Abstract
This quasi-experimental study examined the impact of a statewide integrated special needs program Health and Recovery Plan (HARP) for individuals with serious mental illness and identified racial and ethnic disparities in access to Medicaid services. Generalized estimating equation negative binomial models were used to estimate changes in service use, difference-in-differences, and difference-in-difference-in-differences in the pre- to post-HARP periods. Implementation of the special needs plan contributed to reductions in racial/ethnic disparities in access and utilization. Notable among those enrolled in the special needs plan was the declining Black–White disparities in emergency room (ER) visits and inpatient stays, but the disparity in non-behavioral health clinic visits remains. Also, the decline of Hispanic–White disparities in ER, inpatient, and clinic use was more evident for HARP-enrolled patients. Health equity policies are needed in the delivery of care to linguistically and culturally disadvantaged Medicaid beneficiaries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Access to appropriate and timely health care is critical to reduce disease progression and improve quality of life and health status. Unfortunately, racial/ethnic minorities experience significant disparities in rates of behavioral and physical health care access in the USA compared to White Americans.1,2 While behavioral health (BH) conditions (mental illnesses and substance use disorders) are generally undertreated, racial/ethnic minority populations receive lower rates of BH treatment than White populations.3,4,5 Some of this difference can be explained by sociological factors including culturally based perceptions and stigma; however, it may also be attributable to institutional barriers to access to care, and the patient’s ability to afford treatment.6,7
A growing body of research shows that the variations in health outcomes and health disparities experienced by racial/ethnic minority populations cannot be explained by individual-level factors alone.8,9,10,11,12 There are social, economic, political, and environmental determinants that contribute disparately to the health of minority populations. The interpersonal factors, key determinants (such as quality education, safe and affordable housing, food security, safe and clean neighborhoods, and freedom from discrimination), and systemic biases in policies and practices (structural/institutional racism) adversely affect marginalized or excluded populations and produce health inequity.9,13 The fundamental driving force underneath the multiple determinants systemic biases in policies and practices creates health inequities that are rooted in racism and discrimination.
Recently, there has been some recognition and naming of racism as a public health crisis.10,11,14 As noted in the report by Mendez et al., “Recognizing and naming racism as a public health crisis is a critical first step in dismantling structures and systems of oppressions that not only impede health and well-being but contribute to racial inequities in health.” This recognition is also critical in defining and framing discussions on the need to shift from a disparity model to an equity model.8,12 Additionally, the USA’s history of exploiting racial and ethnic minority groups for medical experimentation has planted seeds of mistrust that continue to negatively affect these populations’ access to medical care today. Experiments such as the Tuskegee Study and the San Antonio Contraceptive Study encouraged minority populations to distrust health care institutions and fueled generational trauma regarding medical care.15,16
Expanding eligibility for Medicaid through the Affordable Care Act (ACA) contributed to the reduction, but not elimination, of long-established racial disparities in health care access in the USA.17 Although the ACA cannot be solely credited with reducing coverage disparities, some states’ rejection of these programs served as a natural experiment and allowed researchers to determine that a large percentage of the reduction in coverage disparity can be attributed to these programs.18 Black and Hispanic populations experienced higher levels of physical health coverage gains and reduced levels of uninsured rates by as much as 23% following ACA enactment.17,19 There is also evidence that ACA contributed to the increased access to and utilization of mental health treatment for ethnic/racial minority populations in the form of outpatient mental health services.20
Despite strides made by the ACA, the rates of being insured among minority groups are still lower than those in the White population. Specifically, the Black population is 1.5 times, and the Hispanic population is 2.5 times more likely to be uninsured than their White counterparts.21 In addition, a Kaiser Family Foundation study found that Black and Hispanic populations are less likely than White populations to have a regular healthcare provider and are less likely to have confidence in their ability to afford regular and unexpected medical costs, which contributes to reduced healthcare usage rates by these groups.22 This study also found that Medicaid enrollees experience fewer differences in care utilization across ethnic groups than do the privately insured, except Hispanic adults are less likely than non-Hispanic White adults to postpone or do without medical care, although no significant differences have been observed between racial groups with regards to delaying or forgoing care due to cost.22 Other studies found an unintended consequence of the ACA, which is that it may increase access to health care and simultaneously inflict barriers to care in other ways. One barrier often cited is comparatively narrow networks of providers, as insurers offer plans with limited doctors and hospitals to keep premium payments as low as possible.23,24
Minority populations in the USA also experience lower rates of insurance coverage due to loss of private insurance primarily attributable to trigger events such as job loss, divorce, and losing a spouse.25,26 Regaining insurance coverage after a loss is more likely if the individual presents with certain socioeconomic characteristics including higher educational attainment, higher income, and full-time employment; it is also associated with their race/ethnicity.27,28 Hispanic and Black populations are more likely to experience adverse trigger events and have socioeconomic characteristics that are associated with greater instances of insurance loss and slower insurance gain than White populations.28,29
Research conducted in 2018 determined that managed care programs are associated with more reductions in preventable emergency department visits among non-Hispanic Black and Hispanic populations relative to non-Hispanic White populations.30 Research done on a Medicaid Managed Care (MMC) program implemented in Kentucky found that the program reduced racial/ethnic disparities seen in healthcare utilization.24 The program, called the Passport Health Plan, reduced disparities between racial and ethnic groups regarding visits to a health professional and resulted in an increased monthly professional visit rate for minorities compared to the White population. In addition, MMC plans and providers have extensive experience providing services to address the specific needs of the populations they serve and can deliver more appropriate and culturally tailored interventions.4,31
