Abstract
The integration of multiple ancillary services into mental health treatment settings may improve outcomes, but there are no national studies addressing whether comprehensive services are distributed equitably. We investigated whether the availability of a wide range of service types differs based on the facility’s racial/ethnic composition. We used the 2020 National Mental Health Services Survey to identify twelve services offered in outpatient mental health treatment facilities (N = 1,074 facilities). We used logistic regression to model each of the twelve services, predicted by the percentage of a facility’s clientele that was White, Black, and Hispanic, adjusted for covariates. Facilities with the highest proportions of Black and Hispanic clientele demonstrated the lowest predicted probabilities of offering comprehensive and integrated services. Our findings offer context around upstream factors that may, in part, drive treatment disparities. We orient our findings around frameworks of structural racism and inequities in mental healthcare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental health treatment outcomes are disproportionately worse among underrepresented racial/ethnic minority groups (SAMHSA Center for Mental Health Services, 2001). Mental health services and epidemiologic literature has focused largely on disparities in healthcare utilization, with a majority of research focused on individual-level predictors of success such as age, gender, attitudes and readiness, and symptom severity (Bucher, Suzuki, & Samuel, 2019; Cross et al., 2022; Green et al., 2020). For example, Black and Hispanic individuals with mental health diagnoses are less likely than White individuals to initiate treatment (Le Cook, Trinh, Li, Shu-Yeu Hou, & Progovac, 2017; Le Cook et al., 2014). Social and environmental determinants of health outside of the treatment setting have also been shown to be strong influences on mental health and treatment outcomes (Alegria, NeMoyer, Bague, Wang, & Alvarez, 2018). While treatment use and individual predictors of treatment outcomes are important pieces of the overall story of disparities in mental health services, there remains a dearth of national research investigating the upstream causes of racial disparities in access to appropriate mental health treatment facilities.
All mental health treatment is not equal. Whether a facility offers comprehensive, integrated, and/or co-located services is an indicator of the overall structural clinical environment that likely affects multiple treatment endpoints. Co-located ancillary and physical health services have been shown to improve health among mental health treatment clients (Annamalai, Staeheli, Cole, & Steiner, 2018; Pirraglia et al., 2012), but no national epidemiologic studies have reported on the pace of service integration or whether emerging trends in integration are distributed equally across mental health facilities. The extent to which mental health treatment facilities are expanding the breadth of services offered may depend on the socioeconomic status and the racial/ethnic composition of their clientele. People typically receive healthcare where they live, and healthcare services are generally more limited, under-resourced, and more strained in communities that are predominately Black, Hispanic, or low income (Agurs-Collins et al., 2019; Artiga et al., 2020; Chan et al., 2020; Perry Crear et al., 2021). Consequently, there is a need to look beyond individual-level characteristics and explore upstream barriers to treatment access and ultimately successful treatment outcomes.
Our approach to investigating disparities in mental health systems is underpinned by Link and Phelan’s Fundamental Causes Theory (Link & Phelan, 1995; Phelan et al., 2010), which provides a framework for addressing the upstream and systematic factors that create health disparities. Recognizing and measuring downstream disparities in mental health treatment outcomes is an important piece of the narrative, including research findings that Black patients are more likely to terminate treatment early (Delphin-Rittmon et al., 2015; Lester et al., 2010; Olfson et al., 2009). However, long-term and sustainable solutions to reducing health and healthcare disparities must address higher-level systems of wealth and power. For example, structural racism is defined by the National Institutes of Health as “the macro-level conditions (e.g. residential segregation and institutional policies) that limit opportunities, resources, power and well-being of individuals and populations based on race/ethnicity and other statuses” (National Institutes of Health, 2022). These conditions are fundamental causes of inequities in health through the perpetuation of policies and practices that deny comprehensive health resources to minority and low-income communities while enhancing access in privileged White communities (Gee & Hicken, 2021; Phelan & Link, 2015). Our study aims to provide additional context around structural determinants in mental health treatment by investigating whether the quality of services is conditional on the racial/ethnic composition of a given treatment facility. We hypothesized that facilities with the least comprehensive services would serve higher concentrations of Black and Hispanic patients. Importantly, we chose to investigate a wide range of possible ancillary services offered in mental health treatment settings to approximate the comprehensiveness of a facility’s services. The motivation behind selecting diverse service types – from smoking cessation counseling to crisis intervention teams – was to highlight a common thread of disparities across a broad range of services, regardless of which specific service is under study. Such a service-agnostic approach is useful when focusing attention on the disparities without delving into the specific implications or merits of one service type over another. Taken together, commonalities in the direction and size of racial/ethnic differences across service types were the central to our research findings.
