoc analyses comparing adjusted means were performed on all significant interactions in ANCOVA. Univariable and multivariable logistic regressions were performed to explore the determinants of NCI using the IHDS and MMSE, respectively. Variables with p < .10 in univariable analysis were included in multivariable model. Backward selection was used with retention at a significance level of p < .10. Sensitivity analysis was conducted to assess the robustness of the results using an IHDS score cut-off point of ≤ 9 for defining NCI, as suggested by Hosein and colleagues that it might be more appropriate for identifying NCI in those with low education level (2015).
Results
Participant Characteristics
Characteristics of 345 HIV-infected and 345 uninfected participants were summarized in Table 1. HIV-infected group was similar to HIV-uninfected group except the HIV-infected group had a lower proportion of hypertension and more depressive and insomnia symptoms (p < .05). With regards to HIV-related characteristics, the median time since HIV diagnosis was 3.0 years. About 87% was receiving cART, with the median treatment duration of 2.2 years.
In both HIV-infected and HIV-uninfected participants, compared to the age groups of 40–49 and 50–59 years, the oldest age group (60–82 years) were significantly less likely to have at least middle school education, but significantly more likely to have hypertension and a history of diabetes. HIV-infected participants aged 50–59 years were significantly less likely to have current CD4 count ≥ 500 cells/μL (Table 1).
Prevalence of Neurocognitive Impairment by HIV Serostatus and Age Group
As shown in Table 1, using cut-off of ≤ 10 for IHDS, 46.7% of HIV-infected participants were detected to have NCI compared to 15.1% of the uninfected participants (p < .01). Using the MMSE, 17.1% of HIV-infected participants were detected to have NCI compared with 2.6% of the uninfected participants (p < .01) (Table 1). In multivariable models adjusting for sex, education, BMI, current alcohol use, current smoker, hypertension, history of diabetes, history of cardiovascular events and depressive and insomnia symptoms, HIV infection is associated with NCI using the IHDS and MMSE, respectively (OR, 4.98 for IHDS using cut-off of ≤ 10; 95% CI, 3.24–7.66; p < .001; OR, 8.49 for MMSE; 95% CI, 3.78–19.07; p < .001). Furthermore, in both groups, the highest prevalence of NCI was observed in the age group of 60–82 years (p < .05), and such association (60–82 vs 40–49 years) remained significant (OR, 2.87 for IHDS using cut-off of ≤ 10; 95% CI, 1.73–4.76; p < .001; OR, 4.18 for MMSE, 95% CI, 1.99–8.77; p < .001) after adjusted for aforesaid potential confounding variables.
Main and Interaction Effects of HIV Serostatus and Age on Neurocognitive Performance
In ANCOVA model adjusting for education, depressive symptoms and hypertension, significant main effects of HIV and age on NCI were observed for all domains and IHDS and MMSE composite scores except for the main effect of HIV on attention and calculation (p = 0.070). Significant interaction effects were observed for motor speed, orientation, registration and recall, and also marginally significant interaction effects were observed for IHDS and MMSE composite scores (p = 0.094 and p = 0.099, respectively) (Table 2). Post-hoc analyses showed that interaction effect on recall was mainly attributable to the superior performance of the HIV-uninfected group aged 40–49 years and the inferior performance of the HIV-infected group aged 60–82 years, whereas the interaction effects on motor speed, orientation and registration were mainly attributable to the inferior performance of the HIV-infected group aged 60–82 years. Such attributions were also observable in Fig. 1a–d, showing that HIV-infected group aged 60–82 years had the much lower scores on these four domains than other five subgroups.
Factors Associated with NCI in HIV-Infected Patients Only
As shown in Table 3, in multivariable models, older age, more depressive symptoms, and history of nevirapine (NVP) treatment (vs efavirenz or EFV) were associated with NCI using IHDS with a cut-off of ≤10 and MMSE. Also, lower education level and current smoker were associated with NCI only using the IHDS with a cut-off of ≤ 10, while hypertension was associated with NCI only using the MMSE. In terms of HIV-related variables, only current CD4 count ≥ 800 cells/μL was negatively associated with NCI using the IHDS with a cut-off of ≤ 10.
