Abstract
Although it has been clearly shown that Pueraria mirifica and its phytoestrogens can mimic estrogen in preventing bone loss, as osteoporosis is an asymptomatic disease, the therapeutic effects of P. mirifica should be acknowledged. In this study, 6-month-old female rats were ovariectomized, kept for 4 weeks to induce bone loss, divided into five groups, and treated with P. mirifica at doses of 0, 5, 25, and 50 mg/kg BW/day (PM0, PM5, PM25, and PM50 groups, respectively) or 7 mg/kg BW/day of puerarin (PU group) for 12 weeks. Only the trabecular bone mineral densities (BMDs) of tibia metaphysis (at the 12th, 14th, and 16th week) and total and trabecular BMDs of L4 (at the 16th week) of the PM50 group were significantly higher than those of the PM0 group. However, the BMDs of tibia metaphysis and L4 at the 16th week of the study period were kept significantly lower than those of the 0 week, and the BMD was also significantly lower than that of the 4th week for tibia metaphysis. The trabecular bone area (BV/TV), trabecular number (Tb.N), and osteoblast surface (Ob.S/BS) were significantly higher, and trabecular space (Tb.Sp) was significantly lower in the PM50 group, as compared with those of the PM0 group. This study indicates that P. mirifica could be used as an anti-osteoporotic agent for postmenopausal women. Since P. mirifica could mainly retain bone mass at the levels before bone loss is initiated, the use of other anabolic agents in combination with P. mirifica is recommended for osteoporotic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a common disorder of aging, which is characterized by low bone mass and micro-architectural deterioration of bone tissue [1]. The cause of the disease is multifactorial with the dominant factor often sex hormone deficiency, particularly estrogen deficiency in postmenopausal women [1, 2]. Several studies have demonstrated the beneficial effect of estrogen replacement therapy in preventing and curing bone loss following menopause [3–6]. However, use of estrogens has several downsides that may lead to serious side effects such as breast or endometrial cancer [7].
Thus, other antiresorptive and anabolic agents have been widely prescribed. Oral bisphosphonates are currently the most potent antiresorptive agents for prevention or treatment of osteoporosis. They can reduce vertebral and hip fractures by 50–60 % in postmenopausal women. However, bisphosphonates have adverse side effects on the gastrointestinal tract such as induction of esophageal ulceration, acid reflux, vomiting, and heart burn, which is why physicians hesitate to use these in some women [8]. Another weak point for antiresorptive agents is that they are unable to build a new bone or lead to bone formation; thus, it might not be justified to use them with osteoporotic patients. The evidence for the use of recombinant human parathyroid hormone (hPTH) analogue PTH(1–34), an anabolic agent that will increase bone mass and bone strength while reducing bone loss [9], is still equivocal for application in humans. Since PTH is a protein hormone, oral administration of hPTH is susceptible to protease digestion, while absorption through the intestinal layers is low [10]. Both bisphosphonates and hPTH are also expensive for low-income patients. Therefore, natural products that show few side effects and are substantially safe and cheap become a focal point of interest.
Pueraria candollei var. mirifica (Airy Shaw et. Suvatabandhu) Niyomdham (1992) (syn. P. mirifica) is an endemic Thai plant whose tuberous roots contain at least 17 phytoestrogenic substances [11, 12]. The plant’s estrogenic potency has been widely tested on reproductive organs [13, 14] and bones [15–18]. For bones, P. mirifica powder could prevent bone loss in orchidectomized [15] and ovariectomized [16] rats. It ameliorated the lowered bone mineral content (BMC) and density (BMD) caused by sex steroid hormone deficiency [15, 16], functioning through both osteoblast and osteoclast cells [17]. Additionally, the vast majority of reports have focused on puerarin, a major phytoestrogen constituent in Pueraria plants, especially in P. mirifica, and its effects on bone. Puerarin can decrease bone loss and increase bone mass in primary bone cells [18–20], cell lines [17, 21], and rats [22, 23]. In light of the literature mentioned above, P. mirifica should be a strong potential candidate for development as an anti-osteoporotic agent for human use. Besides P. mirifica also elicits cytotoxicity toward mammary cancer, both in the MCF-7 cell line [24] and a laboratory rat model [25].