Methods
Data Source and Sample
We used cross-sectional data from the 2020 National Mental Health Services Survey (N-MHSS) to identify a range of characteristics of specialty outpatient treatment facilities in the US. N-MHSS is planned and directed by the Center for Behavioral Health Statistics and Quality, which is housed within the Substance Abuse and Mental Health Services Administration. In brief, N-MHSS includes data on characteristics of all known public and private facilities in the US that provide specialty mental health treatment, defined by SAMHSA as any facility or entity that provides mental health treatment services to people with mental illness. Administrative representatives from each facility completed an annual survey about services provided. In 2020, the response rate among facilities eligible to participate was 89% (Substance Abuse and Mental Health Services Administration, 2020). This study was a secondary analysis of publicly available administrative data describing characteristics of mental health facilities. As such, no human subjects were involved in this study and no individual-level data was available or used.
N-MHSS collects aggregate demographic information about treatment clientele demographics on even years. Respondents are asked about the racial/ethnic composition of their clientele by reporting either the number or percentage of clients in each racial/ethnic group, but not both. Although more facilities opted to report the raw number of clients, we used the percentage of clients in each racial/ethnic group as our primary predictor because the total facility size (denominator) is integrated into the pre-calculated percentage estimate. Moreover, counting the number of clients in each racial/ethnic group is likely an indication of the overall facility size and fails to accurately capture the racial/ethnic distribution of a facility’s patient population. There is no way to accurately derive a racial/ethnic percentage using the raw frequency variable with N-MHSS data; as such, we opted to only include the facilities that reported percentages. Our final sample included 1,074 facilities that had complete data for all study variables, which was 22% of all 4,835 outpatient facilities included in the 2020 N-MHSS. We used chi-square tests to determine whether our sample of facilities (those that reported demographics as percentages) was statistically significantly different from the remaining facilities that were excluded from our analysis (those that reported demographics as raw frequencies in ranges). Nine out of 12 study outcomes were not significantly different between facilities included and excluded from our sample (p > 0.05; Table 1), suggesting that our analytic sample is broadly representative of outpatient facilities in N-MHSS and our results are generalizable to the wider population of outpatient mental health treatment facilities in the US.
Study Outcomes, Focal Predictors, and Covariates
Our study was designed to investigate the relationship between the distribution of racial/ethnic groups served by the facility and whether facilities offered a variety of multiple services, which we contextualized as indicators of more comprehensive and integrated mental health services. As such, we developed twelve separate models each with a different binary outcome to identify differences in the probability of each service being offered (yes/no). These outcomes were selected to assess racial/ethnic differences across a wide range of mental health service types, as the goal was not to investigate any one domain of mental health treatment but rather to showcase the breadth of possibilities. Our twelve outcomes included whether a mental health facility: (1) offers family and couple therapy; (2) offers family psychoeducation; (3) offers telehealth; (4) uses a sliding fee scale; (5) offers integrated dual disorders treatment; (6) offers suicide prevention services; (7) offers dialectical behavior therapy; (8) offers substance use treatment; (9) offers smoking/tobacco cessation counseling; (10) offers consumer-run peer support services; 11) offers eye movement desensitization and reprocessing (EDMR), and; 12) is accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF).
We considered three focal predictors in our models, each represented by three variables with pre-defined response options in the N-MHSS dataset. Specifically, we looked at the percentage of a facility’s clientele that was White, Black, and Hispanic (1–10%, 11–20%, 21–30%, 31–40%, 41–50%, 51–75%, and 76–100%). We also included several covariates in our models based on a priori understanding of factors related to our outcomes. Covariates drawn from the N-MHSS data included the facility owner type (private non-profit, private for-profit, or public agency or department) and whether the facility accepts Medicaid as payment for services (yes or no). We also considered three state-level variables sourced externally that described the state environment in which each facility was located, including whether the facility was located in a Medicaid expansion state (Henry J. Kaiser Family Foundation, 2020), the percentage of a state’s population living in a rural area (Iowa Community Indicators Program, 2020), and the percentage of a state’s population that is White (U.S. Census Bureau, 2020).
