Abstract
The aim of this study was to estimate the prevalence and probabilities of comorbidities between self-reported PTSD and smoking, alcohol binge drinking and substance use disorders (SUDs) from a national Canadian sample. Data were taken from the Statistics Canada Public Use Microdata File of the 2012 Canadian Community Health Survey–Mental Health (n = 17,311). The prevalence of (a) smoking, (b) alcohol binge drinking and (c) SUDs was estimated among those with a PTSD diagnosis versus those without a PTSD diagnosis. After controlling for potential socioeconomic and mental health covariates, self-reported PTSD acted as a significant predictor for membership in the heaviest smoking, alcohol, and substance use categories. Individuals self-reporting a diagnosis of PTSD have a significantly higher likelihood of engaging in smoking and alcohol binge drinking, and are more likely to meet criteria for SUDs than individuals not reporting a PTSD diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Post-traumatic stress disorder (PTSD) is a disabling psychiatric disorder that reflects an inability to cope with overwhelming stress caused by trauma that is followed by a distinctive pattern of symptoms. Most research pertaining to PTSD has been conducted on military veterans; however, research on community populations in Canada has indicated a prevalence of lifetime PTSD of approximately 9.2%, with a rate of current (1-month) PTSD of 2.4% (Van Ameringen et al. 2008). PTSD also commonly co-occurs with other impairing psychiatric disorders, and epidemiologic surveys estimate that 80% of individuals with PTSD meet criteria for at least one other psychiatric diagnosis (Brady 1997). PTSD is particularly likely to be comorbid with mood disorders, other anxiety disorders, dissociative disorders and substance use disorders (SUDS; Galatzer-Levy et al. 2013).
Drug and alcohol use is common in individuals with PTSD with research suggesting that individuals with PTSD are two to three times more likely than those without PTSD to have a SUD (Kessler et al. 1995). In addition, surveys of those seeking treatment for SUDs have revealed that between 25 and 58% of these individuals have comorbid PTSD (Brady 1997; Galatzer-Levy et al. 2013; Mills et al. 2006); however, research using population-based samples is limited. Research in this area is important because it will allow for early identification and treatment, and the current research will fill this gap in the literature by exploring the prevalence and probabilities of PTSD in relation to smoking, binge drinking and SUDs based on self-report data from a large nationwide Canadian sample.
PTSD and Comorbid Disorders
It has been consistently shown that individuals with PTSD are more likely than those without PTSD to have substantial psychiatric comorbidity (Hernandez et al. 2013; Mills et al. 2006). Population-based surveys have demonstrated that the lifetime prevalence of PTSD with any other mental health (MH) disorder is approximately 79% (Kessler et al. 1995), and have indicated that PTSD is most commonly associated with anxiety disorders, major depression disorder, bipolar disorder and SUDs (Cerimele et al. 2017; Galatzer-Levy et al. 2013).
Approximately, 16% of patients with PTSD have one other psychiatric diagnosis, 17% have two other psychiatric diagnoses, and nearly 50% have three or more additional psychiatric diagnoses, which indicates that comorbidity between PTSD and other MH diagnoses is the rule rather than the exception (Brady 1997). It is difficult to tell whether the development of PTSD contributes to the development of MH disorders, or whether MH disorders contribute to the development of PTSD. One possible explanation is that a prior history of MH disorders might be associated with an increased probability of trauma exposure resulting in an increased risk of developing PTSD (Wild et al. 2016). The other possible explanation is that PTSD might be associated with increased risk of subsequent disorders (Kessler 2000; Sharkansky et al. 1999). Regardless of which disorder predisposes the development of the other, the co-occurrence of PTSD with other psychiatric disorders can be complex. At least a third of the individuals who develop PTSD remain symptomatic for 3 years or longer, and are at risk of secondary problems such as SUDs (Kessler et al. 1995).
PTSD and Comorbid SUDs
PTSD and SUDs frequently co-occur, and the overlap between these disorders has been an area of increasing clinical, research and public health interest (Kaysen et al. 2014; Kline et al. 2014; Miller et al. 2006; Ouimette et al. 2003; Read et al. 2013). A problem stemming from substance use related to PTSD symptoms is the development of SUDs with repeated use.
Although substance use can induce sensations of euphoria and well-being, these sensations are generally outweighed by negative consequences. These negative consequences include accidents leading to physical harm of self and others, impaired social relationships, and engaging in law-breaking behaviours and incurring subsequent difficulties with the law (Symmes et al. 2015). Specific drugs may also have other detrimental effects on one’s physical well-being, including sleep disturbances and irregular sleeping patterns (Ogeil et al. 2011), acute memory problems, psychomotor impairment and bronchial or pulmonary illnesses (Fischer et al. 2012). Substances are often abused as means of coping with the negative symptoms of PTSD, and as a result, the individual can become vulnerable to developing SUDs, which could exacerbate other issues and make treatment of the disorder less effective (Bremner et al. 1996).