Since osteoporosis is an asymptomatic disease occurring gradually with no pain, most patients do not realize that they are suffering from it until after bone fracture. As the preventive strategy might not be reasonable for most osteoporotic patients, this study aims to determine if P. candollei var. mirifica and puerarin can exert anti-osteoporotic effects in ovariectomy-induced osteoporotic rats. As P. mirifica elicited estrogenic potency on both reproductive organs and bone [13–18], P. mirifica at dose ranges effective on bone but not on reproductive organs were selected for this study.
Materials and methods
Animals
Two-month-old female Sprague–Dawley rats, weighing 210–220 g, were obtained from the National Laboratory Animal Center, Mahidol University, Nakhon Pathom, Thailand. They were housed (three rats/cage) in a room with controlled lighting (lights on 0600–1800 hours) and temperature (25 ± 1 °C) at the Laboratory Animal Unit, Faculty of Science, Chulalongkorn University, Thailand. The rats were fed with standard rat diet containing 4000 IU/kg of vitamin D, 0.94% wt/wt of calcium and 0.83% wt/wt of phosphorus (Perfect Companion Group Co., Ltd., Samutprakarn, Thailand) and supplied water ad libitum until they became 6 months old when peak bone mass was achieved [16]. The experimental protocol was approved by the Animal Ethical Committee in accordance with the guide for the care and use of laboratory animals prepared by Chulalongkorn University (Protocol Review No. 1223007).
Experimental design
The BMDs of the rats were measured at tibia and 4th lumbar vertebra (L4) on the first day (0 week) of the experiment. Rats were randomly assigned to one of five groups (6–8 rats per group) so that their BMD values between groups were non-significantly different. After that, they were bilaterally ovariectomized under sodium pentobarbital anesthesia (40 mg/kg BW, i.p.). The BMDs of the tibia and L4 were followed up every 2 weeks after ovariectomy until the end of the experiment. When the rats showed a significantly lowered BMD value, namely osteoporotic rats in this study, the treatments were started. Five groups of rats were gavaged daily with P. mirifica at dosages of 0, 5, 25, and 50 mg/kg BW/mL/day (PM0, PM5, PM25, and PM50 groups, respectively) or subcutaneously injected with 7 mg/kg BW/0.2 mL/day of puerarin (PU group) at 1600-1800 hours for 12 weeks. P. mirifica and puerarin at these dose ranges were selected because they did not stimulate reproductive organs in female mice [26], rats [14, 27, 28], or monkeys [13, 29].
At the end of the 16-week experiment, the rats were weighed to determine their body mass. Then, they were euthanized and the uterus and vagina were dissected and weighed. The tibiae were collected and processed for histomorphometry of the trabecular microstructures [30].
Preparation of P. mirifica suspension and puerarin solution
P. mirifica powder (Lot no. 121408) was provided by Smith Natural Co., Ltd. and used throughout this study. Dry powder (<100 µm in size) of P. mirifica was mixed with distilled water and administered to the rats via gavage. P. mirifica suspension was freshly prepared every 2 weeks and kept at 4 °C in a dark bottle. The major phytoestrogens, including genistin, genistein, puerarin, daidzin, daidzein, miroestrol, and deoxymiroestrol, were analyzed by liquid chromatography–mass spectrometry (LC/MS). One kilogram of the powder was extracted with 95 % ethanol using the Bio-Chelated® cold extraction process, and glycerin was added into the extract to prevent oxidation of miroestrol before LC/MS analysis [31]. Briefly, 5 μL of 1 mg/mL of P. mirifica extract was injected into a Micromass Waters UPLC-TQD system. A Waters C18 UPLC column (2 × 50 mm) with 1.7-μm particles was used. The flow rate was set to 0.25 mL/min. Seven phytoestrogen components in the sample were identified and quantified by comparison of their retention time and peak areas with reference to known standards and concentrations, respectively, resolved under the same conditions. The concentrations of miroestrol, deoxymiroestrol, puerarin, daidzin, genistin, daidzein, and genistein were 0.25, 0.008, 23.7, 2.9, 0.9, 1.3, and 0.5 mg/100 g of the P. mirifica extract, respectively.
