Abstract
Arsenic exposure has been associated with the risk of diabetes or insulin resistance (IR), which are also related with overweight/obesity. This study aimed to explore the interaction between arsenic exposure and being overweight/obesity on diabetes or IR risk. Data from the National Health and Nutrition Examination Survey (NHANES) in cycles 2007–2016 were used to assess the interaction between arsenic exposure and being overweight/obesity on IR or diabetes risk among adults. Urinary total arsenic concentrations (UTAs) were used as a biomarker for arsenic exposure. The homeostasis model of insulin resistance (HOMA-IR) was calculated to index IR. Survey-weighted logistic regression and restricted cubic spline (RCS) analyses were performed to determine the association and dose–response relationship between UTAs and IR or diabetes risk. Additive interaction was evaluated by relative excess risk due to interaction (RERI), attributable proportion of interaction (AP), and synergy index (S). A total of 3,133 participants were included. The median (interquartile range) UTAs were 6.61 (3.83, 13.95) μg/L. The adjusted OR of IR was 1.40 (95% CI: 0.99–1.97) for UTAs, comparing the highest with the lowest quartile. And significant additive interaction was observed between high UTAs and being overweight/obesity on IR risk (RERI = 2.47, 95% CI: 0.30–4.63; AP = 0.29, 95% CI: 0.07–0.50; S = 1.48, 95% CI: 1.03–2.13). Our results suggested that there might be a potential additive interaction between high UTAs with being overweight/obesity on diabetes risk (AP = 0.27, 95%CI: 0.04–0.51). Our results indicated an additive interaction between arsenic exposure and being overweight/obesity on IR risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes, an endocrine disease characterized by chronic hyperglycemia, is the ninth leading cause of death in the world (Zheng et al. 2018). Insulin resistance (IR) is an important risk factor of diabetes and is also associated with cardiovascular diseases and cancer (Lebovitz 2001; Pichard et al. 2008). The pathogenesis of diabetes or IR involved multiple factors, including environmental factors (Tremblay and Hamet 2019), lifestyle factors (Carbone et al. 2019), genetic factors (Tremblay and Hamet 2019), and their interactions (Zhi et al. 2016). For decades, the role of arsenic exposure in the development of diabetes or IR has attracted extensive attention.
Arsenic, a naturally occurring metalloid, has been recognized as an environmental pollutant. It is estimated that approximately 200 million people worldwide may be exposed to potentially toxic levels of arsenic (Chen and Costa 2021). Experimental studies indicated that arsenic could induce diabetes in at least two ways. First, chronic arsenic exposure might decrease insulin-stimulated glucose uptake in muscles and fat tissues, resulting in IR, which then lead to the development of diabetes. Second, beta cell dysfunction could be induced by chronic arsenic exposure, and then eventually manifests as diabetes (Tseng 2004). However, population-based studies assessing the effect of arsenic exposure on diabetes or IR risk have yielded inconsistent results (Mondal et al. 2020; Peng et al. 2015; Wang et al. 2014; Yang et al. 2019; Zhou et al. 2022). For instance, Mondal et al found that arsenic exposure was positively associated with the homeostasis model of insulin resistance (HOMA-IR) index among participants from arsenic-endemic and non-endemic areas in Bangladesh (Mondal et al. 2020). And Zhou et al observed that higher urinary total arsenic was related with increased risk of IR among adults from the National Health and Nutrition Examination Survey (NHANES) (Zhou et al. 2022). However, Peng et al failed to detect a significant association between urinary total arsenic concentration and the HOMA-IR index among adolescents from NHANES (Peng et al. 2015). The inconsistencies could be attributed to various factors, such as arsenic dose, exposure time, and individual factors.
Several epidemiologic studies have indicated that the risks of arsenic-induced diseased are markedly increased among individuals with obesity, suggesting obesity as a potential susceptibility factor (Eick and Steinmaus 2020). Several cross-sectional studies investigated the modifying effect of body mass index (BMI) on the association of arsenic exposure with diabetes, and observed a greater risk of diabetes with arsenic exposure among populations with higher BMI (Castriota et al. 2018; Pan et al. 2013). A joint effect of BMI with urinary total arsenic concentration on HOMA-IR was reported among children and adolescents (urinary total arsenic concentration: 25.54±1.22 μg/L and 25.92±1.23 μg/L) (Lin et al. 2014). However, most previous studies were conducted in arsenic-endemic regions. Data from NHANES 2015-2016 showed that BMI did not influence the association between urinary total arsenic concentrations [6.82 (3.74-15.40) µg/L] and IR, but the sample size was relatively small (815 adults) (Zhou et al. 2022). Whether higher BMI interacts with arsenic exposure at levels common in the general population to alter the risk of IR or diabetes is still unclear.
Therefore, we used data from NHANES to evaluate the association of arsenic exposure with diabetes or IR risk among adults. And further, we explored whether there were interaction effects between being overweight/obesity and arsenic exposure on the risk of diabetes or IR.
