Abstract
The healthy aging index (HAI) has been recently developed as a surrogate measure of biological age. However, to what extent the HAI is associated with all-cause and cause-specific mortality and whether this association differs in younger and older adults remains unknown. We aimed to quantify the association between the HAI and mortality in a population of UK adults. In the prospective cohort study, data are obtained from the UK Biobank. Five HAI components (systolic blood pressure, reaction time, cystatin C, serum glucose, forced vital capacity) were scored 0 (healthiest), 1, and 2 (unhealthiest) according to sex-specific tertiles or clinically relevant cut-points and summed to construct the HAI (range 0–10). Cox proportional hazard regression models were used to estimate the associations of the HAI with the risk of all-cause and cause-specific mortality. 387,794 middle-aged and older participants were followed up for a median of 8.9 years (IQR 8.3–9.5). A total of 14,112 all-cause deaths were documented. After adjustments, each 1-point increase in the HAI was related to a higher risk of all-cause mortality (hazards ratio [HR], 1.17; 95%CI, 1.15–1.18). Such association was stronger among adults younger than 60 years (1.19, 1.17–1.21) than that among those 60 years and older (1.15, 1.14–1.17) (P interaction < 0.001). For each unit increment of the HAI, the multivariate-adjusted HRs for risk of death were 1.28 (1.25–1.31) for cardiovascular diseases, 1.09 (1.07–1.10) for cancer, 1.36 (1.29–1.44) for digestive disease, 1.42 (1.35–1.48) for respiratory disease, 1.42 (1.33–1.51) for infectious diseases, and 1.15 (1.09–1.21) for neurodegenerative disease, respectively. Our findings indicate that the HAI is positively associated with all-cause and cause-specific mortality independent of chronological age. Our results further underscore the importance of effective early-life interventions to slow aging and prevent premature death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rapid population aging has posed severe threats to health and social care systems [1]. Between 2019 and 2050, the number of persons aged 65 or over worldwide is projected to more than double (1.5 billion), which will outnumber adolescents and youth aged 15 to 24 years (1.3 billion) [2]. Nevertheless, between-person variations in the pace of aging may exist among individuals of the same chronological age, which manifest as differences in susceptibility to disease and death [3, 4]. Therefore, it is of paramount importance to study the biological determinants of the between-person variations in “healthy aging.”
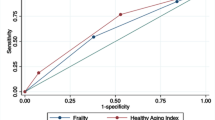
While several aging indicators have been proposed in the UK Biobank, such as the biological age based on 72 biomarkers [5] and the frailty index based on 49 items [6], which have provided multisystem approaches to research and prevention of diseases of aging, surrogate aging measures with relative affordability and practicality are needed to be applicable to the clinical settings. The healthy aging index (HAI), a modified Physiological Index of Comorbidity developed by Newman et al. [7], has been associated with increased mortality risk in older adults (≥ 60 years) in the United States (US) and China [8,9,10,11,12,13]. Using only five noninvasive clinical tests (systolic blood pressure, reaction time, cystatin C, serum glucose, forced vital capacity), the HAI not only captures subclinical hypofunction across multiple organ systems, but also provides incremental value for death prediction beyond clinically diagnosed chronic diseases among elders [12]. The global proportion of older individuals is increasing, and this phenomenon is more pronounced in the UK than in the US and China, which may result in a growing risk of adverse age-related outcomes in the UK [14]. Although the HAI has been applied in the UK Biobank recently and has a significant impact on major vascular events [15], the association of the HAI with all-cause and cause mortality risk remains unclear.
In the present study, we aimed to assess whether an adaptation of the HAI using data from UK Biobank (a large prospective cohort of over 500,000 middle-aged people) can be used to identify people at increased risk of all-cause and cause-specific mortality across a wide range of ages; and to further investigate whether the effect of HAI on mortality risk could be modified by sociodemographic characteristics, lifestyle factors, and health status.
Method
Study participants
In this prospective cohort study, we sourced data from the UK Biobank. Details of the design and survey methods of the UK Biobank have been described elsewhere [16,17,18]. In brief, UK Biobank, a general population cohort study, recruited more than 500,000 middle-aged participants between April 2007 and December 2010 (5.5% response rate for around 9 million people who received invitations). The baseline survey was done in 22 assessment centers across England, Wales, and Scotland, where participants completed a touch screen questionnaire, took physical measurements, and provided biological samples.
From the initial sample of 502,527 participants, we excluded those with missing information on all five HAI components [SBP, reaction time, cystatin C, serum glucose, and FVC; n = 113,372), and other key covariates [race/ethnicity; n = 1361], leaving 387,794 participants included in the present study. Written informed consent was provided by all participants, and the study was approved by the North West Multicenter Research Ethics Committee. We conducted this research using the UK Biobank Resource under Application Number 44430. Ethical approval was also obtained from the Ethical Committee of Peking University (Beijing, China).
Index components
Systolic blood pressure
Two SBP measurements were taken in a seated position after a 2-min rest using an appropriate cuff and an Omron HEM-7015IT digital BP monitor, and in this study, the average was calculated. For individuals with missing automated SBP readings, we used the mean of these 2 manual values for imputation. We used sex-specific tertiles of SBP values to classify participants into three categories: 0 = < 135 mmHg for men and < 127 mmHg for women; 1 = 135–150 mmHg for men and 127–146 mmHg for women; and 2 = ≥ 150 mmHg for men and ≥ 146 mmHg for women. Participants who reported a physician diagnosis of hypertension or were taking BP-lowering medications were also grouped in the unhealthiest category (component score = 2).