Puerarin dry powder (99 % purity; R&D system, MN, USA) was diluted with small amounts of absolute ethanol, mixed with olive oil (Fluka, MO, USA), and the concentration was adjusted to 7 mg/0.2 mL. The ethanol was evaporated overnight, and the solution was kept at room temperature in a dark bottle.
BMD measurement
BMDs were measured by peripheral quantitative computed tomography (pQCT) in the research M mode (XCT Research SA+, Stratec Medizintechnik GmbH, Germany) and analyzed by XCT-6.20 software (Stratec Medizintechnik GmbH, Germany) according to the method of Urasopon et al. [15, 16].
Bone histomorphometry
Since only a significant difference of the BMDs compared to the PM0 group could be detected in the PM50 group, the bones of PM0 and PM50 were selected for bone histomorphometry analysis. Tibiae were cleaned of adhering muscles and connective tissue, cut at the mid-diaphysial position, and cleaned up to the bone marrow. The proximal tibia was dehydrated, embedded in methyl methacrylate resin, cut longitudinally at a thickness of 7 µm, mounted onto a slide, and stained with Goldner’s trichrome reagent according to the method of Seriwatanachai et al. [30]. Slices subjected to bone histomorphometry were assessed under a light/fluorescent microscope (model BX51TRF; Olympus, Tokyo, Japan) using the computer-assisted Osteomeasure system (Osteomeric, Atlanta, GA). The region of interest was at 1–2 mm distal to the epiphyseal plate in the trabecular region of the proximal tibia metaphysis (secondary spongiosa). One slide was randomly selected from each animal, and the data from 5–6 animals in each group were pooled for statistical analysis. Statistical parameters consisting of trabecular bone volume normalized by tissue volume (BV/TV, %), trabecular thickness (Tb.Th, µm), trabecular separation (Tb.Sp, µm), trabecular number (Tb.N, mm−1), osteoblast surface normalized by bone surface (Ob.S/BS, %), and osteoclast surface (Oc.S/BS, %) were measured.
Statistical analysis
Results are reported as mean ± SE. The significant differences of BMD at each time point in the same individual and between groups and body mass, uterus and vagina weights between groups were examined by one-way ANOVA followed by a multiple comparison test with Turkey post hoc test. The significant differences of bone histomorphometry between PM0 and PM50 groups were examined by T test. The level of significant differences was accepted at p < 0.05. Statistical Packages for Social Science version SPSS/PC 16.0 (IL, USA) was used.
Results
Body, uterus, and vagina weights
Body, uterus, and vagina weights in all groups of P. mirifica (PM5, PM25, and PM50 group) and puerarin (PU group) treated rats were not significantly different when compared with the PM0 group (Table 1). Although the uterus and vagina weights of the PM50 group were marginally higher than in the PM0 group, the differences did not reach statistical significance (p = 0.149 for uterus weight and p = 0.197 for vagina weight). This indicates that the estrogenic activity of P. mirifica and puerarin at all selected dose ranges and treatment for 12 weeks was not be able to stimulate the aforementioned reproductive organs.
Ovariectomy-induced bone loss
To find out when the ovariectomy-induced estrogen deficiency could induce significant bone loss, the BMDs in the PM0 group were followed up every 2 weeks. There was no significant decrease in total BMDs of tibia diaphysis throughout the 16-week experiment, whereas it was significantly lowered at the 2nd week for tibia metaphysis and at the 6th week for L4 compared with the 0 week (Fig. 1a–c). Since the tibia metaphysis and L4 consisted of both cortical and trabecular bone, each bone compartment was separately analyzed. Similarly to that of tibia diaphysis, which contains mainly the cortical bone, cortical BMDs of tibia metaphysis and L4 were not significantly different throughout the 16-week experiment (Fig. 1d, e). However, the trabecular BMDs were evident and continuously decreased throughout the 16-week study period (Fig. 1f, g). Thus, P. mirifica and puerarin treatments were initiated at the 4th week of the study period, and only the total and trabecular BMDs were analyzed afterward.
