Abstract
Maternal protein restriction (MPR) in pregnancy causes life course organ dysfunction, but few studies link the developmental origins of disease hypothesis to early aging. Suboptimal developmental nutrition increases oxidative stress (OS) and male infertility, damaging sperm function. We hypothesized that MPR in pregnancy accelerates age-related changes in testicular and sperm function related to both maternal diet and increased testicular OS in rat offspring. We studied male rats whose pregnant mothers ate either control (C, 20 % casein) or restricted (R, 10 % casein) isocaloric diet. After birth, mothers and offspring ate C diet. Testes were retrieved at 19 days gestation and across the life course (postnatal day (PND) 21, 36, 110, and 850) to measure OS markers, antioxidant enzymes, serum FSH, LH, and testosterone, and PND 110 sperm OS and quality. Fertility rate was evaluated at PND 110, 450, and 850. Offspring showed age- and MPR-related changes in testosterone, testicular OS markers and antioxidant enzymes and fertility, and maternal diet-related OS and sperm antioxidant enzyme changes. Developmental programming is considered a key factor in predisposing to chronic disease. Our data show that programming also plays an important role in aging trajectory. This interaction is a little studied area in aging biology that merits more investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suboptimal maternal nutrition occurring in critical windows of embryo, fetal, and neonatal life alters organ development modifying adult phenotype and predisposing to early onset of organ dysfunction and chronic diseases (Gluckman et al. 2005). These important effects of the environment on lifetime health are termed developmental programming defined as the response to a specific challenge in a critical time window during the plastic fetal and neonatal periods that alters offspring development by gene-environment interactions with persistent effects on phenotype. Decreased nutrition in development is also thought to accelerate aging and shorten life span (Ozanne and Hales 2004; Tarry-Adkins and Ozanne 2011). Human epidemiological and experimental animal studies have shown that developmental programming affects the risk of developing diseases during adulthood and correlates with the quality of the maternal diet and availability of nutrients during development (McMullen and Mostyn 2009). With regard to reproduction, controlled animal studies indicate that several reproductive disorders are influenced by adverse factors during intrauterine development and postnatal growth (Davies and Norman 2002). Protein restriction during perinatal development delays sexual maturation and decreases reproductive capacity in female offspring (Guzman et al. 2006). Maternal undernutrition alters male offspring reproductive function at multiple levels critical to normal reproductive function: decreased pituitary function and GnRH sensitivity, Sertoli cell number, sperm motility and count, and increased numbers of sperm exhibiting morphological abnormalities in adulthood. These changes lead to delayed Sertoli cell maturation and germ cell differentiation, including alterations of intratubular organization that likely contribute to the observed low fertility rate (Aitken and Roman 2008; Rae et al. 2002a; Rae et al. 2002b; Rodríguez-González et al. 2012; Toledo et al. 2011). Males who experienced maternal protein restriction during fetal life and pre-weaning, although receiving a control diet after weaning, show delayed testicular descent, low serum LH and testosterone, reduced sperm count, and impaired reproductive capacity (Zambrano et al. 2005b). In contrast to the extensive literature on the existence of developmental programming of reproductive dysfunction, there are virtually no studies addressing the effects of developmental programming by maternal nutrition on the rate of aging of the male reproductive system. Such studies require similar data to be collected over multiple stages of the life course.
Suboptimal nutrition during early stages of development is associated with increased oxidative stress (OS) (Franco et al. 2007; Luo et al. 2010). Thus, we hypothesize that OS is likely to be a major factor among the multifactorial causes of both normal and potentially accelerated age-related male infertility (Agarwal et al. 2003; Sikka 1996). Oxidative stress may act either directly through modulation of gene expression or indirectly via the disruptive effects of oxidized molecules (Luo et al. 2006; Luo et al. 2010); however, a correlation between maternal malnutrition and offspring infertility associated with OS has not been clearly established.
The study reported here addressed two related questions. First, we wished to determine developmental programming effects of an isocaloric, low-protein maternal diet on key components of fetal and postnatal male reproductive function across the life span. These factors include the gonadotropins that regulate testicular function and testosterone production. We related these changes to levels of the enzyme glutathione peroxidase and superoxide dismutase since these are the most important antioxidant enzymes produced in germ cells and Sertoli and Leydig cells. Secondly, by studying five stages of the life course, we were able to evaluate the extent to which the maternal low-protein diet accelerates aging of various male offspring reproductive functions and the association of age-related changes with the ROS mechanisms evaluated. We hypothesized that maternal protein restriction during pregnancy impairs later life testicular and sperm function leading to accelerated aging related to both maternal diet and increased testicular OS in male rat offspring. Our aim was to provide firm data for the novel hypothesis that developmental programming accelerates the trajectory of aging of male reproductive function.
