Abstract
Age-related deterioration of condylar cartilage is an etiological factor in temporomandibular joint-osteoarthritis (TMJ-OA). However, its underlying mechanism remains unknown. Therefore, we examined age-related changes and the relationship between mTOR signaling and primary cilia in condylar cartilage to determine the intrinsic mechanisms of age-related TMJ-OA. Age-related morphological changes were analyzed using micro-computed tomography and safranin O-stained histological samples of the mandibular condyle of C57BL/6J mice (up to 78 weeks old). Immunohistochemistry was used to assess the activity of mTOR signaling, primary cilia frequency, and Golgi size of condylar chondrocytes. Four-week-old mice receiving an 11-week series of intraperitoneal injections of rapamycin, a potent mTOR signaling inhibitor, were used for the histological evaluation of the condylar cartilage. The condylar cartilage demonstrated an age-related reduction in cartilage area, including chondrocyte size, cell density, and cell size distribution. The Golgi size, primary cilia frequency, and mTOR signaling also decreased with age. Rapamycin injections resulted in both diminished cartilage area and cell size, resembling the phenotypes observed in aged mice. Rapamycin-injected mice also exhibited a smaller Golgi size and lower primary cilia frequency in condylar cartilage. We demonstrated that a loss of primary cilia due to a decline in mTOR signaling was correlated with age-related deteriorations in condylar cartilage. Our findings provide new insights into the tissue homeostasis of condylar cartilage, contributing to understanding the etiology of age-related TMJ-OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a prevalent degenerative joint disorder characterized by the progressive breakdown of articular cartilage and subsequent changes in the underlying bone [1]. While OA can affect various joints in the body, its impact on the temporomandibular joint (TMJ), a crucial component of the masticatory system, has gained increasing attention [2]. Patients with TMJ-OA commonly experience pain, joint noise, and limited jaw movement, which have serious impacts on their oral health and quality of life [3]. With age, the TMJ undergoes a series of morphological and functional alterations that may contribute to the development and progression of the TMJ-OA [4,5,6]. The intricate relationship between aging and TMJ-OA is multifaceted and influenced by a range of extrinsic and intrinsic factors. Extrinsic factors include mechanical stress, trauma, and functional habits, whereas intrinsic factors include genetic predisposition, hormonal changes, and systemic conditions [7,8,9]. However, it remains unclear how aging affects the development of TMJ-OA.
Proteoglycans are major components of the extracellular matrix (ECM) and are essential for maintaining the integrity and functionality of the condylar cartilage [10, 11]. The glycosaminoglycan chains within proteoglycans have a high affinity for water molecules, creating a hydrated gel-like environment within the ECM [12]. However, proteoglycan production and cartilage thickness decrease in the condylar cartilage of aged mice [6, 13, 14] and senescence-accelerated mice [15, 16]. Further, alterations in proteoglycan content, structure, and metabolism result in decreased water retention capacity against elastic and shear pressures [17, 18]. Consequently, the condylar cartilage becomes more susceptible to mechanical stress with age, predisposing individuals to TMJ-OA. Thus, understanding the intricate mechanisms underlying age-related deterioration in the condylar cartilage is crucial for early diagnosis and identification of potential therapeutic targets for TMJ-OA.
The primary cilium is an antenna-like organelle that coordinates multiple signaling pathways to the cells and plays a crucial role in tissue development and homeostasis [19,20,21]. Disruption of primary cilia via mutations in the genes encoding the ciliary proteins, involving cilia assembly or function, results in a wide spectrum of pathophysiological conditions termed as “ciliopathies” [21, 22]. Failure of primary cilia affects various cellular processes, including chondrocyte differentiation [23] and ECM production [20, 24, 25]. Deletion or mutation of ciliary genes, such as intraflagellar transport (Ift) 80 [26] and Tg737/Ift88,[27], have been reported to reduce proteoglycan production and type X collagen expression in the articular cartilage. Moreover, we have recently reported that condylar cartilage-specific deletion of primary cilia using Ift20fl/fl: NG2-CreER mice results in decreased proteoglycan production and thinning of the mandibular condylar cartilage [28], indicating the essential roles of primary cilia in maintaining condylar cartilage tissue.
The mechanistic/mammalian target of rapamycin (mTOR) is a serine/threonine kinase that plays a crucial role in cellular processes such as protein synthesis, autophagy, and cell growth [29]. Previous studies have shown that mTOR plays a crucial role in primary cilia [30], maintaining its length [31,32,33] and frequency [34]. Moreover, mTOR has been shown to participate in chondrocyte hypertrophy and proliferation [35]. Therefore, we hypothesized that the age-related deterioration of condylar cartilage is caused by the loss of primary cilia due to the reduction in mTOR signaling. The present study aimed to elucidate the potential intrinsic regulation of age-related deterioration in condylar cartilage by investigating age-related changes and their correlation with mTOR signaling and primary cilia in mouse condylar cartilage.
Materials and methods
Animals
The animal experimental protocols were approved by the Animal Care and Experimentation Committee of Niigata University (SA00959). C57BL/6J male mice (4, 5, 15, 26, 52, and 78 weeks old) were obtained from Charles River Laboratories Japan (Yokohama, Japan). Mice were housed in air-conditioned rooms at an ambient temperature of 23 ± 2 °C and a relative humidity of 55–65%. They were exposed to an artificial light–dark cycle of 12:12 h. At each week of age, five mice were used for histological analysis. Sample size was determined using resource equation methods [36]. Samples were fixed with 4% paraformaldehyde for 24 h.