P. mirifica and puerarin treatments and anti-osteoporotic effects
After treatments of 5, 25, and 50 mg/kg BW/day of P. mirifica and 7 mg/kg BW/day of puerarin for 12 weeks, the total and trabecular BMDs of tibia metaphysis and L4 were gradually and continuously decreased in the same pattern as those of the PM0 group (Fig. 2). Only the trabecular BMDs of tibia metaphysis (at the 12th, 14th, and 16th week or after 8, 10, and 12 weeks of treatment) and L4 (at the 16th week or after 12 weeks of treatment), and total BMDs of L4 (at the 16th week) were significantly higher than those of the PM0 group (p < 0.05). After that the BMDs of the PM50 group were compared between the 16th week (the end of the study period) and those of the 4th week (the treatment onset) and 0 week (the initiation of the ovariectomy). The BMD values of tibia metaphysis and L4 of the PM50 group at the 16th week of the study period were kept significantly lower than those of the 0 week (p < 0.01 for tibia metaphysis and p < 0.05 for L4, respectively), and it was also significantly lower than that of the 4th week for tibia metaphysis (p < 0.05).
Total BMDs and trabecular BMDs of tibia metaphysis (a, b) and L4 (c, d) of the ovariectomized rats treated with 0, 5, 25, 50 mg/kg BW/day of Pueraria mirifica (PM0, PM5, PM25, and PM50, respectively) and 7 mg/kg BW/day of puerarin (PU). The gray area indicates the duration of 12-week treatment (at the 4th–16th week). *p < 0.05 compared to the PM0 group. †p < 0.05 and ††p < 0.001 compared to the 0 week. # p < 0.05 compared to the 4th week
To clearly depict the significant differences among five groups of treatments, only the total and trabecular BMDs of tibia metaphysis and L4 at the 16th week of the experiment were taken and redrawn in the graph. PM50 ameliorated the decreased total and trabecular BMDs of L4 as well as trabecular BMD of the tibia, whereas PM5 could abate only the decreased trabecular BMD of the tibia compared with those of the PM0 group (Fig. 3).
Total BMDs and trabecular BMDs of tibia metaphysis (a, b) and L4 (c, d) at 16th week of the study period in ovariectomized rats treated with 0, 5, 25, 50 mg/kg BW/day of Pueraria mirifica (PM0, PM5, PM25, and PM50, respectively) and 7 mg/kg BW/day of puerarin (PU). *p < 0.05 and **p < 0.001 compared to the PM0 group. The number s in parentheses indicate the number of rats used in each group
Bone histomorphometry
Histological sections depicted that the epiphyseal plate and metaphyseal region were filled with trabecular bones and intertrabecular spaces (Fig. 4). Sixteen weeks after ovariectomy, PM0 rats had sparse and thinner trabeculae, which led to greater intertrabecular spaces (Fig. 4a). In agreement with the higher total and trabecular BMDs of tibia metaphysis, the trabeculae of the proximal tibia metaphysis were thicker, and the intertrabecular spaces were narrower in the PM50 rats (Fig. 4b).
Representative micrographs of proximal tibia metaphysis at the 16th week of the study period in the ovariectomized rats treated with 0 (a) and 50 (b) mg/kg BW/day of Pueraria mirifica. Tissue sections were processed using Goldner’s trichrome staining. EP epiphyseal plate. The metaphyseal trabecular (arrow) in the treated PM50 rat was markedly thicker and less spaced than for the PM0 treated rat. Scale bars 500 µm
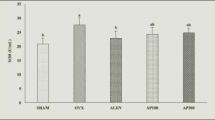
The trabecular bone area (BV/TV, %), trabecular number (Tb.N, mm−1), and osteoblast surface (Ob.S/BS, %) were significantly higher (p < 0.05), and trabecular space (Tb.Sp, µm) was significantly lower (p < 0.05) in the PM50 group, as compared with those of the PM0 group. Trabecular bone thickness and osteoclast surface did not differ significantly between the two groups (Fig. 5).