Analysis
We used summary statistics to describe the distribution of our outcomes and predictors, reporting frequencies, proportions, and means depending on the variable type. We further stratified each outcome by the proportion of each facility that was White, Black, and Hispanic. We used multiple logistic regression to model each study outcome, predicted by facility demographic estimates for racial/ethnic composition (percent White, Black, and Hispanic) and adjusted for covariates. We treated the seven race/ethnicity categories as linear (i.e., 1–10%, 11–20%, 21–30%, 31–40%, 41–50%, 51–75%, and 76–100%) as the ranges between each ordinal level are nearly equivalent and may be expressed as a quasi-linear approximation. This approach of using pre-defined ordered categorical bins as proxy indicators of a linear scale substantially facilitates interpretation of trends as the racial/ethnic composition of each facility changes. Several studies have discussed the appropriateness and usefulness of treating ordinal variables as continuous in regression-based models (Li, 2016; Rhemtulla et al., 2012; Robitzsch, 2020). Finally, to visualize the adjusted trends in health service availability and services integration, we used estimates generated from our logistic models to plot the predicted probability of each outcome (y-axis) across facility-level percentages of White, Black, and Hispanic clientele (x-axis).
The N-MHSS includes administrative, aggregate, facility-level data and does not include individual-level data. Analysis of such data is not defined as human subjects research under the Common Rule as described by the US Health and Human Services Office for Human Research Protections (U.S. Department of Health and Human Services, 2022). The authors report no known conflicts of interest. All authors certify responsibility for this manuscript.
Results
Our analytic sample included 1,074 outpatient mental health treatment facilities. The most common services and administrative offerings were family and couples therapy (88%), family psycho-education (78%), telehealth (77%), and offering a sliding fee scale (70%) (Table 2). Fewer than one-in-three facilities offered consumer-run peer support (31%), EDMR (23%), or had CARF accreditation (22%). Over a quarter of all facilities (27%) had more than 75% White clientele, while only 2% had more than 75% Black or Hispanic clientele. Hispanic clientele were the least represented group, with half of all treatment facilities (50%) having only 1–10% Hispanic clients, followed by 41% of treatment facilities having only 1–10% Black clients.
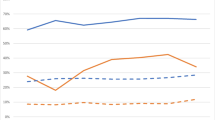
In our fully adjusted models (Table 3), higher proportions of Black clients were associated with facilities being less likely to offer family-based psycho-education (adjusted odds ratio [aOR] = 0.81, 95% confidence interval [CI] = 0.70–0.92, p < 0.01), suicide prevention (aOR = 0.87, 95% CI = 0.78–0.97, p = 0.01), consumer-run peer support (aOR = 0.86, 95% CI = 0.78–0.97, p < 0.01), and EDMR (aOR = 0.84, 95% CI = 0.74–0.95, p < 0.01). An increasing proportion of Hispanic clients was positively associated with offering family-based psycho-education (aOR = 1.21, 95% CI = 1.06–1.39, p < 0.01) and suicide prevention (aOR = 1.11, 95% CI = 1.00, 1.22, p = 0.04) and negatively associated with offering family and couples therapy (aOR = 0.87, 95% CI = 0.76–0.99, p = 0.03), smoking/tobacco cessation (aOR = 0.92, 95% CI = 0.84, 1.01, p = 0.06), and CARF accreditation (aOR = 0.84, 95% CI = 0.74–0.95, p < 0.01). Higher proportions of White clients were negatively associated with family psychoeducation (aOR = 0.82, 95% CI = 0.70–0.96, p = 0.01) and positively associated with offering a sliding scale fee (aOR = 1.14, 95% CI = 1.02–1.28, p = 0.02). Our adjusted results can also be visualized as predicted probabilities for each of the twelve outcomes (Fig. 1). In ten out of the 12 models, the predicted probability of offering a comprehensive service in a mental health treatment setting was lowest among facilities with high proportions of Black or Hispanic clientele (blue and green lines).
Predicted probability of offering a wide variety of services in specialty mental health treatment facilities (NMHSS 2020; N = 1,074 facilities). Note: Models adjusted for facility ownership, Medicaid payment acceptance, location in a Medicaid expansion state, the percentage of a state?s population that lives in a rural area, and the percentage of a state?s population that is White
Discussion
This study evaluated a national sample of mental health facilities in the US and found that for several of outcomes assessed, service availability decreased as the proportion of Black and Hispanic clients increased. There were no positive relationships between offered services with an increase in Black clientele. These findings help contextualize previous research that identified racial/ethnic differences in mental health treatment success (Delphin-Rittmon et al., 2015; Lester et al., 2010; Olfson et al., 2009) given our finding of reduced access to more comprehensive clinical services among Black and Hispanic clients. While the twelve measured outcomes may provide specific interpretations for the services themselves, they likely serve as a proxy for an overall clinic environment and the range of services offered as well as proxies for healthcare funding, health policy, or community investment, all of which are upstream factors affecting how people navigate healthcare and thrive in mental health treatment. Our study contributes to the mental health disparities literature, in part, by suggesting mechanisms for how and why disparities in mental health outcomes exist.