Micro-computed tomography analysis
Micro-computed tomography (μCT) images were scanned with a CT system (CosmoScanGX; Rigaku Corporation, Tokyo, Japan) at 90 kV energy and 88 μA intensity. The slices were reconstructed to produce 2D and 3D images. From the 3D images, only the mandibular condylar head was extracted for bone mineral density measurement. Bone mineral density was measured using Analyze12.0 (AnalyzeDirect Inc., Overland Park, KS, USA).
Histological analysis and immunofluorescence staining
Mandibular condyle samples were dissected and decalcified with 10% ethylenediaminetetraacetic acid for four weeks at 4 °C and embedded in paraffin or Tissue-Tek O.C.T. compound (Sakura Finetek, Tokyo, Japan). Frontal sections of condylar cartilage were prepared for histological analysis. The orientation of histologic specimens was standardized by the anatomic location of the mandibular condyle and the gonial angle on the same section [28].
Paraffin sections were stained with safranin O and Fast Green. The cartilage area was defined as the area enclosed by the surfaces of the mandibular condylar cartilage and the subchondral bone of the condyle. Safranin O-positive areas within this defined cartilage area were measured using ImageJ software. The number of chondrocytes was counted within the defined cartilage area, and the cell density was calculated by dividing the number of chondrocytes per μm2 of cartilage area. Cell size distribution was calculated by measuring the area of each chondrocyte within the cartilage area using ImageJ software and expressed as a percentage of the cell size range. Cryosections were used for immunofluorescence staining. The primary antibodies used were as follows: Acetylated tubulin (1:400, T6793; Sigma-Aldrich, St Louis, MO, USA), Gamma-tubulin (1:400, T5326; Sigma-Aldrich), GM130 (1:200, 610,822; BD Biosciences, Franklin Lakes, NJ, USA), and Phospho-S6 (1:400, 5364; Cell Signaling Technology, Danvers, MA, USA). The slides were analyzed with an Olympus FluoView FV1200 laser scanning confocal microscope (Olympus, Tokyo, Japan) using an FV10-ASW Viewer. The pS6-positive cell ratio was calculated as the number of pS6-positive chondrocytes to the total chondrocytes in the cartilage area. The primary cilia frequency was calculated as the number of acetylated tubulin-positive cells to the total chondrocytes in the cartilage area. Golgi size was determined by measuring the GM130-positive area of all chondrocytes in the cartilage area using ImageJ software.
Cell culture and immunocytochemistry
The mouse chondroprogenitor cell line ATDC5 cells (RIKEN Cell Bank, Tsukuba, Japan) were cultured in Dulbecco’s modified eagle medium (DMEM)/F-12 (11,765–054; Gibco, Thermo Fisher Scientific, Waltham, MA, USA) containing 5% fetal bovine serum (FBS; 10,270–098; Gibco), antibiotic–antimycotic 100 × (15,240,062; Thermo Fisher Scientific), and 1% insulin-transferrin-selenium (51,300–044; Gibco) at 37 °C in a humidified atmosphere of 5% CO2. The medium was changed every other day.
For the stimulation of mTOR signaling, ATDC5 cells were cultured at a density of 1.0 × 104 cells/cm2 in 6-well plates for 48 h. MHY1485 (Tokyo Chemical Industry, Tokyo, Japan) was reconstituted in dimethyl sulfoxide (DMSO) (FUJIFILM Wako Pure Chemical Co., Osaka, Japan). ATDC5 cells were starved in DMEM/F-12 medium containing 0.5% FBS for 24 h to induce ciliogenesis and then treated with 10 µM MHY1485 in culture medium or 0.1% DMSO as a control [37]. For the inhibition of mTOR signaling, ATDC5 cells were cultured at a density of 5.0 × 104 cells/cm2 in 6-well plates for 48 h. Rapamycin (R-5000; LC Laboratories, Woburn, MA, USA) was reconstituted in absolute ethanol at 20 mg/mL and diluted in a culture medium. ATDC5 cells were starved in DMEM/F-12 medium containing 0.5% FBS for 24 h to induce ciliogenesis and then treated with 0.1 μM rapamycin in culture medium or 0.01% ethanol as a vehicle [38].
After 48 h of the treatment, cells were fixed in 4% paraformaldehyde for 10 min and analyzed via immunocytochemistry. The primary antibodies used were as follows: acetylated tubulin (1:1,000), gamma-tubulin (1:1,000), and phospho-S6 (1:1,000). Samples were analyzed using an Olympus FluoView FV1200 laser scanning confocal microscope with an FV10-ASW Viewer. To determine the cell number, three fields of view per sample (n = 3) were randomly selected, and all cells within these fields were counted. The pS6-positive cell ratio was calculated as the number of pS6-positive chondrocytes divided by the total cells in the field. The primary cilia frequency was calculated as the number of acetylated tubulin-positive cells divided by the total number of cells in the field.