Bone volume (BV/TV), trabecular thickness (Tb.Th), trabecular separation (Tb.Sp), trabecular number (Tb.N), osteoblast surface normalized by bone surface (Ob.S/BS), and osteoclast surface (Oc.S/BS) at the 16th week of the study period in the ovariectomized rats treated with 0 and 50 mg/kg BW/day of Pueraria mirifica (PM0, and PM50, respectively). * p < 0.05 compared to PM0 group. The numbers in parentheses indicate the number of rats used in each group
Discussion
Compared to previous reports on uterus weight of sham control rats (0.459 ± 0.030 g [32]), this study confirms that ovariectomy could induce an estrogen-deficient stage in the PM0 rats (0.153 ± 0.011 g for uterus weight). Ovariectomy-induced estrogen-deficient rats are a good model for osteoporotic research and can be used as representative of postmenopausal women [33]. The significant bone loss could be seen as early as 2–6 weeks after ovariectomy as regards the total and trabecular BMDs. As reported previously, P. mirifica contained at least 17 phytoestrogens, and their estrogenic activities were tested mainly on the reproductive organs [13, 14, 29, 34, 35]; however, 5–50 mg/kg BW/day of P. mirifica used in this study did not affect the uterus and vaginal weight after 12 weeks of treatment in comparison with those of the PM0 rats. Still, the P. mirifica at doses of 25 and 50 mg/kg BW/day used in this study fell into the dose ranges of 10–100 mg/kg BW/day, which could prevent bone loss in ovariectomized and orchidectomized rats [15, 16]. In line with this rat study, Udomsuk et al. [36] subcutaneously injected ovariectomized mice with 2.5 and 25 mg/kg BW/day for 60 days and found that P. mirifica downregulated the expression of receptor activator of nuclear factor kappa B ligand (RANKL; an osteoclast differentiation stimulating factor) mRNA levels and elevated the expression of osteoprotegerin (OPG; a decoy protein for RANKL) mRNAs.
In a previous study of the preventive effects of P. mirifica in ovariectomized rats [15, 16], the trabecular BMDs of tibia and L4 in 10 mg/kg BW/day of P. mirifica treated rats, although significantly higher than the ovariectomized (PM0) control rats, were kept lower than the sham control rats. However, the trabecular BMDs of tibia and L4 in the 100 mg/kg BW/day of P. mirifica treated rats were comparable with those of the sham control rats. Similarly to the preventive effects, only the trabecular tibia and total and trabecular L4 BMDs of the PM50 rats were significantly higher than those of the PM0 rats at the 16th week. Comparing the BMD values between the 16th week with the 4th week (the initiation of P. mirifica treatment) and 0 week (the initiation of estrogen deficient state) in the PM50 group, the BMD levels were still significantly lower than those of the 4th week (for trabecular tibia metaphysis BMD; p < 0.05) and 0 week [for trabecular tibia metaphysis (p < 0.01) and trabecular L4 BMDs (p < 0.05)]. This indicates that PM50 could retain, but not increase, bone mass at the point of the initiation of estrogen deficiency. There are two possible hypotheses to explain this phenomenon. One indicates that P. mirifica can slow bone loss but cannot stimulate bone formation. This might imply that P. mirifica does not show any anabolic effect on bone. Another is that P. mirifica could enhance both bone formation and resorption. This was suggested by histomorphometry analysis (Fig. 5) in which the osteoblast and osteoclast surfaces in the PM50 group were higher (significantly different for the osteoblast surface and marginally higher, but not significant, for the osteoclast surface) than the PM0 group. It is noted that both osteoblast and osteoclast surfaces were increased in estrogen-deficient rats [30]. Therefore, in the present study, PM50 increased osteoblast surface and had a tendency to increase osteoclast surface over the pre-existing elevated baseline, leading to increased bone volume and trabecular number as well as decreased trabecular separation. It was previously reported that P. mirifica stimulated osteoblast and suppressed osteoclast function in cell cultures [17, 18]. Indeed, osteoblast and osteoclast expressed estrogen receptors [17, 18, 37] and can respond to either estrogen or phytoestrogens. Thus, the latter hypothesis has higher possibility. However, the underlying mechanism of actions of P. mirifica on osteoblast and osteoclast cells needs to be investigated further.
