Abstract
Vietnam is one Southeast Asian country most vulnerable to climate change. By the end of the twenty-first century, temperature could rise above 5°C across Vietnam according to the IPCC highest emission pathway scenario. However, research on the temperature-health effects from the geographically diverse sub-tropical northern region of Vietnam is limited making location specific health system preparedness difficult. This study examines the elevated temperature-hospitalization relationship for the seven provinces in northern Vietnam by using generalized linear and distributed lag models. A random-effect meta-analysis was used to estimate the pooled temperature hospitalizations risks for all causes, and for infectious, cardiovascular, and respiratory diseases. The pooled estimates show a significant effect of high temperature on hospitalizations for the same day (lag 0), when a 1°C increase in temperature above 24°C was significantly associated with 1.1% (95% CI, 0.9–1.4%) increased risk for all-cause hospital admissions, 2.4% (95% CI, 1.9–2.9%) increased risk for infectious disease admissions, 0.5% (95% CI, 0.1–0.9%) increased risk for cardiovascular disease admissions, and 1.3% (95% CI, 0.9–1.6%) increased risk for respiratory disease admissions. This research adds to the scant evidence examining heat and health morbidity effects in sub-tropical climates and has important implications for better understanding and preparing for the future impacts of climate change related temperature on Vietnam residents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Like many parts of the world, an increase in temperature has been observed across Southeast Asia over past decades (Hijioka et al. 2014). Vietnam, located in Southeast Asia, is one of the ten countries most affected by global warming in the past 20 years (Eckstein et al. 2020). The rate of warming in Vietnam is estimated at 0.26°C per decade for 1971–2010, which is almost twice the rate of global warming for the same period (Nguyen et al. 2014). Global warming scenarios also indicate Vietnam is among five countries in the world most likely to be affected in the future (WBG and ADB 2021). Temperature is projected to increase across Vietnam including northern regions, with annual changes ranging from 2.4 to 5.1°C for high emission scenarios by the end of the twenty-first century (Katzfey et al. 2014). Growing evidence indicates that temperature increases are likely to intensify the existing impacts of temperature on human health via increased mortality, morbidity, and health care utilization (Watts et al. 2015). Ample research indicate that high temperature is associated with increased risk of deaths and illnesses (Green et al. 2019; Chen et al. 2018; Song et al. 2017; Bunker et al. 2016), including chronic cardiovascular (Bai et al. 2018) and respiratory conditions (Wu et al. 2021; Turner et al. 2012) and infectious diseases associated with food, water, and vector transmission (Phung et al. 2015a, 2015b, 2015c; Hashizume et al. 2008). However, research on temperature morbidity effects is still under-represented globally particularly from low-income and tropical and sub-tropical climates (Campbell et al. 2018; Green et al. 2019). Increased health impacts associated with high temperatures have been reported in several studies from southern Vietnam (Phung et al. 2015a, 2015b, 2015c, 2015d; Phung et al. 2016a, 2016b) with less attention on the sub-tropical northern area (Giang et al. 2014; Xuan et al. 2014a, 2014b). A more nuanced understanding of spatiotemporal differences in heat-health impacts is essential, requiring the conduct of location-specific studies to inform local climate and health adaptation policies tailored to local vulnerable populations (Green et al. 2019).
The few studies targeting Vietnam have reported an increased risk of water- and vector-borne diseases (Phung et al. 2015a, 2015b, 2015c), cardiovascular (Phung et al. 2016c; Giang et al. 2014) and respiratory diseases (Phung et al. 2016a, 2016b; Phung et al. 2018), and risk of hospital admissions among young children from exposure to high temperatures (Luong et al. 2019; Phung et al. 2015d), but most of this research is focused on tropical, southern Vietnam. Although WHO’s health vulnerable assessment to climate change has indicated northern Vietnam as one of the most highly vulnerable areas (WHO 2011), very few studies have reported temperature-morbidity and mortality relationships from the region. Studies from Hanoi (Xuan et al. 2014a) and Thai Nguyen provinces (Giang et al. 2014) indicate significant increase in mortality and hospital admissions due to cardiovascular diseases only with cold temperatures, especially in the elderly. However these studies were limited to single disease outcomes, single city, and the older population group.
This study examines the effect of temperature on risk of all-cause hospitalizations, and hospitalizations due to cardiovascular, respiratory, and infectious illnesses in multiple cities in northern Vietnam.