In subgroup analysis restricted to those on cART (n = 300), similar variables were found to be significantly associated with NCI using IHDS with a cut-off of ≤ 10 and MMSE, respectively. But, current CD4 count ≥ 800 cells/μL was no longer significantly associated with NCI using the IHDS with a cut-off of ≤ 10. It is possibly due to the fact that among HIV-infected patients on cART, none of them with current CD4 count ≥ 800 cells/μL (n = 7) had NCI using IHDS or MMSE. Of note, duration on cART was negatively associated with NCI using the MMSE. In addition, among HIV-infected individuals without treatment (n = 45), only current smoker and hypertension were significantly associated with NCI using the IHDS with a cut-off of ≤ 10, and only depressive symptoms were significantly associated with NCI using the MMSE (data not shown).
Sensitivity Analysis
We repeated all the analysis using an IHDS score cut-off point of ≤ 9 for defining NCI. About 34.5% of HIV-infected participants were detected to have NCI compared to 8.7% of the uninfected participants (p < .01). Such association remained significant (OR, 5.73; 95% CI, 3.44–9.55; p < .001) after adjusting potential confounders. Similarly, the highest prevalence of NCI with a cut-off of ≤ 9 was observed in the age group of 60–82 years (p < .05), and such association (60–82 vs 40–49 years) remained significant (OR, 3.28; 95% CI, 1.88–5.72; p < .001) in multivariable model. Again, similar as using a cut-off of ≤ 10 for IHDS (Table 3), age, education, depressive symptoms, current CD4 count ≥ 800 cells/μL and history of NVP treatment were independently associated with NCI using IHDS with a cut-off of ≤ 9 at significance level of p < .05 except for current smoker (data not shown). In subgroup analysis restricted to those on cART (n = 300), similar variables as in all HIV-infected participants were found to be significantly associated with NCI using IHDS with a cut-off of ≤ 9 except for current CD4 count ≥ 800 cells/μL (data not shown).
Discussion
Approximately a half of HIV-infected participants were detected to have NCI using the IHDS, which were similar to previous reports from Africa (Cross et al. 2013; Oshinaike et al. 2012), but higher than reports from developed countries (Ku et al. 2014). The discrepancy may be due to the older age of participants or/and the later initiation of cART in developing countries in these studies. In contrast, 17.1% of participants had NCI using the MMSE. This was consistent with previous observations that MMSE detected a lower rate of NCI than IHDS, possibly because of lacking sensitivity to HIV-related subcortical dysfunctions (Oshinaike et al. 2012). Consistent with other research (Bonnet et al. 2013; Oshinaike et al. 2012), HIV-infected patients were more likely to be cognitively impaired than similar but uninfected individuals. Furthermore, the prevalence of NCI was highest in the oldest age group. These support the previous findings that HIV and aging are independent risk factors for reduced neurocognitive performance (Ciccarelli et al. 2012; Valcour et al. 2011).
Importantly, in contrast to previous neuropsychological studies identifying either no interaction effect or interaction effect only on verbal memory (Ciccarelli et al. 2012; Scott et al. 2011; Seider et al. 2014; Valcour et al. 2011), we observed significant interaction effects between HIV infection and age on motor speed, orientation, registration and recall. Some neuroimaging studies also identified the interaction effects between HIV and aging in selective brain functions (Chang et al. 2013; Kuhn et al. 2017). This may be due to the fact that our study included a relatively large sample of older HIV-infected cases aged over 60 years, as suggested by Scott et al. that a lag occurs between when brain changes and when changes can be observed on neuropsychological tests (Seider et al. 2014). Post hoc analysis further indicated that the interaction effects on motor speed and recall were mainly attributed to the youngest HIV-uninfected age group and the oldest HIV-infected age group, whereas interaction effects on orientation and registration were mainly attributed to the oldest HIV-infected age group. These support the evidence that HIV infection and older age act synergistically to affect some domains of cognitive function. It is possible that HIV accelerates age-associated cognitive decline (Cohen et al. 2015; Hellmuth et al. 2014) but it is also possible that age exacerbates the adverse effects of HIV on NCI among older HIV-infected patients as prevalence of co-morbidities is rapidly increasing (Cysique and Brew 2014). Our findings further suggest that among HIV-infected population, different cognitive domains have different dynamic changes with age as a combined effect of HIV infection and aging, which may be attributed to different mechanisms.