Materials and methods
Care and maintenance of animals
All procedures were approved by the Animal Experimentation Ethics Committee of the Instituto Nacional de Ciencias Médicas y Nutrición, Salvador Zubirán (INNSZ), Mexico, and in accordance with the guidelines of Mexican law on animal protection (NOM-062-ZOO-1999). Details of maternal diet, breeding, and management of offspring groups have been previously described in detail (Zambrano et al. 2005b). Briefly, at the age of 4 months, 28 female Wistar rats weighing between 220 and 260 g were obtained from the INNSZ animal colony and maintained under controlled lighting (lights on from 7:00 am to 7:00 pm at 22–23 °C). Female rats were mated overnight with proven male breeders. The day on which spermatozoa were detected in a vaginal smear was designated as conception day 0. Only rats that were pregnant within 5 days of mating with males were studied. Pregnant rats were transferred to individual cages and allocated at random to one of two groups. The control group (group C) (n = 14) was fed with 20 % casein containing 20.0 % protein, 65.0 % carbohydrates, 5.0 % lipids, 5.0 % fiber, 3.5 % minerals, and 1.0 % vitamins (w/w), energy 3.85 kcal g−1 and the restricted group (n = 14) with 10 % casein isocaloric diet (group R) containing 10 % protein, 75.2 % carbohydrates, 5.0 % lipids, 5.0 % fiber, 3.5 % minerals, and 1.0 % vitamins (w/w), energy 3.85 kcal g−1 (Zambrano et al. 2005a; Zambrano et al. 2005b). Food and water were available ad libitum. At 19 days of gestation (dG) between 12.00 and 14.00 h after food withdrawal for 6 h, eight mothers from each group were euthanized by decapitation, using a rodent guillotine (Thomas Scientific, NJ) by trained experienced personnel, to obtain fetal testes, which were isolated, weighed, and pooled per litter and immediately frozen in liquid nitrogen. Delivery of the six remaining rats in each group occurred on post-conceptual day 22. The day of delivery was considered as postnatal day (PND) 0. All rats were delivered vaginally and offspring anogenital distance was measured with calipers for gender identification as previously described (Zambrano et al. 2006). To ensure homogeneity, only litters between 12 and 15 pups were studied. Litters were adjusted to 12 pups for each mother while maintaining as close to a 1:1 sex ratio as possible. After birth, all mothers were fed with C diet. The time line of the study is shown in Fig. 1.
Postnatal maintenance
After weaning (PND 21), both male and female pups were separated into groups of three to four per cage and fed rodent chow diet (Zeigler Rodent RQ 22–5, USA) containing 22.0 % protein, 62.0 % carbohydrates, 5.0 % lipids, 4.0 % fiber, 6.0 % minerals, and 1.0 % vitamins (w/w), energy 4.0 kcal g−1, until the end of the study ad libitum. Only data on male offspring are reported. At PND 21, 36, 110, and 850, after 6 h of fasting, rats were decapitated between 12.00 and 14.00 h of the day.
For each age group, blood was collected, centrifuged, and serum frozen until assayed. Testes were dissected, cleaned from fat, weighed, frozen, and stored at −70 °C until analyzed. The epididymal fat pads were dissected and weighed individually. At PND 110, the cauda epididymis and vas deferens were rapidly removed and placed in saline at 37 °C to release sperms by clearing out the vas deferens with tweezers and by triturating the cauda epididymis with scissors.
Tissue and sample preparation
Testes were homogenized in saline at 4 °C and aliquots obtained and frozen at −70 °C for later protein quantification using the Bradford method and for determination of biomarkers of oxidative stress (ROS and antioxidant enzymes). Lipid peroxidation was determined at the time of testicular homogenization and sperm release. All determinations were performed in duplicate and averaged for statistical analysis.
Sperm aliquots containing 5 × 106 and 10 × 106 spermatozoa underwent six thermal shock cycles from −70 °C to 45 °C, sonication for 2 min with six intervals of 20 s each and were then placed in ice and frozen at −70 °C until quantification of ROS and antioxidant enzymes.
Hormone measurements
Serum follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels were determined by double antibody radioimmunoassay (RIA) using standard and specific anti-rat LH antibodies from the National Institute of Diabetes, Digestive Kidney Diseases. FSH and LH were iodinated by the chloramine-T method, following separation of protein-bound and free [125I] by Sephadex G-100. Results are expressed as NIDDK-rat-FSH-RP2 and NIDDK-rat-LH-RP3. The intra- and inter-assay coefficients of variations were <4 and <7.9 and <5.1 and <6.5, respectively (Zambrano et al. 2005b).
Serum testosterone was determined using a commercial rat kit, DPC Coat-a-Count (TKTT1) from Diagnostic Products (Los Angeles, USA). The intra-and inter-assay variability was <8.17 and <8.83, respectively (Zambrano et al. 2005b).
Lipid peroxidation assay
Lipid peroxidation was determined the same day on which testes were homogenized and sperm were obtained. Aliquots containing 5 million of sperm were adjusted with saline to 100 μl, no thermal shock and sonication were needed. Lipid peroxidation was determined in 100 μl aliquots of either homogenized testes or 5 × 106 sperm by measuring malondialdehyde (MDA) by the thiobarbituric acid-reactive substances assay (TBARS). All samples were read in a plate at 532 nm in a PerkinElmer LS50-B luminescence spectrometer. Results were expressed as nanomole MDA per milligram of protein or nmol MDA per 5 x 106 sperm (Vega et al. 2013). Intra- and inter-assay coefficients of variation were <6 and <8 %, respectively.