In 2015, New York State (NYS) was granted an amendment to its 1115 Medicaid waiver demonstration program to enable qualified Managed Care Organizations to comprehensively meet the needs of adults with BH conditions.32 Clinical integration and payment reform were the focus of this change and led to the adoption of an MMC product referred to as the Health and Recovery Plan (HARP). HARPs are fully integrated special needs plans that cover all medical and behavioral health needs for an estimated 150,000 NYS residents with serious mental illness (SMI). HARPs also offer access to an enhanced benefit package comprised of Home and Community Based Services (HCBS) designed to provide the individual with a specialized scope of support services not currently covered under the State Plan. Individuals enrolled in HARPs were offered Health Home care management services. Health Homes develop person-centered plans of care that integrate physical and behavioral health services including HCBS for eligible individuals. The HCBS are recovery-oriented and designed to assist individuals with independent daily living and social skills, education and employment support services, peer and family support, habilitation services (daily living skills), non-medical transportation, and crisis management. Beyond those efforts at coverage expansions, HARPs also have specialized staffing requirements and qualifications along with focused BH performance metrics and incentives to achieve health, wellness, recovery, and community inclusion for enrollees.33
This study aims to examine the impact of the HARP program enacted in 2015–2016 on Medicaid services utilization among racial and ethnic minorities. We hypothesized that the HARP program can reduce the relative differences in ER, inpatient, and outpatient service use between White and other racial/ethnic enrollees. Based on previous research on MMC and historical and cultural trends, rates of health care access and utilization are not equal between White and minority populations.4,24,31 This disparity is thought to improve with implemented care coordination and management, especially if that care is provided by teams well-versed in delivering culturally sensitive care and interventions to beneficiaries. In this analysis, this hypothesis was tested, and the HARP program’s impact among racial/ethnic minorities was estimated using quasi-experimental difference-in-differences (DD) and difference-in-difference-in-differences (DDD) approach. That is, the DD compared changes in service use over time between minority patients and White patients within the HARP-enrolled population and similarly within the HARP-eligible population. The DDD compared changes in service use over time between HARP-enrolled racial/ethnic differences and HARP-eligible racial/ethnic differences.
Method
Data source
As described in a prior report,34 the New York State Office of Mental Health (OMH, which is the State’s mental health authority) view of the New York State Medicaid claims and encounter data system was used to identify the study population and health services used. This database provided information on all Medicaid recipients who were eligible for HARP and the associated health services claimed during the study period.
Study period and population
The HARP program was implemented for New York City residents (NYC) in October 2015. The exposure group (HARP) was defined as HARP-enrolled at some point during the year’s “rollout phase.” The control group was defined as HARP-eligible but never enrolled during the “rollout phase.” The pre-HARP period was defined as two years prior to the implementation start date, from October 2013 to October 2015. It took time to fully implement the HARP; as such, a “rollout phase” was used as a ramp-up period and was excluded from pre-post comparison periods. As such, the post-HARP period was defined as October 2016 to October 2018 (Fig. 1). Individuals in the HARP-enrolled group and HARP-eligible control group were required to be continuously eligible for Medicaid with no more than a 45-day gap for the entire study period (pre-, rollout, and post-phase). Among 85,121 individuals who were enrolled in Medicaid and were eligible for HARP enrollment, 16,135 (18.96%) were enrolled in Medicaid for less than 48 months of the entire study period and hence were considered as not continuously enrolled in Medicaid and excluded from the study sample. The DD and DDD approach ideally require outcomes/events (continuous services use) in at least 2 pre- and 2 post-periods, which presents unique challenges with individuals having major gaps in services/coverage. However, we acknowledge that individuals with major gaps in Medicaid coverage are a problem worthy of future independent investigation. Individuals in the HARP-enrolled group and HARP-eligible control group were excluded from the study if they “switched” enrollment, i.e., disenrolled from or enrolled in the HARP in the two-year post period. In this analysis, only 40 patients in the control group and 18 patients in the HARP group switched in and out of the HARP program, respectively, during the study period. The final study population consisted of Medicaid-enrolled adults ages 21–64 years who were enrolled (HARP-enrolled, N = 35,579) or HARP-eligible (control group, N = 10,997).
HARP eligibility was based on Medicaid beneficiaries meeting targeting criteria and/or certain risk factors.35 The targeting criteria were defined as adults with SMI and/or substance use disorder (SUD) diagnoses presenting serious functional deficits using a State-derived algorithm. The risk factors were based on receiving Supplemental Security Income; having a current or expired Assisted Outpatient Treatment order; living in an Office of Mental Health (OMH) operated or licensed residential program; Department of Corrections and Community Supervision clients with SMI discharged from OMH-operated facilities; and past use of OMH-licensed recovery-oriented community-based services, inpatient services, or emergency room services. HARP-eligible enrollees of a Medicaid Managed Care Organization that runs a HARP did not have to do anything to join. They received a notice from New York Medicaid Choice. They then had 30 days to opt-out or choose to enroll in another HARP. HARP-eligible enrollees of a Medicaid Managed Care Organization without a HARP needed to take action to join a HARP. They received a notice from NYS telling them how to join a HARP. Once enrolled in a HARP, members have 90 days to choose another HARP or return to their previous plan. After 90 days, members are locked into their HARP of choice for 9 additional months. SMI or SUD individuals enrolled in an HIV (human immunodeficiency virus) Special Needs Plan (SNP) were able to receive HCBS services through the HIV SNP. They were notified of their HARP eligibility by the NYS Enrollment Broker. HARP enrollment was voluntary, and eligible individuals could also choose to remain in a mainstream plan.36,37
Variables
We used Medicaid fee-for-service claims and managed care encounter claims to categorize the dependent variable into three service types: inpatient stays, ER, and outpatient visits. Medicaid programs that operate a fee-for-service system pay providers directly for their services based on submitted claims. With managed care, the Medicaid agency pays managed care organizations a monthly capitation for each beneficiary enrolled in each managed care organization. The managed care organizations then pay providers for services delivered to Medicaid enrollees. The data from these claims, fee-for-service, and encounters create a snapshot of services provided to Medicaid beneficiaries.