In terms of HIV-related and treatment factors, we found that a much lower prevalence of NCI, comparable to the prevalence in HIV-uninfected individuals, was seen in those with current CD4 count above 800 cells /μL, which is the lower tail of the CD4 count distribution in HIV-infected persons and associated with ART initiation at earlier stage of HIV infection (Le et al. 2013). This may explain the findings from a previous study that low prevalence of NCI was observed among early diagnosed and treated HIV-infected patients (Crum-Cianflone et al. 2013). Also, we found that NVP in comparison to EFV was associated with more NCI, which appears to conflict with other reports indicating that EFV is associated with cognitive disorders (Ciccarelli et al. 2011; Winston et al. 2012). However, in these studies the drug for comparison was either not NVP (Ciccarelli et al. 2011) or undefined (Winston et al. 2012). NVP has a higher central nervous system (CNS) penetration-effectiveness (CPE) rank than EFV and high CPE is associated with poor neuropsychological tasks (Libertone et al. 2014). Animal studies indicated that both NVP and EFV had CNS toxicity (Romão et al. 2011; Streck et al. 2008). These combined with our results suggest the possibility that NVP may increase the risk for NCI. But, two possible explanations should be noted. First, NVP is recommended to be prescribed to patients with lower CD4 count as compared to EFV. The other is that clinicians avoid to use EFV in patients with history of psychiatric disorders or suspected to have some level of NCI.
Other factors for NCI identified in HIV-infected patients included lower education level, smoking, hypertension, depressive and insomnia symptoms. Cognitive reserve has been found to be a protective factor for older HIV-positive adults who are at high risk for cognitive decline, and education is an important component of cognitive reserve (Foley et al. 2012; Morgan et al. 2012). It should be also noted that education and depression may be the factors impacting neuropsychological testing performance (Antinori et al. 2007). The association of depression with NCI was consistent with other research (Cross et al. 2013) and should be noted because it is highly prevalent in HIV-infected patients. Current guidelines recommend the initiation of ART in all HIV-infected individuals regardless of CD4 count. Consistent with other studies (Wright et al. 2010, 2015), the association of overweight and hypertension with NCI underscores the importance of attention to the metabolic side effects of treatment and its combined effects with HIV infection and aging on NCI.
Our study had several limitations. We conducted a cross-sectional study, hence could not assess temporality or causation between factors of interest and the development of NCI. Second, NCI was detected by IHDS and MMSE, a full battery of neurocognitive tests to diagnose NCI was not administered. The major issue with IHDS is its relatively lower specificity when using a high cut-off point for positive screen although with high sensitivity (Goodkin et al. 2014), but our sensitivity analysis revealed that there is not much change in significant variables identified when using a cut-off of ≤ 9 for IHDS. In addition, the relatively short duration of treatment limited the ability to explore the impact of metabolic changes associated with treatment on the development of NCI.
In conclusion, we found that HIV and aging act synergistically on several domains of cognitive function, and also such interaction effects are mainly attributed to the inferior performance of older HIV-infected patients. Additional follow-up studies are warranted to observe the trajectories of cognitive changes among HIV-infected versus HIV-uninfected individuals with NCI. In addition, our findings suggest that early diagnosis of HIV infection and early treatment initiation that restoring or maintaining CD4 count above 800 cells/μL may prevent or reverse the presence of NCI, but extra attention should be given to the metabolic changes and other adverse effects due to long-term treatment and their impact on the development of NCI.