Regardless of which substance has contributed to the problem, by the time an individual has developed a diagnosable SUD, substance use will have adversely affected their overall level of functioning and their physical and mental health. Among individuals with co-occurring PTSD and SUDs, the symptoms of PTSD and SUDs tend to be more severe, which is supported by evidence that the comorbidity is associated with a higher rate of psychosocial and medical problems and higher utilization of inpatient hospitalization (Trivedi et al. 2015). Additionally, individuals with comorbid PTSD and SUDs are more prone to substance use relapse than individuals without PTSD (Brown et al. 1996). Once SUDs develop in individuals with PTSD, any effort to treat the disorders becomes increasingly complicated (Mills 2013).
While a specific mechanism to explain why individuals with a diagnosis of PTSD abuse substances is uncertain, it is known that substance use can exacerbate PTSD symptoms and lead to worse outcomes than either disorder alone. It is essential that health professionals are aware of comorbid substance abuse or dependence among those with PTSD because of the severity of these co-occurring disorders and the special attention that the comorbidity requires.
The Current Study
While there is a body of research investigating the associations between PTSD and smoking, alcohol use and substance abuse or dependence, there has been no comprehensive investigation of these relationships using a population-based study within a Canadian context. The aim of this study will be to estimate the prevalence and probabilities of PTSD and smoking, binge drinking and SUDs from a nationwide Canadian sample. It is anticipated that increased levels of smoking and binge drinking will be observed in participants reporting a diagnosis of PTSD. Additionally, it is also anticipated that SUDs will be observed more frequently in participants reporting a diagnosis of PTSD.
Method
Participants
Data from the Public Use Microdata File of the 2012 Canadian Community Health Survey (CCHS; Statistics Canada 2013) were analyzed. During this year, the CCHS assessed the mental health (MH) status of Canadians in terms of selected MH disorders, assessed functioning in relation to MH and examined potential links between MH and sociodemographic variables. Respondents for the survey were selected in three stages. First, geographical areas were selected, followed by households within each geographical area. Finally, one respondent from each household was randomly selected. The national response rate for the survey was 68.9% with the CCHS-MH providing cross-sectional data from 25,113 Canadians aged 15 years or older who were residing in private residences in the 10 provinces at the time of the survey. Statistics Canada (2013) estimates the total number of individuals excluded from the survey to represent less than 3% of the target population. In the survey database, age is recorded categorically and ranges from “15 to 19 years” to “80 years or older”. As the focus of the present study was on adults, individuals in the age category “15 to 19 years” (n = 2024 and age categories 65 years and older (n = 6117) were not included in the analyses. The sample size for each outcome measure is recorded individually in each “Results” subsection of this article.
Data Collection
The majority of interviews (87%) for the CCHS-MH (Statistics Canada 2013) were conducted in person with the remaining interviews completed via telephone. No proxy interviews were allowed. Interviews were conducted by lay people trained by representatives from Statistics Canada’s Collection Planning and Management Division. Interviews were completed using the computer-assisted personal interviewing (CAPI) method, which allows for customs interviews for each respondent based on his or her individual characteristics and survey results, ensuring that interviewers do not ask questions that do not apply to the respondent (Statistics Canada 2013). Data were collected during the period from January to December 2012. The survey sample does not include individuals living in the three Canadian territories, individuals living on reserves, full-time members of the Canadian Forces or individuals who are institutionalized.
Materials
Self-report of PTSD
As part of the CCHS-MH interview, respondents were asked to indicate whether they had been diagnosed by a health professional with a variety of mental health conditions that had lasted or were expected to last for 6 months or longer. One of these questions was, “Do you have post-traumatic stress disorder?” (no/yes). Prevalence of PTSD was determined based on the number of individuals in the entire sample of respondents who responded “yes” to the question of whether they had been diagnosed by a health professional with PTSD.
Substance Abuse Behaviours
Alcohol abuse and dependence and substance use, abuse and dependence modules do not require screening questions as all respondents are administered a minimum set of questions on smoking, alcohol and substance use. The questions used for the CCHS-MH modules on nicotine use, alcohol abuse and dependence, and substance abuse and dependence are based on a recognized WHO version of the Composite International Diagnostic Interview (CIDI) modified for the needs of CCHS-MH (Statistics Canada 2013). The WHO-CIDI is a standardized instrument for the assessment of mental disorders and conditions based on the definitions and criteria of Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; APA 1994) and International Classification of Diseases and Related Health Problems (ICD-10; WHO 1992). Mental conditions or problems found in the CCHS-MH are partially coded to DSM-IV (Statistics Canada 2013).
Computer-based algorithms were used to calculate criteria for each disorder based on respondents’ answers to the questions within each disorder module. For each disorder, 12-month criteria included meeting the criteria for a lifetime diagnosis of the disorder, experiencing an episode of the disorder within the previous 12 months, and experiencing a marked impairment in occupational and social functioning. Smoking habits, frequency of alcoholic beverage consumption and criteria for substance abuse or dependence (including cannabis) were examined over a 12-month period.
Type of Smoker
Type of smoker assessed smoking habits (daily smoker, occasional smoker or not at all). Type of smoker was assessed with the question, “At the present time, do you smoke cigarettes daily, occasionally or not at all?”