The fee-for-service and encounters data were converted into service types (inpatient stays, emergency, and outpatient visits) using rate codes, diagnosis-related group codes, specialty codes, procedure codes, revenue codes, and hospital provider type. Inpatient was categorized as all-cause, behavioral, and non-behavioral stays at licensed general or private hospitals. BH inpatient stays included treatment for mental illnesses and substance use (detoxification, rehabilitation, and diagnosis-based) disorders. Non-BH inpatient comprised stays that did not meet the conditions for mental and substance use disorder treatment. ER was also categorized as all-cause, behavioral, and non-behavioral health-related visits to general hospitals and comprehensive psychiatric emergency programs. BH ER visits were comprised of mental health- and substance use disorder-related visits. Non-BH ER use was comprised of visits that were related to neither mental health nor substance use disorders. Outpatient was defined as BH and non-BH clinic visits. BH clinic visits were comprised of psychiatry-related or substance use disorder-related visits at an OMH-licensed clinic or Office of Addiction Services and Supports (OASAS) outpatient setting/clinic. Non-BH clinic use was comprised of visits that were related to neither mental health nor substance use.
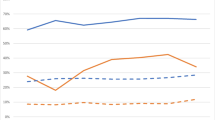
Race/ethnicity data were obtained through Medicaid-covered services. Medicaid agencies ask applicants to self-report their race and ethnicity, but it is not mandatory since that data are not considered when determining Medicaid eligibility. Racial/ethnic groups were categorized as non-Hispanic Whites (hereafter Whites), non-Hispanic Blacks (hereafter Blacks), non-Hispanic Asians/Pacific Islander (hereafter Asians), non-Hispanic American Indian/Alaskan native (hereafter AIANs), and Hispanics. Individuals with racial/ethnic group indicated as “other” or unknown were excluded from this analysis. In this analysis, the health behaviors of White patients were considered as the standard because the trends of their average ER, average inpatient, and average clinic use were like the thresholds of the expected/average use in the entire study population. When looking at the trends of the minority patients, the thresholds were either lagging or ahead of the thresholds of the entire study population. See Fig. 2. Although the thresholds of White patients were held as the standard, it must not be inferred that their rate of service use necessarily means better care or better health. Lesser use may indicate lesser need, underuse, or lack of accessibility in a different service setting or type. Also, greater use in a particular service type may indicate a greater need, overuse, or compensation for non-available or accessible appropriate service type. For instance, the use of more ER services may mean greater access; it may also be used as compensation for non-available needed service types. Notwithstanding the complexities of ER usage, this analysis included ER visits to address the wholistic differences in service use among different racial groups.
Claims and encounter data were also used to characterize other demographic characteristics, behavioral diagnoses, and health conditions/clinical risks status during the pre-HARP period. Other demographics were sex, age, and Health Home assignment (yes, no). Principal diagnoses include schizophrenia, mood disorders, anxiety disorders, non-mental health disorders, organic mental disorders, and substance use disorders. Clinical Risk Group (CRG) status,38 developed by 3 M, is a population classification system that uses inpatient and ambulatory diagnosis and procedure codes, pharmaceutical data, and functional health status to assign individuals to a single, severity-adjusted group. These were used to assign patients to 1 of 9 mutually exclusive CRG groups.
Statistical analyses
We report clinical and demographic characteristics for HARP-enrolled and HARP-eligible individuals by race/ethnicity. HARP program effects were estimated using difference-in-differences (DD) and difference-in-difference-in-differences (DDD) analyses. One of the assumptions the DD model makes is that the trends in the outcomes (average service use) are parallel for White individuals and minority population groups prior to the implementation of the HARP MMC program. In other words, in the absence of the HARP MMC program, the two groups would have continued to move in tandem. This assumption is usually evaluated with a parallel-trends test or graphical analysis, or both. A visual check of these trends can be obtained by plotting the means of the outcome over time for both groups, as seen in Fig. 2. The graphical analysis of Fig. 2 supports the parallel-trends assumption. The HARP program effect (DD estimate) on service use between racial/ethnic groups hinges on the assumption that there were no shocks (unexpected or unpredictable events) other than the HARP program to all racial/ethnic groups or the effect of other shocks did not vary by race/ethnicity. For example, the DD in services used between White (W) patients and Black (B) patients over time within the HARP-enrolled group can be specified as follows: DD = (Upost-B – Upre-B) – (Upost-W – Upre-W). Specifically, the DD is equivalent to calculating the after-before HARP difference in services used in the Black patients and subtracting from this difference the after-before HARP difference in the White patients. Likewise, the DDD which extends the DD model controls for racial/ethnic differences in service use trends unrelated to the HARP program that might have affected the DD estimates of the HARP program effect. Using the above example, the DDD can be specified as follows :
Generalized estimating equation (GEE) negative binomial models with a robust error variance (accounting for multiple observations per individual)39,40 were used to estimate the inpatient stay, ER, and outpatient visit incident rate changes in the pre-relative to post-HARP periods between racial/ethnic groups and HARP-enrolled vs. HARP-eligible. The GEE models were specified for the service use outcomes with interaction terms between the variables, pre-post HARP, racial/ethnic groups, and HARP-enrolled or HARP-eligible. All models adjusted for factors known to influence service utilization41 including demographic characteristics (gender and age), need variables (principal diagnoses and CRG Status), and Health Home assignment.