References
Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, Clifford DB, Cinque P, Epstein LG, Goodkin K, Gisslen M, Grant I, Heaton RK, Joseph J, Marder K, Marra CM, JC MA, Nunn M, Price RW, Pulliam L, Robertson KR, Sacktor N, Valcour V, Wojna VE (2007) Updated research nosology for HIV-associated neurocognitive disorders. Neurology 69:1789–1799
Bonnet F, Amieva H, Marquant F, Bernard C, Bruyand M, Dauchy FA, Mercié P, Greib C, Richert L, Neau D, Catheline G, Dehail P, Dabis F, Morlat P, Dartigues JF, Chêne G, S CO3 Aquitaine Cohort (2013) Cognitive disorders in HIV-infected patients: are they HIV-related? AIDS 27:391–400
Chang L, Holt JL, Yakupov R, Jiang CS, Ernst T (2013) Lower cognitive reserve in the aging human immunodeficiency virus-infected brain. Neurobiol Aging 34:1240–1253
Ciccarelli N, Fabbiani M, Di Giambenedetto S, Fanti I, Baldonero E, Bracciale L, Tamburrini E, Cauda R, De Luca A, Silveri MC (2011) Efavirenz associated with cognitive disorders in otherwise asymptomatic HIV-positive patients. Neurology 76:1403–1409
Ciccarelli N, Fabbiani M, Baldonero E, Fanti I, Cauda R, Di Giambenedetto S, Silveri MC (2012) Effect of aging and human immunodeficiency virus infection on cognitive abilities. J Am Geriatr Soc 60:2048–2055
Cohen RA, Seider TR, Navia B (2015) HIV effects on age-associated neurocognitive dysfunction: premature cognitive aging or neurodegenerative disease? Alzheimers Res Ther 7:37
Cross S, Önen N, Gase A, Overton ET, Ances BM (2013) Identifying risk factors for HIV-associated neurocognitive disorders using the international HIV dementia scale. J NeuroImmune Pharmacol 8:1114–1122
Crum-Cianflone NF, Moore DJ, Letendre S, Poehlman Roediger M, Eberly L, Weintrob A, Ganesan A, Johnson E, Del Rosario R, Agan BK, Hale BR (2013) Low prevalence of neurocognitive impairment in early diagnosed and managed HIV-positive persons. Neurology 8:371–379
Cysique LA, Brew BJ (2014) The effects of HIV and aging on brain functions: proposing a research framework and update on last 3 years’ findings. Curr Opin HIV AIDS 9:355–364
Cysique LA, Maruff P, Brew BJ (2004) Prevalence and pattern of neuropsychological impairment in human immunodeficiency virus positive/acquired immunodeficiency syndrome (HIV/AIDS) patients across pre and post-highly active antiretroviral therapy eras: a combined study of two cohorts. J Neuro-Oncol 10:350–357
Cysique LA, Lane T, Moffat K, Lane TA, Davies NW, Carr A, Brew BJ, Rae C (2013) HIV, vascular and aging injuries in the brain of clinically stable HIV-infected adults: a (1)H MRS study. PLoS One 8:e61738
Dang C, Wei B, Long J, Zhou M, Han X, Zhao T (2015) Validity of the international HIV dementia scale as assessed in a socioeconomically underdeveloped region of southern China. Int J Infect Dis 33:56–61
Ding Y, Lin H, Liu X, Wong F, Sun Y, Marconi V, He N (2017) Higher prevalence of frailty among a sample of Chinese HIV-infected middle-aged and older adults is associated with neurocognitive impairment and depressive symptoms. J Infect Dis 215: 687–692
Foley JM, Ettenhofer ML, Kim MS, Behdin N, Castellon SA, Hinkin CH (2012) Cognitive reserve as a protective factor in older HIV-positive patients at risk for cognitive decline. Applied Neuropsychology Adult 19:16–25
Goodkin K, Hardy DJ, Singh D, Lopez E (2014) Diagnostic utility of the international HIV dementia scale for HIV-associated neurocognitive impairment and disorder in South Africa. J Neuropsychiatr Clin Neurosci 26:352–358
Heaton RK, Clifford DB, Franklin DR Jr, Woods SP, Ake C, Vaida F, Ellis RJ, Letendre SL, Marcotte TD, Atkinson JH, Rivera-Mindt M, Vigil OR, Taylor MJ, Collier AC, Marra CM, Gelman BB, JC MA, Morgello S, Simpson DM, McCutchan JA, Abramson I, Gamst A, Fennema-Notestine C, Jernigan TL, Wong J, Grant I; CHARTER Group (2010) HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER study. Neurology 75:2087–2096