Reaction time
Although previous studies of HAI have identified the Digit Symbol Substitution Test (DSST) as a potential indicator of cognitive performance [8, 13], only a subset of participants who accepted the invitation to the follow-up assessment have completed the DSST in the UK Biobank [19]. Given the strong correlation between DSST score and reaction time, we proposed that reaction time could substitute for DSST, both of which fall within the cognitive domain of processing speed. Although the replacement measurement may not represent a phenotype identical to that represented by the original components, they are nonetheless indicators of neurological health. Reaction times were collected via a touchscreen at the baseline assessment, in which participants were asked to complete a computerized version of the card game “Snap,” pressing a button as quickly as possible when two cards displayed on the screen matched. Scores consisted of the average time to give a correct response. Sex-specific tertiles of reaction time were applied to classify participants into three groups: 0 = < 493 ms for men and < 509 ms for women; 1 = 493–574 ms for men and 509–591 ms for women; and 2 = ≥ 574 ms for men and ≥ 591 ms for women.
Cystatin C
Cystatin C was measured by latex-enhanced immunoturbidimetric analysis on a Siemens ADVIA 1800, which was scored using sex-specific tertiles of the cystatin C values: 0 = < 0.87 mg/dL for men and < 0.81 mg/dL for women; 1 = 0.87–0.98 mg/dL for men and 0.81–0.91 mg/dL for women; and 2 = ≥ 0.98 mg/dL for men and ≥ 0.91 mg/dL for women.
Serum glucose
Random glucose was measured by hexokinase analysis on a Beckman Coulter AU5800 for all participants with an available blood sample at baseline. Given the majority (> 95%) of the participants who took the random test fasted < 8 h, we classified participants into 3 groups according to clinical cutoff points of random glucose as follows: 0 = ≤ 140 mg/dL, 1 = 140–200 mg/dL, and 2 = ≥ 200 mg/dL [20]. In addition, participants who reported a diagnosis of diabetes or who were using medication for diabetes were coded as 2.
Forced vital capacity
FVC value was calculated from blow using a Vitalograph Pneumotrac 6800. We divided participants into three FVC categories using sex-specific tertiles: 0 = ≥ 4750 mL for men and ≥ 3400 mL mg/dL for women; 1 = 4000–4750 mL for men and 2870–3400 mL for women; and 2 = < 4000 mL for men and < 2870 mL for women.
All the above HAI components are known risk factors for death [21,22,23,24,25,26,27]. The sum of these five scores together gave a total HAI score ranging from 0 to 10, with a higher value indicating a worse, unhealthier aging status. The summary of cutoffs used in this study can be seen in eTable 1. With reference to previous studies [8, 9, 13, 28], we further categorized HAI scores into the following four levels: 0–2 (healthiest), 3–4, 5–6, and 7–10 (unhealthiest).
Mortality status follow-up
Long-term follow-up for mortality was done in the UK Biobank through comprehensive data linkage. Date and cause of death were obtained from the National Health Service (NHS) Information Centre for participants from England and Wales, and from the NHS Central Register, Scotland, for participants from Scotland. Details of information about the linkage procedure can be found at http://content.digital.nhs.uk/services. Linkage recorded all deaths occurring until 14 February 2018 for England and 31 December 2016 for Scotland. The outcomes of this study were all-cause mortality and cause-specific mortality (cardiovascular diseases, cancer, respiratory disease, digestive disease, neurodegenerative disease, infectious disease, and all other causes), based on the 10th revision of the International Classification of Diseases (ICD-10) (eTable 2).
Covariates
This study utilized the following potential confounding factors: sociodemographic characteristics [age, sex, ethnicity, UK Biobank assessment center, social deprivation (Townsend deprivation index), and highest education levels]; anthropometric indicators [body mass index (BMI)]; lifestyle behaviors [smoking status (current, former, or never), alcohol intake, physical activity, and diet], personal health and medical history [cardiovascular diseases, cancer, respiratory disease, digestive disease, neurodegenerative disease, infectious disease, and medication use (anti-hypertensive medication, cholesterol-lowering medication, hormone replacement therapy, oral contraceptive pill, or none)], and biomarkers [high-density lipoprotein, low-density lipoprotein, triglycerides, and total cholesterol].
Daily physical activity levels were calculated by multiplying the metabolic equivalent tasks (METs) value for a specific type of physical activity by hours spent on that activity per week and then adding up the MET hours for all activities. Overall dietary pattern was assessed by healthy diet score including the following factors: fruit intake at least three pieces each day; vegetable intake at least four tablespoons each day; fish intake at least twice each week; processed meat intake no more than twice each week; and unprocessed red meat intake no more than twice each week. We added each healthy dietary factor to calculate the final diet score ranging from 0 to 5 [29, 30]. Information on prevalent diseases was obtained through self-reported and hospital inpatient records (eTable 3). For continuous variables, missing values were imputed sex-specific median values, while categorical variables were handled with missing indicators.