In vivo administration of an mTOR inhibitor
Twenty-four mice were randomly assigned to one of four groups. Six mice received intraperitoneal injections of rapamycin (8 mg/kg) every other day for either one or 11 weeks, starting at four weeks of age [39, 40]. The control group included six mice injected intraperitoneally with vehicle solution [phosphate buffered saline, 5% Tween 80 (Sigma-Aldrich), 5% polyethylene glycol-400 (FUJIFILM Wako Pure Chemical Co.)] following the same schedule as the rapamycin injection.
Statistical analysis
Data are expressed as mean ± SD. Statistical differences between groups were determined using Tukey’s test after analysis of variance or a two-tailed Student’s t-test. A p-value of less than 0.05 was considered statistically significant.
Results
Histological changes in mouse condylar cartilage with age
Micro-CT analysis of the mouse mandibular condyle revealed age-related changes in surface morphology changes (Fig. 1A). At five weeks of age, the condylar head exhibited a rough bone surface, which gradually became smoother. However, at 78 weeks of age, the condylar surface appeared irregular. Furthermore, the bone mineral density of the mandibular condyle increased with age, peaking at 26 weeks (Fig. 1B). Safranin O-stained histological samples (Fig. 1C) exhibited an age-dependent decline in cartilage area (Fig. 1D) and safranin O-positive area (Fig. 1E), indicating the abundance of proteoglycans. In addition, the cell density (Fig. 1F) and size (Fig. 1G) of the condylar cartilage decreased with age. Cells larger than 200 μm2 in size accounted for approximately 35% of the total chondrocytes at five weeks, but this proportion gradually decreased with age. At 52 and 78 weeks, cells smaller than 40 μm2 in size accounted for more than 50% of the total chondrocytes. These observations are consistent with previous studies reporting age-related deterioration changes in mouse condylar cartilage [6, 13, 14, 16].
Age-related alterations in primary cilia frequency and mTOR signaling in mouse condylar cartilage
As the age-related deterioration of mouse condylar cartilage was confirmed by histological observations, we subsequently analyzed the size of the Golgi apparatus, which reflects the activity of ECM production in the cells [41]. The GM130-positive area, representing the area of cis-Golgi, was well-developed in the hypertrophic layer of the condylar cartilage at five weeks (Fig. 2A). In accordance with the cell size (Fig. 1G), the GM130-positive area decreased with age (Fig. 2B). We also analyzed the age-related change of primary cilia frequency in the condylar cartilage (Fig. 2C, D). The proportion of ciliated chondrocytes was 38.9% at five weeks and decreased to 27.9% and 2.4% at 15 and 26 weeks, respectively.
Because mTOR signaling is involved in ciliogenesis [30,31,32,33,34] and chondrocyte hypertrophy [35], we analyzed the age-related change of mTOR signaling in condylar cartilage by assessing the expression of phosphorylated S6 kinase (pS6), a downstream target of mTOR signaling (Fig. 2E, F). Cells positive for pS6 were observed throughout the condylar cartilage at five weeks, whereas the ratio of pS6-positive cells decreased significantly at 26 weeks and further decreased with age. Our results demonstrate that age-related decreases in primary cilia frequency and mTOR signaling were observed concurrently in the condylar cartilage.
Manipulation of mTOR signaling affects primary cilia frequency in chondrocytes
To investigate the significance of mTOR signaling in the maintenance of primary cilia, we manipulated mTOR signaling and analyzed its effect on cilia frequency using a chondroprogenitor cell line (ATDC5). Treatment of ATDC5 cells with MHY1485, an activator of mTOR signaling, did not significantly affect cell number, confirming that the MHY1485 did not exhibit cytotoxicity at the concentration used (Fig. 3A, B). Activation of mTOR signaling by treatment with MHY1485 was confirmed by the significant increase in pS6-positive cells (Fig. 3A, C). Furthermore, treatment with MHY1485 significantly increased the frequency of primary cilia from 9.1% to 73.9% (Fig. 3 A, D).
Next, we treated ATDC5 cells with rapamycin, a potent mTOR signaling inhibitor. Notably, the number of cells was not affected by rapamycin at the concentration used (Fig. 3E, F). While the pS6-positive signal was observed in approximately 60% of control cells, the ratio of pS6-positive cells significantly decreased with rapamycin treatment (Fig. 3E, G). In addition, rapamycin significantly decreased the primary cilia frequency from 67.3% to 37.1% (Fig. 3E, H). Collectively, our data clearly demonstrate that mTOR signaling positively regulates cilia frequency in ATDC5 cells.
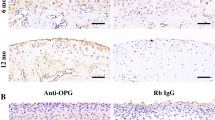
Inhibition of mTOR signaling affects primary cilia frequency in condylar cartilage
To analyze the effect of rapamycin on condylar cartilage in vivo, rapamycin was intraperitoneally administered every other day, for one week, to four-week-old mice. While pS6-positive cells were robustly present in the chondrocytes of vehicle-injected mice, they were rarely detected in the chondrocytes of rapamycin-injected mice (Fig. 4A, B). Rapamycin treatment significantly reduced the primary cilia frequency from 42.2% to 9.3% in the condylar cartilage (Fig. 4A, C).