Material and methods
Study population
NHANES is a program of studies that combines interviews and physical examinations. It is designed to assess the health and nutritional status of children and adults in the US. For the sample design, NHANES used complex, multistage, probability methods to select participants representing the civilian, non-institutionalized US population. NHANES protocols were approved by the National Center for Health Statistics (NCHS) Institutional Review Board of the US Centers for Disease Control and Prevention (CDC), and consents were obtained from all participants. More specific and detailed survey design, methods, and data can be obtained from the NHANES official website (https://www.cdc.gov/nchs/nhanes/).
For this study, we used data from NHANES cycles 2007/2008 to 2015/2016. A total of 50,588 participants were enrolled in 5 consecutive survey cycles (2007/2008, 2009/2010, 2011/2012, 2013/2014, 2015/2016), and 29,201 participants were adults aged 20 years and older. Then, 26,068 participants were excluded because of missing information on diabetes and IR assessments (fasting plasma glucose, HbA1c, oral glucose tolerance test, physician-diagnosed diabetes, fasting insulin), urinary total arsenic concentrations, BMI, or other covariates including age, gender, race/ethnicity, education level, the poverty income ratio (PIR), smoking status, alcohol drinking, physical activity, fish consumption, and urinary creatinine concentrations. Finally, 3,133 study participants were included in the present study (Fig. 1). There was no significant difference in urinary total arsenic concentrations between individuals included in our study and those excluded with age ≥ 20 years. However, significant difference in urinary creatine concentrations, gender, and race/ethnicity were found between individuals included and those excluded with age ≥ 20 years (Supplementary Table S1).
Measurement of urinary total arsenic concentrations
Urine samples were collected with the subjects’ consent. Then the samples were processed, stored, and shipped to the Division of Laboratory Sciences, National Center for Environmental Health, CDC, Atlanta, GA for analysis and quality control. Urinary total arsenic concentrations were measured by the inductively coupled-plasma dynamic reaction cell-mass spectrometry (ICP-DRC-MS) method. The limit of detection (LOD) of urinary total arsenic concentrations was 0.74μg/L in the cycle from 2007 through 2010, 1.25μg/L in the cycle 2011/2012, and 0.26μg/L in the cycle from 2013 through 2016 (https://www.cdc.gov/nchs/nhanes/). For samples below the LOD, the value was set to the LOD divided by the square root of 2. There were 23 study subjects whose urinary total arsenic concentrations were below LOD in our study.
Diabetes and IR
To test fasting plasma glucose and fasting insulin, blood samples were collected following at least 9-h fasting. Diabetes was defined according to the American Diabetes Association (ADA) criteria (ADA Professional Practice Committee 2022) and self-report questionnaires. Participants were identified as diabetes cases if they fulfilled at least one of the following criteria: (1) Fasting plasma glucose ≥ 7 mmol/L, (2) HbA1c ≥ 6.5%, (3) 2-h plasma glucose during oral glucose tolerance test ≥ 11.1 mmol/L (ADA Professional Practice Committee 2022), (4) diagnosed with diabetes by a doctor in the self-report questionnaire.
IR was assessed using HOMA-IR index: fasting serum insulin (μU/mL) × fasting plasma glucose (mmol/L) / 22.5. Based on the World Health Organization (WHO), insulin sensitivity was defined as values less than the highest quartile of the HOMA-IR index which was determined in individuals without diabetes (Alberti and Zimmet 1998). However, previous studies had different cut-off values as for the definition of IR (Tang et al. 2015), and one of the most commonly used values was still the 75th percentile of HOMA-IR index for non-diabetic individuals (Kabadi et al. 2012; Tucker 2022; Xu et al. 2022; Zuk et al. 2018). Therefore, in this study, IR was defined as being above the highest quartile of the HOMA-IR index (3.57) among participants without diabetes.
Covariates
The covariates in our study involved sociodemographic characteristics, lifestyle factors, laboratory data, and other information.
Sociodemographic characteristics included age, gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), education level (less than high school, high school or equivalent, college or above), and PIR (< 1, 1–3, > 3). The PIR was calculated as a ratio of family income to poverty threshold determined annually by the United States Department of Health and Human Service (National Center for Health Statistics 2017). Lifestyle factors contained smoking status, alcohol drinking, physical activity, and fish consumption. Smoking status was divided into current smoking, former smoking, and never smoking according to responses to questions " Smoked at least 100 cigarettes in life?" and " Do you now smoke cigarettes?". For alcohol drinking, drinking and non-drinking status were determined based on the answer to question "Had at least 12 alcohol drinks/1yr?" Physical activity was divided into no/low intensity and moderate/high intensity according to answers of the questions " In a typical week do you do any vigorous-intensity sports, fitness, or recreational activities that cause large increases in breathing or heart rate like running or basketball for at least 10 min continuously?" and "In a typical week do you do any moderate-intensity sports, fitness, or recreational activities that cause a small increase in breathing or heart rate such as brisk walking, bicycling, swimming, or volleyball for at least 10 min continuously?" Participants were defined as fish consumer if they answered “yes” to the question “During the past 30 days did you eat any types of fish listed on this card including any foods that had fish in them such as sandwiches, soups, or salads?” Urinary creatinine concentrations were obtained from laboratory data. Individuals’ height and weight were measured at the Mobile Examination Center (MEC) exam. BMI was calculated by dividing the weight (kg) by the square of height (m2). BMI ≥ 30 kg/m2, 25 ≤ BMI ≤ 29.99 kg/m2, and 18.5 ≤ BMI ≤ 24.99 kg/m2 were classified as obesity, overweight and normal BMI, respectively.