Alcohol Binge Drinking
Alcohol binge drinking is assessed by the frequency of consuming more than five drinks at one occasion within the previous 12 months (never, less than once a month, once a month, 2 to 3 times a month, once a week, more than once a week). Alcohol binge drinking was assessed with the question, “How often in the past 12 months have you had 5 or more drinks on one occasion?”
Substance Abuse or Dependence
Substance abuse or dependence is a composite variable that identifies whether the respondent meets CCHS-MH/WHO-CIDI criteria for any drug abuse or drug dependence for the past 12 months. The respondents’ use of illegal drugs or nonmedical use of prescription drugs during the past 12 months was assessed with questions such as, “The second group of medicines is stimulants, sometimes called speed, ice, glass, crystal, crank, pep pills, or uppers. These are medicines that people sometimes use to stay awake, to improve their low mood, or to lose weight. Examples include dexamyl, methamphetamine, Adderall, and Ritalin. Have you ever used a stimulant non-medically?” and “Have you used it in the past 12 months?” Substances included in this variable are cannabis, cocaine/crack, club drugs, hallucinogens, heroin/opium, inhalants/solvents or any other substances.
Sociodemographic Covariates
A battery of sociodemographic covariates was used within the regression analyses, which included sex (male/female), age (5-year increments from 20 to 64), race (White/non-White), marital status (married, common-law, widowed, divorced/separated, single), education (less than high school, high school, some post-secondary, post-secondary graduation), income in Canadian dollars (less than $10,000; $10,000–$19,999; $20,000–$29,999; $30,000–$39,999; $40,000–$49,999; and $50,000 and above) and province (see Table 1 for descriptive statistics).
Mental Health Covariates
Mental health covariates were also included in the regression analyses. These covariates included diagnoses of General Anxiety Disorder (GAD), Major Depressive Disorder (MDD) and/or Bipolar Disorder (BP). These mental health variables are included because they are known to be comorbid with PTSD (Hernandez et al. 2013; Price and Van Stolk-Cooke 2015), and it is important to account for their effect on the relationships between PTSD and smoking, alcohol binge drinking and SUDs.
To reduce respondent burden, the survey modules for depression, generalized anxiety disorder and bipolar disorder were preceded by a section with screener questions for each disorder. Participants who responded “no” to the screening questions were not asked questions from the module associated with that disorder and were categorized as failing to meet the criteria for that disorder. The questions used for the CCHS-MH modules on GAD, MDD and bipolar I and II disorders (BPD I and II) are based on a recognized World Health Organization version of the Composite International Diagnostic Interview (WHO-CIDI) modified for the needs of CCHS-MH (Statistics Canada 2013). The WHO-CIDI is a standardized instrument for the assessment of mental disorders and conditions based on the definitions and criteria of Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association 1994) and International Classification of Diseases and Related Health Problems (ICD-10; World Health Organization 1992). Mental conditions or problems found in the CCHS-MH are partially coded to DSM-IV (Statistics Canada 2013). Computer-based algorithms were used to calculate lifetime criteria for each disorder based on respondents’ answers to the questions within each disorder module. For each disorder, 12-month criteria included meeting the criteria for a lifetime diagnosis of the disorder, experiencing an episode of the disorder within the previous 12 months, and experiencing a marked impairment in occupational and social functioning (see Table 1 for descriptive statistics).
Data Analysis
Hierarchical multinomial logistic regression (cigarette smoking and binge drinking) and hierarchical binary logistic regression (drug abuse or dependence) were used to investigate whether PTSD predicted substance abuse or disorders. Odds ratios (ORs) or relative risk ratios (RRRs) were used for each model to remain consistent with previous research (Saunders et al. 2015; Sripada et al. 2014). In each model, demographic covariates (age, sex, race, marital status, household income, education and province of residence) were assessed in Block 1, and mental health covariates were assessed in Block 2. Mental health covariates were chosen because of their relationships with either PTSD or SUDs. Finally, PTSD was assessed as a predictor in Block 3. Data were weighted in accordance with instructions from CCHS-MH user guide (Statistics Canada 2013).
Researchers used a weighting variable provided by Statistics Canada (2013) to ensure that the analyses were representative of the broader Canadian population. All regression models used heteroscedastic-consistent corrections in their estimation of standard error. All significant results of interest to the researchers were discussed in the context of their effect sizes, because small differences between groups may become statistically significant at high levels of statistical power. Significant effect sizes that were less than small (i.e. Cohen’s d < .20) were not discussed substantively as they failed to meet the cut-off point. All data analysis was performed with Stata 15.
Results
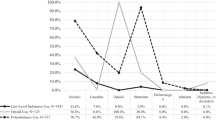
Prevalence of Substance Use
Researchers assessed the prevalence rates of SUDs across those who reported a diagnosis of PTSD, Bipolar I/II, GAD or ADHD versus those who did not report a diagnosis. Results suggest that the incidence of smoking, alcohol use and substance abuse or dependence is greater for those who reported a diagnosis of PTSD, Bipolar I/II, GAD or ADHD than those who did not report a diagnosis of these disorders. The prevalence rates of smoking, alcohol use, and substance abuse or dependence across people reporting a diagnosis of PTSD, Bipolar I/II, GAD or ADHD compared with those who do not have a diagnosis is reported in Table 2.