The DD and DDD comparisons were used to evaluate the changes (1) within racial/ethnic groups between HARP-enrolled and HARP-eligible populations and (2) between racial/ethnic groups on the impact of HARP implementation across HARP-enrolled and HARP-eligible populations. For the DDD estimates, the reference groups were non-Hispanic Whites, pre-HARP period, and HARP-eligible population. Rate ratios (RRs) with 95% confidence intervals are presented. A review by Nathan S. Kline Institute’s Institutional Review Board deemed this study to not involve human subjects’ research.
Results
Demographic characteristics
Table 1 reports the pre-HARP sample characteristics by racial/ethnic groups. Fewer males enrolled in the HARP program (48.5%) compared to the non-HARP (HARP-eligible, control) population (59.2%). The average age ranged from 43.1 to 48.7 years. Overall, compared to Whites, other racial/ethnic groups especially Black and Hispanic patients were less likely to be healthy and more likely to have a catastrophic condition (patients hospitalized for an acute illness or catastrophic event) according to the clinical risk groups.
Difference-in-differences estimates of pre vs. post comparing racial/ethnic groups in the HARP-enrolled population
The difference-in-differences estimates in service use between White and minority patients over time within the HARP group are presented in Table 2. Black patients compared to White patients had relatively more BH-related ER visits (DD = 1.14, 95% CI = 1.02, 1.27), inpatient stays (DD = 1.11, 95% CI = 1.02, 1.21), and clinic visits (DD = 1.05, 95% CI = 1.02, 1.08), as well as significantly lower non-BH clinic visits (DD = 0.96, 95% CI = 0.93, 0.98). The relative increases in the BH-related services among Black patients may signal greater accessibility to or need of BH services, along with a lack of appropriate medical services given the relatively lesser non-BH clinic visits. It could also mean that Black patients are relatively sicker compared to White patients and may require additional services.
Hispanic patients in comparison to White patients had relatively more all-cause inpatients stays (DD = 1.11, 95% CI = 1.03, 1.2) and non-BH clinic visits (DD = 1.04, 95% CI = 1.01, 1.07). The increase in clinic visits may signal an improvement in the use of medical services among HARP-enrolled Hispanic patients.
Difference-in-differences estimates of pre vs. post comparing racial/ethnic groups in the non-HARP (HARP-eligible) population
Table 2 also presents the DD estimates in service use between White and minority patients over time within the non-HARP group. Hispanic patients compared to White patients had relatively more all-cause inpatient (DD = 1.19, 95% CI = 1.01, 1.4) stays. However, they had relatively lower all-cause ER visits (DD = 0.84, 95% CI = 0.71, 0.98), BH clinic visits (DD = 0.82, 95% = 0.74, 0.91), and non-BH clinic visits (DD = 0.87, 95% CI = 0.8, 0.95). Unlike Hispanic patients in the HARP group, the relatively lower ER and clinic visits may indicate underuse, lack of access to these service settings, or lack of culturally competent services.
AIAN patients in comparison to White patients had relatively lower non-BH ER visits (DD = 0.63, 95% CI = 0.45, 0.88). This reduction in relative medical ER service use, as in the case of Hispanic patients, may indicate a lack of culturally competent services.
Difference-in-difference-in-differences estimates comparing racial/ethnic groups pre-post and HARP-enrolled versus non-HARP (HARP-eligible)
As stated above, the DDD extends the DD model and controls for racial/ethnic possible differences in service use trends that are unassociated with the HARP program. The DDD estimate indicates whether the differences in the relative service use between minority patients and White patients in the HARP group were larger or lesser than those seen in the corresponding racial/ethnic groups in the non-HARP group. In the DD analysis, the observed relative increase in BH and non-BH clinic visits among Hispanic patients in the HARP group might have resulted from underlying racial/ethnic differences in clinic visits not associated with the HARP program. After controlling for such potential differences in the DDD analysis, the difference in relative level of BH (DDD = 1.19, 95% CI = 1.08, 1.32) and non-BH (DDD = 1.19, 95% CI = 1.08, 1.30) clinic visits among Hispanic patients in the HARP group remained significant. Also, the DDD analysis showed a significant relative increase in all-cause ER (DDD = 1.22, 95% CI = 1.03, 1.45) and BH ER (DDD = 1.47, 95% CI = 1.02, 2.11) visits that the DD analysis had failed to show. The DD analysis comparing AIAN patients to White patients in the HARP group showed no relative difference in all-cause ER and non-BH ER visits. However, the DDD analysis for change in relative all-cause ER (DDD = 1.48, 95% CI = 1.01, 2.17) and non-BH ER (DDD = 1.69, 95% CI = 1.16, 2.46) visits were positive and significant. This is an indication that HARP-enrolled AIAN patients had greater access to ER services.