Statistical analysis
All data download and data analyses were carried out using SAS 9.4 (SAS Institute, Cary NC) and STATA SE16 (Stata Corp, College Station, TX, USA). Two-sided P < 0.05 was considered statistically significant. Considering the complexity of the sampling design, the data in this study were processed according to the weighting method recommended by the NHANES website, and the SAS survey procedures were used for data analysis. Continuous variables were presented as weighted mean ± standard error or median (interquartile range), and we conducted the analysis of variance (ANOVA) to identify the difference in means across groups (urinary total arsenic and urinary creatinine concentrations were skewed and natural log-transformed for analysis). Categorical variables were shown as the number of cases and the weighted proportion [n (%)], and the comparisons between groups were performed by the Rao-Scottχ2test. Survey-weighted logistic regression was performed to evaluate the association of urinary total arsenic concentrations with the risk of IR or diabetes. To further explore the possible dose–response or nonlinear relationship between urinary total arsenic concentrations and the risk of IR or diabetes, we used a restricted cubic spline model with four knots located at the 20th, 50th, 75th, and 90th percentiles of urinary total arsenic concentrations (the reference: median) (Desquilbet and Mariotti 2010). Confounding was assessed based on prior literature (James et al. 2013; Li et al. 2021; Lin et al. 2014; Peng et al. 2015; Zhou et al. 2022) through the use of Directed Acyclic Graphs (www.dagitty.net/dags.html). The following covariates were included in adjusted model as confounding variables: age, gender, race/ethnicity, education level, PIR, smoking status, alcohol drinking, physical activity, fish consumption, and BMI (supplementary Figure S1). As suggested by O’Brien et al., urinary total arsenic was standardized by the covariate-adjusted standardization plus creatinine adjustment method (O'Brien et al. 2016), so we fitted a model for creatinine (natural log-transformed) as a function of age, gender, BMI, and race/ethnicity, and urinary creatinine concentration was included in the adjusted model. Interactions of urinary total arsenic concentrations with being overweight/obesity on IR or diabetes risk were investigated on both additive and multiplicative scales. For the calculation of multiplicative interaction, a cross-product interaction term was included into the logistic regression model. To assess the additive interaction, we calculated relative excess risk due to interaction (RERI), attributable proportion of interaction (AP), and synergy index (S) (Andersson et al. 2005). These measurements were calculated as follows: RERI = OR11-OR10-OR01 + 1; AP = RERI/OR11; S = (OR11-1) / ((OR10-1) + (OR01-1)), where the subscripts indicate presence (1) or absence (0) of the two risk factors. If there is no additive interaction, RERI and AP are equal to 0 and S is equal to 1. We also conducted power calculations for the additive interaction analyses by Power V3.0 software (National Cancer Institute, Bethesda, MD, USA; available online: https://dceg.cancer.gov/tools/design/power).
Results
Characteristics of study participants
Table 1 showed the characteristics of participants in the current study. A total of 3,133 subjects aged 20 and older were included, containing 1584 males and 1549 females, with an average age of 47.77 years old. The median (interquartile range) of urinary total arsenic concentrations were 6.61 (3.83, 13.95) μg/L. Participants were mostly non-Hispanic White (weighted proportion, 70.40%), had a college education or above (62.57%), and had a PIR > 3 (49.73%). More than half of the participants reported never smoking (54.84%) and had moderated/high intensive physical activity (54.72%). Only 21.92% of the participants were non-drinkers. According to the diagnostic criteria, participants were divided into three groups: diabetes group, IR group, and control group (participants without IR or diabetes). Significant differences in urinary total arsenic concentrations (control group: 6.34 μg/L, IR group: 6.99 μg/L, diabetes group: 7.58 μg/L; P = 0.045) and BMI (control group: 26.76 ± 0.13 kg/m2, IR group: 33.60 ± 0.39 kg/m2, diabetes group: 32.06 ± 0.39 kg/m2; P < 0.001) were detected among the three groups. And there were notable differences in age, gender, race/ethnicity, education level, PIR, smoking status, alcohol drinking, physical activity, and urinary creatinine concentrations among the three groups (P < 0.05).
