Abstract
While mental health (MH) services are expected to support client recovery, very little is known about services provided by MH teams in relation to this goal. This study explored relationships between a comprehensive collection of team effectiveness variables and the perspectives of MH professionals regarding the recovery orientation of their teams. A model developed by path analysis revealed eight team-related variables that were significantly and positively associated with recovery-oriented teams: primary care versus specialized MH services; greater proportions of clients with severe mental disorders or with suicide ideation on caseloads; knowledge sharing and knowledge production among team members; team climate; work role performance; and trust in coworkers. Results underline the importance of building knowledge and professional competence on MH teams, and the need for a positive team climate that offers flexibility and innovation for addressing the complex needs of people in MH recovery living in the community.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
First introduced by consumer-survivors, recovery may be described as living a satisfying, hopeful, and contributing life despite limitations caused by mental disorders (MD).1 Recovery among service users is strongly associated with positive outcomes, such as quality of life, continuity of care, and met needs.2,3,4,–5 The recovery vision has driven international mental health (MH) policy and system reforms in developed countries for over two decades.6,7,8,9,10,–11 Recovery-oriented systems ultimately aim to promote MH services and practices that better support the personal recovery of individuals with MDs.12,13 To this end, the innovative 2013 Australian national recovery framework established a series of core principles around organizational commitment and workforce development.11 A particularly important contribution of this document was recognition of the need to equip, train, and support MH teams in strengthening the recovery orientation of their service delivery and practices. MH professionals increasingly work as members of multidisciplinary teams, which have been described as a hallmark of recovery-oriented service delivery.14,15 The Australian framework also recommended team-level assessments of recovery orientation using standardized measures.
In Canada, Quebec stands out as the first jurisdiction to introduce recovery into MH policy in the context of the 2005–2015 MH reform,16 which equated recovery with personal empowerment, community integration, and the inclusion of MH clients in working partnerships. Coinciding with a major restructuring of the Quebec healthcare system, the MH reform aimed to strengthen the functioning of clinical teams, particularly within primary care services, through the integration of highly skilled and experienced MH professionals from specialized psychiatric institutes or general hospitals. Furthermore, the addition of new staff as well as organizational links and partnerships were encouraged among local service organizations and networks.17 Shared care initiatives, notably the introduction of respondent psychiatrists to support primary care MH teams, were also implemented.18
In addition, the Quebec reform introduced a number of clinical best practices and system-level elements that have been identified in various studies as promising for client recovery. Collaborative relationships between clients and MH professionals, individualized treatment planning, and better continuity of care were encouraged.19,20,–21 Clinical best practices were also introduced, such as cognitive behavioral therapy, motivational interviewing, strength-based approaches, illness self-management, and stepped care.22 Other key features of the new recovery-enhancing MH system for Quebec included the development of integrated service networks, training for MH professionals, more adequate financing, and the use of standardized assessment tools.18,23,24,25,26,–27 Yet, how to reconcile client-driven recovery with traditional clinical treatment protocols continued to represent a fundamental challenge for MH service delivery.27
Certain models originating in other healthcare fields have been used to describe categories of variables associated with team work and team effectiveness. According to the Input-Mediator-Output-Input (IMOI) model from organizational psychology, individual characteristics (e.g., age, gender, type of profession) are viewed as nested within the team context (e.g., size, setting, composition), and, in turn, within the organizational environment (e.g., structure, culture, interactions with other teams or organizations).28,29 All of these variables are considered inputs that influence other mediating variables within one of two categories: team processes (i.e., conditions affecting team work such as knowledge sharing and collaboration) or emergent states (i.e., motivating factors such as team climate and trust); both of which directly affect the ability of team members to work together and produce the desired outcomes (outputs).29
Based on the IMOI model, other studies have found that perceived recovery orientation in services was influenced by individual socio-professional characteristics, including higher age, greater professional experience, and more advanced education.30,31,–32 Personal optimism among MH professionals was another associated variable.33 Significant differences in perceptions of recovery orientation were also identified for different professional groups.33,34 Considering that personal recovery among MH services users was strongly associated with the presence of strong or enduring therapeutic relationships between MH professionals and clients, it is possible that employment status (full-time vs. part-time) may influence the perceived recovery orientation of services, directly or indirectly, due to such mediator effects.32 An association between the gender of MH professionals and recovery orientation has yet to be identified.