Reactive oxygen species assay
Homogenized testes, 5 μl aliquots containing 5 × 106 sperm were used to determine reactive oxygen species (ROS). A standard curve was obtained using increasing concentrations of 2′,7′-dichlorofluorescein (DCF) and incubated in parallel with the samples (37 °C for 60 min). At the end of the incubation period, fluorescent signals at an excitation wavelength of 488 nm and an emission wavelength of 525 nm were recorded in a PerkinElmer LS50-B luminescence spectrometer. Results were expressed as nanomoles of DCF formed per milligram of protein per minute or DCF formed per 5 x 106 sperm per minute (Vega et al. 2013).
Superoxide dismutase activity
Superoxide dismutase (SOD) activity was determined in 10 μl aliquots of homogenized testes or 5 x 106 sperm with a RANSOD kit (Randox Laboratories limited, UK). A standard curve was obtained according to the manufacturer’s instructions. All samples were read in a plate at 505 nm in a PerkinElmer LS50-B luminescence spectrometer at 0, 30 s, and 3 min at 37 °C. Results were expressed as units of activity per milligram of protein or as units of activity per 5 x 106 sperm (Vega et al. 2013).
Glutathione peroxidase activity
Glutathione peroxidase (GPx) activity was determined in 10 μl aliquot of homogenized testes or 10 x 106 sperm with the RANSEL kit (Randox Laboratories limited, UK). All samples were read in a plate at 304 nm in a PerkinElmer LS50-B luminescence spectrometer at basal 1, 2, and 3 min at 37 °C. Results were expressed as milliunits per milligram of protein or milli units per 10 x 106 sperm (Vega et al. 2013).
Sperm measurements
Sperm viability was assessed by mixing 10 μl of saline (0.90 % w/v of NaCl) containing spermatozoids with 10 μl of eosin. Live spermatozoa were identified by membrane integrity, which prevents the spermatozoa from being stained with eosin, whereas the dead sperm were easily identified after staining as previously described (Bjorndahl et al. 2003; WHO 2010). Two hundred cells were counted under a light microscope. Results were expressed as the percentage of live cells. Sperm concentration and motility were evaluated with a computerized sperm analyzer (Sperm Quality Analyzer). For sperm morphology, 10 μl of sample was taken, smeared, and subsequently stained using a quick staining kit for sperm morphology (FertiMexico S.A. de C.V, Mexico). Abnormal sperm morphology was classified as defects in the sperm head, midpiece, or tail. Head defects included large, small, tapered, pyriform, round, and amorphous heads, heads with a small acrosomal area and double heads. Midpiece defects included bent neck, asymmetrical insertion of the midpiece into the head, a thick or irregular midpiece, and an abnormally thin midpiece. Tail defects included short, multiple, hairpin, broken or bent tails, tails of irregular width, and coiled tails. For analysis of sperm abnormalities, 200 cells were counted under light microscope at ×40.
Evaluation of fertility rate
At PND 110, 450, and 850, one experimental male was placed for 1 week with two non-experimental group virgin females aged 4 months. Males were then separated from the females who were kept individually until day 15 of gestation. The male was considered fertile when at least one of the two females became pregnant. Results were expressed as the percentages of fertile males and pregnant females.
Statistical analysis
Two independent studies were performed; the first at 19 dG (n = 8 pregnant rats per group) in which fetal tissue from the same litter were pooled for analysis to provide 8 litters per group. The second study across the life span at PND 21 and 36, 110, 450, and 850 (n = 6 litters per group), one male per litter was chosen randomly to provide n = 6 rats. Two-way multiple analysis of variance (ANOVA) followed by Holm-Sidak was used to evaluate differences between C and R groups at the same age and within the same group but at different ages. Unpaired Student’s t test was used for differences in the sperm quality. Fertility rate was analyzed using χ 2. A p < 0.05 was considered significant. All data are presented as mean ± SEM.
Results
Body, testicular, and epididymal fat weight
No differences were observed in gender ratio of pups between litters from mothers fed with the different diets. At 19 dG, PND 21, 36, and 110, no statistical differences were found between groups in body weight, but at PND 850, body weight was higher in offspring from the R mothers compared with C (Fig. 2a). No differences were observed in testicular weight between C and R at all ages studied (Fig. 2b). The increase in body and testicular weight in both groups was related to age (Fig. 2a, b). There were no differences between C and R offspring in testicular weight relative to body weight at all ages studied: 19dG (C, 0.09 ± 0.01; R, 0.08 ± 0.01), PND 21 (C, 0.28 ± 0.01; R, 0.28 ± 0.01), PND 36 (C, 0.5 ± 0.02; R, 0.44 ± 0.02), PND 110 (C, 0.33 ± 0.02; R, 0.36 ± 0.01), and PND 850 (C, 0.28 ± 0.02; R, 0.28 ± 0.02) g*g body weight−1. At 110 PND, epididymal fat was similar in the two groups; however, at 850 PND, the epididymal fat was statistically heavier in R offspring, with no age-related changes in the C group (Fig. 2c).