Independent association of urinary total arsenic concentrations and being overweight/obesity with IR or diabetes risk
As presented in Table 2, urinary total arsenic concentrations were categorized into quartiles or tertiles for analysis. When compared with individuals in the lowest quartile, a borderline significant association was found between the highest quartile and increased risk of IR (adjusted OR = 1.40, 95% CI: 0.99–1.97; P = 0.055). And the adjusted ORs of IR were 1.40 (95% CI: 0.96–2.03) and 1.36 (95% CI: 0.90–2.04) for the second and third quartiles of urinary total arsenic concentrations. When classified based on tertiles, no significant relationship was detected between urinary total arsenic and the risk of IR. No significant association was observed between urinary total arsenic and the risk of diabetes.
As shown in Table 2, compared with individuals with normal BMI, individuals with being overweight and those with obesity had higher risks of IR (overweight: adjusted OR = 3.34, 95% CI:2.19–5.08; obesity: adjusted OR = 15.79, 95% CI:10.74–23.22) or diabetes (overweight: adjusted OR = 2.49, 95% CI: 1.69–3.67; obesity: adjusted OR = 10.04, 95% CI: 6.74–14.97).
The dose–response relationship between urinary total arsenic concentrations with IR or diabetes risk
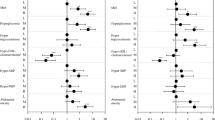
Restricted cubic spline analyses were conducted to explore the possible dose–response or nonlinear relationship of urinary total arsenic concentrations with the risk of IR or diabetes (Fig. 2). In the total population, no significant dose–response relationship was observed between urinary total arsenic concentrations and the risk of IR (P overall = 0.655, P nonlinearity = 0.539) or diabetes (P overall = 0.335, P nonlinearity = 0.231) after adjustments. When stratified by BMI, a nonlinear relationship of urinary total arsenic concentrations with diabetes risk might exist among individuals with normal BMI (P overall = 0.049, P nonlinearity = 0.023).
Dose–response curves for the associations between urinary total arsenic concentrations with adjusted odds ratios of IR or diabetes. Dose-response curves for the association between urinary total arsenic concentrations with IR risk in the total population (A), in normal BMI subgroup (B), and overweight/obesity subgroup (C); Dose-response curves for the association between urinary total arsenic concentrations with diabetes risk in the total population (D), in normal BMI subgroup (E), and overweight/obesity subgroup (F). The solid line and dashed line represent the adjusted estimated odds ratios and 95% confidence intervals. Urinary total arsenic concentrations were standardized using the covariate-adjusted standardization plus covariate adjustment method. Analyses were adjusted for age, gender, race/ethnicity, education level, PIR, smoking status, alcohol drinking, physical activity, fish consumption, urinary creatine concentrations, and BMI.
Interaction effects between urinary total arsenic concentrations and being overweight/obesity on IR or diabetes risk
As shown in Table 3, participants with urinary total arsenic above median (> 6.61 μg/L) were classified as high exposure group, and others were defined as low exposure group. Individuals with a combination of high arsenic group and being overweight/obesity had a significantly higher risk of IR compared with individuals with low arsenic group and normal BMI (adjusted OR = 8.58, 95% CI: 5.13–14.35). The independent ORs for high arsenic alone and being overweight/obesity alone were 0.98 (95% CI: 0.42–2.26) and 6.14 (95% CI:3.69–10.23), respectively. The corresponding RERI, AP, and S were 2.47 (95% CI: 0.30–4.63), 0.29 (95% CI: 0.07–0.50), and 1.48 (95% CI:1.03–2.13), respectively. It suggested that there was a significant additive interaction between urinary total arsenic concentrations and being overweight/obesity on IR risk, and about 29% of the OR of being IR was attributed to the interaction effect.
As for the additive interaction of urinary total arsenic with being overweight/obesity on diabetes risk, only the estimated AP was statistically significant (AP = 0.27, 95% CI: 0.04–0.51), while RERI and S were not (RERI = 1.29, 95% CI: -0.14 to 2.72; S = 1.53, 95% CI: 0.98–2.39; Table 3), suggesting that there might be a potential additive interaction between urinary total arsenic and being overweight/obesity on diabetes risk.
There was no significant multiplicative interaction between urinary total arsenic and being overweight/obesity on the risk of IR (P = 0.386) or diabetes (P = 0.125, Table 3).
Discussion
In the present study, urinary total arsenic concentrations were positively associated with IR risk in the general adult population of the US. Furthermore, we observed an additive interaction between being overweight/obesity and high urinary total arsenic on IR risk. When stratified by BMI, there was a nonlinear relationship between urinary total arsenic and diabetes risk in the normal BMI subgroup. Our results also suggested that there might be a potential additive interaction between urinary total arsenic and being overweight/obesity on diabetes risk.