Statistical analysis
Baseline characteristics were described across four categories of HAI (i.e., 0–2, 3–4, 5-–6, and 7–10) as means (SD) for continuous variables and percentages for categorical variables. In addition, we plotted the mean HAI and the prevalence of unhealthiest aging status by age and sex to examine the associations of the HAI with age.
In the full cohort, we used Cox proportional hazard regression models to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of the risk of all-cause and cause-specific mortality associated with the HAI, which was included in the models as a continuous or a categorical variable. Follow-up person-years were calculated from baseline until the date of death, or end of follow-up, whichever occurred first. No violations to the proportional hazards assumption were observed by inspection of the plots of the Schoenfeld residual. We undertook separate models by sequential inclusion of three groups of covariates to examine the different potential confounding effects on the associations between HAI levels and mortality risk. Model 1 included basic sociodemographic characteristics (sex, age, UK Biobank assessment center, and race/ethnicity), followed by model 2 that additionally included other sociodemographic characteristics (Townsend deprivation index and highest education level), anthropometric indicators (BMI), and lifestyle factors (smoking status, alcohol intake, and physical activity). Model 3 additionally included chronic health conditions (eTable 3) and medication use (anti-hypertensive medication, cholesterol-lowering medication, hormone replacement therapy, oral contraceptive pill, or none). Notably, we adjusted for all the chronic conditions in the all-cause analysis, and for only one disease in the corresponding cause-specific analyses. To visually explore non-linear associations between HAI and mortality risk, we used restricted cubic splines for HAI score with 3 knots at the 25th, 50th, and 75th percentiles of the distribution, stratified by sex and baseline age. We also applied a Kaplan–Meier survival curve to compare survival probabilities after baseline recruitment between different groups of HAI stratified by sex and baseline age. In addition, interaction terms of potential covariates (age, sex, smoking status, alcohol intake, level of physical activity, and BMI) were tested using the likelihood ratio test, which involved comparing models with and without interaction terms, and we performed subgroup analyses. Considering that most studies of the HAI used 60 years as the cutoff of age, we conducted subgroup analysis by age (≥ 60 vs. < 60 years) for convenience of comparison, with 60 years old also being the median age. Additionally, we also calculated the population attributable risk percent (PAR%) to estimate the proportion of death that theoretically would not have occurred if all participants were in a low-risk group, in the case of assuming causality.
To examine the robustness of our findings, we also conducted several sensitivity analyses: additionally adjusting for dietary factors; excluding individuals with one or more of these diseases at baseline from the analysis, either separately or together; excluding those who had ever used medications; excluding current smokers and current drinker. In order to avoid bias from the imputation of missing covariates, participants with missing values were also removed in another sensitivity analysis. In addition, we excluded those who had died during the first 5 years of follow-up to minimize the influence of reverse causality.
All statistical analyses were conducted using Stata version 16.0. All p values were two-sided and we defined the level of statistical significance as a P value less than 0.05.
Patient and public involvement
No patients or the public were involved in setting the research question or the outcome measures, nor were they involved in developing plans for the design or implementation of the study. No patients were asked to advise on the interpretation or writing up of results. There are no plans to disseminate the results of the research to study participants or the relevant patient community.
Results
Population characteristics
Of the 502,527 participants recruited to UK Biobank, 387,794 (77%) who had complete data on HAI and key covariates were included, with a median follow-up of 8.9 years (IQR 8.3–9.5; total follow-up 3,425,798 person-years). Table 1 summarizes the main characteristics of the participants by quarters of HAI. Among 387,794 participants (mean age 56.4 years, 45.8% men), 90,804 (23.4%) had a score of 0–2, 122,574 (31.6%) had a score of 3–4, 113,505 (29.3%) had a score of 5–6, and 60,911 (15.7%) had a score of 7–10. Participants with lower HAI were more likely to be women, White people, younger, non-smoker, and more educated, and less likely to use medications, and to have lower Townsend index, and a lower prevalence of comorbidities, but higher level of physical activity. There were no significant differences between the included and the whole populations from UK Biobank in terms of most baseline characteristics.
The HAI showed a right-skewed distribution towards older age, either in combination or separately (eFigs. 1 and 2). The mean HAI across all participants was 4.23 (SD 2.16). Both the mean HAI and the prevalence of unhealthiest aging status increased with age. The prevalence of unhealthiest aging status increased from 2319 (2.5%) in 92,794 people aged < 50 years to 12,827 (9.9%) in 129,870 people aged 50–60 years, and to 45,765 (27.7%) in 165,130 people aged > 60 years. As shown in Fig. 1, women had a higher mean HAI between the ages 40 and 59 years, while men had a higher prevalence of unhealthiest aging status across all age subgroups.