Although many studies of the effects of P. mirifica on bone loss were found, they have focused mainly on cell lines [17, 18]. The research in laboratory animals (mice and rats) and humans conducted have been done solely on the preventive effects of the plant on bone loss. As osteoporosis is an asymptomatic disease, the therapeutic effects of P. mirifica should be acknowledged. This study confirms that P. mirifica (only high dose of 50 mg/kgBW/day) could ameliorate bone loss in ovariectomy-induced osteoporotic rats, especially at the trabecular bone of both axial (L4) and appendicular (tibia) bone. Bone histology and histomorphometry corroborated the measured BMD values. Interestingly, this study did not find any differences of BMDs and bone histomorphometry of the PU treated rats when compared to the control (PM0) group. It might be that in this study the dose of puerarin is too low to exert an effect on bone, or the route of administration is not suitable for this study. In fact, it was reported that puerarin at doses of 40 and 60 mg/kg BW/day intraperitoneally injected into ovariectomized mice for 12 weeks could ablate bone loss [38]. Puerarin at a dose of 5 mg/kg BW/day fed to ovariectomized mice for 2 months restored the structure of the femur and decreased the level of serum tartrate-resistant acid phosphatasee (TRAP), a bone resorption marker [39].
This study indicates that P. mirifica could be used as an anti-osteoporotic agent for postmenopausal women, but the administration should be initiated as early as possible such as at the premenopausal period. In addition, the low doses of P. mirifica, which are safe and do not demonstrate any estrogen-like effect on reproductive organs, can demonstrate the effects on bone. This was confirmed by a previous study in postmenopausal women demonstrating that P. mirifica at dosages of 20, 30, and 50 mg/day for a 24-week period had no effects on endometrial proliferation, breast tissue, hematology, and hepatic and renal organs, but it showed antiresorptive activity on bone [40]. Because P. mirifica could mainly retain bone mass at levels before bone loss is initiated, the use of this natural product for osteoporotic patients would be more effective if it is used in combination with other anabolic agents.
References
Klein-Nulend J, van Oers RF, Bakker AD, Bacabac RG (2014) Bone cell mechanosensitivity, estrogen deficiency, and osteoporosis. J Biomech 48:855–865
Khosla S, Oursler MJ, Monroe DG (2012) Estrogen and the skeleton. Trends Endocrinol Metab 23:576–581
Ettinger B, Genant HK, Cann CE (1985) Long-term estrogen replacement therapy prevents bone loss and fractures. Ann Intern Med 3:319–324
Kanis JA (1995) Treatment of osteoporosis in elderly women. Am J Med 98:60S–66S
Gallagher JC, Fowler SE, Detter JR, Sherman SS (2001) Combination treatment with estrogen and calcitriol in the prevention of age-related bone loss. J Clin Endocrinol Metab 86:3618–3628
Villareal DT, Binder EF, Williams DB, Schechtman KB, Yarasheski KE, Kohrt WM (2001) Bone mineral density response to estrogen replacement in frail elderly women: a randomized controlled trial. JAMA 286:815–820
Adami H, Persson I, Hoover R, Schaier C, Bergkvist L (1989) Risk of cancer in women receiving hormone replacement therapy. Int J Cardiol 44:833–839
Kennel KA, Drake MT (2009) Adverse effects of bisphosphonates: implications for osteoporosis management. Mayo Clin Proc 84:632–638
Babu S, Sandiford NA, Vrahas M (2015) Use of teriparatide to improve fracture healing: what is the evidence? World J Orthop 6:457–461