Type of Smoker (n = 16,557)
Using hierarchical multinomial logistic regression, researchers regressed smoking categories (using “Daily Smoker” as the base category) onto demographic covariates in Block 1, χ2(40) = 524.29, p < .001. Smoking categories were regressed onto mental health covariates in Block 2, χ2(6) = 30.33, p < .001. GAD, MDD and BPD predicted a greater likelihood of being in the base category than the “Never” and “Occasional Smoker” category.
In Block 3, researchers entered PTSD into the overall model, χ2(2) = 13.38, p = .001, and it significantly improved the overall prediction of smoking categories. Overall, PTSD was not helpful in differentiating between “Occasional Smoker” and “Daily Smoker”; however, participants who reported a diagnosis of PTSD were 2.1 times more likely to be in the “Daily Smoker” group than in the “Never” group (see Table 3).
Alcohol Binge Drinking (n = 13,615)
Using a hierarchical multinomial logistic regression, the prediction of binge drinking using “More than once a week” as a reference category was explored. Binge drinking categories were regressed onto demographic covariates in Block 1, χ2(100) = 1150.93, p < .001, which significantly improved the prediction of binge drinking. Mental health covariates were entered in Block 2, χ2(100) = 26.98, p = .029, which also significantly improved the overall model. Generally, when participants reported they had BPD, it was associated with a reduced likelihood of being in categories other than the base categories. GAD was generally non-significant, and MDD was only sporadically associated with an increased likelihood of being in the base category. Framed differently, mental health covariates were inconsistently related to binge-drinking categories, although BPD tended to have a more consistent relationship.
Post-traumatic stress disorder was entered in Block 3, χ2(5) = 13.47, p = .019, which significantly improved the overall model. Participants who reported a diagnosis of PTSD were 3.7 times more likely to be in the base category (“Binge drink more than once a week”) than the “Never binge drink” category, 5 times more likely to be in the base category than the “Binge-drink once a month” category and 3.2 times more likely to be in the base category than the “Binge-drink 2–3 times a month” category. These significant findings represented medium-to-large effects sizes. Please note that while there were non-significant comparisons in “Binge drink once a week” and “Binge drink less than once a month”, the directionality of the findings was the same (~ 2 times more likely to be in the base category). Overall, the hypothesis that PTSD would predict membership in the more severe binge-drinking category was supported (see Table 4).
Substance Abuse or Dependence (n = 16,356)
Using hierarchical binary logistic regression, researchers regressed drug abuse onto demographic covariates in Block 1, χ2(20) = 203.45, p < .001, which significantly improved the overall model. Researchers added mental health covariates in Block 2, χ2(3) = 89.18, p < .001; depression, bipolar disorder and anxiety were all associated with scoring more positively for drug abuse or dependence.
Post-traumatic disorder was entered in Block 3, χ2(1) = 6.87, p = .009, and was a significant, positive predictor of drug abuse or dependence that was in the medium-to-large effect size range, OR = 2.98, 95% CI (1.31, 6.78), z = 2.62, p = .009. These results were consistent with the hypothesis that PTSD would be associated with substance abuse (see Table 5).
Discussion
Post-traumatic stress disorder is common among people seeking treatment for SUDs (Jacobsen et al. 2001), and research has increasingly attempted to understand the mechanisms accounting for this comorbidity. However, potential differential associations between PTSD symptoms based on different substances of abuse have been underexplored (Dworkin et al. 2018). Research indicates that co-occurring PTSD and substance abuse or dependence can have more severe negative consequences than either disorder alone, and that the problems that individuals with PTSD experience are exacerbated with the addition of substance abuse or dependence symptoms (Back et al. 2006; Jacobsen et al. 2001). Therefore, the purpose of the present research was to estimate the prevalence and probabilities of smoking, alcohol binge drinking and substance abuse or dependence among adults reporting a PTSD diagnosis within the general Canadian population.
Generally, the results from the current study suggest that reporting a diagnosis of PTSD was associated with higher levels of binge drinking, smoking and substance abuse or dependence than not having PTSD. Results indicated that individuals who reported a diagnosis of PTSD were more likely to smoke on a daily basis, to binge drink on a weekly basis and to meet criteria for substance abuse or dependence than people who did not report a diagnosis of PTSD. These results were significant while including comorbid psychiatric variables for GAD, MDD and BPD. Framed differently, these results suggest that while controlling for the shared variance between PTSD and GAD, MDD and BPD, PTSD substantively and meaningfully contributed to the overall model. The significant effects associated with PTSD were in the medium-to-large effect size range, suggesting that there was practical significance to the current study’s findings.