We further analyzed the long-term effect of rapamycin on condylar cartilage, wherein rapamycin was intraperitoneally administered for 11 weeks. The pS6-positive cell ratio and primary cilia frequency were significantly reduced in the condylar cartilage of rapamycin-injected mice (Fig. 4D-F). These results indicate that the suppression of mTOR signaling by rapamycin and its effect on cilia frequency was sustained for a long time with continuous intraperitoneal administration. Consistent with the observations in ATDC5 cells, these results demonstrate that the inhibition of mTOR signaling by rapamycin significantly decreased cilia frequency in the condylar cartilage.
Next, we histologically analyzed the effect of mTOR signaling inhibition by rapamycin on the condylar cartilage. Rapamycin injection for 11 consecutive weeks significantly decreased the cartilage area and safranin O-positive area in the condylar cartilage (Fig. 5A-C). Although rapamycin did not significantly affect the cell density (Fig. 5D), the proportion of small cells tended to increase (Fig. 5E). The size of the Golgi apparatus was significantly decreased in the condylar cartilage of rapamycin-injected mice compared to that of the vehicle-injected mice (Fig. 5F, G). These results indicate that the inhibition of mTOR signaling induced the deterioration of condylar cartilage, resembling the phenotype observed in aged mice.
Discussion
Age-related changes in the condylar cartilage are critical etiological factors in TMJ-OA [4,5,6]; however, the mechanisms underlying the development of TMJ-OA remain unknown. Therefore, the present study investigated age-related changes and their possible association with mTOR signaling and primary cilia in the condylar cartilage. We observed an age-related decline in mTOR signaling and primary cilia frequency, associated with tissue deterioration in the condylar cartilage. With age, decreased cell proliferation [16], density [13, 14], and size [14] have been reported in condylar chondrocytes. Decreased proteoglycan production in condylar cartilage is a common histological observation in aged mice, as confirmed by safranin O staining [6, 13, 16] and aggrecan (Acan) immunohistochemistry [14]. Moreover, gene ontology enrichment analysis revealed that genes associated with ECM organization, including Col1a1, Col1a2, Col2a1, and Acan, were the most differentially expressed genes in the condylar cartilage of 50-week-old mice compared to that of 10-week-old mice [14]. The histological observations in the present study are consistent with previous studies reporting age-related deterioration changes in the condylar cartilage. Furthermore, we demonstrated that the manipulation of mTOR signaling with rapamycin resulted in tissue deterioration in the condylar cartilage, which was phenotypically similar to that observed in aged mice (Fig. 4, 5). These results strongly indicate that age-related deterioration changes in the condylar cartilage are attributed to a reduction in mTOR signaling.
In the present study, we observed a reduction in cilia frequency in the condylar cartilage in both aged and rapamycin-injected mice. This result suggests the involvement of primary cilia in the age-related deterioration of the condylar cartilage. We have previously reported that condylar cartilage-specific deletion of primary cilia in Ift20fl/fl;NG2-CreER mice results in condylar cartilage deterioration, including suppressed chondrocyte hypertrophy, decreased proteoglycan production, and reduced cartilage thickness [28]. Similarly, the cartilage-specific deletion of primary cilia in Kif3afl/fl;Col2a1-Cre mice also exhibited a deterioration in the condylar cartilage [42]. Therefore, given that dysfunction of primary cilia causes deterioration of condylar cartilage [28, 42], our results suggest that age-related attenuation of mTOR signaling decreases primary cilia, contributing to the deterioration of the condyle cartilage (Fig. 6). Although further validations are required, this study suggested a possible intrinsic mechanism that could illustrate the etiology of age-related deterioration of the condylar cartilage.
In the present study, we showed that mTOR signaling positively regulates primary cilia in condylar chondrocytes. However, in general, the impact of mTOR signaling on primary cilia is cell type- and context-dependent [30]. Consistent with the result of our study, mTOR signaling has been reported to maintain cilia length and frequency in mouse embryonic fibroblasts [31, 32, 34] and zebrafish [33]. In contrast, conflicting results have also been reported, with the inhibition of mTOR signaling by rapamycin resulting in cilia elongation in epithelial cells [43, 44]. Although mTOR signaling is thought to regulate ciliogenesis via autophagy, its effect on ciliogenesis depends on the cell type and environment [45]. Therefore, further studies are required to comprehensively understand the roles of mTOR signaling on primary cilia in a context-dependent manner.
The mTOR signaling is essential for tissue development and growth as it promotes cell proliferation and differentiation; however, with advancing age, excessive cellular activities, such as vigorous protein secretion, may accelerate age-related disease progressions[46]. Therefore, the administration of mTOR inhibitors, such as rapamycin, has received considerable attention for its anti-aging properties [47]. Rapamycin exhibits a protective effect against injury-induced ECM damage and cell death in cartilage explants [48] and ameliorates cartilage degradation in experimental OA [49]. In contrast, in the present study, we demonstrated that the administration of rapamycin resulted in the deterioration of condylar cartilage. This discrepancy, characterized by the acceleration of aging-like tissue deterioration accompanied by a protective effect on damaged tissues, may be attributed to the unique tissue maintenance properties of articular cartilage, where continuous ECM secretion is required to maintain tissue integrity. Notably, the impact of mTOR signaling on chondrocytes depends on their differentiation status, as the activity of mTOR signaling changes dynamically during chondrocyte differentiation [35]. Therefore, rapamycin has dual functions in articular cartilage, inducing aging-like tissue deterioration under physiological conditions while ameliorating tissue degradation in OA. Therefore, it is important to elucidate whether the dual function of rapamycin is unique to articular cartilage or a common characteristic of cartilage in general.