IR, a condition where body’s cells cannot adequately respond to insulin, is associated with increased risks of type 2 diabetes (T2D), cardiovascular diseases, and cancers (Lebovitz 2001; Pichard et al. 2008). Previous studies regarding the effect of arsenic exposure on IR risk yielded inconsistent results. A study conducted in Bangladesh reported that water arsenic (129.5 ± 155.8 μg/L), hair arsenic (3.60 ± 5.78 μg/g), and nail arsenic (6.92 ± 7.72 μg/g) concentrations were positively correlated with HOMA-IR, and part of the mechanism of arsenic exposure leading to IR was the loss of skeletal muscle mass (Mondal et al. 2020). However, urinary total arsenic concentrations (41.2 μg/L) were negatively correlated with HOMA-IR in two arsenic-endemic areas of Mexico (β = -4.538, 95% CI: -7.514 ~ -1.562) (Del et al. 2011). That study population consisted of 9.7% diabetic patients, whose HOMA-IR might be affected by lifestyle modification or using antidiabetic agents. No significant association was found between HOMA-IR and urinary total arsenic among adolescent population from NHANES (Peng et al. 2015), while higher urinary total arsenic was associated with increased risk of IR among adults from NHANES (Zhou et al. 2022). And the median urinary total arsenic concentration [adolescent: 7.01 (4.13, 12.80) μg/L; adults: 6.82 (3.74,15.40) μg/L] were both close to the value in our study [6.63 (3.83, 14.03) μg/L]. There are several factors that could account for the inconsistency. Firstly, it is possible that the adult population were exposed to arsenic for a longer duration compared to adolescents. Secondly, the discrepancy might be attributed to differences in the employed data analysis methods. Zhou et al. used multifactorial logistic regression and reported that individuals in the highest quintile of urinary total arsenic exhibited an elevated risk of IR than those in the lowest quintile (adjusted OR = 1.41, 95% CI: 1.07–1.87) (Zhou et al. 2022). Likewise, our study employed survey-weighted logistic regression and found that higher urinary total arsenic was associated with increased risk of IR. While Peng et al. utilized the generalized additive mixed model and no significant association was observed between HOMA-IR (log-transformed) and urinary total arsenic (Peng et al. 2015). Therefore, we also analyzed the association between HOMA-IR (log-transformed) and urinary total arsenic using the generalized additive mixed model, and failed to detect a significant relationship (Q4 vs Q1, β = 0.176, P = 0.931). However, Peng et al. did not examine potential effect modification by BMI. Zhou et al. did subgroup analyses by BMI and multiplicative interaction between BMI and urinary total arsenic on the risk of IR (P = 0.051). Nevertheless, they did not further explore additive interaction, which reflect biological interaction better (Andersson et al. 2005).
Therefore, to better understand the interaction between urinary total arsenic and overweight/obesity on IR risk, we performed formal analyses regarding the additive interaction. Our results indicated that there was significant additive interaction between high urinary total arsenic with being overweight/obesity on the risk of IR. A cross-sectional study reported a joint effect of BMI and urinary total arsenic concentrations on IR risk among adolescents and children in an area of Taiwan with low arsenic exposure, and the regression coefficients of HOMA-IR value were 2.146 (95% CI:1.192–3.100) for subjects with combined overweight/obesity and high urinary total arsenic (> 19.54 μg/L), 0.366 (-0.631–1.326) for subjects with normal weight and high urinary total arsenic, and 1.605 (0.674–2.536) for subjects with abnormal weight and low urinary total arsenic when using subjects with normal weight and low urinary total arsenic concentrations (≤ 19.54 μg/L) as reference (Lin et al. 2014). The mean urinary total arsenic concentration of children (25.54 ± 1.22 μg/L) and adolescents (25.92 ± 1.23 μg/L) were higher than that in our study. The mechanism underlying the interaction between urinary total arsenic and being overweight/obesity on IR remains unclear. Previous studies have shown that NOD-like receptor protein 3 (NLRP3) inflammasome-dependent post-translational processing of IL-1β and IL-18 is involved in obesity-induced inflammation and IR (Vandanmagsar et al. 2011). Recently, researchers found that the activation of NLRP3 inflammasome and subsequent IL-1β, IL-18 maturation and secretion participated in arsenic-induced hepatic IR (Jia et al. 2020; Qiu et al. 2022). Thus, it is plausible to speculate that arsenic-induced NLRP3 inflammasome activation may be aggravated by overweight/obesity. Future studies are warranted to clarify our findings and explore the underlying mechanisms.
Inconsistent with previous studies (Grau-Perez et al. 2018; Sung et al. 2015; Wang et al. 2014), we failed to detect a significant association between urinary total arsenic concentrations and diabetes risk in the total population. A meta-analysis conducted in 2013 reported that iAs exposure was significantly positively associated with T2D with a dose–response relationship (Wang et al. 2014). Most previous studies were conducted in arsenic-endemic regions, while our study population was derived from a large, nationally representative sample of general population, and the urinary total arsenic concentrations in the current study were 6.63 (3.83, 14.03) μg/L. Results from the Coronary Artery Risk Development in Young Adults (CARDIA) study indicated that there was no association between diabetes risk and low to moderate toenail arsenic levels (Yang et al. 2019). Some other factors may also contribute to this discrepancy, such as arsenic exposure pathways and arsenic exposure evaluation methods. For instance, a meta-analysis showed that arsenic exposure through ingestion was a risk factor for diabetes (RR = 1.57, 95% CI:1.27–1.93), while arsenic exposure through inhalation was not associated with diabetes (RR = 1.08, 95% CI:0.79–1.46) (Sung et al. 2015). In addition, the urinary total arsenic concentrations used in our study might not be a true reflection of inorganic arsenic exposure, which could lead to potential misclassification of exposure and inconsistency between our results and previous studies using inorganic arsenic exposure. Although no significant dose–response relationship was observed in the total population, our results suggested that a nonlinear relationship of urinary total arsenic concentrations with diabetes risk might exist among individuals with normal BMI. Therefore, BMI should be considered as a modifier of the association between arsenic exposure and diabetes risk.