Discussion
Consistent with previous research, the findings reported here suggest that the HARP MMC program contributed to reductions in racial/ethnic disparities in access and utilization.24,30,42,43 Specifically notable in the HARP group were the declining Black–White disparities in inpatient stays and ER visits for both behavioral and non-behavioral reasons. It is unclear whether the relatively higher levels of ER and inpatient use for both behavioral and non-behavioral reasons reflect greater access to needed services or alternative use for non-available or accessible appropriate service type.43 Evidence suggests that Black patients are more likely than White patients to access healthcare through the emergency room.43,44,45 Commonly accepted explanations that focus on travel distances, socioeconomic characteristics, environmental factors, institutional barriers, and limited access to patients’ preferred outpatient services remain hypotheses that merit rigorous testing.45,46,47
There were also notable Black–White differences in outpatient service use. The results show evidence of substantial increments in BH-related clinic visits among Black patients. This is counter to broad findings from prior studies.48,49,50 Also notable in the HARP group were the Black–White disparities in non-behavioral health clinic visits. The differential reduction in the relative use of non-behavioral health clinic visits—that is, primary care/physical health visits—indicates that Black patients may require greater assistance in finding primary care providers. This finding mirrors the results of studies that examined the effects of MMC programs on racial/ethnic disparities in health care access and utilization in the past two decades.41,43 The fact that Black–White disparities in primary care remain worst after many federal and state healthcare reforms implies that further increases in coverage will require improvements not only in non-behavioral health programs uptake but also the adoption of Medicaid expansion with an emphasis on equity51 and primary care.52 Evidence from Oregon’s prioritization of disparities as a key target for Medicaid expansion suggest that using a multi-faceted approach that includes strategic planning with managed care organizations, expanding the use of community health workers in the areas with a higher percentage of Black residents, and coordinating with regional health equity coalitions can be effective in reducing Black–White disparities in primary care.51 At the same time, other approaches will be necessary to improve access to primary care for Black patients. One such approach would be renewed policies and clinical efforts targeting health equity, increasing community centers, and recruiting and expanding the diversity of providers.53
This study also found evidence of declining Hispanic–White disparities in service use among HARP enrollees. Notable were the declining Hispanic–White disparity in all-cause inpatient stays. Also, unlike Black patients, Hispanic patients compared to White patients saw a significant increase in non-behavioral health visits indicating greater access to primary/physical health care. This confirms previous findings that racial/ethnic minority groups may not equally benefit from access to needed health care. For example, LeCook43 found that MMC narrowed the gap in having a usual source of care for both Black and Hispanic patients. The same study also found reductions in Black–White disparity in having any doctor visit, but no change in Hispanic–White disparity.
This study found no statistically significant Asian–White or AIAN–White differences in service use among HARP enrollees. Despite the lack of statistically significant results in the current study, the difficulties in getting appointments, dissatisfaction with the care received, and less continuity of care among Asian and AIAN patients among Medicaid Managed Care beneficiaries in the past two decades are well documented.54,55,56 Findings from a recent national study that investigated health care experiences of adult Medicaid beneficiaries by race/ethnicity and rural/urban status showed that these difficulties persist. They found that compared to White beneficiaries, AIAN and Asian patients reported worse experiences with access to care, provider communications, and customer service received from plans.57
One somewhat striking result was the difference between HARP-enrolled Hispanic patients compared to HARP-eligible Hispanic patients. The observed differences show that HARP-eligible Hispanics had the worse experience in terms of access to, or use of, or both, for BH and non-Services. These gaps between HARP-enrolled Hispanic and HARP-eligible Hispanic patients cannot be explained by differences in culture, personal characteristics, or community, but rather by plan type. Evidence from previous studies suggest that linguistically and culturally targeted outreach strategies can be effective in increasing program uptake among eligible patients.4,31 This finding necessitates state policy makers to adopt MMC arrangements that require plans to create provider networks that can serve the language and cultural needs of Medicaid beneficiaries.58
Overall, HARP-enrolled Hispanic patients appeared to have benefited most from the HARP MMC implementation. The DDD results suggest that the relatively higher levels of ER and clinic use were even more evident for HARP-enrolled Hispanics. Although these increases may not reflect effectiveness or quality of care, it indicates greater access and substantial reductions in Hispanic–White disparities in service use. Although the DD results showed no statistically significant differences between AIAN and White patients, the DDD showed that HARP-enrolled AIAN patients had relatively more ER visits compared to White patients. While the increase in ER visits may reflect overutilization or greater access to needed services, it is possible that HARP-enrolled AIAN patients might be accessing healthcare through the ER. It is also possible that they might require assistance in finding preferred behavioral and non-behavioral health services. The Oregon study that prioritized disparities as a key target for Medicaid expansion found reductions in AIAN–White disparities in primary care visits, and persistently higher visit rates among AIAN patients compared to White patients. This further emphasizes the need for states and policy makers to adopt culturally targeted outreach strategies in program uptake among eligible patients.
While these findings may offer some encouragement to policy makers, other studies showed that insurance coverage alone does not ensure improved access to care, quality of care, and better health among racial/ethnic minorities.59,60,61,62,63 Also, HCBS was not fully implemented during the time frame of the study. Therefore, we should try to understand the complexity of the areas in which the HARP offers the greatest value for racial/ethnic minorities and explore approaches to improve the delivery of care to culturally disadvantaged Medicaid beneficiaries.
Limitations
This analysis had some limitations. First, this analysis was conducted in a single state, and the results may not be generalizable to other states. New York State has one of the largest Medicaid programs in the country with estimated spending of almost $78 billion a year (second highest in the nation) and roughly 24% of the NYS population enrolled in the program.64 Also, NYS has geographically diverse populations, especially in the NYC region; therefore, the results of this study should provide information for other state policy makers. Second, submitting race/ethnicity information on the Medicaid application is optional and can lead to missing data if instructions and rationale for such information are not clear. Also, applicants may select multiple races and ethnicity categories, limiting the ability to meaningfully interpret and group the data. Third, there are historical experiences and cultural differences in the broad categories of racial/ethnic groups that are not accounted for in this analysis. Fourth, there were several complaints and action appeals filed by consumers with MMC plans regarding service accessibility/utilization and quality of care. These complaints showed that HARP insurance coverage did not always guarantee access to health care. Detailed information on service denials were not available and therefore were not accounted for in this analysis. Finally, the impact of HARP implementation on service use does not necessarily reflect changes in quality of care or improvement in clinical outcomes. Future studies will investigate whether HARP leads to improvements in quality of care and long-term clinical outcomes for all racial/ethnic groups.