Our findings of less comprehensive mental health services for Black and Hispanic client populations align with the concept of structural determinism, articulated by Ford and Airhihenbuwa (2010) in their introduction to public health critical race methodology. In the context of our study, the structural nature of racialization in healthcare drives inequities and reinforces existing power structures. The systematic denial of robust and quality mental health care for communities of color – or conversely, the systematic construction of comprehensive mental healthcare for White and wealthy populations – serves to exacerbate morbidity among the former and thriving among the latter. Such morbidity and thriving may subsequently be passed down across generations and help sustain social stratification and further the racialization of group differences.
In our adjusted regression model, not all service types were significantly associated with the racial/ethnic composition of the clinic, and some relationships were in the opposite direction of our hypothesis. For example, offering family psychoeduction was more likely in clinics that had higher proportions of Hispanic clients. While definitions of family psychoeducation vary, it generally refers to the involvement of family members in the day-to-day management of a loved one’s mental health symptoms, financial management of mental health care, and addressing the stress often involved in caring for someone with a mental health disorder (Substance Abuse and Mental Health Services Administration, 2009). A lack of access to Spanish-speaking and bilingual providers is a major barrier to mental health treatment use among Hispanic adults (Pro et al., 2022; Rastogi et al., 2012), which is likely driving the continued decline in mental health treatment among Hispanic men in particular (Manuel, 2017). While language and culturally humble care are vital characteristics of evidence-based family psychoeducation programs (Substance Abuse and Mental Health Services Administration, 2009), professional Spanish language interpreter services are not always reimbursed or available across healthcare settings (Showstack, Guzman, Chesser, & Keene Woods, 2018), resulting in family members often stepping in as informal medical interpreters (Ginde, Clark, & Camargo, 2009). The pre-existing necessity of family involvement may aid in the success of family psychoeduction among Hispanic families. However, family psychoeducation in Hispanic populations is not without challenges, as participants have noted the competing elements of strong Hispanic family ties (familismo) and stigma towards mental illness by family members (Hackethal et al., 2013).
We noted several other strong associations with increased Black clientele in our adjusted models, including declines in facilities offering suicide prevention services as the proportion of Black mental health clients increased. Nationally, age-adjusted suicide rates increased by 30% among Black individuals between 2014 and 2019, and by 47% among Black youth specifically (Ramchand, Gordon, & Pearson, 2021). Mental health service use is universally low among adolescents at risk for suicide (Wu, Katic, Liu, Fan, & Fuller, 2010). Furthermore, Black adolescents are less likely than their White counterparts to receive suicide prevention services or consult with a mental health professional before their suicide attempt (Freedenthal, 2007). Importantly, in a study validating prediction models in a national sample, Coley and colleagues (2021) found that the rate for suicide within 90 days of a visit to an outpatient mental health facility was lowest among Black individuals. These findings suggest that mental health services may have a strong protective effect for Black clients in particular. Our study is aligned with others who have found disproportionately low access to suicide prevention services among Black populations, while also providing support for the strengthening suicide prevention services in clinics that predominately serve Black clients.
We also found that the availability of peer support services decreased as the proportion of Black clients increased. Peer support models vary, but generally peer support workers are people who have been successful in their own recovery process and help others navigate similar situations through understanding, respect, and mutual empowerment (Substance Abuse and Mental Health Services Administration, 2022). Peer support services have been shown to improve a range of recovery indicators (Chinman et al., 2014). In one systematic review of peer support in behavioral health, the authors concluded that the evidence was strong enough to call for peer support to be embedded into routine mental health and addiction care (Hameed Shalaby & Agapong, 2020). In two additional systematic reviews, peer support demonstrated effectiveness at improving psychosocial outcomes like hope, recovery, and empowerment, while showing mixed or modest results for other clinical outcomes (Lloyd-Evans et al., 2014; White et al., 2020). Our study contributes a novel finding to the peer support literature, as there is a dearth of national studies that address racial/ethnic disparities in peer support availability within outpatient mental health settings. Zemore and colleagues (2021) conducted a literature review investigating a related intervention of self-help group attendance for people with substance use problems. The authors arrived at a similar conclusion that racial/ethnic disparities research in this domain was sparse, inconsistent, and dated. Further research is needed to better understand peer support outcomes for Black mental health clients, as well as identifying strategies to bolster components of the peer support model that are relevant to Black communities.