Accordingly, we further explored the interaction of urinary total arsenic concentrations with being overweight/obesity on the risk of diabetes. And our results suggested that there might be a potential additive interaction between high urinary total arsenic and being overweight/obesity on diabetes risk. In agreement with our findings, Castriota et al. and Pan et al. reported significant additive interaction between arsenic exposure and high BMI on T2D risk (Castriota et al. 2018; Pan et al. 2013). However, only one interaction evaluation index, the synergy index, was reported in Castriota’s study, and the synergy index was 3.12 (95% CI: 0.91–10.70) with 95% CI containing 1 (Castriota et al. 2018), which should not be considered statistically significant (Andersson et al. 2005). Besides, Pan et al. reported that 62% of the OR of diabetes was attributed to the interaction between BMI and arsenic in drinking water [diabetes:71.5 (269.9) μg/L, controls: 13.9 (134.2) μg/L], but the RERI was 8.93 (95% CI:0.14–32.2), with a large range of CI which might be due to the small sample size of diabetes (n = 84) and then lead to instability of the estimates (Pan et al. 2013).. Thus, future studies with larger sample size are needed to confirm or refute our findings, especially among populations with arsenic exposure at levels common in the general population.
To our knowledge, this is the first study to report a significant additive interaction between urinary total arsenic concentrations and being overweight/obesity on IR risk. This study population was derived from a large, nationally representative sample. It is also noteworthy that the urinary total arsenic concentrations in our study represent exposure levels common in the general population of US. Nevertheless, there are some limitations to our study. First, due to the cross-sectional nature of NHANES, no conclusions can be drawn regarding the temporal association and causal determination of arsenic exposure and the risk of IR or diabetes. Second, urinary total arsenic concentrations might be affected by food containing organic arsenic. Although dietary fish intake was adjusted in this study, the influence of other organic arsenic exposure sources cannot be completely excluded. Third, potential selection bias might exist because there were significant differences in urinary creatine concentration, gender, and race/ethnicity between individuals included in our study and those excluded with age ≥ 20 years. Although sample weights were applied in data analyses, populations beyond those included in this study might affect the assessment of association between urinary total arsenic and the risk of diabetes or IR. Fourth, the sample sizes of some subgroups were small, so we performed power calculations and the results suggested that the power of additive interaction analysis of urinary total arsenic with being overweight/obesity on IR and diabetes risk were 84.3% and75.2%, respectively, the interactive effect between urinary total arsenic and being overweight/obesity on diabetes risk is likely to be underpowered. Thus, future studies with a large sample size may be required to validate or refute our results.
In summary, our results demonstrated that there was a significant additive interaction between high urinary total arsenic concentrations and being overweight/obesity on IR risk. Considering that obesity and arsenic exposure are prevalent and widespread, especially that the arsenic exposure in our study was at levels common in the general population of US, these findings have important public health implications. Prevention strategies for IR aimed at both weight management and reducing arsenic exposure may surpass the expected benefits based on addressing these risk factors alone. Future prospective studies and mechanism research are needed to further confirm and elucidate our results.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553. https://doi.org/10.1002/(SICI)1096-9136(199807)15:7%3c539::AID-DIA668%3e3.0.CO;2-S
American Diabetes Association Professional Practice Committee (2022) 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care 45:S17–S38. https://doi.org/10.2337/dc22-S002
Andersson T, Alfredsson L, Kallberg H, Zdravkovic S, Ahlbom A (2005) Calculating measures of biological interaction. Eur J Epidemiol 20:575–579. https://doi.org/10.1007/s10654-005-7835-x
Carbone S, Del BM, Ozemek C, Lavie CJ (2019) Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog Cardiovasc Dis 62:327–333. https://doi.org/10.1016/j.pcad.2019.08.004