Concerning team context, client profile has emerged in the literature as a variable of interest; that is, MH professionals working with clients affected by serious MDs (e.g., schizophrenia, bipolar disorder) rated the recovery orientation of their organization more positively than those whose clients had more moderate MDs (e.g., anxiety, depression).32 A strong working alliance between MH professionals and clients, paired with a more directive intervention style, also related to better recovery orientation.32 By contrast, emotional exhaustion and depersonalization (i.e., negative views toward clients) among MH professionals were associated with negative perceptions of recovery orientation.35
Other associated variables involved work settings: MH professionals working in community-based services rated the recovery orientation of their services higher than those working in hospitals.33 The only known study to focus on recovery orientation at the team level found that the type of team made a difference in provider perceptions: that is, early intervention teams were rated more recovery-oriented than adult MH teams.36 Moreover, this study identified a strong association between team recovery orientation and more positive perceptions of personal recovery among the clients served.36 Additionally, it is possible that recovery best practices and standardized assessment tools may have an influence on recovery orientation in services; these practices and tools have been identified as promising for client recovery, while favoring the acquisition of new knowledge and skills among MH professionals and improving team effectiveness.22,37,38
The influence of organizational environment on recovery orientation needs to be further investigated. Research has identified one association for a single type of organizational culture: that is, the more adhocratic (i.e., flexible and innovative) the organization, the more recovery oriented.30 Furthermore, as better integration of MH services has been identified in association with both higher satisfaction among MH professionals and team effectiveness,39 it is possible that the use of integration strategies, as well as the frequency of interaction between MH teams and organizations, may also directly or indirectly influence recovery orientation.
Regarding team processes, studies reveal that the implementation of recovery-oriented services was associated with both knowledge production and knowledge sharing.15,22 Result-oriented leadership and larger organizational budgets, recognized as dimensions of team support, were also associated with recovery orientation.30 Finally, a recovery orientation may be associated with team autonomy, team collaboration, involvement in decisions, and with team reflexivity, as well as the capacity of teams to adapt their objectives, strategies, and processes to current or anticipated circumstances.40
Regarding team emergent states, recovery-oriented services were associated with higher job satisfaction among MH professionals as well as multifocal identification, which is viewed as the potential of professionals to identify with both their team and profession.35,41,42 Research has also identified the importance of work role performance, or the capacity of teams to produce effective outcomes.2,43 Similar to the concept of trust within teams, which has been identified as a protective factor against burnout and job dissatisfaction among MH professionals, other emergent states variables may provide possible associations with recovery-oriented services.44 Moreover, the implementation of recovery-oriented services would likely benefit from a good team climate; although this association has not been tested.
While highly effective healthcare teams are important for clients, professionals, and healthcare systems alike, available studies concerned with healthcare teams have investigated very few related variables.45,46,–47 Studies on the recovery orientation of teams (e.g., team processes and emergent states) are even more sparse, despite the known importance of team recovery orientation for personal recovery among clients with MDs. Furthermore, studies have yet to conduct analyses using standardized measures. In short, little, if any, empirical understanding exists regarding how team effectiveness, or the organizational environment of teams, may be associated with recovery orientation. Finally, no known study has assessed relationships between recovery orientation and possible mediating variables (i.e., team processes and emergent states). A better knowledge of these relationships would be particularly important in the context of current MH reforms, which have had considerable impact on MH practices and the structure and dynamics of MH teams in Quebec and elsewhere.
The present study unfolded in the context of a larger evaluation of the 2005–2015 Quebec MH reform. Considering that this reform implemented a number of tools, practices, and strategies geared toward enhancing the recovery orientation of services, the Quebec MH service system represents an interesting context for evaluating variables in connection with recovery that have not often been studied. Based on the IMOI model that brings together variables related to individual characteristics, team context, organizational environment, team processes, and team emergent states, the objectives of the study were (1) to comprehensively identify variables related to the recovery orientation of MH teams based on the perceptions of MH professionals using path analysis and (2) to assess covariance among the independent variables introduced into the analysis.
Methods
Study design, sample, and data collection
This study used a cross-sectional and multisite design. Respondents were selected from four local health service networks that varied in terms of geographic area (three urban, one semi-urban) and presence or absence of a psychiatric hospital. The selected networks included diverse practice settings such as hospital units, outpatient clinics, and primary care. Territorial populations ranged from 135,000 to 300,000 inhabitants. Respondents were MH professionals and managers working in public primary care or specialized MH services, either inpatient or outpatient settings. They had to be working in clinical teams with at least three members representing two or more disciplines. All MH professionals who met these eligibility criteria, and their managers, were invited to participate in the study.
Data collection took place between October 2013 and June 2014. A questionnaire consisting of 21 standardized scales and six separate questions on socio-professional characteristics was developed for MH professionals. Fourteen of these scales were used in the present study. The questionnaire took approximately 45 min to complete. A second questionnaire eliciting additional information on team settings, client profiles, the time allocated to treatment, use of recovery best practices, and use of standardized assessment tools was developed for team managers, who retrieved this information from administrative databases. While managers were asked to provide administrative information, they did not evaluate recovery orientation. A 12-member research advisory committee that included representatives from each of the four selected networks provided oversight for the study and facilitated access to the research sites. The research ethics board of a MH university institute approved the multisite study protocol.
Conceptual framework, variables, and instruments
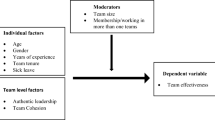
A conceptual framework was developed for the study based on the IMOI model and was used to measure variables associated with recovery orientation of team, the dependent variable.28 The independent variables were organized according to the five-block IMOI conceptual framework: namely, professional characteristics, team context, organizational environment, team processes, and team emergent states (see Fig. 1).