Rapamycin is widely used to prevent rejection in transplantation and as a treatment for autoimmune diseases owing to its immunosuppressive effects [50]. Rapamycin inhibits mTOR signaling, suppressing the immune response by preventing cell cycle progression in T cells [51]; however, this inhibitor effect differs depending on the type of T cells [50]. In this study, we observed that rapamycin induced a notable reduction in mTOR signaling in ATDC5 cells, without affecting cell proliferation. This observation indicates that the deteriorative changes in condylar cartilage induced by rapamycin are likely not mediated through the modulation of cell proliferation, but rather through the regulation of cilia assembly. However, the assembly and disassembly of primary cilia depend on and impact cell cycle progression, although the exact mechanism remains unknown [52]. Overall, these results warrant further investigations into the relationship between the regulation of cilia assembly by mTOR signaling and cell cycle regulation.
In summary, a loss of primary cilia due to a decline in mTOR signaling correlated with age-related deteriorations in condylar cartilage. In addition, this study is the first to show the significance of mTOR signaling on ciliogenesis in condylar cartilage. Although inhibition of mTOR signaling has been considered to be effective for age-related tissue deterioration, our study showed an essential role of mTOR signaling in the tissue maintenance of the condylar cartilage. Our findings provide new insights into the tissue homeostasis and regeneration of condylar cartilage, which contributes to understanding the etiology of age-related TMJ-OA and the development of therapeutic strategies.
Abbreviations
- TMJ:
-
Temporomandibular joint
- OA:
-
Osteoarthritis
- ECM:
-
Extracellular matrix
- IFT:
-
Intraflagellar transport
- mTOR:
-
Mechanistic/mammalian target of Rapamycin
- pS6:
-
Phosphorylated ribosomal protein S6 kinase
References
Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, Carr AJ. Osteoarthr Lancet. 2015;386:376–87. https://doi.org/10.1016/S0140-6736(14)60802-3.
Al-Ani Z. Temporomandibular joint osteoarthrosis: a review of clinical aspects and management. Prim Dent J. 2021;10:132–40. https://doi.org/10.1177/2050168420980977.
Kelemen K, Konig J, Czumbel M, Szabo B, Hegyi P, Gerber G, Borbely J, Mikulas K, Schmidt P, Hermann P. Additional splint therapy has no superiority in myogenic temporomandibular disorders: a systematic review and meta-analysis of randomized controlled trials. J Prosthodont Res. 2024;68:12–9. https://doi.org/10.2186/jpr.JPR_D_22_00264.
Zhou Y, Al-Naggar IMA, Chen PJ, Gasek NS, Wang K, Mehta S, Kuchel GA, Yadav S, Xu M. Senolytics alleviate the degenerative disorders of temporomandibular joint in old age. Aging Cell. 2021;20:e13394. https://doi.org/10.1111/acel.13394.
Pereira FJ Jr, Lundh H, Westesson PL. Morphologic changes in the temporomandibular joint in different age groups. An autopsy investigation. Oral Surg Oral Med Oral Pathol. 1994;78:279–87.
Chen PJ, Dutra EH, Mehta S, O’Brien MH, Yadav S. Age-related changes in the cartilage of the temporomandibular joint. Geroscience. 2020;42:995–1004. https://doi.org/10.1007/s11357-020-00160-w.
Delpachitra SN, Dimitroulis G. Osteoarthritis of the temporomandibular joint: a review of aetiology and pathogenesis. Br J Oral Maxillofac Surg. 2022;60:387–96. https://doi.org/10.1016/j.bjoms.2021.06.017.
Ootake T, Ishii T, Sueishi K, Watanabe A, Ishizuka Y, Amano K, Nagao M, Nishimura K, Nishii Y. Effects of mechanical stress and deficiency of dihydrotestosterone or 17β-estradiol on temporomandibular joint osteoarthritis in mice. Osteoarthritis Cartilage. 2021;29:1575–89. https://doi.org/10.1016/j.joca.2021.08.005.
Sangani D, Suzuki A, VonVille H, Hixson JE, Iwata J. Gene mutations associated with temporomandibular joint disorders: A systematic review. OAlib. 2015;2:e1583. https://doi.org/10.4236/oalib.1101583.
Lai Y, Zheng W, Qu M, Xiao CC, Chen S, Yao Q, Gong W, Tao C, Yan Q, Zhang P, Wu X, Xiao G. Kindlin-2 loss in condylar chondrocytes causes spontaneous osteoarthritic lesions in the temporomandibular joint in mice. Int J Oral Sci. 2022;14:33. https://doi.org/10.1038/s41368-022-00185-1.
Nakao Y, Konno-Nagasaka M, Toriya N, Arakawa T, Kashio H, Takuma T, Mizoguchi I. Proteoglycan expression is influenced by mechanical load in TMJ discs. J Dent Res. 2015;94:93–100. https://doi.org/10.1177/0022034514553816.
Knudson CB, Knudson W. Cartilage proteoglycans. Semin Cell Dev Biol. 2001;12:69–78. https://doi.org/10.1006/scdb.2000.0243.
Livne E. Matrix synthesis in mandibular condylar cartilage of aging mice. Osteoarthr Cartil. 1994;2:187–97. https://doi.org/10.1016/s1063-4584(05)80068-8.