Finally, while offering a sliding scale fee was one of the most common services offered, it was only positively associated with increasing proportions of White clientele (1–10% White, predicted probability = 63%; 75–100% White, predicted probability = 72%). Sliding scale fees are used to calculate a fee for services based on a person’s income, and were broadly developed in the US to act as a safety-net payment structure for people in need of treatment but who cannot afford care at the standard rates (Smith, Kuramoto-Crawford, & Lynch, 2016). The value and importance of sliding scale fees was codified in the Fees and Business Practices section (A.10.c) of the Code of Ethics in the Affordable Care Act in 2014, which stated that, “In establishing fees for professional counseling services, counselors consider the financial status of clients and locality. If a counselor’s usual fees create undue hardship for the client, the counselor may adjust fees, when legally permissible, or assist the client in locating comparable, affordable services” (American Counseling Association, 2014). The high cost for services and medications has been reported as disproportionately affecting lower mental health services use among Black and Hispanic individuals (Bogue-Kawaii, Williams, & MacNear, 2017; Dridges, Andrews III, & Deen, 2012; Mojtabai, 2005), which may be an indicator of a higher need for sliding scale fees in treatment facilities located in minoritized communities. However, we identified an increase in sliding scale fees only in relation to increases in White clientele, which supports our hypothesis of fewer comprehensive services for clients in predominately Black and Hispanic facilities. Several reports have identified the prevalence of mental health disorders to be highest among White individuals (McGuire & Miranda, 2008; Miranda et al., 2008; Panchal et al., 2022). At the same time, morbidity and mortality from mental health- and substance abuse-related diseases have increased most drastically among White populations, referred to as an epidemic of despair (Brignone et al., 2020; Case & Deaton, 2015; Stein et al., 2017). In this environment of growing poverty and debt and the diminishing accumulation of wealth among many White Americans, lowering the cost of mental healthcare through sliding scale fees is a positive reaction to a growing need. At the same time, our study identified that offering sliding scale fees is not changing for facilities that cater to Black and Hispanic majorities. Such notable differences in sliding scale access is a clear disparity that negatively affects Black and Hispanic groups who have experienced generational poverty, discrimination, and structural racism in healthcare settings for centuries (Yearby, 2020; Yearby et al., 2022). Such a swift response by the mental healthcare system to address the growing financial burden of mental health services may be duly applauded, while simultaneously acknowledging that changes in payment structures were only recently driven by an emerging need for White clients – it is rare when such consensus is reached in response to behavioral health burdens unique to communities of color.
Limitations
Our sample included outpatient mental health treatment facilities that opted to report patient demographics as percentages rather than raw numbers, which was 22% of all outpatient facilities in the 2020 N-MHSS dataset. For facilities that reported raw numbers for both client demographics and the total number of clients, N-MHSS provides pre-constructed variables that represent ranges, not the raw number. Thus it is not possible to derive the percentage of clients from these categories. For example, one may not calculate a proportion of Black clients using categories such as 51–75 Black clients as the numerator and 101–250 total clients as the denominator. We considered calculating the most conservative estimate by using the smallest Black frequency (51) divided by the largest total facility population (250), which equates to an estimate of 20% Black clients in a facility. However, equally likely would be 75 divided by 101, which is 74% Black clients. With such a drastic gap between calculations we were not confident that this approach would approximate the real percentage of Black clients in a facility. Despite the limitation, we identified that the facilities included in our sample were not statistically different than those excluded on nine out of the 12 outcomes tested. Thus, we are confident that this novel application of national data is useful in drawing generalizable conclusions about racial/ethnic disparities in mental health treatment in the US.
Conclusion
We identified differences in the availability of a wide range of integrated, comprehensive mental health services among treatment clinics with varying proportions of White, Hispanic, and Black clientele. Broadly, facilities with higher proportions of Black and Hispanic clients offered fewer services. We conceptualized the treatment environment as an upstream factor that likely influences racial disparities in treatment outcomes. Clinical and administrative resources that are availed or withheld from certain groups shape the trajectory of treatment success and recovery. Funding and mental health policy must support multilevel interventions that dismantle structural racism and promote equitable distribution of comprehensive, evidence-based care.
Data Availability
This study did not use human subjects or individual-level data. Only publicly available, aggregate, administrative, facility-level data was used.
The N-MHSS dataset is free and publicly available through SAMHSA (https://www.datafiles.samhsa.gov/dataset/national-mental-health-services-survey-2020-n-mhss-2020-ds0001).
References
Agurs-Collins, T., Persky, S., Paskett, E., Barkin, S., Meissner, H., Nansel, T., Arteaga, S. S., Zhang, X., Das, R., & Farhat, T. (2019). Designing and assessing multilevel interventions to improve minority health and reduce health disparities. American Journal of Public Health, 109(S1), S86–S93.