The dependent variable, recovery orientation of team (RSA-team), was measured with the provider version of the Recovery Self-Assessment Scale (RSA) developed by O’Connell et al., which is the most widely used scale for assessing recovery orientation of MH services.48,49 This 32-item instrument includes six domains of recovery orientation related to the performance of MH programs and staff: promoting life goals, consumer involvement, diversity of treatment options, consumer choice, individually tailored services, and inviting environment, with scoring on a 5-point Likert scale. The RSA has demonstrated good internal consistency, test-retest reliability, and convergent and discriminant validity.33,48,50,51,–52 Items on the RSA were slightly adapted so that the responses of MH professionals would reflect recovery orientation at the level of their respective teams. This is shown in the following statements: “the members of my team believe in the ability of program participants to recover” and “members of my team regularly attend training sessions on cultural competency”.
As for the independent variables, data on professional characteristics were provided by the professional questionnaire that included: age, gender, type of profession (medical, psycho-social, and others), years of professional practice, seniority on team (years), and employment status (full/part time). Team context data came from the manager questionnaire and included: client profiles (e.g., severe MDs, suicidal ideation), time allocated to treatment, use of recovery best practices (e.g., cognitive behavioral therapy, motivational interviewing), and standardized assessment tools (e.g., screening tools for MDs, client satisfaction evaluation tools). Recovery best practices as well as standardized assessment tools were measured with 5-point Likert scales and were merged into a global score.
Moreover, data on organizational environment were also obtained from the manager questionnaire, and included frequency of interactions (e.g., with psychiatric/general hospital teams, community organizations) and integration strategies (e.g., liaison officers, service agreements). The two organizational-level variables were also measured with 5-point Likert scales and merged into global scores. Team processes were measured with eight standardized instruments, while team emergent states were measured with five others; all data was provided by the MH professional questionnaire. Due to the large number of variables included in the study, we used all available brief versions of the standardized instruments; they represent the instruments most frequently used by researchers to assess team work and team effectiveness. All standardized instruments were translated and validated in French, except for the measure of team collaboration, which was originally developed in French. The standardized instruments are described in Table 1, and reliability measures are provided.
Statistical analyses
The data were screened for missing values, univariate outliers, and normality assumptions (skewness and kurtosis). Univariate, bivariate, and multivariate analyses were carried out. Univariate analyses included frequency distributions, percentages for categorical variables, and central tendency measures for continuous variables (mean values and standard deviations). Bivariate analyses included comparison analyses and interclass correlations. Using one-way ANOVA, tests were performed for differences in RSA-team scores among the three types of work setting as follows: MH teams in primary care vs. outpatient vs. inpatient services. The same test was used to compare local networks with a psychiatric hospital (n = 3) vs. a general hospital (n = 1). Interclass correlation was also calculated to account for the nested nature of the variables, testing for homogeneity within teams and heterogeneity between teams, in association with RSA-team scores. A clustering into nine types of teams (e.g., hospital, day hospital, assertive community treatment teams), with an average of 35 respondents each (range, 30 to 55), was calculated using maximum likelihood ratio with random effects.
Multivariate analysis consisted of a path analysis based on variables from the IMOI model and a linear regression model that assessed variables associated with RSA-team. The path analysis was built step-by-step, guided by model quality parameters: chi-square statistics, degrees of freedom, and goodness-of-fit statistics. The latter relied notably on the root mean square residual (RMR), the comparative fit index (CFI), the root mean square error of approximation (RMSEA), the p value close fit (PCLOSE), and the Akaike information criterion (AIC). The p value of the chi-square statistics reflects agreement between the path analysis model and the data. The null hypothesis would indicate that the model fits the data, and the chi-square p value should be non-significant (p > 0.05).62 The RMR is the amount by which sample variances and covariances differ from their estimates: the smaller the RMR (i.e., as close to zero as possible), the better, as it indicates a perfect fit.
In addition, the CFI is the ratio of the model being estimated to the baseline model, based on discrepancy and degrees of freedom.63 A CFI close to 1 indicates a very good fit. The RMSEA reflects the residuals in the model estimates; an RMSEA of 0.05 or less indicates a close fit.64 The PCLOSE is the p value from the assessment of the null hypothesis confirming that the RMSEA is not greater than an alpha value of 0.05. A non-significant PCLOSE (p > 0.05) indicates a close fit. The AIC, as a comparative criterion of fit, takes its meaning from a comparison of different models, and reflects the balance between model fit and parsimony. Parsimony is violated when unnecessary parameters are retained in the model. As such, the AIC indicates improvement in model fit and parsimony from one model to another.65 When comparing different models, a smaller AIC indicates a better model.
Results
Description of the sample
Of the 466 MH professionals invited to participate in the study, 315 respondents were included in the sample, resulting in a 68% response rate. There were no significant differences between respondent and non-respondent MH professionals on the distributions for gender (χ2 (1, N = 466) = 0.03; p = 0.87) or type of team (χ2 (1, N = 466) = 0.79; p = 0.68). Managers from the 49 teams (clustered into nine types of team) were also invited to the study. Forty-one managers participated, which produced an 84% response rate. Comparison analyses revealed no differences between respondent and non-respondent managers in terms of gender (Pearson chi-square = 0.966; df = 1; Fisher exact test 2-sided: p = 0.663) or type of team (Pearson chi-square = 1.861; df = 1; Fisher exact test 2-sided: p = 0.245].