Weight and hormone concentrations at different ages: a body weight, b testicular weight, c epididymal fat, d FSH, e LH, and f testosterone. Mean ± SEM, n = 8 for fetal tissue at 19 dG and n = 6 for different postnatal ages; control (C) open bars, restricted (R) closed bars. Analysis was by two-way ANOVA. p < 0.05 for data not sharing at least one letter on the same maternal diet. The asterisk on top of the closed bars indicates p < 0.05 vs control. dG days of gestation, d postnatal days
Hormone concentrations
At all PND evaluated, serum FSH levels were similar in C and R males (Fig. 2d); whereas at PND 110, serum LH was lower in R than C males with no differences between groups at the other ages studied (Fig. 2e). Serum testosterone was lower at PND 110 and 850 in R compared to C offspring (Fig. 2f). When hormone concentrations were analyzed within the same groups at different ages, serum FSH decreased with age only in the R males (Fig. 2d). Serum LH and testosterone levels increased at PND 110 in both groups (Fig. 2e, f) and dropped in both groups between 110 and 850 days (Fig. 2f). At PND 110, LH was lower in R than C, and at both PND 110 and 850, testosterone was lower in R than C.
Testicular oxidative stress biomarkers
At 19 dG and at PND 110 and 850, MDA concentrations were higher in testes of R compared to C offspring (Fig. 3a). Testicular ROS levels of R were higher than those from the C group at PND 110 and 850 (Fig. 3b). In regard to antioxidant enzyme activities in the testes, fetal SOD did not show any significant difference between 19 dG and at PND 110; however, at PND 21 and 36, the activity of this enzyme was lower in R compared to C males. In older rats (PND 850), SOD activity was higher in R than C males (Fig. 3c). Testicular GPx activity was higher at 19 dG in R males compared with C males, with no differences at PND 21, 36, and 110. However, by PND 850, GPx activity was higher in the testes from R offspring compared to C (Fig. 3d). When oxidative stress biomarkers were analyzed at different ages within groups, MDA levels were higher at PND 110 and 850 for R offspring and only at PND 850 for C compared with earlier ages (Fig. 3a). The ROS levels in both groups did not differ at early ages, but at PND 110 and 850, levels were similar and significantly higher than at earlier ages (Fig. 3b). For both groups, SOD activity was higher at 19 dG and PND 21 compared to PND 36. However, in the C group, SOD activity declined at PND 36 and further at PND 110 and 850; while in the R group, SOD activity declined at PND 36, 110, and 850 in comparison with PND 21 (Fig. 3c). In C males, GPx activity decreased at PND 36 compared to 19 dG; however, it increased at PND 110 with no further change at PND 850 in comparison with earlier ages. The same tendency was observed in the R group in which GPx activity was higher compared to the other ages at PND 850 (Fig. 3d).
Testicular oxidative stress biomarkers at different postnatal ages: a malondialdehyde (MDA), b reactive oxygen species, c superoxide dismutase (SOD), and d glutathione peroxidase (GPx). Mean ± SEM, n = 8 for fetal tissue at 19 dG and n = 6 for different postnatal ages; control (C) open bars, restricted (R) closed bars. Analysis was by two-way ANOVA. p < 0.05 for data not sharing at least one letter on the same maternal diet. The asterisk on top of the closed bars indicates p < 0.05 vs control. dG days of gestation, d postnatal days
Oxidative stress biomarkers in the sperm at PND 110
MDA and ROS levels were higher in sperm from R compared to C offspring (Fig. 4a, b). SOD activity was lower in sperm in the R group, while GPx activity was not different between groups (Fig. 4c, d).
Oxidative stress biomarkers in sperm at postnatal day 110: a malondialdehyde, b reactive oxygen species, c superoxide dismutase, and d glutathione peroxidase. Mean ± SEM, n = 6 rats from different litters; control (C) open bars, restricted (R) closed bars. Analysis was by unpaired Student’s t test. The asterisk on top of the closed bars indicates p < 0.05 vs control
Sperm parameters at PND 110
Sperm quality evaluated by sperm concentration, viability, motility, and morphology at PND 110 revealed a modest but significant decrease in R offspring in both sperm concentration and viability (Fig. 5a, b) while motility was unchanged (Fig. 5c). Analysis of sperm morphology showed the presence of abnormalities particularly in the flagellum and midpiece that were more abundant in R offspring (Fig. 5d, e).
Sperm quality and morphology at postnatal day 110: a sperm concentration, b viability, c motility, d sperm abnormalities, and e representative photographs showing the presence of alterations in the flagellum (denoted by an asterisk). Mean ± SEM, n = 6 rats from different litters; control (C) open bars, restricted (R) closed bars. Analysis was by unpaired Student’s t test. The asterisk on top of the closed bars indicate p < 0.05 vs control
Fertility rate
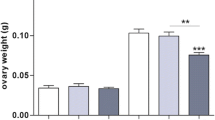
Fertility rate reported as the percentages of fertile males (Fig. 6a) and pregnant females (Fig. 6b) was the same in both groups at PND 110 but decreased in terms of fertile males in the R group at PND 450 (Fig. 6a, b) and PND 850 when expressed as pregnant females (Fig. 6b). The fertility decline in the R group was dependent of both maternal diet and age (Fig. 6).