Yang MC, Nakamura M, Kageyama Y, Igari Y, Sasano Y. Age-related gene and protein expression in mouse mandibular condyle analyzed by cap analysis of gene expression and immunohistochemistry. Gerontology. 2023;69:1295–306. https://doi.org/10.1159/000533921.
Elshawi A, Wakamatsu N, Iinuma M, Nagayama M, Tamura Y. TMJ degenerative changes in SAMP3 mice by occlusal disharmony and aging. J Hard Tissue Biol. 2012;2012(21):399–406. https://doi.org/10.2485/jhtb.21.399.
Ishizuka Y, Shibukawa Y, Nagayama M, Decker R, Kinumatsu T, Saito A, Pacifici M, Koyama E. TMJ degeneration in SAMP8 mice is accompanied by deranged Ihh signaling. J Dent Res. 2014;2014(93):281–7. https://doi.org/10.1177/0022034513519649.
Cardoneanu A, Macovei LA, Burlui AM, Mihai IR, Bratoiu I, Rezus II, Richter P, Tamba BI, Rezus E. Temporomandibular joint osteoarthritis: Pathogenic mechanisms involving the cartilage and subchondral bone, and potential therapeutic strategies for joint regeneration. Int J Mol Sci. 2022;24:171. https://doi.org/10.3390/ijms24010171.
Shi Y, Hu X, Cheng J, Zhang X, Zhao F, Shi W, Ren B, Yu H, Yang P, Li Z, Duan X, Fu X, Zhang J, Wang J, Ao Y. A small molecule promotes cartilage extracellular matrix generation and inhibits osteoarthritis development. Nat Commun. 2019;10:1914. https://doi.org/10.1038/s41467-019-09839-x.
Chen HY, Kelley RA, Li T, Swaroop A. Primary cilia biogenesis and associated retinal ciliopathies. Semin Cell Dev Biol. 2021;110:70–88. https://doi.org/10.1016/j.semcdb.2020.07.013.
Noda K, Kitami M, Kitami K, Kaku M, Komatsu Y. Canonical and noncanonical intraflagellar transport regulates craniofacial skeletal development. Proc Natl Acad Sci U S A. 2016;113:E2589–97. https://doi.org/10.1073/pnas.1519458113.
Berbari NF, O’Connor AK, Haycraft CJ, Yoder BK. The primary cilium as a complex signaling center. Curr Biol. 2009;19:R526–35. https://doi.org/10.1016/j.cub.2009.05.025.
Kaku M, Komatsu Y. Functional diversity of ciliary proteins in bone development and disease. Curr Osteoporos Rep. 2017;15:96–102. https://doi.org/10.1007/s11914-017-0351-6.
Chinipardaz Z, Liu M, Graves DT, Yang S. Role of primary cilia in bone and cartilage. J Dent Res. 2022;101:253–60. https://doi.org/10.1177/00220345211046606.
Arseni L, Lombardi A, Orioli D. From structure to phenotype: Impact of collagen alterations on human health. Int J Mol Sci. 2018;19:1407. https://doi.org/10.3390/ijms19051407.
Collins I, Wann AKT. Regulation of the extracellular matrix by ciliary machinery. Cells. 2020;9:278. https://doi.org/10.3390/cells9020278.
Yuan X, Yang S. Deletion of ift80 impairs epiphyseal and articular cartilage formation due to disruption of chondrocyte differentiation. PLoS ONE. 2015;10:e0130618.
McGlashan SR, Haycraft CJ, Jensen CG, Yoder BK, Poole CA. Articular cartilage and growth plate defects are associated with chondrocyte cytoskeletal abnormalities in Tg737orpk mice lacking the primary cilia protein polaris. Matrix Biol. 2007;26:234–46. https://doi.org/10.1016/j.matbio.2006.12.003.
Kitami M, Yamaguchi H, Ebina M, Kaku M, Chen D, Komatsu Y. IFT20 is required for the maintenance of cartilaginous matrix in condylar cartilage. Biochem Biophys Res Commun. 2019;509:222–6. https://doi.org/10.1016/j.bbrc.2018.12.107.
Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471–84. https://doi.org/10.1016/j.cell.2006.01.016.
Lai Y, Jiang Y. Reciprocal regulation between primary cilia and mTORC1. Genes (Basel). 2020;11:711. https://doi.org/10.3390/genes11060711.
DiBella LM, Park A, Sun Z. Zebrafish TSC1 reveals functional interactions between the cilium and the TOR pathway. Hum Mol Genet. 2009;18:595–606. https://doi.org/10.1093/hmg/ddn384.
Rosengren T, Larsen LJ, Pedersen LB, Christensen ST, Moller LB. TSC21 and TSC2 regulate cilia length and canonical hedgehog signaling via different mechanisms. Cell Mol Life Sci. 2018;75:2663–80. https://doi.org/10.1007/s00018-018-2761-8.
Yuan S, Li J, Diener DR, Choma MA, Rosenbaum JL, Sun Z. Target-of-rapamycin complex 1 (Torc1) signaling modulates cilia size and function through protein synthesis regulation. Proc Natl Acad Sci U S A. 2012;109:2021–6. https://doi.org/10.1073/pnas.1112834109.