Association of healthy aging index with all-cause mortality
During follow-up, 14,112 all-cause deaths were documented. Absolute mortality rates according to HAI categories were 1.40, 2.86, 4.92, and 9.42 deaths per 1000 person-years for participants with a score of 0–2, 3–4, 5–6, and 7–10, respectively (Table 2). As shown in Table 2, each HAI component was significantly associated with all-cause mortality; after further adjustment, the magnitude of associations was slightly attenuated in models 2 and 3. Among all components, serum random glucose and cystatin C were most strongly associated with mortality. When all 5 components were combined, the multivariate-adjusted HRs for participants scoring 3–4, 5–6, and 7–10, as compared with those scoring 0–2, were 1.31 (1.22, 1.40), 1.60 (1.49, 1.72), and 2.28 (2.11, 2.46) (P for trend < 0.001). Each 1-point increase in HAI was associated with a 17% higher risk of all-cause mortality (HR 1.17; 95%CI 1.15, 1.18). As presented in Kaplan–Meier survival curves, there was a graded decrease in the survival probabilities as HAI increased, and the difference between the HAI categories in survival probability over time was larger in men and increased with baseline age (eFig. 3). For participants with healthy aging status (scoring 3–10), the PAR of all-cause mortality was 29.8% (95% CI 25.6%, 33.8%), suggesting that approximately one-third of the deaths might have been prevented if all participants had not been in the healthy aging status, regardless of chronological age. Estimates of the PAR for the alternative levels of HAI or individual components can be found in eTable 4. In addition, we found potential evidence of a non-linear dose-response association between HAI and mortality risk (P non-linearity < 0.0001, eFig. 4).
Association of healthy aging index with cause-specific mortality
Over the follow-up period, 2848 (0.7%) participants died from cardiovascular disease, 8107 (2.1%) from cancer, 530 (0.1%) from digestive disease, 757 (0.2%) from respiratory disease, 369 (0.1%) from infectious disease, and 575 (0.2%) from neurodegenerative disease. A strong graded increase in the risk of cause-specific mortality was also observed across the HAI categories (Table 3). For each unit increment of the HAI, the corresponding HRs for risk of death were 1.28 (1.25, 1.31) for cardiovascular diseases, 1.09 (1.07, 1.10) for cancer, 1.36 (1.29, 1.44) for digestive disease, 1.42 (1.35, 1.48) for respiratory disease, 1.42 (1.33, 1.51) for infectious diseases, 1.15 (1.09, 1.21) for neurodegenerative disease, and 1.33 (1.28, 1.38) for all other causes. The PAR of cause-specific mortality ranged from 17.1 to 86.7% for participants who had a relatively higher HAI of 3–10, and the reclassification of HAI groups yielded similar estimates (eTable 4). Furthermore, we found linear associations with the risk of death for cardiovascular diseases (P non-linearity = 0.059), cancer (P non-linearity = 0.100), digestive disease (P non-linearity = 0.720), neurodegenerative disease (P non-linearity = 0.822), and infectious disease (P non-linearity = 0.741), and non-linear associations with respiratory disease (P non-linearity = 0.022) and all other cause (P non-linearity < 0.001) (eFig. 4).
Subgroup analyses
For all-cause mortality, the effect estimates were stronger among younger adults (< 60 years) than among older adults (≥ 60 years; P interaction < 0.0001; Fig. 2). Compared with the reference group (HAI 0–2), the group with the HAI of 7–10 had a 1.15-fold greater risk of mortality in adults aged ≥ 60 years, while the HRs decreased to 1.19 in adults aged < 60 years. The association was also significantly different between men and women, with men generally having higher HRs associated with HAI than women (P interaction < 0.0001; Fig. 3). In analyses of cause-specific mortality, stratified analyses by age showed that the association of the HAI persisted in both age groups, but the association was larger in participants aged < 60 years than participants aged ≥ 60 years for cancer mortality (Fig. 2). In addition, there was a significant difference in the association of the HAI with the risk of mortality from cardiovascular diseases (P interaction = 0.047) and cancer (P interaction < 0.0001) between men and women, the difference in the effect estimates was not clinically meaningful (Fig. 3).
The association of HAI with all-cause and cause-specific mortality by age. Models were adjusted for age, sex, UKB center, education level, TDI, alcohol intake, smoking status, physical activity, medications (lowing cholesterol, hormone, oral pills), and chronic conditions (cardiovascular disease, cancer, respiratory disease, digestive disease, neurogenerative disease, infectious disease)
The association of HAI with all-cause and cause-specific mortality by sex. Models were adjusted for age, UKB center, education level, TDI, alcohol intake, smoking status, physical activity, medications (lowing cholesterol, hormone, oral pills), and chronic conditions (cardiovascular disease, cancer, respiratory disease, digestive disease, neurogenerative disease, infectious disease)
Notably, significant interactions between HAI and smoking status were observed in mortality outcome (P = 0.026 for interaction in all participants; P < 0.0001 for interaction in women) (eTable 5). The test for the interaction item of physical activity was also statistically significant (P = 0.004 for interaction in all participants; P = 0.021 for interaction in women). In subgroup analyses with stratification by these covariates, the effect sizes between HAI and all-cause mortality were somewhat stronger among regular smokers (versus never or former smokers) and adults with high MET hours (versus low or moderate MET hours). However, the associations between HAI and mortality risk were similar across subgroups stratified according to alcohol intake and BMI (eTable 5).