Implications for Behavioral Health
The HARP MMC goals were to decrease ER and inpatient services, increase outpatient and recovery services, and improve the quality of healthcare. The findings of this study showed that HARP MMC contributed to reductions in disparities in access and utilization for Hispanic and Black patients. Specifically, the study found reductions of disparities in inpatient stays and notably non-behavioral clinic visits for Hispanic patients, and disparity reductions in ER visits and inpatient stays for Black patients. Despite these differential increases, racial/ethnic minority groups may not equally benefit from enhanced access to primary care. Most discouragingly, the disparity in non-behavioral clinic (essentially primary care) visits for Black patients persists in a HARP MMC program designed to increase access to both behavioral and non-behavioral services. These findings suggest that HARP MMC increased access and unitization, and that while some racial/ethnic disparities were improved, some remained. Existing policies may be amended, or new health equity policies should be enacted to systematically monitor services used by racial/ethnic groups. Improving equal access to quality care for all racial/ethnic groups can improve the overall health care system and reduce health care disparities and cost. To achieve such improvements, the four key steps to advancing health equity put forth by Kerkhoff and colleagues12 are strongly recommended. (1) Identify important stakeholders related to equity and establish roles for partners throughout the entire implementation process. (2) Include equity-related considerations when deciding which intervention(s) to implement and/or de-implement. (3) Evaluate the performance gap related to the intervention or program of interest in vulnerable populations. (4) Identify and prioritize barriers faced by vulnerable populations, including structural racism and power dynamics. These key steps together with other recommendations outlined elsewhere9 may systematically move identifying health disparities to action to achieve better health equity.
References
Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Transactions of the American Clinical and Climatological Association. 2012;123:167-172;
Copeland VC. African Americans: disparities in health care access and utilization. Health & Social Work 2005;30(3):265-270. https://doi.org/10.1093/hsw/30.3.265
Cook BL, Zuvekas SH, Carson N, et al. Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Services Research. 2014;49(1):206-229. https://doi.org/10.1111/1475-6773.12095
Kohn-Wood L, Hooper L. Cultural competency, culturally tailored care, and the primary care setting: possible solutions to reduce racial/ethnic disparities in mental health care. Journal of Mental Health Counseling. 2014;36(2):173-188. https://doi.org/10.17744/mehc.36.2.d73h217l81tg6uv3
Substance Abuse and Mental Health Services Administration, Racial/ ethnic differences in mental health service use among adults. HHS Publication No. SMA-15-4906. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015. https://www.samhsa.gov/data/sites/default/files/MHServicesUseAmongAdults/MHServicesUseAmongAdults.pdf Accessed 30 March, 2022.
Jha A, Orav E, Epstein A. Low quality, high-cost hospitals, mainly in south, care for sharply higher shares of elderly black, Hispanic, and Medicaid patients. Health Affairs. 2011;30(10):1904-1911. https://doi.org/10.1377/hlthaff.2011.0027
Chauhan A, Walton M, Manias E, et al. The safety of health care for ethnic minority patients: a systematic review. International Journal for Equity in Health. 2020;19(1):118. https://doi.org/10.1186/s12939-020-01223-2
Srinivasan S, Williams SD. Transitioning from health disparities to a health equity research agenda: the time is now. Public Health Reports. 2014;129:71-6. https://doi.org/10.1177/00333549141291S213
Braveman P, Arkin E, Orleans T, et al. What is health equity? And what difference does a definition make? Princeton, NJ: Robert Wood Johnson Foundation, 2017.
Analysis: declarations of racism as a public health crisis. American Public Health Association. https://www.apha.org/topics-and-issues/health-equity/racism-and-health/racism-declarations Accessed 9 June, 2022.
Mendez DD, Scott J, Adodoadji L, et al. Racism as public health crisis: assessment and review of municipal declarations and resolutions across the United States. Frontiers in Public Health. 2021:1142. https://doi.org/10.3389/fpubh.2021.686807
Kerkhoff AD, Farrand E, Marquez C, et al. Addressing health disparities through implementation science – a need to integrate an equity lens from the outset. Implementation Science. 2022;17(1):1-4. https://doi.org/10.1186/s13012-022-01189-5
Lett E, Adekunle D, McMurray P, et al. Health equity tourism: ravaging the justice landscape. Journal of Medical Systems. 2022;46(3):1-6. https://doi.org/10.1007/s10916-022-01803-5
Schouler-Ocak M, Bhugra D, Kastrup MC, et al. Racism and mental health and the role of mental health professionals. European Psychiatry. 2021;64(1). https://doi.org/10.1192/j.eurpsy.2021.2216
Scharff DP, Mathews KJ, Jackson P, et al. More than Tuskegee: understanding mistrust about research participation. Journal of Health Care for the Poor and Underserved. 2010;21(3):879. https://doi.org/10.1353/hpu.0.0323
Kim WO. Institutional review board (IRB) and ethical issues in clinical research. Korean Journal of Anesthesiology 2012;62(1):3-12. https://doi.org/10.4097/kjae.2012.62.1.3
Courtemanche C, Marton J, Ukert B, et al. The three-year impact of the Affordable Care Act on disparities in insurance coverage. Health Services Research. 2019;54 Suppl 1:307-316. https://doi.org/10.1111/1475-6773.13077
Flores RD, Vargas R. Medicaid expansion and ethnoracial disparities in health insurance coverage. Journal of Ethnic and Migration Studies. 2017;43(12):2055-2071. https://doi.org/10.1080/1369183x.2017.1323451
Angier H, Hoopes M, Marino M, et al. Uninsured primary care visit disparities under the Affordable Care Act. Annals of Family Medicine. 2017;15(5):434-442. https://doi.org/10.1370/afm.2125
Breslau J, Han B, Lai J, et al. Impact of the affordable care act Medicaid expansion on utilization of mental health care. Medical Care. 2020;58(9):757-762. https://doi.org/10.1097/MLR.0000000000001373
Health coverage by race and ethnicity, 2010–2019. Kaiser Family Foundation https://www.kff.org/racial-equity-and-health-policy/issue-brief/changes-in-health-coverage-by-race-and-ethnicity-since-the-aca-2010-2018/. Published July 16, 2021. Accessed 30 March, 2022.