Castriota F, Acevedo J, Ferreccio C, Smith AH, Liaw J, Smith MT, Steinmaus C (2018) Obesity and increased susceptibility to arsenic-related type 2 diabetes in Northern Chile. Environ Res 167:248–254. https://doi.org/10.1016/j.envres.2018.07.022
Chen QY, Costa M (2021) Arsenic: A Global Environmental Challenge. Annu Rev Pharmacol Toxicol 61:47–63. https://doi.org/10.1146/annurev-pharmtox-030220-013418
Del RL, Garcia-Vargas GG, Valenzuela OL, Castellanos EH, Sanchez-Pena LC, Currier JM, Drobna Z, Loomis D, Styblo M (2011) Exposure to arsenic in drinking water is associated with increased prevalence of diabetes: a cross-sectional study in the Zimapan and Lagunera regions in Mexico. Environ Health 10:73. https://doi.org/10.1186/1476-069X-10-73
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057. https://doi.org/10.1002/sim.3841
Eick SM, Steinmaus C (2020) Arsenic and Obesity: a Review of Causation and Interaction. Curr Environ Health Rep 7:343–351. https://doi.org/10.1007/s40572-020-00288-z
Grau-Perez M, Navas-Acien A, Galan-Chilet I, Briongos-Figuero LS, Morchon-Simon D, Bermudez JD, Crainiceanu CM, de Marco G, Rentero-Garrido P, Garcia-Barrera T, Gomez-Ariza JL, Casasnovas JA, Martin-Escudero JC, Redon J, Chaves FJ, Tellez-Plaza M (2018) Arsenic exposure, diabetes-related genes and diabetes prevalence in a general population from Spain. Environ Pollut 235:948–955. https://doi.org/10.1016/j.envpol.2018.01.008
James K, Marshall J, Hokanson J, Meliker J, Zerbe G (2013) A case-cohort study examining lifetime exposure to inorganic arsenic in drinking water and diabetes mellitus. Environ Res 123:33–38. https://doi.org/10.1016/j.envres.2013.02.005
Jia X, Qiu T, Yao X, Jiang L, Wang N, Wei S, Tao Y, Pei P, Wang Z, Zhang J, Zhu Y, Yang G, Liu X, Liu S, Sun X (2020) Arsenic induces hepatic insulin resistance via mtROS-NLRP3 inflammasome pathway. J Hazard Mater 399:123034. https://doi.org/10.1016/j.jhazmat.2020.123034
Kabadi S, Lee B, Liu L (2012) Joint effects of obesity and vitamin D insufficiency on insulin resistance and type 2 diabetes: results from the NHANES 2001–2006. Diabetes Care 35:2048–2054. https://doi.org/10.2337/dc12-0235
Lebovitz HE (2001) Insulin resistance: definition and consequences. Exp Clin Endocrinol Diabetes 109(Suppl 2):S135–S148. https://doi.org/10.1055/s-2001-18576
Li X, Wang X, Park SK (2021) Associations between rice consumption, arsenic metabolism, and insulin resistance in adults without diabetes. Int J Hyg Environ Health 237:113834. https://doi.org/10.1016/j.ijheh.2021.113834
Lin HC, Huang YK, Shiue HS, Chen LS, Choy CS, Huang SR, Han BC, Hsueh YM (2014) Arsenic methylation capacity and obesity are associated with insulin resistance in obese children and adolescents. Food Chem Toxicol 74:60–67. https://doi.org/10.1016/j.fct.2014.08.018
Mondal V, Hosen Z, Hossen F, Siddique AE, Tony SR, Islam Z, Islam MS, Hossain S, Islam K, Sarker MK, Hasibuzzaman MM, Liu LZ, Jiang BH, Hoque MM, Saud ZA, Xin L, Himeno S, Hossain K (2020) Arsenic exposure-related hyperglycemia is linked to insulin resistance with concomitant reduction of skeletal muscle mass. Environ Int 143:105890. https://doi.org/10.1016/j.envint.2020.105890
National Center for Health Statistics, 2017. NHANES 2015–2016: Demo-graphic Variables and Sample Weights Data Documentation, Codebook, and Frequencies. Cent Dis Control Prev. https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/DEMO_I.htm (accessed 25 May, 2023)
O’Brien KM, Upson K, Cook NR, Weinberg CR (2016) Environmental Chemicals in Urine and Blood: Improving Methods for Creatinine and Lipid Adjustment. Environ Health Perspect 124:220–227. https://doi.org/10.1289/ehp.1509693
Pan WC, Seow WJ, Kile ML, Hoffman EB, Quamruzzaman Q, Rahman M, Mahiuddin G, Mostofa G, Lu Q, Christiani DC (2013) Association of low to moderate levels of arsenic exposure with risk of type 2 diabetes in Bangladesh. Am J Epidemiol 178:1563–1570. https://doi.org/10.1093/aje/kwt195
Peng Q, Harlow SD, Park SK (2015) Urinary arsenic and insulin resistance in US adolescents. Int J Hyg Environ Health 218:407–413. https://doi.org/10.1016/j.ijheh.2015.03.006
Pichard C, Plu-Bureau G, Neves-E CM, Gompel A (2008) Insulin resistance, obesity and breast cancer risk. Maturitas 60:19–30. https://doi.org/10.1016/j.maturitas.2008.03.002
Qiu T, Wu C, Yao X, Han Q, Wang N, Yuan W, Zhang J, Shi Y, Jiang L, Liu X, Yang G, Sun X (2022) AS3MT facilitates NLRP3 inflammasome activation by m(6)A modification during arsenic-induced hepatic insulin resistance. Cell Biol Toxicol 1–17. https://doi.org/10.1007/s10565-022-09703-7