Sensitivity analyses
In the sensitivity analyses, the associations of the HAI with all-cause and cause-specific mortality did not change appreciably with additional adjustment for blood lipids, or additional adjustment for dietary factors (eTable 6). After excluding participants with diabetes, hypertension, cardiovascular disease, cancer, respiratory disease, digestive disease, neurodegenerative disease, or infectious disease at baseline, the association of the HAI with all-cause mortality and cause-specific mortality showed small to moderate changes (eTable 7). The most apparent attenuation of associations occurred in mortality risk after participants who had any of the five aforementioned diseases at baseline were removed from the analyses, but these significant associations persisted. Among relatively healthy participants, the HR for all-cause mortality per unit increment in the HAI was 1.12 (1.09, 1.14). The exclusion of people from the analyses who were current smokers, current drinkers, with missing covariates, or died during the first 5 years of follow-up only changed the HRs slightly.
Discussion
In this large-scale prospective UK cohort, we constructed a 5-item HAI to characterize healthy aging levels. Higher HAI was significantly associated with an increased risk of all-cause and cause-specific mortality with the highest risk from respiratory diseases and the lowest risk from cancer, even after adjustment for chronological age and other known risk factors. In addition, we found that the effect sizes decreased with chronological age, indicating that interventions to slow the biological aging to prevent premature death at an earlier stage of life course might be more effective.
The strength of association of the HAI with all-cause mortality reported in the present study is in line with previous research in smaller cohorts of older adults (> 60 years), primarily in the US and China [8,9,10,11,12,13]. Our finding of a HR for all-cause mortality of 1.15 for participants aged > 60 years and 1.19 for those aged < 60 years, for one point higher HAI, in our fully adjusted model, is in agreement with observations from the Framingham Offspring Study of 934 subjects (> 60 years), which reported that per unit higher of the 5-item HAI was, after adjustment, associated with a HR of 1.15 for all-cause mortality [10]. Furthermore, our findings for all-cause mortality are also comparable to those reported in the National Health and Nutrition Examination Survey, the Cardiovascular Health Study, and the Health, Aging, and Body Composition Study, with a HR of 1.19, 1.17, and 1.19, respectively. [8, 11, 13] However, China Health and Retirement Longitudinal Study (n = 3740) suggested that each point increase in HAI was associated with a 28% higher mortality risk in older adults (> 60 years) [12]. A potential reason for this observation may be that the measurements of HAI in the Wu et al. [8] study included C-reactive protein additionally, which is a measurement of overall inflammation rather than specific to a particular organ system as the traditional definition of HAI, leading to an overestimated effect on mortality. While another Chinese cohort, the Rugao Longevity and Ageing Study (n = 1719), has found that the HRs per unit increment of the HAI for all-cause mortality were 1.11 (95% CI 1.05–1.18), partially due to the selection criteria of participants aged 70 years or older [9]. These studies, including ours, collectively showed that public efforts to understand and promote a healthy aging status in the whole population will lead to an overall reduction in mortality risk.
Compared with all-cause mortality, we found that the HAI was more strongly associated with mortality from cardiovascular diseases, digestive diseases, respiratory diseases, infectious diseases, and all other causes. To our knowledge, only one study has analyzed the relationships between HAI and cause-specific mortality, suggesting that each point increase in HAI was associated with a 23% higher cardiovascular mortality risk while no significant association with cancer mortality [8]. This is partially similar to our finding that per unit higher HAI was associated, in the fully adjusted model, with a HR of 1.28 for mortality risk from cardiovascular diseases. However, in our study, the association between the HAI and the risk of death from cancer remained even after we excluded participants with cancer at baseline or those who died during the first 5 years of follow-up. Findings on cancer mortality warrant further confirmation because of inconsistency between study results [8]. The excess risk for cause-specific mortality may be partially due to reduced immunocompetence, progressive deterioration of organ function, or decreased likelihood of cure among people with higher HAI, leading to the development of diseases that caused death. For instance, some of the excess mortality from digestive diseases may be owing to gut dysbiosis associated with healthy aging status, which triggers the innate immune response and chronic low-grade inflammation, leading to many age-related degenerative pathologies, all together contributing to the development of digestive diseases [31,32,33]. As a whole, our findings support the notion that healthy aging status, which could be reflected by HAI, may have protean protective effects on all these specific systems to promote longevity.
Although the HAI has been applied in the UK Biobank with a positive effect on major vascular events [15], this is the first attempt to associate the HAI with mortality in the European population, which includes a considerably younger age range than previous studies [8,9,10,11,12,13]. Little is known about whether HAI is related to mortality risk in y ADDIN EN.CITE [15]ounger populations. We observed that in these associations for all-cause and cancer mortality, the effect estimates were moderately stronger among younger adults (< 60 years) than that among older adults (≥ 60 years). Therefore, the use of a continuous HAI as a surrogate for biological age is more sensitive in younger adults who are at the lower end of the aging spectrum, which is meaningful for the prevention of premature death and the extension of healthy life expectancy. As longevity is a complex trait determined by a combination of genetics, environment, and stochasticity, accelerated aging may play a more critical role in younger participants (< 60 years) who lives longer, while deaths in elders (≥ 60 years) may occur more stochastically [34]. Such findings suggest that more studies focusing on healthy aging across the age spectrum and the development of relevant screening and intervention strategies are needed.