Alegria, M., NeMoyer, A., Bague, I., Wang, Y., & Alvarez, K. (2018). Social determinants of mental health: Where we are and where we need to go. Current Psychiatry Reports, 20(95), 1–13.
American Counseling Association (2014). 2014 ACA Code of Ethics: As Approved by the ACA Governing Council. American Counseling Association. Alexandria, VA. Sourced from: <https://www.counseling.org/Resources/aca-code-of-ethics.pdf.
Annamalai, A., Staeheli, M., Cole, R., & Steiner, J. (2018). Establishing an integrated health care clinic in a community mental health center: Lessons learned. Psychiatric Quarterly, 89, 169–181.
Artiga, S., Orgera, K., & Pham, O. (2020). Disparities in Health and Health Care: Five Key Questions and Answers. Henry J. Kaiser Family Foundation. Issue Brief. March 2020. Sourced from: <https://www.careinnovations.org/wp-content/uploads/Issue-Brief-Disparities-in-Health-and-Health-Care-Five-Key-Questions-and-Answers.pdf.
Bogue-Kawaii, B., Williams, N., & MacNear, K. (2017). Mental health care access and treatment utilization in african american communities: An integrative care framework. Ingenta Connect, 13(2), 11–29.
Brignone, E., George, D., Sinoway, L., Katz, C., Sauder, C., Murray, A., Gladden, R., & Kraschnewski, J. (2020). Trends in the diagnosis of diseases of despair in the United States, 2009–2018: A retrospective cohort study. British Medical Journal Open, 10, e037679.
Bucher, M., Suzuki, T., & Samuel, D. (2019). A meta-analytic review of personality traits and their associations with mental health treatment outcomes. Clinical Psychology Review, 70, 51–63.
Case, A., & Deaton, A. (2015). Rising morbidity and mortality in midlife among white non-hispanic Americans in the 21st Century. PNAS - Proceedings of the National Academy of Sciences of the United States of America, 112(49), 15078–15083.
Chan, K., Parikh, M., Thorpe, R., & Gaskin, D. (2020). Health care disparities in race-ethnic minority communities and populations: Does the availability of health care providers play a role? Journal of Racial and Ethnic Health Disparities, 7, 539–549.
Chinman, M., George, P., Dougherty, R., Daniels, A., Shoma Ghose, S., Swift, A., & Delphin-Rittmon, M. (2014). Peer support services for individuals with serious mental illnesses: Assessing the evidence. Psychiatric Services, 65(4), 429–441.
Coley, R., Johnson, E., Simon, G., Cruz, M., & Shortreed, S. (2021). Racial/ethnic disparities in the performance of prediction models for death by suicide after mental health visits. JAMA Psychiatry, 78(7), 1–9.
Cross, S., Karin, E., Staples, L., Bisby, M., Ryan, K., Duke, G., Nielssen, O., Kayrouz, R., Fisher, A., Dear, B. F., & Titov, N. (2022). Factors associated with treatment uptake, completion, and subsequent symptom improvement in a national digital mental health service. Internet Interventions, 27, 100506.
Delphin-Rittmon, M., Flanagan, E., Andres-Hyman, R., Ortiz, J., Amer, M., & Davidson, L. (2015). Racial-ethnic differences in access, diagnosis, and outcomes in public-sector inpatient mental health treatment. Psychological Services, 12(2), 158–166.
Dridges, A., Andrews, I. I. I., A., & Deen, T. (2012). Mental health needs and service utilization by hispanic immigrants residing in mid-Southern United States. Journal of Transcultural Nursing, 23(4), 359–368.
Ford, C., & Airhihenbuwa, C. (2010). The public health critical race methodology: Praxis for antiracism research. Social Science & Medicine, 71, 1390–1398.
Freedenthal, S. (2007). Racial disparities in mental health service use by adolescents who thought about or attempted suicide. Suicide and Life-Threatening Behavior, 37(1), 22–34.
Gee, G., & Hicken, M. (2021). Structural racism: The rules and regulations of inequity. Ethnicity & Disease, 31(Supplement 1), 293–300.
Ginde, A., Clark, S., & Camargo, C. (2009). Language barriers among patients in Boston emergency departments: Use of medical interpreters after passage of interpreter legislation. Journal of Immigrant and Minority Health, 11(6), 527–530.
Green, J., McLaughlin, K., Fillbrunn, M., Fukuda, M., Jackson, J., Kessler, R., Sadikova, E., Sampson, N. A., Vilsaint, C., Williams, D. R., Cruz-Gonzalez, M., & Alegria, M. (2020). Barriers to mental health service use and predictors of treatment drop out: Racial/ethnic variation in a population-based study. Administration and Policy in Mental Health and Mental Health Services Research, 47, 606–616.