Although these analyses did not test the role of self-medication within the models, the findings may be consistent with the hypothesis that individuals with PTSD use substances to medicate for the negative symptoms that they experience as a form of coping (Sheerin et al. 2016). In self-medication models of substance abuse, drugs are thought to serve a coping function whereby they facilitate general mood regulation (Khantzian 1997). There is reason to believe that some people use a diverse array of psychoactive drugs, including tobacco (Kassel et al. 2003), alcohol (Cooper et al. 1992), cannabis (Schafer and Brown 1991) and opioids (Calhoun et al. 2000) as a means of coping with stressors and regulating mood. Those with PTSD are known to experience high levels of distress brought on by symptoms of the disorder, which makes it highly plausible that the high levels of substance use observed among this population is a result of self-medication (Sheerin et al. 2016).
Virtually, all smokers attribute their smoking, at least in part, to its anxiolytic properties (Gilbert and Spielberger 1987). Smokers report that they smoke more when they are stressed, angry, anxious or sad, and they hold the expectation that smoking will alleviate these negative moods (Copeland and Brandon 2002). Additionally, much of the research on comorbid PTSD and alcohol dependence suggests that individuals with PTSD are more likely than those without PTSD to endorse using alcohol to cope with negative affect (O'Hare and Sherrer 2011). This is likely because of the depressant properties of alcohol and the effect of decreasing stress and anxiety associated with PTSD. In terms of other drugs that are abused among those with a diagnosis of PTSD, cannabis and opioids are among the most commonly reported.
There is evidence that cannabis may be used by those with PTSD as a short-term emotion regulation strategy to reduce or manage perceived aversive psychological and mood states (Metrik et al. 2011). Cannabis is often abused to decrease distress (Potter et al. 2011), or to cope with symptoms of anxiety among the general population (Bonn-Miller et al. 2008). Among those with PTSD, coping to relieve PTSD-related negative affect has been established as a powerful motivator for cannabis use (Bonn-Miller et al. 2011; Bujarski et al. 2012). Opioids, such as heroin, are also described by PTSD patients as having benefits for coping with negative affect and distress due to their calming effects and ability to relieve stress and ease physical tension (Calhoun et al. 2000).
Although many individuals with PTSD smoke, binge drink alcohol and abuse other drugs in an attempt to cope with their negative symptoms, the development of SUDs can worsen their symptoms by leading to greater psychological distress (Najavits et al. 1999), and worse psychosocial adjustment (Riggs et al. 2003).
Therefore, comorbid PTSD should be considered when an individual does not have an adequate response to the standard treatment for a diagnosed SUD (Benton et al. 2012). Health professionals working with individuals diagnosed with PTSD need to be aware of concomitant substance use issues and should tailor their assessments to screen for substance use among individuals with PTSD.
Current treatments for PTSD primarily include Cognitive Behavioural Therapy and pharmacological interventions. CBT is a time-limited therapy that involves setting specific treatment goals and working towards the remediation of problematic symptoms. CBT treatments have been specifically designed for PTSD symptoms, and have demonstrated particularly strong empirical support and, subsequently, have been designated as evidence-based interventions for PTSD (Bernardy and Friedman 2015). These treatments include, but are not limited to, exposure therapy (Foa and Rothbaum 1998), cognitive processing therapy (Resick et al. 2010) and Imagery Rehearsal Therapy (Moore and Krakow 2010).
In addition to CBT treatments, research in pharmacotherapy for PTSD has indicated that antidepressant and anxiolytic medications have been effective, specifically the selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs; Bernardy and Friedman 2015). The efficacy of SSRIs and other antidepressant medications is due primarily to the overlap of PTSD symptoms with those of depression and many anxiety disorders, and it has been suggested that SSRI or SNRI treatments are especially effective for PTSD symptoms such as irritability, anger, anxiety and depression (Shiromani et al. 2012). Treatment for PTSD symptoms will help reduce the level of substance use, but if substance dependence has developed, it will need to be treated before the patient can benefit from treatments for PTSD (Berenz and Coffey 2012). While the nature of PTSD and SUD comorbidity is largely unknown, it is clear that there are negative implications for comorbid PTSD and SUDs and that the individuals with this comorbidity represent a group with unique treatment needs.
Limitations
There are several limitations to the study. First, PTSD was assessed using self-report, which is in itself a limiting factor. Individuals may not have had the opportunity to be diagnosed by a health professional. Without access to medical files or a diagnostic interview from the respondents, it was not possible to confirm the accuracy of respondents’ self-reports. This lack of verification of PTSD diagnosis may have also affected the association between self-reported PTSD and related SUDs. Second, a significant limitation is that full-time military personnel were not included in the CCHS database. Military personnel have higher rates of PTSD than the general populations due to exposure to traumatic events that take place in combat (Misca and Forgey 2017). Additionally, the database does not include prison populations. Research indicates an interlink between traumatic experiences and criminal behaviour revealing that offenders present a higher prevalence of PTSD and associated symptoms when compared with the general population (Wright et al. 2006). Third, there was no information in the database to indicate symptom severity or the nature of current PTSD symptoms. Fourth, there was no information available in the database to identify whether participants had received any form of treatment for PTSD. Without treatment information, the researchers could not determine whether treatment mitigated the relationship between PTSD and SUD. As the focus of the present study was adults aged 20 to 64, these findings cannot be generalized to teen or senior populations. These age groups should be a focus of future research.