Hellmuth J, Milanini B, Valcour V (2014) Interactions between aging and NeuroAIDS. Curr Opin HIV AIDS 9:527–532
Hosein MM, Saylor D, Nakigozi G, Nakasujja N, Kong X, Robertson K, Gray RH, Wawer MJ, Sacktor N (2015) Validation of the international HIV dementia scale screening tool for HAND in Uganda. Conference on retroviruses and opportunistic infections, Seattle, USA. Abstract Number: 453
Imp BM, Rubin LH, Tien PC, Plankey MW, Golub ET, French AL, Valcour VG (2017) Monocyte activation is associated with worse cognitive performance in HIV-infected women with virologic suppression. J Infect Dis 215:114–121
Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM (1988) A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol 41:313–321
Kamminga J, Cysique LA, Lu G, Batchelor J, Brew BJ (2013) Validity of cognitive screens for HIV-associated neurocognitive disorder: a systematic review and an informed screen selection guide. Current HIV/AIDS Rep 10:342–355
Ku NS, Lee Y, Ahn JY, Song JE, Kim MH, Kim SB, Jeong SJ, Hong KW, Kim E, Han SH, Song JY, Cheong HJ, Song YG, Kim WJ, Kim JM, Smith DM, Choi JY (2014) HIV-associated neurocognitive disorder in HIV-positive Koreans: the Korean NeuroAIDS project. HIV Med 15:470–477
Kuhn T, Schonfeld D, Sayegh P, Arentoft A, Jones JD, Hinkin CH, Bookheimer SY, Thames AD (2017) The effects of HIV and aging on subcortical shape alterations: a 3D morphometric study. Hum Brain Mapp 38:1025–1037
Le T, Wright EJ, Smith DM, He W, Catano G, Okulicz JF, Young JA, Clark RA, Richman DD, Little SJ, Ahuja SK (2013) Enhanced CD4+T-cell recovery with early HIV-1 antiretroviral therapy. N Engl J Med 368:218–230
Li L, Ji G, Liang LJ, Ding Y, Tian J, Xiao Y (2011) A multi-level intervention for HIV affected families: together for empowerment activities (TEA). Soc Sci Med 73:1214–1221
Libertone R, Lorenzini P, Balestra P, Pinnetti C, Ricottini M, Plazzi MM, Menichetti S, Zaccarelli M, Nicastri E, Bellagamba R, Ammassari A, Antinori A (2014) Central nervous system penetration-effectiveness rank does not reliably predict neurocognitive impairment in HIV-infected individuals. J Int AIDS Soc 17:19655
McCutchan JA, Marquie-Beck JA, Fitzsimons CA, Letendre SL, Ellis RJ, Heaton RK, Wolfson T, Rosario D, Alexander TJ, Marra C, Ances BM, Grant I; CHARTER Group (2012) Role of obesity, metabolic variables, and diabetes in HIV-associated neurocognitive disorder. Neurology 78:485–492
Morgan EE, Woods SP, Smith C, Weber E, Scott JC, Grant I (2012) Lower cognitive reserve among individuals with syndromic HIV-associated neurocognitive disorders (HAND). AIDS Behav 16:2279–2285
Oshinaike OO, Akinbami AA, Ojo OO, Ojini IF, Okubadejo UN, Danesi AM (2012) Comparison of the Minimental state examination scale and the international HIV dementia scale in assessing cognitive function in Nigerian HIV patients on antiretroviral therapy. AIDS Res Ther 2012:581531
Pfefferbaum A, Rogosa DA, Rosenbloom MJ, Chu W, Sassoon SA, Kemper CA, Deresinski S, Rohlfing T, Zahr NM, Sullivan EV (2014) Accelerated aging of selective brain structures in human immunodeficiency virus infection: a controlled, longitudinal magnetic resonance imaging study. Neurobiol Aging 35:1755–1768
Romão PR, Lemos JC, Moreira J, de Chaves G, Moretti M, Castro AA, Andrade VM, Boeck CR, Quevedo J, Gavioli EC (2011) Anti-HIV drugs nevirapine and efavirenz affect anxiety-related behavior and cognitive performance in mice. Neurotox Res 19:73–80
Sacktor N, Wong M, Nakasujja N, Skolasky RL, Selnes OA, Musisi S, Robertson K, McArthur JC, Ronald A, Katabira E (2005) The international HIV dementia scale: a new rapid screening test for HIV dementia. AIDS 19:1367–1374
Sacktor N, Skolasky RL, Seaberg E, Munro C, Becker JT, Martin E, Ragin A, Levine A, Miller E (2016) Prevalence of HIV-associated neurocognitive disorders in the multicenter AIDS cohort study. Neurology 86:334–340