Sturmer A, Mehta N, Giacchi J, Cagatay T, Tavakkol R, Mitta S, Fitzpatrick L, Wald J, Trang J, Stern W (2013) Pharmacokinetics of oral recombinant human parathyroid hormone [rhPTH(1-31)NH2] in postmenopausal women with osteoporosis. Clin Pharmacokinet 52:995–1004
van der Maesen LJG (2002) Pueraria: botanical characteristics. In: Keung WM (ed) Pueraria: the genus pueraria. Taylor and Francis, London
Cherdshewasart W, Sriwatcharakul S (2007) Major isoflavonoid contents of the 1-year-cultivated phytoestrogen-rich herb, Pueraria mirifica. Biosci Biotechnol Biochem 71:2527–2533
Trisomboon H, Malaivijitnond S, Watanabe G, Taya K (2004) Estrogenic effects of Pueraria mirifica on the menstrual cycle and hormone-related ovarian functions in cyclic female cynomolgus monkeys. J Pharmacol Sci 94:51–59
Cherdshewasart W, Kitsamai Y, Malaivijitnond S (2007) Evaluation of the estrogenic activity of the wild Pueraria mirifica by vaginal cornification assay. J Reprod Dev 53:385–393
Urasopon N, Hamada Y, Asaoka K, Cherdshewasart W, Malaivijitnond S (2007) Pueraria mirifica, a phytoestrogen-rich herb, prevents bone loss in orchidectomized rats. Maturitas 56:322–331
Urasopon N, Hamada Y, Cherdshewasart W, Malaivijitnond S (2008) Preventive effects of Pueraria mirifica on bone loss in ovariectomized rats. Maturitas 59:137–148
Tiyasatkulkovit W, Charoenphandhu N, Wongdee K, Thongbunchoo J, Krishnamra N, Malaivijitnond S (2012) Upregulation of osteoblastic differentiation marker mRNA expression in osteoblast-like UMR106 cells by puerarin and phytoestrogens from Pueraria mirifica. Phytomedicine 19:1147–1155
Tiyasatkulkovit W, Malaivijitnond S, Charoenphandhu N, Havill LM, Ford AL, VandeBerg JL (2014) Pueraria mirifica extract and puerarin enhance proliferation and expression of alkaline phosphatase and type I collagen in primary baboon osteoblasts. Phytomedicine 21:1498–1503
Sheu SY, Tsai CC, Sun JS, Chen MH, Liu MH, Sun MG (2012) Stimulatory effect of puerarin on bone formation through co-activation of nitric oxide and bonemorphogenetic protein-2/mitogen-activated protein kinases pathways in mice. Chin Med J (Engl) 125:3646–3653
Wang C, Meng MX, Tang XL, Chen KM, Zhang L, Liu WN, Zhao YY (2014) The proliferation, differentiation, and mineralization effects of puerarin on osteoblasts in vitro. Chin J Nat Med 12:436–442
Wang Y, Yang C, Xie WL, Zhao YW, Li ZM, Sun WJ, Li LZ (2014) Puerarin concurrently stimulates osteoprotegerin and inhibits receptor activator of NF-κB ligand (RANKL) and interleukin-6 production in human osteoblastic MG-63 cells. Phytomedicine 21:1032–1036
Zhang MY, Qiang H, Yang HQ, Dang XQ, Wang KZ (2012) In vitro and in vivo effects of puerarin on promotion of osteoblast bone formation. Chin J Integr Med 18:276–282
Li B, Liu H, Jia S (2014) Puerarin enhances bone mass by promoting osteoblastogenesis and slightly lowering bone marrow adiposity in ovariectomized rats. Biol Pharm Bull 37:1919–1925
Cherdshewasart W, Cheewasopit W, Picha P (2004) The differential anti-proliferation effect of white (Pueraria mirifica), red (Butea superba), and black (Mucuna collettii) Kwao Krua plants on the growth of MCF-7 cells. J Ethnopharmacol 93:255–260
Cherdshewasart W, Panriansaen R, Picha P (2007) Pretreatment with phytoestrogen-rich plant decreases breast tumor incidence and exhibits lower profile of mammary ERα and ERβ. Matuaritus 58:174–181
Jaroenporn S, Malaivijitnond S, Wattanasirmkit K, Trisomboon H, Watanabe G, Taya K, Cherdshewasart W (2007) Assessment of fertility and reproductive toxicity in adult female mice after long term exposure to Pueraria mirifica herb. J Reprod Dev 53:995–1005
Urasopon N, Hamada Y, Asaoka K, Poungmali U, Malaivijitnond S (2008) Isoflavone content of rodent diets and its estrogenic effecton vaginal cornification in Pueraria mirifica-treated rats. Sci Asia 34:371–376