GAD, MDD and BPD were included as covariates in the analyses to control for the co-occurrence of these disorders. However, the literature suggests that these disorders can precede the development of PTSD, and that having a diagnosis of these disorders is predictive of developing PTSD following exposure to a traumatic event (Yehuda et al. 2001). Additionally, anxiety and depression are symptoms of PTSD, and by controlling for GAD, MDD and BPD, the analyses may have also partially controlled for PTSD and attenuated the degree to which PTSD was shown to predict smoking, alcohol binge drinking and substance abuse or dependence. This pattern of findings could be considered evidence for the self-medication model, although it is important to note that causal inferences cannot be made.
Although the aforementioned issues do present some degree of ambiguity when interpreting the results, it is important to note the strength of the study: a nationally representative sample of Canadians. Although researchers excluded groups from analyses, the retained sample still offers a high degree of external validity. Canadians from every province between the age of 20 and 64 were selected in a representative fashion. This level of external validity is unusual and was only possible because the CCHS-MH database was accessible. Future research would benefit from using a more comprehensive measure of PTSD that includes classification of symptoms, rather than relying on a self-reported diagnosis from a medical professional.
Conclusion
Limitations notwithstanding, this study improves our understanding of the relationship between PTSD and SUDs in a nationally representative sample. The results add to the literature suggesting that an individual with a diagnosis of PTSD is at an increased risk for developing a SUD. Furthermore, the findings from this research highlight the importance of screening individuals with PTSD for comorbid SUDs, given the high rate of comorbidity between the two disorders.
Exposure to trauma cannot be prevented; therefore, the prevention of PTSD is virtually impossible. Given that it is not possible to prevent traumatic events from occurring, the next best approach would be to promote resilience and provide behavioural strategies that provide individuals exposed to trauma the tools necessary to cope effectively with severely stressful situations. Therefore, future research should investigate the impact of improving resiliency and teaching behavioural strategies on reducing comorbid PTSD and SUDs symptom development. The comorbidity of substance use disorders is a significant problem among people with PTSD. This study demonstrates that a self-reported diagnosis of PTSD is associated with increased severity of smoking, alcohol binge drinking and drug abuse or dependence in a national Canadian sample. Routine screening and treatment of SUDs should be undertaken among those receiving treatment for PTSD, and conversely, screening and treatment of PTSD may be justified in substance disorder treatment settings. Although these findings do not show cause and effect, they do support the self-medication hypothesis as they demonstrate a link both between the severity of PTSD symptoms and the severity of substance use.
References
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
Back, S., Brady, K., Sonne, S., & Verduin, M. (2006). Symptom improvement in co-occurring PTSD and alcohol dependence. The Journal of Nervous and Mental Disease, 194, 690–696.
Benton, D., Deering, D., & Adamson, S. (2012). Treating co-occurring posttraumatic stress disorder and substance use disorders in an outpatient setting in New Zealand. New Zealand Journal of Psychology, 41, 30–37.
Berenz, E., & Coffey, S. (2012). Treatment of co-occurring posttraumatic stress disorder and substance use disorders. Current Psychiatry Reports, 14, 469–477. https://doi.org/10.1007/s11920-012-0300-0.
Bernardy, N., & Friedman, C. (2015). Psychopharmacological strategies in the management of posttraumatic stress disorder (PTSD): What have we learned? Current Psychiatry Reports, 17, 1–10.
Bonn-Miller, M., Vujanovic, A., & Zvolensky, M. (2008). Emotional dysregulation: AssociationWith coping-oriented marijuana use motives among current marijuana users. Substance Use & Misuse, 43, 1653–1665.
Bonn-Miller, M., Vujanovic, A., Boden, M., & Gross, J. (2011). Posttraumatic Stress, Difficulties in Emotion Regulation, and Coping-Oriented Marijuana Use. Cognitive Behaviour Therapy, 40, 34–44. https://doi.org/10.1080/16506073.2010.525253.
Brady, K. (1997). Posttraumatic stress disorder and comorbidity: Recognizing the many faces of PTSD. Journal of Clinical Psychiatry, 58, 12–15.
Bremner, J., Southwick, S., Darnell, A., & Charney, D. (1996). Chronic PTSD in Vietnam combat veterans: Course of illness and substance abuse. The American Journal of Psychiatry, 153, 369–375.
Brown, P., Stout, R., & Mueller, T. (1996). Posttraumatic stress disorder and substance abuse relapse among women: A pilot study. Psychology of Addictive Behaviours, 10, 124–128.
Bujarski, S., Norberg, M., & Copeland, J. (2012). The association between distress tolerance and cannabis use-related problems: The mediating and moderating roles of coping motives and gender. Addictive Behaviors, 37, 1181–1184.
Calhoun, P. S., Sampson, W. S., Bosworth, H. B., Feldman, M. E., Kirby, A. C., Hertzberg, M. A., Wampler, T. P., Tate-Williams, F., Moore, S. D., & Beckham, J. C. (2000). Drug use and validity of substance use self-reports in veterans seeking help for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 68, 923–927. https://doi.org/10.1037/0022-006X.68.5.923.