It is well known that women live longer than men, while the reasons are still largely unknown. Sex gap in healthy aging and survival prospects was also noticed in this study, which are often attributed to cultural differences (e.g., lifestyle factors and poor social status) in common thinking [35, 36]. However, after we adjusted for these confounders, the association between healthy aging and death was still stronger in men than in women. We assumed that biological factors, such as sex hormones and telomere shortening, may at least partly contribute to such sex differences [37,38,39]. For instance, estrogen has been related to lower risks of various life-threatening diseases, while testosterone has been associated with higher risks [40]. In addition, compared with women, men have greater telomere shortening, which is associated with accelerated aging [38, 41]. Further studies focusing on the underlying mechanism of the sex differences in unhealthy aging and death are warranted.
The finding that the HAI was able to stratify the risk of mortality even among apparently healthy adults, with no clinically diagnosed chronic conditions, is also novel. The HAI, which measures the burden of subclinical disease in multiple physiological systems, may therefore provide a complementary explanation of the variation in survival in clinically healthy adults. Compared with the biological age based on 72 biomarkers [5] and the frailty index based on 49 items [6], which have shown significant associations with mortality risk, the HAI has better performance with relative affordability and practicality. We also found that unhealthy lifestyle factors such as smoking and low physical activity level may further increase the detrimental impacts of HAI on mortality risk, indicating the positive influence of smoking cessation and regular exercise to delay aging [42,43,44]. Therefore, in a clinical setting, HAI may be a marker which tracks the effect of aging before diseases occurred to stratify risk, especially among younger adults and men as well as individuals who smoke regularly and lack exercise.
The present study has several strengths. First, this study was a large-scale prospective cohort study (n = 387,794) based on data from a geographically and socioeconomically diverse population in the UK. The inclusion of 222,664 adults younger than 60 years with a median follow-up of 8.9 years allowed a thorough analysis of cause-specific mortality in younger adults. Second, since measures of several potential confounding factors (personal, lifestyle, and chronic conditions) were available, we were able to adjust for these factors in our models. Thirdly, several sensitivity analyses were performed to confirm our findings. Finally, we constructed the HAI using objectively measured traits, which have been suggested to be more robust than self-reported health measures obtained from questionnaire information. It is worth noting that there are intricate connections between various health markers. Therefore, it is important to establish the HAI combining these various markers, which could be associated with human health or disease risk in a more concerted manner compared to just looking at these concepts individually. From the perspective of public health, the use of the simple scoring algorithm makes the results of epidemiological research easier to be interpreted and translated into practice, thereby being more informative for the general population. Despite these strengths, our study had some limitations. First, the assessment of HAI components was conducted only at one time point at baseline. The healthy aging status might have altered over the follow-up period, which could result in an underestimate of the magnitude of the true association. Second, although in our study we considered a variety of potential confounding factors, including personal variables, lifestyle factors, and history of chronic conditions, residual and unmeasured confounding might have influenced the association. Third, a large proportion of participants were excluded based on missing data in the present study, which may lead to selection bias. However, we have conducted a sensitivity analysis and found that the baseline characteristics of these participants excluded are similar to our analytic sample (eTable 8). Finally, as a prospective cohort, the UK Biobank was not representative of the general UK population. Therefore, the generalizability to the broader UK population or the populations of other races and ethnicities outsides the UK should be made with caution.
Our findings from the large prospective cohort study of the UK population for the first time show the independent associations between the HAI and the risk of all-cause and cause-specific mortality, with a stronger association in younger adults (< 60 years) than that in older adults (≥ 60 years). Our results suggest that the HAI is a better predictor of mortality in younger adults than in those older. Further research is needed to explore the use of these routine clinical measures in clinical settings in identifying individuals whose biological age exceeds their chronological age, especially among younger adults. The identification of high-risk individuals may facilitate the development of effective intervention strategies to prevent premature death and improve the quality of life.
Data availability
UKB data are available in a public, open-access repository. This research has been conducted using the UKB Resource under Application Number 44430. The UKB data are available on application to the UK Biobank (http://www.ukbiobank.ac.uk/).
References
Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. 2019;4:e159–67. https://doi.org/10.1016/s2468-2667(19)30019-2.
United Nations, Department of Economic and Social Affairs, Population Division (2019) World Population Prospects 2019: highlights. ST/ESA/SER.A/423.
Hamczyk MR, Nevado RM, Barettino A, Fuster V, Andrés V. Biological versus chronological aging: JACC Focus Seminar. J Am Coll Cardiol. 2020;75:919–30. https://doi.org/10.1016/j.jacc.2019.11.062.
Jylhävä J, Pedersen NL, Hägg S. Biological age predictors. EBioMedicine. 2017;21:29–36. https://doi.org/10.1016/j.ebiom.2017.03.046.
Chan MS, Arnold M, Offer A, Hammami I, Mafham M, Armitage J, Perera R, Parish S. A Biomarker-based biological age in UK Biobank: composition and prediction of mortality and hospital admissions. J Gerontol A Biol Sci Med Sci. 2021;76:1295–302. https://doi.org/10.1093/gerona/glab069.
Williams DM, Jylhävä J, Pedersen NL, Hägg S. A frailty index for UK Biobank participants. J Gerontol A Biol Sci Med Sci. 2019;74:582–7. https://doi.org/10.1093/gerona/gly094.
Newman AB, Boudreau RM, Naydeck BL, Fried LF, Harris TB. A physiologic index of comorbidity: relationship to mortality and disability. J Gerontol A Biol Sci Med Sci. 2008;63:603–9. https://doi.org/10.1093/gerona/63.6.603.