Racial and ethnic disparities in access to and utilization of care among insured adults. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-and-ethnic-disparities-in-access-to-and-utilization-of-care-among-insured-adults/. Published August 6, 2015. Accessed 30 March, 2022.
Kominski GF, Nonzee NJ, Sorensen A. The affordable care act’s impacts on access to insurance and health care for low-income populations. Annual Review of Public Health. 2017;38:489-505. https://doi.org/10.1146/annurev-publhealth-031816-044555
Marton J, Yelowitz A, Shores M, et al. Does Medicaid Managed Care help equalize racial and ethnic disparities in utilization? Health Services Research. 2016;51(3):872-891. https://doi.org/10.1111/1475-6773.12396
Bureau of Labor Statistics. Labor force characteristics by race and ethnicity, 2013. https://www.bls.gov/opub/reports/race-and-ethnicity/archive/race_ethnicity_2013.pdf Accessed 30 March, 2022.
Lavelle B, Smock PJ. Divorce and women’s risk of health insurance loss. Journal of Health and Social Behavior 2012;53(4):413-431. https://doi.org/10.1177/0022146512465758
Peters HE, Simon K, Taber JR. Marital disruption and health insurance. Demography. 2014;51(4):1397-1421. https://doi.org/10.1007/s13524-014-0317-6
Sohn H. Racial and ethnic disparities in health insurance coverage: dynamics of gaining and losing coverage over the life-course. Population Research Policy Review. 2017;36(2):181-201. https://doi.org/10.1007/s11113-016-9416-y
Health coverage by race and ethnicity: the potential impact of the Affordable Care Act. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity-the-potential-impact-of-the-affordable-care-act/. Published March 13, 2013. Accessed 30 March, 2022.
Hu T, Mortensen K, Chen J. Medicaid Managed Care in Florida and racial and ethnic disparities in preventable emergency department visits. Medical Care. 2018;56(6):477-483. https://doi.org/10.1097/MLR.0000000000000909
Yamada AM, Brekke JS. Addressing mental health disparities through clinical competence not just cultural competence: the need for assessment of sociocultural issues in the delivery of evidence-based psychosocial rehabilitation services. Clinical Psychology Review. 2008;28(8):1386-1399. https://doi.org/10.1016/j.cpr.2008.07.006
Health and recovery plans (HARPs). Omh.ny.gov. https://omh.ny.gov/omhweb/bho/harp.html. Accessed 30 March, 2022
New York State Office of Mental Health. Interim report to the statewide comprehensive plan (USA). https://www.omh.ny.gov/omhweb/planning/docs/2017-interim-report-web.pdf Accessed 30 March, 2022.
Frimpong EY, Ferdousi W, Rowan GA, et al. Impact of the 1115 behavioral health Medicaid waiver on adult Medicaid beneficiaries in New York State. Health Services Research. 2021;56(4):677-690. https://doi.org/10.1111/1475-6773.13657
New York State Office of Alcoholism and Substance Abuse Services. New York Request for Qualifications for Behavioral Health Benefit Administration. https://www.omh.ny.gov/omhweb/bho/final-rfq.pdf Accessed 30 March, 2022.
New York State Department of Health. Independent Evaluation of the New York State (NYS) Health and Recovery Plans (HARP) Program and Self-Directed Care (SDC) Pilot Program. https://www.health.ny.gov/funding/rfp/20024/20024.pdf Accessed 30 March, 2022.
New York State Office of Alcoholism and Substance Abuse Services. Behavioral health providers, health home care managers and consumer advocates. https://omh.ny.gov/omhweb/bho/docs/harp-plans.pdf Accessed 30 March, 2022.
3M Health Information Systems. 3M clinical risk groups: measuring risk, managing care. https://multimedia.3m.com/mws/media/765833O/3m-crgs-measuring-risk-managing-care-white-paper.pdf
Lechner M. The estimation of causal effects by difference-in-difference Methods Estimation of spatial panels. Found Trends® Economy. 2010;4(3):165–224. https://doi.org/10.1561/0800000014
Ziegler A, Kastner C, Blettner M. The generalised estimating equations: an annotated bibliography. Biometrical Journal. 1998;40(2):115-139. https://doi.org/10.1002/(sici)1521-4036(199806)40:2<115::aid-bimj115>3.0.co;2-6
Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Services Research. 2000;34(6):1273-1302.
Tai-Seale M, Freund D, LoSasso A. Racial disparities in service use among Medicaid beneficiaries after mandatory enrollment in managed care: a difference-in-differences approach. Inquiry. 2001;38(1):49-59. https://doi.org/10.5034/inquiryjrnl_38.1.49
Cook BL. Effect of Medicaid Managed Care on racial disparities in health care access. Health Services Research. 2007;42(1 Pt 1):124-145. https://doi.org/10.1111/j.1475-6773.2006.00611.x
Nearly half of US medical care comes from emergency rooms: figures are even higher for minorities and women. Science Daily. https://www.sciencedaily.com/releases/2017/10/171017091849.htm. Accessed 30 March, 2022.