Fertility rate in male offspring at postnatal day 110, 450, and 850 expressed as a fertile males (two females for each male; male was considered fertile when one of the two females got pregnant) and b pregnant females (n = 12 females). Mean ± SEM, n = 6 male rats from different litters; control (C) open bars, restricted (R) closed bars. p < 0.05 for data not sharing at least one letter on the same maternal diet. Analysis was by χ 2. The asterisk on top of the closed bars indicate p < 0.05 vs control. d postnatal days
Discussion
In recent years, a large number of epidemiological (Barker et al. 2002; Galjaard et al. 2013; Gluckman et al. 2007) and animal (Heindel 2008; McMullen and Mostyn 2009; Nathanielsz 2006) studies have shown that environmental challenges experienced by the developing mammalian organism in utero and in early neonatal life can induce a persistent response in a variety of organs, predisposing to enhanced susceptibility to later life onset of diseases such as type 2 diabetes (Portha et al. 2011), hypertension (Ingelfinger and Nuyt 2012), obesity (Sarr et al. 2012), and alterations in reproductive function (Zambrano et al. 2014a). In the model studied here, we have previously reported that at PND 270, male offspring of mothers fed a low-protein diet during pregnancy had a lower sperm count and a 50 % decrease in fertility rate compared to controls (Zambrano et al. 2005b). In addition, reduced maternal protein intake during pregnancy decreases male offspring Sertoli cell numbers. This reduction is important since Sertoli cells play an important role in generating the required environment for the proliferation and maturation or germ cells (Rodríguez-González et al. 2012). Seminiferous tubular development is also delayed accompanied by an increase in testicular apoptosis (Zambrano et al. 2014a).
We report several male offspring reproductive outcomes resulting from low maternal protein intake nutrition that have not been demonstrated previously. Since our goal was to study as much of the life span as possible, we were able to show that body weight and epididymal fat were increased in offspring of protein-restricted mothers at PND 850. Our data at PND 850 is later in the life course than previous studies for both control and restricted rats. The oldest age we have found based on the data in the literature for male sexual development and fertility in control rats is around PND 720 (Hokao et al. 1993) and PND 270 for male offspring of protein-restricted mothers (Zambrano et al. 2005b). Since our goal was to study as much of the life span as possible, we were able to show that body weight and epididymal fat were increased in the offspring of protein-restricted mothers at the oldest age studied—PND 850 an older age than previously studied. The observed decrease in fetal LH is likely to have major consequences on gonadal development is the likely cause of the observed decrease in testosterone during adulthood in the restricted group. Deficient maternal nutrition in sheep does not affect serum FSH and LH concentrations, semen quality, and fertility rate in male offspring at 20 months of age, a stage proportional to the life span approximately equal to PND 110 in a rat’s life indicating the need for studies across species and care when comparing different programming models (Rae et al. 2002a). Maternal protein restriction in the rat decreases LH and testosterone serum levels and sperm concentration without changes in FSH concentrations and fertility rate in male offspring of 70 days (Zambrano et al. 2005b). The present study shows lower serum testosterone levels at all ages studied in male R group offspring. There is evidence that obesity can affect fertility through different mechanisms, including dysfunction of the hypothalamo-pituitary-gonadal axis (Cabler et al. 2010) in addition to increased release and activity of adipose-derived hormones from fat accumulated around the testes (Martini et al. 2012; Palmer et al. 2012). In this context, we have reported that male offspring of pregnant rats fed the low-protein diet became obese and have increased serum triglycerides, insulin, and leptin levels (Zambrano et al. 2006; Zambrano et al. 2005a). In the present study, we found that at PND 110, R male offspring had a significant decrease in sperm concentration and viability with a significant increase in the incidence of sperm morphological abnormalities. These defects may be due to deficiencies in specific nutrients resulting from the decreased maternal dietary protein intake or, as discussed, caused by increased OS.
Spermatogenesis requires a high rate of cell division implying significant oxygen consumption resulting in lowered oxygen tension in testicular tissue which may constitute an important regulatory factor within the testes (Aitken and Roman 2008; Free et al. 1976). As stated above, both spermatogenesis and Leydig cell steroidogenesis are vulnerable to OS. Therefore, low testicular oxygen tension may be important as one of the mechanisms protecting the testes from free radical generation. In addition, the presence of an array of testicular antioxidant enzymes and free radical scavengers help protect this organ from the impact of OS (Aitken and Roman 2008). In this regard, several perinatal conditions such as maternal malnutrition, maternal obesity, or excessive exposure to glucocorticoids (a common fetal response to developmental programming challenges) (Zambrano et al. 2014b) increase OS (Bernal et al. 2010; Mutsaers and Tofighi 2012; Zambrano and Nathanielsz 2013). Tarry-Adkins et al. have reported that maternal undernutrition using a low-protein diet (8 %), similar to the one we used, is associated with increased OS and an impaired antioxidant defense capacity in the pancreas of male rat offspring at 3 and 15 months of age (Tarry-Adkins et al. 2010). The maternal low-protein diet was associated with markers of greater offspring ROS in testis and sperm and decreased fertility. Thus, our results suggest a link between the intrauterine insult and offspring OS that results in developmental programming of male sexual fertility demonstrated by premature aging of fertility. These observations suggest that an imbalance in testicular OS and subsequent reproductive capacity are associated. The observed malformations in the sperm at PND 110 may result from cytotoxic effects of OS generated by maternal protein restriction, particularly since at this age, a significant increase in ROS and MDA levels was found in both testes and sperm.