Hackethal, V., Spiegel, S., Lewis-Fernandez, R., Kealey, E., Salerno, A., & Finnerty, M. (2013). Towards a cultural adaptation of family psychoeducation: Findings from three latino focus groups. Community Mental Health Journal, 49, 587–598.
Hameed Shalaby, R., & Agapong, V. (2020). Peer support in mental health: Literature review. JMIR Mental Health, 7(6), e15572.
Henry, J., & Kaiser Family Foundation. (2020). Status of State Medicaid Expansion Decisions: Interactive Map. Medicaid. Nov 02, 2020. Retrieved from: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/.
Iowa Community Indicators Program (2020). Urban Percentage of the Population for States, Historical. Iowa State University. Sourced from: <https://www.icip.iastate.edu/tables/population/urban-pct-states.
Le Cook, B., Trinh, N., Li, Z., Shu-Yeu Hou, S., & Progovac, A. (2017). Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatric Services, 68(1), 9–16.
Le Cook, B., Zuvekas, S., Carson, N., Wayne, G., Vesper, A., & McGuire, T. (2014). Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Services Research, 49(1), 206–229.
Lester, K., Artz, C., Resick, P., & Young-Xu, Y. (2010). Impact of race on early treatment termination and outcomes in posttraumatic stress disorder treatment. Journal of Counseling and Clinical Psychology, 78(4), 480–489.
Li, C. (2016). The performance of ML, DWLS, and ULS estimation with robust corrections in structural equation models with ordinal variables. Psychological Methods, 21(3), 369–387.
Link, B., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior Special No:80–94.
Lloyd-Evans, B., Mayo-Wilson, E., Harrison, B., Istead, H., Brown, E., Pilling, S., & Kendall, T. (2014). A systematic review and meta-analysis of randomised controlled trials of peer support for people with servere mental illness. Bmc Psychiatry, 14(39), 1–12.
Manuel, J. (2017). Racial/ethnic and gender disparities in health care use and access. Health Services Research, 53(3), 1407–1429.
McGuire, T., & Miranda, J. (2008). New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs, 27(2).
Miranda, J., McGuire, T., Williams, D., & Wang, P. (2008). Mental health in context of health disparities. The American Journal of Psychiatry, 165(9), 1102–1108.
Mojtabai, R. (2005). Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States: 1997–2002. American Journal of Public Health, 95(11), 2009–2014.
National Institutes of Health (2022). Structural Racism and Discrimination. Ending Structural Racism - Understanding Health Disparities Series. National Institute of Minority Health and Health Disparities. Sourced from: <https://nimhd.nih.gov/resources/understanding-health-disparities/srd.html.
Olfson, M., Mojtabai, R., Sampson, N., Hwang, I., Druss, B., Wang, P., Wells, K. B., Pincus, H. A., & Kessler, R. (2009). Dropout from outpatient mental health care in the United States. Psychiatric Services, 60(7), 898–907.
Panchal, N., Saunders, H., & Ndugga, N. (2022). Five Key Findings on Mental Health and Substance Use Disorders by Race/Ethnicity. Race Equity and Health Policy. Kaiser Family Foundation. San Francisco, CA. Sourced from: <https://www.kff.org/racial-equity-and-health-policy/issue-brief/five-key-findings-on-mental-health-and-substance-use-disorders-by-race-ethnicity/.
Perry Crear, J., de Araujo, C., Lewis Johnson, R., McLemore, T., Neilson, M., E., & Wallace, M. (2021). Social and structural determinants of health inequities in maternal health. Journal of Women’s Health, 30(2), 230–235.
Phelan, J., & Link, B. (2015). Is racism a fundamental cause of inequalities in health. Annual Review of Sociology, 41, 311–330.
Phelan, J., Link, B., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior, 51, S28–S40.
Pirraglia, P., Rowland, E., Wu, W., Friedmann, P., O’Toole, T., Cohen, L., & Taveira, T. (2012). Benefits of primary care clinic co-located and integrated in a mental health setting for veterans with serious mental illness. Preventing Chronic Disease, 9, E51.
Pro, G., Brown, C., Rojo, M., Patel, J., Flax, C., & Haynes, T. (2022). Downward national trends in mental health treatment offered in Spanish: State differences by proportion of hispanic residents. Psychiatric Services, E-publication ahead of print, 3. May 2022.