Malaivijitnond S, Tungmunnithum D, Gittarasanee S, Kawin K, Limjunyawong N (2010) Puerarin exhibits weak estrogenic activity in female rats. Fitoterapia 81:569–576
Trisomboon H, Malaivijitnond S, Cherdshewasart W, Gen Watanabe, Taya K (2006) Effect of Pueraria mirifica on the sexual skin coloration of aged menopausal cynomolgus monkeys. J Reprod Dev 52:537–542
Seriwatanachai D, Thongchote K, Charoenphandhu N, Pandaranandaka J, Tudpor K, Teerapornpuntakit J, Suthiphongchai J, Krishnamra N (2008) Prolactin directly enhances bone turnover by raising osteoblast-expressed receptor activator of nuclear factor κB ligand/osteoprotegerin ratio. Bone 42:535–546
Chauhan NS, Sharma V, Thakur M, Christine Helena Frankland Sawaya A, Dixit VK (2013) Pueraria tuberosa DC extract improves androgenesis and sexual behavior via FSH LH cascade. Sci World J 2013:780659. doi:10.1155/2013/780659
Kijkuokool P, Parhar IS, Malaivijitnond S (2006) Genistein enhances N-nitrosomethylurea-induced rat mammary tumorigenesis. Cancer Lett 242:53–59
Komori T (2015) Animal models for osteoporosis. Eur J Pharmacol 759:287–294
Trisomboon H, Malaivijitnond S, Watanabe G, Taya K (2005) Ovulation block by Pueraria mirifica: a study of its endocrinological effect in female monkeys. Endocrine 26:33–39
Malaivijitnond S, Kiatthaipipat P, Cherdshewasart W, Watanabe G, Taya K (2004) Different effects of Pueraria mirifica, a herb containing phytoestrogens, on LH and FSH secretion in gonadectomized female and male rats. J Pharmacol Sci 96:428–435
Udomsuk L, Chatuphonprasert W, Monthakantirat O, Churikhit Y, Jarukamjorn K (2012) Impact of Pueraria candollei var. mirifica and its potent phytoestrogen miroestrol on expression of bone-specific genes in ovariectomized mice. Fitoterapia 83:1687–1692
Nakamura T, Imai Y, Matsumoto T, Sato S, Takeuchi K, Igarashi K, Harada Y, Azuma Y, Krust A, Yamamoto Y, Nishina H, Takeda S, Takayanagi H, Metzger D, Kanno J, Takaoka K, Martin TJ, Chambon P, Kato S (2007) Estrogen prevents bone loss via estrogen receptor α and induction of Fas ligand in osteoclast. Cell 130:811–823
Li H, Chen B, Pang G, Chen J, Xie J, Huang H (2015) Anti-osteoporotic activity of puerarin 6″-O-xyloside on ovariectomized mice and its potential mechanism. Pharm Biol 10:1–7
Michihara S, Tanaka T, Uzawa Y, Moriyama T, Kawamura Y (2012) Puerarin exerted anti-osteoporotic action independent of estrogen receptor-mediated pathway. J Nutr Sci Vitaminol (Tokyo) 58:202–209
Manonai J, Chittacharoen A, Udomsubpayakul U, Theppisai H, Theppisai U (2008) Effects and safety of Pueraria mirifica on lipid profiles and biochemical markers of bone turnover rates in healthy postmenopausal women. Menopause 15:530–535
Acknowledgments
This study was supported by the Grant for International Research Integration: Chula Research Scholar, Ratchadaphiseksomphot Endowment Fund (to S. Malaivijitnond). The authors wish to thank Dr. I. Sandford Schwartz of Smith Naturals Co., Ltd., Thailand for providing the P. mirifica powder. The authors also would like to thank the Office of Research Affairs Chulalongkorn University for improving the manuscript’s English language.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no conflicts of interest.
Additional information
S. Jaroenporn and S. Malaivijitnond contributed equally.
Rights and permissions
About this article
Cite this article
Suthon, S., Jaroenporn, S., Charoenphandhu, N. et al. Anti-osteoporotic effects of Pueraria candollei var. mirifica on bone mineral density and histomorphometry in estrogen-deficient rats. J Nat Med 70, 225–233 (2016). https://doi.org/10.1007/s11418-016-0965-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-016-0965-5