Scott JC, Woods SP, Carey CL, Weber E, Bondi MW, Grant I. The HIV Neurobehavioral Research Center (HNRC) Group (2011) Neurocognitive consequences of HIV infection in older adults: an evaluation of the “cortical” hypothesis. AIDS Behav 15:1187–1196
Seider TR, Luo X, Gongvatana A, Devlin KN, de la Monte SM, Chasman JD, Yan P, Tashima KT, Navia B, Cohen RA (2014) Verbal memory declines more rapidly with age in HIV infected versus uninfected adults. J Clin Exp Neuropsychol 36:356–367
Streck EL, Scaini G, Rezin GT, Moreira J, Fochesato CM, Romão PRT (2008) Effects of the HIV treatment drugs nevirapine and efavirenz on brain creatine kinase activity. Metab Brain Dis 23:485–492
Tozzi V, Balestra P, Bellagamba R, Corpolongo A, Salvatori MF, Visco-Comandini U, Vlassi C, Giulianelli M, Galgani S, Antinori A, Narciso P (2007) Persistence of neuropsychologic deficits despite long-term highly active antiretroviral therapy in patients with HIV-related neurocognitive impairment: prevalence and risk factors. J Acquir Immune Defic Syndr 45:174–182
United Nations Programme on HIV/AIDS (UNAIDS) (2013) HIV and Aging: a special supplement to the UNAIDS report on the global AIDS epidemic, 2013. Retrieved online: February 23, 2016 at: http://www.unaids.org/sites/default/files/media_asset/20131101_JC2563_hiv-and-aging_en_0.pdf
Valcour V, Paul R, Neuhaus J, Shikuma C (2011) The effects of age and HIV on neuropsychological performance. J Int Neuropsychol Soc 17:190–195
Winston A, Puls R, Kerr SJ, Duncombe C, Li PC, Gill JM, Taylor-Robinson SD, Emery S, Cooper DA, Altair Study Group (2012) Dynamics of cognitive change in HIV-infected individuals commencing three different initial antiretroviral regimens: a randomized, controlled study. HIV Med 13:245–251
Wright EJ, Grund B, Robertson K, Brew BJ, Roediger M, Bain MP, Drummond F, Vjecha MJ, Hoy J, Miller C, Penalva de Oliveira AC, Pumpradit W, Shlay JC, El-Sadr W, Price RW, INSIGHT SMART Study Group (2010) Cardiovascular risk factors associated with lower baseline cognitive performance in HIV-positive persons. Neurology 75:864–873
Wright EJ, Grund B, Cysique LA, Robertson KR, Brew BJ, Collins G, Shlay JC, Winston A, Read TR, Price RW, International Network for Strategic Initiatives in Global HIV Trials (INSIGHT) START Study Group (2015) Factors associated with neurocognitive test performance at baseline: a substudy of the INSIGHT strategic timing of AntiRetroviral treatment (START) trial. HIV Med 16(Suppl 1):97–108
Zhang ZX, Zahner GE, Román GC, Liu XH, Wu CB, Hong Z, Hong X, Tang MN, Zhou B, Qu QM, Zhang XJ, Li H (2006) Socio-demographic variation of dementia subtypes in china: methodology and results of a prevalence study in Beijing, Chengdu, shanghai, and Xian. Neuroepidemiology 27:177–187
Zung WWK (1973) From art to science: the diagnosis and treatment of depression. Arch Gen Psychiatry 29:328–337
Acknowledgements
The authors wish to thank all study participants for taking part in the study. This study was supported by the Shanghai Municipal Health and Family Planning Commission (GWTD2015S05, 15GWZK0101), the Natural Science Foundation of China (grant number 81373062, 81402725), and the Junior Faculty Award of Fudan University (grant number JJF201016).
Author information
Authors and Affiliations
Contributions
Y. D. and N. H. conceived and designed the study. Y. D. and H. L. supervised the participant recruitment and data collection. M. G., W. S., and Q.W. recruited the participants and collected data. Y. D. analyzed the data and wrote the first draft of the manuscript. All authors contributed to data interpretation and writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ding, Y., Lin, H., Shen, W. et al. Interaction Effects between HIV and Aging on Selective Neurocognitive Impairment. J Neuroimmune Pharmacol 12, 661–669 (2017). https://doi.org/10.1007/s11481-017-9748-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11481-017-9748-3