Wu C, Smit E, Sanders JL, Newman AB, Odden MC. A modified healthy aging index and its association with mortality: the National Health and Nutrition Examination Survey, 1999–2002. J Gerontol A Biol Sci Med Sci. 2017;72:1437–44. https://doi.org/10.1093/gerona/glw334.
Zhang H, Zhu Y, Hao M, Wang J, Wang Z, Chu X, et al. The modified healthy ageing index is associated with mortality and disability: the Rugao Longevity and Ageing Study. Gerontology. 2021;67:572–80. https://doi.org/10.1159/000513931.
McCabe EL, Larson MG, Lunetta KL, Newman AB, Cheng S, Murabito JM. Association of an index of healthy aging with incident cardiovascular disease and mortality in a community-based sample of older adults. J Gerontol A Biol Sci Med Sci. 2016;71:1695–701. https://doi.org/10.1093/gerona/glw077.
Sanders JL, Minster RL, Barmada MM, Matteini AM, Boudreau RM, Christensen K, et al. Heritability of and mortality prediction with a longevity phenotype: the healthy aging index. J Gerontol A Biol Sci Med Sci. 2014;69:479–85. https://doi.org/10.1093/gerona/glt117.
Wu C, Newman AB, Dong BR, Odden MC. Index of healthy aging in Chinese older adults: China Health and Retirement Longitudinal Study. J Am Geriatr Soc. 2018;66:1303–10. https://doi.org/10.1111/jgs.15390.
Sanders JL, Boudreau RM, Penninx BW, Simonsick EM, Kritchevsky SB, Satterfield S, Harris TB, Bauer DC, Newman AB. Association of a modified physiologic index with mortality and incident disability: the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2012;67:1439–46. https://doi.org/10.1093/gerona/gls123.
Office for National Statistics. Population estimates for UK, England and Wales, Scotland and Northern Ireland: Mid 2020. Newport: Office for National Statistics; 2021.
Huang N, Zhuang Z, Song Z, Wang W, Li Y, Zhao Y, et al. Associations of modified healthy aging index with major adverse cardiac events, major coronary events, and ischemic heart disease. J Am Heart Assoc. 2023;12:e026736. https://doi.org/10.1161/jaha.122.026736.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779. https://doi.org/10.1371/journal.pmed.1001779.
Allen NE, Sudlow C, Peakman T, Collins R. UK Biobank data: come and get it. Sci Transl Med. 2014;6:224ed224. https://doi.org/10.1126/scitranslmed.3008601.
Collins R. What makes UK Biobank special? Lancet. 2012;379:1173–4. https://doi.org/10.1016/s0140-6736(12)60404-8.
Fawns-Ritchie C, Deary IJ. Reliability and validity of the UK Biobank cognitive tests. PLoS One. 2020;15:e0231627. https://doi.org/10.1371/journal.pone.0231627.
Classification and diagnosis of diabetes. standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S15-s33. https://doi.org/10.2337/dc21-S002.
Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:28–36. https://doi.org/10.1001/jamainternmed.2017.6015.
Metter EJ, Schrager M, Ferrucci L, Talbot LA. Evaluation of movement speed and reaction time as predictors of all-cause mortality in men. J Gerontol A Biol Sci Med Sci. 2005;60:840–6. https://doi.org/10.1093/gerona/60.7.840.
Batterham PJ, Bunce D, Mackinnon AJ, Christensen H. Intra-individual reaction time variability and all-cause mortality over 17 years: a community-based cohort study. Age Ageing. 2014;43:84–90. https://doi.org/10.1093/ageing/aft116.
Hart A, Blackwell TL, Paudel ML, Taylor BC, Orwoll ES, Cawthon PM, Ensrud KE. Cystatin C and the risk of frailty and mortality in older men. J Gerontol A Biol Sci Med Sci. 2017;72:965–70. https://doi.org/10.1093/gerona/glw223.
Emberson JR, Haynes R, Dasgupta T, Mafham M, Landray MJ, Baigent C, Clarke R. Cystatin C and risk of vascular and nonvascular mortality: a prospective cohort study of older men. J Intern Med. 2010;268:145–54. https://doi.org/10.1111/j.1365-2796.2010.02214.x.
Sorkin JD, Muller DC, Fleg JL, Andres R. The relation of fasting and 2-h postchallenge plasma glucose concentrations to mortality: data from the Baltimore Longitudinal Study of Aging with a critical review of the literature. Diabetes Care. 2005;28:2626–32. https://doi.org/10.2337/diacare.28.11.2626.
Lee HM, Le H, Lee BT, Lopez VA, Wong ND. Forced vital capacity paired with Framingham Risk Score for prediction of all-cause mortality. Eur Respir J. 2010;36:1002–6. https://doi.org/10.1183/09031936.00042410.
O’Connell MDL, Marron MM, Boudreau RM, Canney M, Sanders JL, Kenny RA, Kritchevsky SB, Harris TB, Newman AB. Mortality in relation to changes in a healthy aging index: the Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2019;74:726–32. https://doi.org/10.1093/gerona/gly114.