Cerimele, J., Bauer, A., Fortney, J., & Bauer, M. (2017). Patients with co-occurring bipolar disorder and posttraumatic stress disorder: A rapid review of the literature. The Journal of Clinical Psychiatry, 78, 506–514.
Cooper, M., Russell, M., Skinner, J., & Windle, M. (1992). Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment, 4, 123–132.
Copeland, A., & Brandon, T. (2002). Do desirability ratings moderate the validity of probability ratings on the smoking consequences questionnaire - adult? A reanalysis using regression. Psychological Assessment, 14, 353–359.
Dworkin, E., Wanklyn, S., Stasiewicz, P., & Coffey, S. (2018). PTSD symptom presentation among people with alcohol and drug use disorders: Comparisons by substance of abuse. Addictive Behaviors, 76, 188–194.
Fischer, B., Dawe, M., Mcguire, F., Shuper, P., Jones, W., Rudzinski, K., & Rehm, J. (2012). Characteristics and predictors of health problems from use among high frequency cannabis users in a Canadian university student population. Drugs: Education, Prevention, and Policy, 19, 49–58. https://doi.org/10.3109/09687637.2011.614970.
Foa, E., & Rothbaum, B. (1998). Treating the trauma of rape: Cognitive behavioral therapy for PTSD. New York: Guilford Press.
Galatzer-Levy, I., Nickerson, A., Litz, B., & Marmar, C. (2013). Kessler patterns of lifetime PTSD comorbidity: A latent class analysis. Depression and Anxiety, 30, 489–496.
Gilbert, D., & Spielberger, G. (1987). Effects of smoking on heart rate, anxiety, and feelings of success during social interaction. Journal of Behavioral Medicine, 10, 629–638.
Hernandez, J., Cordova, M., Ruzek, J., Reiser, R., Gwizdowski, I., Suppes, T., & Ostacher, M. (2013). Presentation and prevalence of PTSD in a bipolar disorder population: A STEP- BD examination. Journal of Affective Disorders, 150, 450–455.
Jacobsen, L., Southwick, S., & Kosten, T. (2001). Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal Of Psychiatry, 158, 1184–1190. https://doi.org/10.1176/appi.ajp.158.8.
Kassel, J., Stroud, L., & Paronis, C. (2003). Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin, 129, 270–304.
Kaysen, D., Schumm, J., Pedersen, E., Seim, R., Bedard-Gilligan, M., & Chard, K. (2014). Cognitive processing therapy for veterans with comorbid PTSD and alcohol use disorders. Addictive Behaviors, 39, 420–427.
Kessler, R. (2000). Posttraumatic stress disorder: The burden to the individual and to society. The Journal of Clinical Psychiatry, 61, 4–12.
Kessler, R., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060.
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4, 231–244. https://doi.org/10.3109/10673229709030550.
Kline, A., Weiner, M., Ciccone, D., Interian, A., Hill, L., & Losonczy, M. (2014). Increased risk of alcohol dependency in a cohort of National Guard troops with PTSD: A longitudinal study. Journal of Psychiatric Research, 50, 18–25.
Metrik, J., Kahler, C., Mcgeary, J., Monti, P., & Rohsenow, D. (2011). Acute effects of marijuana smoking on negative and positive affect. Journal of Cognitive Psychotherapy, 25, 31–46.
Miller, M., Vogt, D., Mozley, S., Kaloupek, D., & Keane, T. (2006). PTSD and substance-related problems: The mediating roles of disconstraint and negative emotionality. Journal of Abnormal Psychology, 115, 369–379.
Mills, K. (2013). Treatment of comorbid substance dependence and posttraumatic stress disorder. Journal of the American Medical Association, 310, 482–483.
Mills, K., Teesson, M., Ross, J., & Peters, L. (2006). Trauma, PTSD, and substance use disorders: Findings from the Australian National Survey of Mental Health and Well-Being. The American Journal of Psychiatry, 163, 652–658.
Misca, G., & Forgey, M. A. (2017). The role of PTSD in bi-directional intimate partner violence in military and veteran populations: A research review. Frontiers in Psychology, 8, 1394. https://doi.org/10.3389/fpsyg.2017.01394.
Moore, B. A., & Krakow, B. (2010). Imagery rehearsal therapy: An emerging treatment for posttraumatic nightmares in veterans. Psychological Trauma: Theory, Research, Practice, and Policy, 2, 232–238. https://doi.org/10.1037/a0019895.
Najavits, L., Weiss, R., & Shaw, S. (1999). A clinical profile of women with posttraumatic stress disorder and substance dependence. Psychology of Addictive Behaviors, 13, 98–104.
Ogeil, R. P., Rajaratnam, S. W., Phillips, J. G., Redman, J. R., & Broadbear, J. H. (2011). Ecstasy use and self-reported disturbances in sleep. Human Psychopharmacology: Clinical & Experimental, 26, 508–516. https://doi.org/10.1002/hup.1233.