Respondent characteristics
The mean age of MH professionals was 43 years, and majority (69%) were female. Thirty-two percent worked in primary care, 56% in outpatient services, and 12% in inpatient services. The average seniority on teams was 3 years. The mean age for managers was 44 years, and 71% were female, 37% worked in primary care, 46% in outpatient services, and 17% in inpatient services. The average seniority among managers was four years. Other information on respondent and team characteristics is presented in Table 2.
Bivariate analyses
Results for comparison analyses among the three work settings revealed a single significant difference: MH professionals working in primary care had significantly higher scores on RSA-team than MH professionals working in outpatient and inpatient services combined (p = 0.009; p = 0.050). No significant differences were found between the responses of MH professionals working in outpatient vs. inpatient services (p = 0.145) on RSA-team. Comparison analyses among the three local networks with a psychiatric hospital vs. the fourth with the general hospital also yielded a non-significant difference (one-way ANOVA: F = 0.071; p = 0.976), which allowed researchers to run a path analysis integrating data from the four networks. Interclass correlation for homogeneity within teams, and heterogeneity between teams, on all variables in association with RSA-team was found to be elevated (84%); while the effect of clustering, based on the maximum likelihood ratio with random effects, was not significant (Wald z = 1.377; p = 168). This suggests that the nested nature of the data, and clustering, did not bring about any added value to the individual-level model. Finally, RSA-team was found to be normally distributed (skewness, − 0.512; kurtosis, 1.270) with a mean of 3.6 and a range from 1.5 to 4.9 (SD = 0.49).
Path analysis
The path analysis model (see Fig. 2) produced a nearly perfect fit with the data. AMOS achieved a minimum chi-square of 23.499, df = 16, p = 0.101; these results indicated that departure of the data from the model was non-significant. The goodness-of-fit estimates were as follows: RMR = 0.538; CFI, 0.994; RMSEA, 0.039; PCLOSE, 0.688. Single-headed arrows represent associations between the exogenous (or independent) variables and endogenous (or dependent) variables. Double-headed arrows represent the magnitude of mutual effect, or covariance, between two exogenous (or independent) variables.
Regarding standardized regression weights (see Table 3), eight variables were significantly associated with RSA-team. In the team context block, primary care was associated with RSA-team as compared with specialized MH services. Two client profiles also emerged as significant: having greater proportions of clients with severe MDs or suicidal ideation were associated with higher RSA-team scores. In the team processes block, knowledge sharing and knowledge production were positively associated with RSA-team. Under emergent states, work role performance, team climate, and trust in coworkers were also positively associated with RSA-team.
Three other variables had an indirect, but significant and positive association with RSA-team: knowledge integration; reflexivity (team processes); and multifocal identification, a measure of professional and team identification (team emergent states). The association between knowledge integration and RSA-team was mediated by knowledge production; whereas, the association between reflexivity and RSA-team was mediated by knowledge sharing. Finally, the association between multifocal identification and RSA-team was mediated by trust in coworkers. Table 4 presents estimates of the variance explained by the four endogenous (or dependent) variables: knowledge production (41%), trust in coworkers (15%), knowledge sharing (7%), and RSA-team (43%).
Discussion
This study tested a broad range of variables across the five conceptual blocks of the IMOI framework.28 The path analysis model revealed eight significant variables ranging across team characteristics (n = 3), team context (n = 2), and team emergent states (n = 3). The two remaining blocks, professional characteristics and organizational environment, did not produce significant findings. In the case of professional characteristics, this was likely due to the extent and novelty of the team effectiveness variables introduced, which may have diminished the significance of socio-demographic variables. Likewise, the variables under organizational environment may have been too far removed to produce significant results.