Pazoki R, Dehghan A, Evangelou E, Warren H, Gao H, Caulfield M, Elliott P, Tzoulaki I. Genetic predisposition to high blood pressure and lifestyle factors: associations with midlife blood pressure levels and cardiovascular events. Circulation. 2018;137:653–61. https://doi.org/10.1161/circulationaha.117.030898.
Wang M, Zhou T, Li X, Ma H, Liang Z, Fonseca VA, Heianza Y, Qi L. Baseline vitamin D status, sleep patterns, and the risk of incident type 2 diabetes in data from the UK Biobank Study. Diabetes Care. 2020;43:2776–84. https://doi.org/10.2337/dc20-1109.
Salazar N, Valdés-Varela L, González S, Gueimonde M, de Los Reyes-Gavilán CG. Nutrition and the gut microbiome in the elderly. Gut Microbes. 2017;8:82–97. https://doi.org/10.1080/19490976.2016.1256525.
Clements SJ, Carding SR. Diet, the intestinal microbiota, and immune health in aging. Crit Rev Food Sci Nutr. 2018;58:651–61. https://doi.org/10.1080/10408398.2016.1211086.
Kim S, Jazwinski SM. The gut microbiota and healthy aging: a mini-review. Gerontology. 2018;64:513–20. https://doi.org/10.1159/000490615.
Carmona JJ, Michan S. Biology of healthy aging and longevity. Rev Invest Clin. 2016;68:7–16.
Luy M, Gast K. Do women live longer or do men die earlier? Reflections on the causes of sex differences in life expectancy. Gerontology. 2014;60:143–53. https://doi.org/10.1159/000355310.
Rochelle TL, Yeung DK, Bond MH, Li LM. Predictors of the gender gap in life expectancy across 54 nations. Psychol Health Med. 2015;20:129–38. https://doi.org/10.1080/13548506.2014.936884.
Clocchiatti A, Cora E, Zhang Y, Dotto GP. Sexual dimorphism in cancer. Nat Rev Cancer. 2016;16:330–9. https://doi.org/10.1038/nrc.2016.30.
Barrett EL, Richardson DS. Sex differences in telomeres and lifespan. Aging Cell. 2011;10:913–21. https://doi.org/10.1111/j.1474-9726.2011.00741.x.
Santoro A, Ostan R, Candela M, Biagi E, Brigidi P, Capri M, Franceschi C. Gut microbiota changes in the extreme decades of human life: a focus on centenarians. Cell Mol Life Sci. 2018;75:129–48. https://doi.org/10.1007/s00018-017-2674-y.
Ostan R, Monti D, Gueresi P, Bussolotto M, Franceschi C, Baggio G. Gender, aging and longevity in humans: an update of an intriguing/neglected scenario paving the way to a gender-specific medicine. Clin Sci (Lond). 2016;130:1711–25. https://doi.org/10.1042/cs20160004.
Yip BW, Mok HO, Peterson DR, Wan MT, Taniguchi Y, Ge W, Au DW. Sex-dependent telomere shortening, telomerase activity and oxidative damage in marine medaka Oryzias melastigma during aging. Mar Pollut Bull. 2017;124:701–9. https://doi.org/10.1016/j.marpolbul.2017.01.021.
Sanchez-Sanchez JL, Izquierdo M, Carnicero-Carreño JA, García-García FJ, Rodríguez-Mañas L. Physical activity trajectories, mortality, hospitalization, and disability in the Toledo Study of Healthy Aging. J Cachexia Sarcopenia Muscle. 2020;11:1007–17. https://doi.org/10.1002/jcsm.12566.
Stenholm S, Head J, Kivimäki M, Kawachi I, Aalto V, Zins M, et al. Smoking, physical inactivity and obesity as predictors of healthy and disease-free life expectancy between ages 50 and 75: a multicohort study. Int J Epidemiol. 2016;45:1260–70. https://doi.org/10.1093/ije/dyw126.
Daskalopoulou C, Koukounari A, Wu YT, Terrera GM, Caballero FF, de la Fuente J, et al. Healthy ageing trajectories and lifestyle behaviour: the Mexican Health and Aging Study. Sci Rep. 2019;9:11041. https://doi.org/10.1038/s41598-019-47238-w.
Funding
The study was supported by grants from the National Key R&D Program of China (2020YFC2003401), the National Natural Science Foundation of China (82173499), and the High-Performance Computing Platform of Peking University. The funders had no role in the study design, data collection, data analysis and interpretation, writing of the report, or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
T. H. and L. Q. designed the research. Z. Z. and T. H. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Z. Z. wrote the paper and performed the data analysis. All authors contributed to the statistical analysis, critically reviewed the manuscript during the writing process, and approved the final version to be published. Z. Z. and T. H. are the guarantors for the study.
Corresponding authors
Ethics declarations
Ethics approval
The UKB study was approved by the National Information Governance Board for Health and Social Care in England and Wales, the Community Health Index Advisory Group in Scotland, and the North West Multicenter Research Ethics Committee. All participants gave written informed consent. This UKB study was also approved by the Ethical Committee of Peking University (Beijing, China).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Zhuang, Z., Zhao, Y., Huang, N. et al. Associations of healthy aging index and all-cause and cause-specific mortality: a prospective cohort study of UK Biobank participants. GeroScience 46, 1241–1257 (2024). https://doi.org/10.1007/s11357-023-00891-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-023-00891-6