O'Hare, T., & Sherrer, M. (2011). Drinking motives as mediators between PTSD symptom severity and alcohol consumption in persons with severe mental illnesses. Addictive Behavior, 36, 465–469.
Ouimette, P., Moos, R., & Finney, J. (2003). PTSD treatment and 5-year remission among patients with substance use and posttraumatic stress disorders. Journal of Consulting and Clinical Psychology, 71, 410–414.
Potter, C., Vujanovic, A., Marshall-Berenz, E., Bernstein, A., & Bonn-Miller, M. (2011). Posttraumatic stress and marijuana use coping motives: The mediating role of distress tolerance. Journal of Anxiety Disorders, 25, 437–443.
Price, M., & van Stolk-Cooke, K. (2015). Examination of the interrelations between the factors of PTSD, major depression, and generalized anxiety disorder in a heterogeneous trauma-exposed sample using DSM 5 criteria. Journal of Affective Disorders, 186, 149–155. https://doi.org/10.1016/j.jad.2015.06.012.
Read, J., Wardell, J., & Colder, C. (2013). Reciprocal associations between PTSD symptoms and alcohol involvement in college: A three-year trait-state-error analysis. Journal of Abnormal Psychology, 122, 984–997.
Resick, P. A., Monson, P. A., & Chard, K. M. (2010). Cognitive processing therapy: Veteran/military version. Washington, DC: Department of Veterans Affairs.
Riggs, D., Rukstalis, M., Volpicelli, J., Kalmanson, D., & Foa, E. (2003). Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: Potential pitfalls to PTSD treatment. Addictive Behaviors, 28, 1717–1730.
Saunders, E., Lambert-Harris, C., McGovern, M., Meier, A., & Xie, H. (2015). The prevalence of posttraumatic stress disorder symptoms among addiction treatment patients with cocaine use disorders. Journal of Psychoactive Drugs, 47, 42–50.
Schafer, J., & Brown, S. (1991). Marijuana and cocaine effect expectancies and drug use patterns. Journal of Consulting and Clinical Psychology, 59, 558–565.
Sharkansky, E. J., Brief, D. J., Peirce, J. M., Meehan, J. C., & Mannix, L. M. (1999). Substance abuse patients with posttraumatic stress disorder (PTSD): Identifying specific triggers of substance use and their associations with PTSD symptoms. Psychology of Addictive Behaviors, 13, 89–97 http://dx.doi.org.qe2a-proxy.mun.ca/10.1037//0893-164X.13.2.89.
Sheerin, C., Berenz, E. C., Knudsen, G. P., Reichborn-Kjennerud, T., Kendler, K. S., Aggen, S. H., & Amstadter, A. B. (2016). A population-based study of help seeking and self- medication among trauma-exposed individuals. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 30, 771–777.
Shiromani, P., Keane, T. M., & LeDoux, J. E. (Eds.). (2012). Posttraumatic stress disorder: Basic science and clinical practice. New York: Humana Press.
Sripada, R., Pfeiffer, P., Valenstein, M., & Bohnert, K. (2014). Medical illness burden is associated with greater PTSD service utilization in a nationally representative survey. General Hospital Psychiatry, 36, 589–593.
Statistics Canada. (2013). Canadian community health survey (CCHS)-mental health user guide. Ottawa: Author.
Symmes, A., Winters, K. C., Fahnhorst, T., Botzet, A. M., Lee, S., August, G. J., & Realmuto, G. M. (2015). The association between attention deficit hyperactivity disorder and nicotine use among adolescents and young adults. Journal of Child & Adolescent Substance Abuse, 24, 37–45. https://doi.org/10.1080/1067828X.2012.756442.
Trivedi, R., Post, E., Sun, H., Pomerantz, A., Saxon, A., Piette, J., et al. (2015). Prevalence, comorbidity, and prognosis of mental health among US veterans. American Journal of Public Health, 105, 2564–2569.
Van Ameringen, M., Mancini, C., Patterson, B., & Boyle, M. (2008). Post-traumatic stress disorder in Canada. CNS Neuroscience & Therapeutics, 14, 171–181.
Wild, J., Smith, K. V., Thompson, E., Béar, F., Lommen, M. J., & Ehlers, A. (2016). A prospective study of pre-trauma risk factors for post-traumatic stress disorder and depression. Psychological Medicine, 46, 2571–2582.
World Health Organization. (1992). International classification of diseases and related health problems (10th rev.). Geneva: Author.
Wright, E., Borrill, J., Teers, R., & Cassidy, T. (2006). The mental health consequences of dealing with self-inflicted death in custody. Counselling Psychology Quarterly, 19, 165–180.
Yehuda, R., Halligan, S., & Bierer, L. (2001). Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of Psychiatric Research, 35, 261–270.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Connolly, R.D., Speed, D. & Hesson, J. Probabilities of PTSD and Related Substance Use Among Canadian Adults. Int J Ment Health Addiction 19, 2178–2193 (2021). https://doi.org/10.1007/s11469-020-00311-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-020-00311-2