Results for the global RSA-team score in this study (mean = 3.6; SD = 0.49) were comparable with those obtained by O’Connell et al., authors of the RSA; the mean global score for MH providers in their study was 3.87 (SD = 0.62).48 RSA scores in the present study were also very close to provider scores in Salyers et al., where the total mean score for hospital staff was 3.30 (SD = 0.54), and for community staff, 3.63 (SD = 0.48).33 Moreover, RSA scores in this study were nearly identical with the total mean scores for clinicians in Leamy et al. (3.59; SD = .005), who also used the RSA to evaluate team recovery orientation.36
Regarding the two team context variables (block 2), the finding that teams working in primary care were more recovery oriented than those in specialized MH services confirms a central recovery principle that MH services should be anchored in the community and is also supported by research suggesting that primary care provides a more effective, and normalizing, context for delivering MH care to people with serious MDs.66,67,–68 A 7-year follow-up study of people with severe MDs living in a rural area reported higher respondent satisfaction with local community services than with hospital inpatient services. Even in areas with well-staffed community MH clinics, respondents were more satisfied with their general practitioners, with whom they enjoyed close and collaborative relationships.69 Integrating MH services into primary care enhanced the quality of services and promoted recovery for MH clients, particularly those at elevated risk for comorbid physical and substance use disorders; access to care increased as did client satisfaction.70
The finding that caseloads with greater proportions of clients with severe MDs were associated with higher RSA-team scores corresponds to findings reported in Osborn et al.32 This finding is unsurprising, as clinical approaches to recovery-oriented MH care, and the recovery philosophy itself, have historically been geared toward the complex needs of people with serious and recurring MDs. What may explain the other positive link between having more suicidal clients in caseloads and a higher RSA-team score was the substantial support available to MH professionals with suicidal clients through the 24-h crisis services established under the Quebec MH reform. Working relationships between MH teams and community-based crisis centers in Quebec were found to be particularly strong.18 The availability of around-the-clock crisis services has also been identified as an important prerequisite for recovery among suicidal clients.71 Risk of suicidal mortality was identified as particularly prevalent among clients with serious MDs.72
Regarding the two team processes variables (block 3), the significance of knowledge production was underscored in the Australian national MH guidelines, where knowledge production was designated as a key organizing principle.73 Similarly, knowledge production was viewed as more important than treatment change for recovery transformation in a large MH organization.15 Knowledge sharing, the other team processes variable, is illustrated by MH “trialogues,” or discussion groups involving MH professionals, clients, and families, which are particularly widespread in German-speaking countries.74 Slade et al. identified MH trialogues as one of ten empirically validated interventions that support recovery.22 These findings underline the importance of knowledge-building activities within, and among, multidisciplinary MH teams for meeting complex needs of MH clients.
Concerning the three associated variables under team emergent states (block 4), work role performance (e.g., individual/team proficiency), and, more specifically, professional competence and experience, may enhance RSA-team.43 This finding corresponds to earlier research where MH professionals who were older, with more education and years of professional experience, rated their services as more recovery oriented.31 Specific recovery training or the integration of a recovery specialist was also associated with greater recovery orientation.24,25,50,75 Support for innovation and task orientation constitute two key dimensions of the second variable, team climate; these variables were identified with team creativity in a 30-year meta-analysis.61,76 An innovative climate, also characteristic of “adhocratic” organizations, provides much-needed flexibility for the implementation of recovery approaches, particularly when supported by result-based leadership.30
Finally, regarding trust in coworkers, two studies revealed that mutual trust in MH teams was a significant protective factor against emotional exhaustion, depersonalization, and burnout among MH professionals; all of which are professional liabilities that were also negatively associated with recovery-oriented services.35,44 The importance of trust between professionals and clients in studies of the therapeutic relationship,77 and the finding that professional/client working alliance was positively associated with recovery orientation,32 support the finding in this study that trust in coworkers was associated with RSA-team.
Concerning the three endogenous variables in the model, knowledge production mediated the association between knowledge integration and RSA-team. Knowledge integration is a frequent topic in recovery policy and research, particularly in relation to training programs for service providers.24,78,79 Similarly, the relationship between team reflexivity and RSA-team was mediated by knowledge sharing, both identified as key elements for recovery-oriented workforce development.73 Finally, the relationship between multifocal identification and RSA-team was mediated by trust in coworkers. Multifocal identification, a measure of personal identification to the team and one’s profession, was identified in a systematic review as an important facilitator for implementing recovery approaches into MH services.42,80 Finally, it should be noted that, while recovery best practices included in the conceptual model were tested for associations with RSA-team, none of these practices emerged as significant in the path analysis model, contrary to expectation. This outcome was likely due to insufficient implementation of recovery best practices by MH teams during the initial stages of the Quebec MH reform.
Certain limitations in this research should be acknowledged. First, as a cross-sectional study, causal inferences about the findings cannot be made. Second, the teams had to be clustered by team types to perform interclass correlations, as some teams had insufficient numbers of respondents for this analysis. Third, the findings may not reflect the perceptions of MH professionals in other regions of Quebec, or other MH systems. Further studies are needed to test variables from the IMOI model in relation to RSA-team in order to further confirm, and build upon, the results of this study. Fourth, this study did not include information concerning prior experiences with recovery among MH professionals. Presumably, those with firsthand experience of successful recovery among their clients would be more receptive to working from a recovery orientation. Finally, the perceptions of clients served by MH teams were not sought. The client perspective, particularly assessments of their personal recovery in relation to RSA-team, and comparative professional-client evaluations of these variables, are important topics for future research.
Implications for Behavioral Health
This study tested multiple variables based on the IMOI model, addressing a major gap in the recovery literature around the importance of team effectiveness for recovery orientation. Findings from the study suggest the potential importance of knowledge-based activities (knowledge integration, knowledge production, and knowledge sharing) for recovery-oriented teams. Building knowledge, in turn, suggests that competence and flexibility may enhance professional/team work, and should be developed. Team climate was also significant in the model, particularly in terms of providing a climate of innovation for advancing recovery. Trust in coworkers mediated identification with the team among MH professionals, somewhat similar to the role of trust in strong therapeutic relationships between MH professionals and their clients. The findings from this study align with the literature in suggesting that the integration of MH services into primary care may help create more recovery-oriented MH service delivery. It may be useful for decision-makers in behavioral health services to focus on creating positive working environments within MH teams, while promoting knowledge-building activities and recovery training among multidisciplinary MH professionals, in order to transform MH services in ways that better address the needs of clients in recovery.