Brown LE, Burton R, Hixon B, et al. Factors influencing emergency department preference for access to healthcare. Western Journal of Emergency Medicine. 2012;13(5):410-415. https://doi.org/10.5811/westjem.2011.11.6820
Chen BK, Cheng X, Bennett K, et al. Travel distances, socioeconomic characteristics, and health disparities in nonurgent and frequent use of Hospital Emergency Departments in South Carolina: a population-based observational study. BMC Health Services Research. 2015;15(1):203. https://doi.org/10.1186/s12913-015-0864-6
Snowden LR. Barriers to effective mental health services for African Americans. Mental Health Services Research 2001;3(4):181-187. https://doi.org/10.1023/a:1013172913880
Hines-Martin V, Malone M, Kim S, et al. Barriers to mental health care access in an African American population. Issues in Mental Health Nursing. 2003;24(3):237-256. https://doi.org/10.1080/01612840305281
Manseau M, Case BG. Racial-ethnic disparities in outpatient mental health visits to U.S. physicians, 1993–2008. Psychiatric Services. 2014;65(1):59–67. https://doi.org/10.1176/appi.ps.201200528
Dobalian A, Rivers PA. Racial and ethnic disparities in the use of mental health services. Journal of Behavioral Health Services & Research. 2008;35(2):128-141. https://doi.org/10.1007/s11414-007-9097-8
Cook BL, Trinh NH, Li Z, et al. Trends in racial-ethnic disparities in access to mental health care, 2004-2012. Psychiatric Services. 2017;68(1):9-16. https://doi.org/10.1176/appi.ps.201500453
McConnell KJ, Charlesworth CJ, Meath THA, et al. Oregon’s emphasis on equity shows signs of early success for black and American Indian Medicaid enrollees. Health Affairs (Millwood). 2018;37(3):386-393. https://doi.org/10.1377/hlthaff.2017.1282
Patel MR, Tipirneni R, Kieffer EC, et al. Examination of changes in health status among Michigan Medicaid expansion enrollees from 2016 to 2017. Journal of American Medical Association Network Open. 2020;3(7):e208776. https://doi.org/10.1001/jamanetworkopen.2020.8776
Appel HB, Nguyen PD. Eliminating racial and ethnic disparities in behavioral health care in the U.S. Journal of Health and Social Sciences. 2020;5:441–8. https://journalhss.com/wp-content/uploads/appel_10.192042020lmnt7.pdf. https://doi.org/10.19204/2020/lmnt7
Misra R, Modawal A, Panigrahi B. Asian-Indian physicians’ experience with managed care organizations. International Journal of Health Care Quality Assurance 2009;22(6):582-599. https://doi.org/10.1108/09526860910986858
Weech-Maldonado R, Morales LS, Elliott M, et al. Race/ethnicity, language, and patients’ assessments of care in Medicaid Managed Care. Health Services Research. 2003;38(3):789-808. https://doi.org/10.1111/1475-6773.00147
Weech-Maldonado R, Elliott MN, Morales LS, et al. Health plan effects on patient assessments of Medicaid Managed Care among racial/ethnic minorities. Journal of General Internal Medicine. 2004;19(2):136-145. https://doi.org/10.1111/j.1525-1497.2004.30235.x
Martino SC, Mathews M, Agniel D, et al. National racial/ethnic and geographic disparities in experiences with health care among adult Medicaid beneficiaries. Health Services Research. 2019;5(1):287-296. https://doi.org/10.1111/1475-6773.13106.
McDonough JE, Gibbs BK, Scott-Harris JL, et al. A state policy agenda to eliminate racial and ethnic health disparities. New York: Commonwealth Fund of New York. 2004.
Alegría M, Alvarez K, Ishikawa RZ, et al. Removing obstacles to eliminating racial and ethnic disparities in behavioral health care. Health Affairs (Millwood). 2016;35(6):991-999. https://doi.org/10.1377/hlthaff.2016.0029
Horvitz-Lennon M, Volya R, Donohue JM, et al. Disparities in quality of care among publicly insured adults with schizophrenia in four large U.S. states, 2002–2008. Health Services Research. 2014;49(4):1121–1144. https://doi.org/10.1111/1475-6773.12162
Horvitz-Lennon M, Volya R, Garfield R, et al. Where you live matters: quality and racial/ethnic disparities in schizophrenia care in four state Medicaid programs. Health Services Research. 2015;50(5):1710-1729. https://doi.org/10.1111/1475-6773.12296
Breslau J, Leckman-Westin E, Yu H, et al. Impact of a mental health based primary care program on quality of physical health care. Administration and Policy in Mental Health. 2018;45(2):276-285. https://doi.org/10.1007/s10488-017-0822-1
Gifford K, Ellis E, Edwards BC, et al. Medicaid moving ahead in uncertain times: results from a 50-state Medicaid Budget Survey for state fiscal years 2017 and 2018. Kaiser Family Foundation. Published October 19, 2017. Accessed 4 April, 2022. https://www.kff.org/medicaid/report/medicaid-moving-ahead-in-uncertain-times-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2017-and-2018/
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Rights and permissions
About this article
Cite this article
Frimpong, E.Y., Ferdousi, W., Rowan, G.A. et al. Racial and Ethnic Disparities in Health Care Access and Utilization among Medicaid Managed Care Beneficiaries. J Behav Health Serv Res 50, 194–213 (2023). https://doi.org/10.1007/s11414-022-09811-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-022-09811-6