Endogenous antioxidant mechanisms in the testes protect against oxidative damage to gonadal cells and mature spermatozoa. Vazquez-Memije et al., have reported that ROS generation and the capacity of the antioxidant system are significantly increased and decreased, respectively, in adulthood and older ages in animals on a control diet (Vazquez-Memije et al. 2008). In contrast with the rat, we observed a fall in both SOD and GPx in early life in the C group. This was followed by a rise in GPx with age in C offspring. We suggest that the observed increase in the antioxidant system with age in the R group above C males may in part be due to compensation for increased OS in this group when compared to the C group.
Hormones play an important role in the establishment and maintenance of reproductive function (Meeker et al. 2007). Reproductive aging is associated with a decrease in circulating levels of testosterone in both male rodents and men (Hardy and Schlegel 2004). Our hypothesis that maternal protein restriction (MPR) leads to accelerated aging is supported by Bonavera et al., who reported that in male rats, testosterone levels decrease with age with a concomitant reduction in LH pulsatile secretion which could be secondary to hypothalamic-pituitary dysfunction (Bonavera et al. 1997; Gruenewald et al. 1994). In the present study, we report that FSH, LH, and testosterone levels all decreased with aging. Our hypothesis that the premature aging is induced by the increased OS levels is supported by data in MA-10 cells (Leydig tumor cells) in which steroidogenesis is inhibited by high ROS concentrations (Diemer et al. 2003). In addition, studies in testes of elderly rats have shown an increase in ROS levels, a reduction in StAR and a decrease in testosterone (Allen et al. 2004). There is evidence which indicates that male obesity negatively impacts reproductive capacity not only by reducing sperm quality but also by affecting germ cells and spermatozoa (Palmer et al. 2012) through different mechanisms such as decreased sex hormone secretion (Aggerholm et al. 2008; Cabler et al. 2010), increased insulin resistance (Hammoud et al. 2008), and/or due to the direct action of leptin or other hormones derived from adipocytes on testicular function (Landry et al. 2013). The findings of the present study of metabolic alterations coupled to the increase in testicular OS level indicate that OS may play an important role in the etiology of the fertility problems observed in adult life of the rat offspring from nutrient-restricted mothers.
Finally, according to the free radical theory of aging, aging is the result of cumulative damage caused by ROS which leads to the progressive decline in physiological functions (Ivanova and Yankova 2013). Our study provides the first evidence that the rate of aging of male reproduction is developmentally programmed as shown by three clear observations in offspring of mothers who eat a low-protein diet: testosterone is lower during adulthood; testicular OS related variables rise earlier and higher, and fertility rate decreases earlier. All these end points are markers of aging of male reproduction. These alterations are likely programmed in early stages of development. Finally, although in the present study, overall fertility rate was the same in C and R at PND 110, we have previously reported that at PND 270, reproductive capacity was already lower in R in comparison to C males, thus indicating premature aging of reproductive capacity in early adult life (Zambrano et al. 2005b). Developmental programming is considered a key factor in predisposing to chronic disease. Our data are consistent with the novel concept that programming also plays an important role in aging trajectory. This interaction is a little studied area in aging biology that merits more investigation. The metaphor in everyday life is that unless an automobile is constructed well, it will not run for as fast, as far or, in the context of aging, as long.
Abbreviations
- C:
-
Control
- dG:
-
Days of gestation DCF 2’,7’-dichlorofluorescein
- FSH:
-
Follicle-stimulating hormone
- GPx:
-
Glutathione peroxidase
- LH:
-
Luteinizing hormone
- MDA:
-
Malonaldialdehyde
- OS:
-
Oxidative stress
- PND:
-
Postnatal days
- RIA:
-
Radioimmunoassay
- ROS:
-
Reactive oxygen species
- R:
-
Restricted
- SOD:
-
Superoxide dismutase
- TBARS:
-
Thiobarbituric acid-reactive substances assay
References
Agarwal A, Saleh RA, Bedaiwy MA (2003) Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril 79:829–843
Aggerholm AS, Thulstrup AM, Toft G, Ramlau-Hansen CH, Bonde JP (2008) Is overweight a risk factor for reduced semen quality and altered serum sex hormone profile? Fertil Steril 90:619–626. doi:10.1016/j.fertnstert.2007.07.1292
Aitken RJ, Roman SD (2008) Antioxidant systems and oxidative stress in the testes. Oxid Med Cell Longev 1:15–24