Ramchand, R., Gordon, J., & Pearson, J. (2021). Trends in suicide rates by race and ethnicity in the United States. JAMA Open Network, 4(5), e2111563.
Rastogi, M., Massey-Hastings, N., & Wieling, E. (2012). Barriers to seeking mental health services in the Latino/a community: A qualitative analysis. Journal of Systemic Therapies, 31(4), 1–17.
Rhemtulla, M., Brosseau-Liard, P., & Savalei, V. (2012). When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychological Methods, 17(3), 354–373.
Robitzsch, A. (2020). Why ordinal variables can (almost) always be treated as continuous variables: Clarifying assumptions of robust continuous and ordinal factor analysis estimation methods. Frontiers in Education, 5(589965).
SAMHSA Center for Mental Health Services. (2001). Mental health: Culture, race, and ethnicity - A supplement to mental health: A report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services.
Showstack, R., Guzman, K., Chesser, A., & Keene Woods, N. (2018). Improving latino health equity through spanish language interpreter advocacy in Kansas. Hispanic Health Care International, 17(1), 18–22.
Smith, K., Kuramoto-Crawford, J., & Lynch, S. (2016). Availability of Payment Assistance for Mental Health Services in U.S. Mental Health Treatment Facilities. The CBHSQ Report - Short Report, March 23, 2016 Substance Abuse and Mental Health Servcies Administration. Rockville, MD. US Health and Human Services.
Stein, E., Gennuso, K., Ugboaja, D., & Remington, P. (2017). The epidemic of despair among White Americans: Trends in the leading causes of premature death, 1999–2015. American Journal of Public Health, 107(10), 1541–1547.
Substance Abuse and Mental Health Services Administration (2009). Family Psychoeducation: Getting Started with Evidence-Based Practices. HHS Pub. No. SMA-09-4422, Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.
Substance Abuse and Mental Health Services Administration. (2020). National Mental Health Services Survey (N-MHSS): 2020. Data on Mental Health Treatment Facilities. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Substance Abuse and Mental Health Services Administration (2022). Peer Support Workers for those in Recovery. Bringing Recovery Supports to Scale: Technical Assistance Center Strategy. Substance Abuse and Mental Health Services Administration, Department of Health and Human Services. Sourced from: <https://www.samhsa.gov/brss-tacs/recovery-support-tools/peers.
U.S. Census Bureau (2020). ACS Demographic and Housing Estimates. The American Community Survey. 2020 ACS 5-Year Estimates Data Profiles. Table DP05. Sourced from: <https://data.census.gov/cedsci/table?t=White&g=0100000US%240400000&y=2020&tid=ACSDP5Y2020.DP05&tp=true>.
U.S. Department of Health and Human Services (2022). What is human subjects research? HHS Office for Human Subjects Research Protections. Online Education. Sourced from: <https://www.hhs.gov/ohrp/education-and-outreach/online-education/human-research-protection-training/lesson-2-what-is-human-subjects-research/index.html.
White, S., Foster, R., Marks, J., Morshead, R., Goldsmith, L., Barlow, S., Sin, J., & Gillard, S. (2020). The effectiveness of one-to-one peer support in mental health services: A systematic review and meta-analysis. Bmc Psychiatry, 20(534), 1–20.
Wu, P., Katic, B., Liu, X., Fan, B., & Fuller, C. (2010). Mental health service use among suicidal adolescents: Findings from a U.S. national community survey. Psychiatric Services, 61(1), 17–24.
Yearby, R. (2020). Structural racism and health disparities: Reconfiguring the social determinants of health framework to include the root causes. The Journal of Law Medicine & Ethics, 48(3), 518–526.
Yearby, R., Clark, B., & Figueroa, J. (2022). Structural racism in historical and modern US health care policy. Health Affairs, 41(2).
Zemore, S., Gilbert, P., Pindeo, M., Tsutsumi, S., McGeough, B., & Dickerson, D. (2021). Racial/ethnic disparities in mutual help group participation for substance use problems. Alcohol Research: Current Reviews, 41(1), 1–21.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
GP conceived of the study, analyzed the data, and drafted the first manuscript version. CB assisted with data analysis and provided substantive feedback on all manuscript sections. OJ, BM, and NZ provided substantive feedback on all manuscript sections and provided expert insight around interpreting study results.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pro, G., Brown, C., Johnson, O. et al. Comprehensive and Integrated Services in Specialty Mental Health Treatment Facilities in the US: Differences by the Racial/Ethnic Composition of the Facility’s Clientele, 2020. Community Ment Health J 60, 272–282 (2024). https://doi.org/10.1007/s10597-023-01168-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-023-01168-0