References
Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal. 1993;16(4):11–23.
Fleury MJ, Grenier G, Bamvita JM. Associated and mediating variables related to quality of life among service users with mental disorders. Quality of Life Research. 2017:1–12.
Ho WWN, Chiu MYL, Lo WTL, et al. Recovery components as determinants of the health-related quality of life among patients with schizophrenia: structural equation modelling analysis. Australian and New Zealand Journal of Psychiatry. 2010;44(1):71–84.
Bowersox NW, Lai Z, Kilbourne AM. Integrated care, recovery-consistent care features, and quality of life for patients with serious mental illness. Psychiatric Services. 2012;63(11):1142–1145.
Lloyd C, King R, Moore L. Subjective and objective indicators of recovery in severe mental illness: a cross-sectional study. The International Journal of Social Psychiatry. 2010;56(3):220–229.
Adams N, Daniels A, Compagni A. International pathways to mental health transformation. International Journal of Mental Health. 2009;38(1):30–45.
Le Boutillier C, Leamy M, Bird VJ, et al. What does recovery mean in practice? a qualitative analysis of international recovery-oriented practice guidance. Psychiatric Services. 2011;62(12):1470–1476.
The New Zealand Mental Health Commission. Blueprint for mental health services in New Zealand. How things need to be. Wellington: Mental Health Commission; 1998.
Ramon S, Shera WES, Healy B, et al. The rediscovered concept of recovery in mental illness. International Journal of Mental Health. 2009;38(2):106–126.
Mental Health Commission. Changing directions, changing lives. The mental health strategy for Canada. Calgary: Mental Health Commission of Canada, 2012.
Australian Health Ministers' Advisory Council. A national framework for recovery-oriented mental health services: a guide for practitioners and providers. Canberra: Commonwealth of Australia, 2013.
Deegan PE. Recovery as a self-directed process of healing and transformation. In: C Brown (Ed). Recovery and wellness: models of hope and empowerment for people with mental illness. New York: The Haworth Press, Inc., 2001, pp. 5–21.
Davidson L, Tondora J, O'Connell MJ, et al. Creating a recovery-oriented system of behavioral health care: moving from concept to reality. Psychiatric Rehabilitation Journal. 2007;31(1):23–31.
Allot P, Loganathan L. Discovering hope for recovery from a british perspective: a review of a sample of recovery literature, implications for practice and systems change. Birmingham: West Midlands Partnerships for Mental Health, 2002.
Malinovsky I, Lehrer P, Silverstein SM, et al. An empirical evaluation of recovery transformation at a large community psychiatric rehabilitation organization. Psychological Services. 2013;10(4):428–441.
Ministère de la Santé et des Services Sociaux (MSSS). Plan D’action en Santé Mentale 2005–2010: La Force des Liens. Québec: MSSS, 2005.
Fleury MJ, Grenier G, Vallée C, et al. Implementation of the Quebec Mental Health Reform (2005-2015). BMC Health Services Research. 2016;16(12):228–240.
Fleury MJ, Grenier G, Robitaille D. Implementation of the consultation-liaison model in Quebec and its impact on primary care providers. Mental Health in Family Medicine. 2016;12:228–240.
Matthias MS, Fukui S, Kukla M, et al. Consumer and relationship factors associated with shared decision making in mental health consultations. Psychiatric Services. 2014;65(12):1488–1491.
Stanhope V, Ingoglia C, Schmelter B, et al. Impact of person-centered planning and collaborative documentation on treatment adherence. Psychiatric Services. 2013;64(1):76–79.
Sweeney A, Davies J, McLaren S, et al. Defining continuity of care from the perspectives of mental health service users and professionals: an exploratory, comparative study. Health Expectations. 2016;19(4):973–987.
Slade M, Amering M, Farkas M, et al. Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry. 2014;13(1):12–20.
Fleury MJ. The implementation of integrated networks of mental health services in quebec: context of introduction, state of implementation, and the views of general practitioners. Sante Publique. 2011;23 Suppl 6:S155–159.
Salgado JD, Deane FP, Crowe TP, et al. Hope and improvements in mental health service providers' recovery attitudes following training. Journal of Mental Health. 2010;19(3):243–248.
Tsai J, Salyers MP, McGuire AB. A cross-sectional study of recovery training and staff attitudes in four community mental health centers. Psychosocial Rehabilitation Journal. 2011;34(3):186–193.
Salkever D, Gibbons B, Ran X. Do comprehensive, coordinated, recovery-oriented services alter the pattern of use of treatment services? Mental health treatment study impacts on SSDI beneficiaries’ use of inpatient, emergency, and crisis services. Journal of Behavioral Health Services & Research. 2014;41(4):434–446.