Methods
Study setting
Vietnam’s land area spans a large latitude range (between the latitudes 8° and 24°N). Southern parts of Vietnam experience a tropical climate, and northern parts in the humid subtropics observe greater seasonal variation (Institute of strategy and policy on natural resources and environment (ISPONRE) 2009). The seven provinces included in this study represent 3 sub-regions: northwest, northeast, and Red River Delta. The northwest is a mountainous region with a population of 3.5 million people. Its climate is characterized by cold, dry, and sunny winters. Summers in the region are hot due to a high frequency of hot and dry days and westerly winds (Institute of strategy and policy on natural resources and environment (ISPONRE)2009). Northeast Vietnam has a population of 13 million accounting for 15% of Vietnam’s population. The climate of this region is strongly influenced by the north-eastern monsoon (Mui 2006). The summers are hot, humid, and coincide with the rainy season, but in contrast to the northwest, dry conditions are rare due to a low frequency of westerly winds. Red River Delta has a population of 17 million, of which a half live in the capital city, Hanoi. Summers are also hot and rainy. The mean temperature in northern regions ranges from 22–27.5°C in summer to 15–20°C in winter.
Data sources
We obtained inpatient hospitalization records from the provincial hospital in each of the seven provinces. Daily hospital admission data were extracted from these records of Bac Giang (BG), Tuyen Quang (TQ), Phu Tho (PT), Dien Bien (DB), Lai Chau (LC), Ha Noi (HN), and Quang Ninh (QN) provincial hospitals (Supplemental Figure 1), representing the major tertiary/large hospital in each region, for the period between January 2005 and December 2015. For each hospitalization, we extracted primary diagnosis, date of admission, and patient’s province of residence. Patients who were not residents of the selected provinces and hospital records (<1%) with missing data were excluded from the analysis. All provincial hospitals used the same hospital record management software, so the data source quality was similar across the provinces. From the hospitalization database, we derived daily counts for all causes (excluding external causes), cardiovascular diseases (I00-99; excluding: acute rheumatic fever, I00-02, and chronic rheumatic heart diseases, I05-09), and respiratory diseases (J00-99; excluding: lung diseases due to external agents, J60-70), and certain infectious and parasitic diseases (ICD10-Code: A00-B99; excluding: infections with predominantly sexual mode of transmission, A50-64, HIV, B20-24, helminthiases, B65-83, sequelae of infectious and parasitic diseases, B90-94). Disease classification was based on discharge diagnosis. The time-span of daily hospitalization data varied from 2 to 11 years as the electronic data management system became operational in the respective provincial hospital.
Daily meteorological data (ambient temperature, humidity, and precipitation) were obtained from the provincial hydro-meteorological stations or from the closest airport weather stations. The precipitation data for province Phu Tho was not available; therefore, humidity only was adjusted for in the respective model. The project was approved by the ethical committee of Griffith University (GU Ref No: ENV/23/15/HREC) and Health and Environment Management Agency, the leading agency of the health sector responsible for climate change and health in Vietnam (1290/MT-SKCD).
Data analysis
Data analyses involved three steps. First, we performed descriptive statistics for exposure (temperature) and outcome (hospitalization) variables (i.e., hospitalization for all causes, infectious diseases, respiratory, and cardiovascular diseases). Second, we examined the temperature-hospitalization relationship for each province using mean temperature centered at 24°C which represents the mean temperature for the majority of the studied provinces (Table 1). For data analysis, we centered the values of the daily average temperature to examine the effect of temperatures with one unit increase from the centered value (rather than value of 0). Third, we performed a random-effect meta-analysis to estimate the pooled effect sizes of temperature on all-cause, infectious, cardiovascular, and respiratory admissions. Poisson generalized linear model (GLM) and distributed lag model (DLM) were used to examine the province-specific association between temperature and daily average temperature and risk of hospitalization. We used a generalized linear model (GLM) with the family of Poisson because the outcome variable is a count (the number of hospital admissions each day), and the distribution of the outcome values was over-dispersed. We incorporated distributed lags into the model (distributed lag model: DLM) to examine the delayed effects of the temperatures on the outcome based on previous research that showed the high temperatures have a short-term effect within a week (Ye et al. 2012). The Poisson regression time-series model to examine the effect of daily average temperature on all-cause, infectious, respiratory, and cardiovascular admissions for each province was:
where Yt is the observed daily count of hospital admissions on day t; α is the intercept; Tt is the daily average temperature on day t and l is the lag days; H is the daily average humidity; R is the daily cumulative rainfall. s is the flexible spline function with 7 knots per year; DOW is the day of the week. The Poisson regression model was applied separately for each province to examine the effect of temperature on each outcome of hospitalizations (i.e., all-cause, infectious, respiratory, and cardiovascular).
The linear distributed lag model of temperature for lags up to 6 days (a week) was used to examine the delayed effect of temperature on hospitalizations. A flexible spline function with 7 knots per year was used to control for long-term trends and seasonal patterns in hospitalizations (Bhaskaran et al. 2013). The model was adjusted for humidity, rainfall, and day of the week to control for potential confounding effects.