Allen JA, Diemer T, Janus P, Hales KH, Hales DB (2004) Bacterial endotoxin lipopolysaccharide and reactive oxygen species inhibit Leydig cell steroidogenesis via perturbation of mitochondria. Endocrine 25:265–275
Barker DJ, Eriksson JG, Forsen T, Osmond C (2002) Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol 31:1235–1239
Bernal AB, Vickers MH, Hampton MB, Poynton RA, Sloboda DM (2010) Maternal undernutrition significantly impacts ovarian follicle number and increases ovarian oxidative stress in adult rat offspring. PLoS One 5:e15558. doi:10.1371/journal.pone.0015558
Bjorndahl L, Soderlund I, Kvist U (2003) Evaluation of the one-step eosin-nigrosin staining technique for human sperm vitality assessment. Hum Reprod 18:813–816
Bonavera JJ et al (1997) In the male brown-Norway (BN) male rat, reproductive aging is associated with decreased LH-pulse amplitude and area. J Androl 18:359–365
Cabler S, Agarwal A, Flint M, du Plessis SS (2010) Obesity: modern man’s fertility nemesis. Asian J Androl 12:480–489. doi:10.1038/aja.2010.38
Davies MJ, Norman RJ (2002) Programming and reproductive functioning. Trends Endocrinol Metab 13:386–392
Diemer T, Allen JA, Hales KH, Hales DB (2003) Reactive oxygen disrupts mitochondria in MA-10 tumor Leydig cells and inhibits steroidogenic acute regulatory (StAR) protein and steroidogenesis. Endocrinology 144:2882–2891. doi:10.1210/en.2002-0090
Franco MC, Akamine EH, Reboucas N, Carvalho MH, Tostes RC, Nigro D, Fortes ZB (2007) Long-term effects of intrauterine malnutrition on vascular function in female offspring: implications of oxidative stress. Life Sci 80:709–715. doi:10.1016/j.lfs.2006.10.028
Free MJ, Schluntz GA, Jaffe RA (1976) Respiratory gas tensions in tissues and fluids of the male rat reproductive tract. Biol Reprod 14:481–488
Galjaard S, Devlieger R, Van Assche FA (2013) Fetal growth and developmental programming. J Perinat Med 41:101–105. doi:10.1515/jpm-2012-0020
Gluckman PD, Hanson MA, Pinal C (2005) The developmental origins of adult disease. Matern Child Nutr 1:130–141. doi:10.1111/j.1740-8709.2005.00020.x
Gluckman PD, Hanson MA, Beedle AS (2007) Early life events and their consequences for later disease: a life history and evolutionary perspective. Am J Hum Biol 19:1–19. doi:10.1002/ajhb.20590
Gruenewald DA, Naai MA, Hess DL, Matsumoto AM (1994) The brown Norway rat as a model of male reproductive aging: evidence for both primary and secondary testicular failure. J Gerontol 49:B42–50
Guzman C, Cabrera R, Cardenas M, Larrea F, Nathanielsz PW, Zambrano E (2006) Protein restriction during fetal and neonatal development in the rat alters reproductive function and accelerates reproductive ageing in female progeny. J Physiol 572:97–108
Hammoud AO, Wilde N, Gibson M, Parks A, Carrell DT, Meikle AW (2008) Male obesity and alteration in sperm parameters. Fertil Steril 90:2222–2225. doi:10.1016/j.fertnstert.2007.10.011
Hardy MP, Schlegel PN (2004) Testosterone production in the aging male: where does the slowdown occur? Endocrinology 145:4439–4440. doi:10.1210/en.2004-0888
Heindel JJ (2008) Animal models for probing the developmental basis of disease and dysfunction paradigm. Basic Clin Pharmacol Toxicol 102:76–81. doi:10.1111/j.1742-7843.2007.00184.x
Hokao R, Saito TR, Wakafuji Y, Takahashi KW, Imamichi T (1993) The change with age of the copulatory behavior of the male rats aged 67 and 104 weeks. Jikken Dobutsu 42:75–82
Ingelfinger JR, Nuyt AM (2012) Impact of fetal programming, birth weight, and infant feeding on later hypertension. J Clin Hypertens (Greenwich) 14:365–371. doi:10.1111/j.1751-7176.2012.00660.x
Ivanova DG, Yankova TM (2013) The free radical theory of aging in search of a strategy for increasing life span. Folia Med 55:33–41
Landry D, Cloutier F, Martin LJ (2013) Implications of leptin in neuroendocrine regulation of male reproduction. Reprod Biol 13:1–14. doi:10.1016/j.repbio.2012.12.001
Luo ZC et al (2006) Tracing the origins of “fetal origins” of adult diseases: programming by oxidative stress? Med Hypotheses 66:38–44. doi:10.1016/j.mehy.2005.08.020
Luo ZC, Xiao L, Nuyt AM (2010) Mechanisms of developmental programming of the metabolic syndrome and related disorders. World J Diabetes 1:89–98. doi:10.4239/wjd.v1.i3.89
Martini AC, Molina RI, Ruiz RD, de Fiol Cuneo M (2012) Obesity and male fertility. Rev Fac Cien Med Univ Nac Cordoba 69:102–110
McMullen S, Mostyn A (2009) Animal models for the study of the developmental origins of health and disease. Proc Nutr Soc 68:306–320. doi:10.1017/S0029665109001396
Meeker JD, Godfrey-Bailey L, Hauser R (2007) Relationships between serum hormone levels and semen quality among men from an infertility clinic. J Androl 28:397–406
Mutsaers HA, Tofighi R (2012) Dexamethasone enhances oxidative stress-induced cell death in murine neural stem cells. Neurotox Res 22:127–137. doi:10.1007/s12640-012-9308-9
Nathanielsz PW (2006) Animal models that elucidate basic principles of the developmental origins of adult diseases. ILAR J 47:73–82