Hartman TR, Liu D, Zilfou JT, Robb V, Morrison T, Watnick T, Henske EP. The tuberous sclerosis proteins regulate formation of the primary cilium via a rapamycin-insensitive and polycystin 1-independent pathway. Hum Mol Genet. 2009;18:151–63. https://doi.org/10.1093/hmg/ddn325.
Yan B, Zhang Z, Jin D, Cai C, Jia C, Liu W, Wang T, Li S, Zhang H, Huang B, Lai P, Wang H, Liu A, Zeng C, Cai D, Jiang Y, Bai X. mTORC1 regulates PTHrP to coordinate chondrocyte growth, proliferation and differentiation. Nat Commun. 7:11151. https://doi.org/10.1038/ncomms11151.
Charan J, Kantharia ND. How to calculate sample size in animal studies? J Pharmacol Pharmacother. 2013;4:303–6. https://doi.org/10.4103/0976-500X.119726.
Zhao S, Chen C, Wang S, Ji F, Xie Y. Mhy1485 activates mTOR and protects osteoblasts from dexamethasone. Biochem Biophys Res Commun. 2016;481:212–8. https://doi.org/10.1016/j.bbrc.2016.10.104.
Yang J, Kitami M, Pan H, Nakamura MT, Zhang H, Liu F, Zhu L, Komatsu Y, Mishina Y. Augmented BMP signaling commits cranial neural crest cells to a chondrogenic fate by suppressing autophagic β-catenin degradation. Sci Signal. 2021;14:eaaz9368. https://doi.org/10.1126/scisignal.aaz9368
Ramos FJ, Chen SC, Garelick MG, Dai DF, Liao CY, Schreiber KH, MacKay VL, An EH, Strong R, Ladiges WC, Rabinovitch PS, Kaeberlein M, Kennedy BK. Rapamycin reverses elevated mTORC1 signaling in lamin A/C-deficient mice, rescues cardiac and skeletal muscle function, and extends survival. Sci Transl Med. 2012;4:144ra103. https://doi.org/10.1126/scitranslmed.3003802
Bitto A, Ito TK, Pineda VV, LeTexier NJ, Huang HZ, Sutlief E, Tung H, Vizzini N, Chen B, Smith K, Meza D, Yajima M, Beyer RP, Kerr KF, Davis DJ, Gillespie CH, Snyder JM, Treuting PM, Kaeberlein M. Transient rapamycin treatment can increase lifespan and healthspan in middle-aged mice. Elife. 2016;5:e16351. https://doi.org/10.7554/eLife.16351.
Cameron DA. The Golgi apparatus in bone and cartilage cells. Clin Orthop Relat Res. 1968;58:191–211.
Kinumatsu T, Shibukawa Y, Yasuda T, Nagayama M, Yamada S, Serra R, Pacifici M, Koyama E. TMJ development and growth require primary cilia function. J Dent Res. 2011;90:988–94. https://doi.org/10.1177/0022034511409407.
Sherpa RT, Atkinson KF, Ferreira VP, Nauli SM. Rapamycin increases length and mechanosensory function of primary cilia in renal epithelial and vascular endothelial cells. Int Educ Res J. 2016;2:91–7.
Jamal MH, Nunes ACF, Vaziri ND, Ramchandran R, Bacallao RL, Nauli AM, Nauli SM. Rapamycin treatment correlates changes in primary cilia expression with cell cycle regulation in epithelial cells. Biochem Pharmacol. 2020;178:114056. https://doi.org/10.1016/j.bcp.2020.114056.
Mukhopadhyay S, Frias MA, Chatterjee A, Yellen P, Foster DA. The enigma of rapamycin dosage. Mol Cancer Ther. 2016;15:347–53. https://doi.org/10.1158/1535-7163.MCT-15-0720.
Blagosklonny MV. Cell senescence, rapamycin and hyperfunction theory of aging. Cell Cycle. 2022;21:1456–67. https://doi.org/10.1080/15384101.2022.2054636.
Sasaki N, Itakura Y, Toyoda M. Rapamycin promotes endothelial-mesenchymal transition during stress-induced premature senescence through the activation of autophagy. Cell Commun Signal. 2020;18:43. https://doi.org/10.1186/s12964-020-00533-w.
Caramés B, Taniguchi N, Seino D, Blanco FJ, D’Lima D, Lotz M. Mechanical injury suppresses autophagy regulators and pharmacologic activation of autophagy results in chondroprotection. Arthritis Rheum. 2012;64:1182–92. https://doi.org/10.1002/art.33444.
Caramés B, Hasegawa A, Taniguchi N, Miyaki S, Blanco FJ, Lotz M. Autophagy activation by rapamycin reduces severity of experimental osteoarthritis. Ann Rheum Dis. 2012;71:575–81. https://doi.org/10.1136/annrheumdis-2011-200557.
Thomson AW, Turnquist HR, Raimondi G. Immunoregulatory functions of mTOR inhibition. Nat Rev Immunol. 2009;9:324–37. https://doi.org/10.1038/nri2546.
Mondino A, Mueller DL. mTOR at the crossroads of T cell proliferation and tolerance. Semin Immunol. 2007;19:162–72. https://doi.org/10.1016/j.smim.2007.02.008.