Slade M. Measuring recovery in mental health services. Israel Journal of Psychiatry and Related Sciences. 2010;47(3):206–212.
Ilgen DR, Hollenbeck JR, Johnson M, et al. Teams in organizations: from input-process-output models to IMOI models. Annual Review of Psychology. 2005;56:517–543.
Mathieu J, Maynard TM, Rapp T, et al. Team effectiveness 1997-2007: a review of recent advancements and a glimpse into the future. Journal of Management. 2008;34(3):410–476.
Brown TT, Mahoney CB, Adams N, et al. What predicts recovery orientation in county departments of mental health? A pilot study. Administration and Policy in Mental Health. 2010;37(5):388–398.
McLoughlin KA, Fitzpatrick JJ. Self-reports of recovery-oriented practices of mental health nurses in state mental health institutes: development of a measure. Issues in Mental Health Nursing. 2008;29(10):1051–1065.
Osborn LA, Stein CH. Mental health care providers’ views of their work with consumers and their reports of recovery-orientation, job satisfaction, and personal growth. Community Mental Health Journal. 2015;52(7):757–766.
Salyers MP, Tsai J, Stultz TA. Measuring recovery orientation in a hospital setting. Psychiatric Rehabilitation Journal. 2007;31(2):131–137.
Leddy-Stacy M, Stefanovics E, Rosenheck R. Veteran and clinician perceptions of recovery and stigma at a veterans affairs medical center. Psychiatric Rehabilitation Journal. 2016;39(2):105–111.
Kraus SW, Stein CH. Recovery-oriented services for individuals with mental illness and case managers’ experience of professional burnout. Community Mental Health Journal. 2013;49(1):7–13.
Leamy M, Clarke E, Le Boutillier C, et al. Recovery practice in community mental health teams: national survey. British Journal of Psychiatry. 2016;209(4):340–346.
Kozlowski SWJ, Bell B. Work groups and teams in organizations. In: IB Weiner, NW Schmitt, S Highhouse (Eds). Handbook of Psychology, Industrial and Organizational Psychology, Volume 12. London: Wiley, 2003, pp. 333–375.
Buljac-Samardzic M, Dekker-van Doorn CM, van Wijngaarden JDH, et al. Interventions to improve team effectiveness: a systematic review. Health Policy. 2010;94(3):183–195.
Longpré C, Dubois CA, Nguemeleu ET. Associations between level of services integration and nurses’ workplace well-being. BMC Nursing. 2014;13(1):50.
West MA. Reflexivity and work group effectiveness. a conceptual integration. In: M West (Ed). Handbook of Work Group Psychology. Chilchester: Wiley, 1996, pp. 555–579.
Le Boutillier C, Slade M, Lawrence V, et al. Competing Priorities: Staff Perspectives on Supporting Recovery. Administration and Policy in Mental Health and Mental Health Services Research. 2015;42(4):429–438.
Van Dick R, Wagner U, Stellmacher J, et al. The utility of a broader conceptualization of organizational identification: which aspects really matter? Journal of Occupational and Organizational Psychology. 2004;77(2):171–191.
Griffin MA, Neal A, Parker SK. A new model of work role performance: positive behavior in uncertain and interdependent contexts. Academy of Management Journal. 2007;50(2):327–347.
Johnson H, Worthington R, Gredecki N, et al. The relationship between trust in work colleagues, impact of boundary violations, and burnout among staff within a forensic psychiatric service. Journal of Forensic Practice. 2016;18(1):64–75.
Mickan SM. Evaluating the effectiveness of health care teams. Australian Health Review. 2005;29(2):211–217.
Oandasan I, Baker GR, Barker K, et al. Teamwork in healthcare: promoting effective teamwork in healthcare in Canada. Ottawa: Canadian Health Services Research Foundation, 2006.
Mickan SM, Rodger SA. Effective health care teams: a model of six characteristics developed from shared perceptions. Journal of Interprofessional Care. 2005;19(4):358–370.
O'Connell M, Tondora J, Croog G, et al. From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatric Rehabilitation Journal. 2005;28(4):378–386.
Williams J, Leamy M, Bird V, et al. Measures of the recovery orientation of mental health services: systematic review. Social Psychiatry and Psychiatric Epidemiology. 2012;47(11):1827–1835.
Kymalainen JA, Henze KT, Deluca M, et al. Are we there yet? the four-year impact of a VA fellowship program on the recovery orientation of rehabilitation programs. Psychosocial Rehabilitation Journal. 2010;33(4):320–327.
Rosenberg D, Svedberg P, Schon UK. Establishing a recovery orientation in mental health services: evaluating the recovery self-assessment (RSA) in a Swedish context. Psychosocial Rehabilitation Journal. 2015;38(4):328–335.
Ye S, Pan JY, Wong DFK, et al. Cross-validation of mental health recovery measures in a Hong Kong Chinese sample. Research on Social Work Practice. 2013;23(3):311–325.