World Health Organization (2010) WHO laboratory manual for the examination and processing of human semen. Fifth Edition edn. WHO Press, Switzerland
Ozanne SE, Hales CN (2004) Lifespan: catch-up growth and obesity in male mice. Nature 427:411–412. doi:10.1038/427411b
Palmer NO, Bakos HW, Fullston T, Lane M (2012) Impact of obesity on male fertility, sperm function and molecular composition. Spermatogenesis 2:253–263. doi:10.4161/spmg.21362
Portha B, Chavey A, Movassat J (2011) Early-life origins of type 2 diabetes: fetal programming of the beta-cell mass. Exp Diabetes Res 2011:105076. doi:10.1155/2011/105076
Rae MT, Kyle CE, Miller DW, Hammond AJ, Brooks AN, Rhind SM (2002a) The effects of undernutrition, in utero, on reproductive function in adult male and female sheep. Anim Reprod Sci 72:63–71
Rae MT, Rhind SM, Kyle CE, Miller DW, Brooks AN (2002b) Maternal undernutrition alters triiodothyronine concentrations and pituitary response to GnRH in fetal sheep. J Endocrinol 173:449–455
Rodríguez-González GL, Vigueras-Villaseñor RM, Millán S, Moran N, Trejo R, Nathanielsz PW, Larrea F, Zambrano E (2012) Maternal protein restriction in pregnancy and/or lactation affects seminiferous tubule organization in male rat offspring. J Dev Orig Health Dis 3:321–326. doi:10.1017/S2040174412000360
Sarr O, Yang K, Regnault TR (2012) In utero programming of later adiposity: the role of fetal growth restriction. J Pregnancy 2012:134758. doi:10.1155/2012/134758
Sikka SC (1996) Oxidative stress and role of antioxidants in normal and abnormal sperm function. Front Biosci : J Virtual Libr 1:e78–86
Tarry-Adkins JL, Ozanne SE (2011) Mechanisms of early life programming: current knowledge and future directions. Am J Clin Nutr 94:1765S–1771S. doi:10.3945/ajcn.110.000620
Tarry-Adkins JL, Chen JH, Jones RH, Smith NH, Ozanne SE (2010) Poor maternal nutrition leads to alterations in oxidative stress, antioxidant defense capacity, and markers of fibrosis in rat islets: potential underlying mechanisms for development of the diabetic phenotype in later life. FASEB J 24:2762–2771. doi:10.1096/fj.10-156075
Toledo FC, Perobelli JE, Pedrosa FP, Anselmo-Franci JA, Kempinas WD (2011) In utero protein restriction causes growth delay and alters sperm parameters in adult male rats. Reprod Biol Endocrinol 9:94
Vazquez-Memije ME, Capin R, Tolosa A, El-Hafidi M (2008) Analysis of age-associated changes in mitochondrial free radical generation by rat testis. Mol Cell Biochem 307:23–30. doi:10.1007/s11010-007-9580-9
Vega CC, Reyes-Castro LA, Bautista CJ, Larrea F, Nathanielsz PW, Zambrano E (2013) Exercise in obese female rats has beneficial effects on maternal and male and female offspring metabolism Int J Obes (Lond) doi:10.1038/ijo.2013.150
Zambrano E, Nathanielsz PW (2013) Mechanisms by which maternal obesity programs offspring for obesity: evidence from animal studies. Nutr Rev 71(Suppl 1):S42–54. doi:10.1111/nure.12068
Zambrano E et al (2005a) Sex differences in transgenerational alterations of growth and metabolism in progeny (F2) of female offspring (F1) of rats fed a low protein diet during pregnancy and lactation. J Physiol 566:225–236
Zambrano E et al (2005b) A maternal low protein diet during pregnancy and lactation in the rat impairs male reproductive development. J Physiol 563:275–284
Zambrano E et al (2006) A low maternal protein diet during pregnancy and lactation has sex- and window of exposure-specific effects on offspring growth and food intake, glucose metabolism and serum leptin in the rat. J Physiol 571:221–230
Zambrano E, Guzmán C, Rodríguez-González G, Durand-Carbajal M, Nathanielsz PW (2014a) Fetal programming of sexual development and reproductive function. Mol Cell Endocrinol 382:538–549
Zambrano E TN, Long N. M., Guo C, Sun K, Cox L. A., Ford S. P., Nathanielsz P. W. and Li C (2014b) Increased Central and Peripheral Glucocorticoid Synthesis Act As an Orchestrator of Developmental Programming. In: Zhang L PD, and Longo L.D, M.D. (ed) Stress and Developmental Programming of Health and Disease: Beyond Phenomenology. Nova Science Publishers, Inc, pp 463–486
Acknowledgments
Rodríguez-González GL and Reyes-Castro LA are graduate students from Doctorado en Ciencias Biomédicas, Facultad de Medicina, Universidad Nacional Autónoma de México, and Carlos Ibáñez is a graduate student from Doctorado en Ciencias Bioquímicas, Facultad de Química, Universidad Nacional Autónoma de México—recipients of Consejo Nacional de Ciencia y Tecnología (CONACyT) fellowship. This work was supported by CONACyT México 155166.
Conflict of interest
The authors have nothing to disclose and have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Rodríguez-González, G.L., Reyes-Castro, L.A., Vega, C.C. et al. Accelerated aging of reproductive capacity in male rat offspring of protein-restricted mothers is associated with increased testicular and sperm oxidative stress. AGE 36, 9721 (2014). https://doi.org/10.1007/s11357-014-9721-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-014-9721-5