Kasahara K, Inagaki M. Primary ciliary signaling: Links with the cell cycle. Trends Cell Biol. 2021;31:954–64. https://doi.org/10.1016/j.tcb.2021.07.009.
Funding
This study was supported by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JP19K19088 and JP21K17035 to MKi).
Author information
Authors and Affiliations
Contributions
Conception and design: M.Ki; Conducting the experiments: M.Ki. L.T.; Analysis and interpretation of the data: M.Ki; Drafting of the article: M.Ki.; Review and editing of the article: M.Ka and T.M.
Corresponding authors
Ethics declarations
Ethical statement
All animal experimental protocols were approved by the Animal Care and Experimentation Committee of Niigata University (SA00959).
Competing interests
No potential conflict of interest was reported by the authors.
(A) Micro-CT analysis of mouse mandibular condyle at 5, 15, 26, 52, and 78 weeks. Bar, 0.5 mm. (B) Bone mineral density (BMD) of the mandibular condyle. (C) The mandibular condyle was stained with safranin O at five, 15, 26, 52, and 78 weeks. Bar, 50 μm. (D–G) Cartilage area, safranin O-positive area, cell density, and cell size distribution were quantified in the condylar cartilage with age. Data in (B), (D), (E), and (F) are represented as mean ± SD; n = 5 in each group. aP < 0.05, vs. 5 w; AP < 0.01, vs. 5 w; bP < 0.05, vs. 15 w; BP < 0.01, vs. 15 w; cP < 0.05, vs. 26 w; CP < 0.01, vs. 26 w; DP < 0.01, vs. 52 w.
(A) Immunohistochemistry of cis-Golgi marker GM130 in condylar cartilage. Bars, 10 μm. (B) The Golgi apparatus size of chondrocytes of all layers in the condylar cartilage was quantified. (C) Age-related changes in primary cilia were examined via immunohistochemistry of the condylar cartilage using anti-acetylated tubulin and anti-gamma-tubulin antibodies. Bars, 10 μm. (D) Primary cilia frequency in chondrocytes. (E) Immunohistochemistry analysis of pS6. Bars, 10 μm. (F) The ratio of pS6-positive chondrocytes. The white square indicates the region of interest in the high-magnification image shown in (A) (C) and (E). Data in (B) (D) and (F) are represented as mean ± SD; n = 5 in each group. aP < 0.05, vs. 5 w; AP < 0.01, vs. 5 w; bP < 0.05, vs. 15 w; BP < 0.01, vs. 15 w; cP < 0.05, vs. 26 w.
(A-D) ATDC5 cells, a chondroprogenitor cell line, were treated with DMSO as control (Cont) or MHY1485. (A) Immunocytochemistry analysis using anti-acetylated tubulin, anti-gamma-tubulin, and anti-pS6. Cells were counterstained with DAPI. Bars, 10 μm. (B) Cell number. (C) The ratio of pS6-positive cells. (D) Primary cilia frequency. (E–H) ATDC5 cells were treated with ethanol as control (Cont) or Rapamycin (RAP). (E) Immunocytochemistry analysis using anti-acetylated tubulin, anti-gamma-tubulin, and anti-pS6. Cells were counterstained with DAPI. Bars, 10 μm. (F) Cell number. (G) The ratio of pS6-positive cells. (H) Primary cilia frequency. The white square indicates the region of interest in the high-magnification image shown in (A) and (E). Arrowheads indicate the primary cilia. Data in (B), (C), (D), (F), (G), and (H) are represented as mean ± SD; n = 6 in each group. *: P < 0.05, as compared to vehicle.
(A-C) Mice were injected with the vehicle as control (Cont) or rapamycin (RAP) for one week. (A) Immunohistochemistry analysis using anti-acetylated tubulin, anti-gamma-tubulin, and anti-pS6 antibodies in the condylar cartilage. Bars, 10 μm. (B) The ratio of pS6-positive cells. (C) Primary cilia frequency. (D-F) Mice were injected with a vehicle as control (Cont) or rapamycin (RAP) for 11 weeks. (D) Immunohistochemistry analysis in the condylar cartilage. Bars, 10 μm. (E) The ratio of pS6-positive cells. (F) Primary cilia frequency. The white square indicates the region of interest in the high-magnification image shown in (A) and (D). Arrowheads indicate the primary cilia. Data in (B), (C), (E), and (F) are represented as mean ± SD; n = 6 in each group. *: P < 0.05, as compared to control.
Mice were injected with a vehicle as control (Cont) or rapamycin (RAP) for 11 weeks. (A) The mandibular condylar cartilage was stained with safranin O Bars, 100 μm. (B–E) Cartilage area, safranin O-positive area, cell density, and cell size distribution of the condylar cartilage in rapamycin/vehicle-injected mice. (F) cis-Golgi marker GM130 in condylar cartilage in rapamycin/vehicle-injected mice. Bars, 10 μm. (G) Golgi apparatus size. The white square indicates the region of interest in the high-magnification image shown in (F). Data in (B), (C), (D), and (G) are represented as mean ± SD; n = 6 in each group. *: P < 0.05, as compared to control.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kitami, M., Kaku, M., Thant, L. et al. A loss of primary cilia by a reduction in mTOR signaling correlates with age-related deteriorations in condylar cartilage. GeroScience (2024). https://doi.org/10.1007/s11357-024-01143-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01143-x