Sung TC, Huang JW, Guo HR (2015) Association between Arsenic Exposure and Diabetes: A Meta-Analysis. Biomed Res Int 2015:368087. https://doi.org/10.1155/2015/368087
Tang Q, Li X, Song P, Xu L (2015) Optimal cut-off values for the homeostasis model assessment of insulin resistance (HOMA-IR) and pre-diabetes screening: Developments in research and prospects for the future. Drug Discoveries & Therapeutics 9:380–385. https://doi.org/10.5582/ddt.2015.01207
Tremblay J, Hamet P (2019) Environmental and genetic contributions to diabetes. Metabolism 100S:153952. https://doi.org/10.1016/j.metabol.2019.153952
Tseng CH (2004) The potential biological mechanisms of arsenic-induced diabetes mellitus. Toxicol Appl Pharmacol 197:67–83. https://doi.org/10.1016/j.taap.2004.02.009
Tucker L (2022) Serum, Dietary, and Supplemental Vitamin D Levels and Insulin Resistance in 6294 Randomly Selected, Non-Diabetic U.S. Adults. Nutrients 14:1844. https://doi.org/10.3390/nu14091844
Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, Ravussin E, Stephens JM, Dixit VD (2011) The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med 17:179–188. https://doi.org/10.1038/nm.2279
Wang W, Xie Z, Lin Y, Zhang D (2014) Association of inorganic arsenic exposure with type 2 diabetes mellitus: a meta-analysis. J Epidemiol Community Health 68:176–184. https://doi.org/10.1136/jech-2013-203114
Xu Z, Gong R, Luo G, Wang M, Li S, Chen Y, Shen X, Wei X, Feng N, Wang S (2022) Association between vitamin D3 levels and insulin resistance: a large sample cross-sectional study. Sci Rep 12:119. https://doi.org/10.1038/s41598-021-04109-7
Yang K, Xun P, Carnethon M, Carson AP, Lu L, Zhu J, He K (2019) Low to moderate toenail arsenic levels in young adulthood and incidence of diabetes later in life: findings from the CARDIA Trace Element study. Environ Res 171:321–327. https://doi.org/10.1016/j.envres.2019.01.035
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14:88–98. https://doi.org/10.1038/nrendo.2017.151
Zhi X, Yang B, Fan S, Li Y, He M, Wang D, Wang Y, Wei J, Zheng Q, Sun G (2016) Additive Interaction of MTHFR C677T and MTRR A66G Polymorphisms with Being Overweight/Obesity on the Risk of Type 2 Diabetes. Int J Environ Res Public Health 13:1243. https://doi.org/10.3390/ijerph13121243
Zhou M, Zhao E, Huang R (2022) Association of urinary arsenic with insulin resistance: Cross-sectional analysis of the National Health and Nutrition Examination Survey, 2015–2016. Ecotoxicol Environ Saf 231:113218. https://doi.org/10.1016/j.ecoenv.2022.113218
Zuk A, Quiñonez C, Saarela O, Demmer R, Rosella L (2018) Joint effects of serum vitamin D insufficiency and periodontitis on insulin resistance, pre-diabetes, and type 2 diabetes: results from the National Health and Nutrition Examination Survey (NHANES) 2009–2010. BMJ Open Diabetes Res Care 6:e000535. https://doi.org/10.1136/bmjdrc-2018-000535
Acknowledgements
This study was funded by the National Natural Science Foundation of China (No. 81903304), the Natural Science Foundation for Colleges and Universities of Jiangsu Province (NO. 19KJB330006), and the China Postdoctoral Science Foundation (NO. 2020T130089ZX). A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD). We gratefully acknowledge the study participants and all staff members who were involved in this study of NHANES.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81903304), the Natural Science Foundation for Colleges and Universities of Jiangsu Province (NO. 19KJB330006), and the China Postdoctoral Science Foundation (NO. 2020T130089ZX). A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Xueyuan Zhi, the guarantor of this work, took full responsibility for the integrity of the data and the accuracy of data analysis. Yiming Ma and Xueyuan Zhi conceived the study design, analyzed the data, and edited the manuscript. Ying Wu, Ye Li, Xiaoming Zhang, Yiting Gong contributed to data collection, data analysis and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
NHANES protocols were approved by the National Center for Health Statistics (NCHS) Institutional Review Board of the US Centers for Disease Control and Prevention (CDC).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, Y., Wu, Y., Li, Y. et al. Additive interaction of urinary total arsenic concentrations with being overweight/obesity on the risk of insulin resistance: NHANES 2007–2016. Environ Sci Pollut Res 30, 92306–92316 (2023). https://doi.org/10.1007/s11356-023-28924-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-28924-9