Spreitzer GM. Social structural characteristics of psychological empowerment. Academy of Management Journal. 1996;39(2):483–504.
Campion MA, Papper EM, Medsker GJ. Relations between work team characteristics and effectiveness: a replication and extension. Personnel Psychology. 1996;49(2):429–452.
De Dreu CKW. Cooperative outcome interdependence, task reflexivity, and team effectiveness: a motivated information processing perspective. Journal of Applied Psychology. 2007;92(3):628–638.
Bock GW, Zmud RW, Kim YG, et al. Behavioral intention formation in knowledge sharing: examining the roles of extrinsic motivators, social-psychological forces, and organizational climate. MIS Quarterly. 2005;29(1):87–111.
Song M, Xie J. Does innovativeness moderate the relationship between cross-functional integration and product performance? Journal of International Marketing. 2000;8(4):61–89.
Chiocchio F, Grenier S, O'Neill A, et al. The effects of collaboration on performance: a multilevel validation in project teams. International Journal of Project Organisation and Management. 2012;4(1):1–37.
Spector PE. Measurement of human service staff satisfaction: development of the job satisfaction survey. American Journal of Community Psychology. 1985;13(6):693–713.
Simons TL, Peterson RS. Task conflict and relationship conflict in top management teams: the pivotal role of intragroup trust. American Journal of Community Psychology. 2000;85(1):102–111.
Anderson NR, West MA. Measuring climate for work group innovation: development and validation of the team climate inventory. Journal of Organizational Behavior. 1998;19(3):235–258.
Bollen KA. Structural equations with latent variables. New York: Wiley, 1989.
Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246.
Browne MW, Cudeck R. Alternative ways of assessing model fit. In: KA Bollen, JS Long (Eds). Testing Structural Equation Models. Newbury Park: Sage, 1993, pp. 136–162.
Akaike H. Factor analysis and AIC. Psychometrika. 1987;52(3):317–332.
Substance Abuse and Mental Health Services Administration. Guiding principles and elements of recovery-oriented systems of care: what do we know from the research? Rockville: Department of Health and Human Services, 2009.
Campbell DG, Bonner LM, Bolkan CR, et al. Stigma predicts treatment preferences and care engagement among veterans affairs primary care patients with depression. Annals of Behavioral Medicine. 2016;50(4):533–544.
Dale H, Lee A. Behavioural health consultants in integrated primary care teams: a model for future care. BMC Family Practice. 2016;17:97.
Ruud T, Aarre TF, Boeskov B, et al. Satisfaction with primary care and mental health care among individuals with severe mental illness in a rural area: a seven-year follow-up study of a clinical cohort. International Journal of Mental Health Systems. 2016;10:33.
Ede V, Okafor M, Kinuthia R, et al. An examination of perceptions in integrated care practice. Community Mental Health Journal. 2015;51(8):949–961.
Foster T. Suicide prevention as a prerequisite for recovery from severe mental illness. International Journal of Psychiatry in Medicine. 2013;46(1):15–25.
Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–160.
Australian Health Ministers’ Advisory Council. A national framework for recovery-oriented mental health services. guide for practitioners and providers. Canberra: Department of Health and Aging, 2013.
Amering M, Mikus M, Steffen S. Recovery in Austria: mental health trialogue. International Review of Psychiatry. 2012;24(1):11–18.
Tsai J, Salyers MP. Recovery orientation in hospital and community settings. Journal of Behavioral Health Services & Research. 2010;37(3):385–399.
Hülsheger UR, Anderson N, Salgado JF. Team-level predictors of innovation at work: a comprehensive meta-analysis spanning three decades of research. Journal of Applied Psychology. 2009;94(5):1128–1145.
Stanhope V, Solomon P. Getting to the heart of recovery: methods for studying recovery and their implications for evidence-based practice. British Journal of Social Work. 2008;38(5):885–899.
Wilrycx G, Croon M, Van den Broek A, et al. Evaluation of a recovery-oriented care training program for mental healthcare professionals: effects on mental health consumer outcomes. International Journal of Social Psychiatry. 2015;61(2):164–173.
Mak WW, Lam BY, Yau SS. Recovery knowledge and recovery-oriented services in Hong Kong. Psychiatric Services. 2010;61(11):1164.
Le Boutillier C, Chevalier A, Lawrence V, et al. Staff understanding of recovery-orientated mental health practice: a systematic review and narrative synthesis. Implementation Science. 2015;10:87.
Acknowledgements
The researchers would like to thank the individuals who participated in this research, in particular François Chiocchio, Catherine Vallée, and Guy Grenier for their valuable assistance.
Funding
This study was funded by the Fonds de la recherche en santé du Québec (FRSQ), grant number 22367, and the Prends soin de toi Program; the researchers gratefully acknowledge the support of these agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fleury, MJ., Sabetti, J. & Bamvita, JM. Modeling Relationships Involving Perceived Recovery Orientation of Mental Health Teams Among Quebec Mental Health Professionals. J Behav Health Serv Res 46, 434–449 (2019). https://doi.org/10.1007/s11414-018-9591-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-018-9591-1