A random-effect meta-analysis was applied to calculate within-province and between-province variation and generate pooled effect size (relative risk, RR). The pooled effect sizes, which were calculated for cause-specific hospitalizations, comprising all-cause, infectious diseases (ID), cardiovascular disease (CVD), and respiratory diseases (RD), were computed by lag day (from 0 to 6 days). I-squared (coefficient of inconsistency) statistics was used to determine the heterogeneity between studies (Higgins et al. 2003).
All the data analyses were conducted using the “glm” and “db metan” packages of Stata 14.0 (Stata Corporation, College Station, TX, USA).
Results
Descriptive statistics
Table 1 summarizes the descriptive statistics for temperature and hospitalizations for the seven provinces in northern Vietnam during the study period. A total of 15,400 total admissions were recorded, and average daily hospital admissions for all causes ranged from 29 to 235 across the provinces, depending on the size of the data-providing hospitals. Daily average respiratory and cardiovascular hospital admissions were higher than infectious admissions in almost all the provinces. The average temperature ranged from 21.8 to 24.9°C.
Temperature-hospitalization risks
Across almost all the provinces, a rise in temperature above 24°C was associated with an increased risk of hospitalization for all-causes (except PT province), infectious (except LC province), and respiratory diseases (except BG province), but the effect sizes were variable across the provinces (Table 2). Similar positive effects of temperature on all-cause, infectious and respiratory hospitalizations were observed on the same day (lag 0) across the provinces (Supplementary Tables 1–4). The percentage changes in risk of hospitalization with a 1°C increase in mean temperature above 24°C are shown in Table 2, and lag effects are shown in Supplementary Tables 1–4.
A 1°C rise in temperature above the mean reference temperature was significantly associated with an increase in all-cause hospital admissions in all but PT province with the lowest positive change observed in TQ (0.8%, 95% CI 0.2–1.4%) and the highest positive change observed in LC (1.8%, 95% CI 1.1–2.5%). When examined for temperature lag effects on all-cause hospitalizations, an identical effect was observed for same day (lag 0) rise in temperature across the provinces (Supplementary Table 1). Regarding temperature and infectious disease hospitalizations the significant positive changes were observed in BG, DB, QN, and TQ provinces, with the lowest positive effect in DB (1.6%, 95% CI 0.2–3.1%) and the highest positive effect in BG (3.5%, 95% CI 2.2–4.9%). The positive effect was also consistent for same day (lag 0) rise in temperature across BG, DB, QN, and TQ provinces (Supplementary Table 2) with the lowest positive effect was observed in DB (1.8%, 95% CI 0.1–3.6%). A significant positive effect on respiratory disease hospitalizations from increase in temperature was observed in all but BG province, with the lowest positive change in QN (1.0%, 95% CI 0.2–1.8%) and highest in LC (2.1%, 95% CI 1.1–3.1%) (Table 2), which was also consistent for same day rise in temperature in all but LC and QN provinces (Supplementary Table 3). None of the other temperature lag days (lag 1–lag 6) showed any significant positive effect on all-cause, respiratory or infectious disease hospitalizations (Supplementary Tables 1–3). In LC, the highest positive effect of temperature was observed for all-cause and respiratory hospitalizations with no statistically significant effect on infectious hospitalizations. Similarly the highest positive change in temperature-infectious disease hospitalizations was observed in BG though no such significant change in respiratory admissions was identified (Table 2). The temperature and cardiovascular hospital admissions relationships were not statistically significant for any province (Table 2), nor for any lag day except in BG where same day rise in temperature showed a positive effect on cardiovascular admissions (Supplementary Table 4).
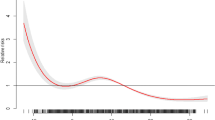
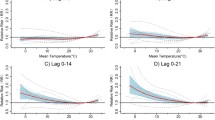
The pooled estimates of the effect of high temperatures on hospitalizations across lag days for all provinces are presented in Fig. 1. The pooled estimates show a significant effect of high temperature on hospitalizations for the same day (lag 0), when a 1°C increase in temperature above 24°C is significantly associated with 1.1% (95% CI, 0.7–1.4%) increased risk for all-cause admissions, 2.3% (95% CI, 1.6–3.0%) increased risk for infectious admissions, 0.9% (95% CI, 0.3–1.5%) increased risk for cardiovascular admissions and 1.3% (95% CI, 0.8–1.8%) increased risk for respiratory admissions. None of the other lag days was significantly associated with any hospital admission category. I-squared statistics for heterogeneity for all-cause hospitalizations were 0.0% across all lag days, for infectious admissions were 0.0% in all but lag 0 (14.8%), for respiratory admissions were 0.0% in all but lag 5 (19.0%) and 6 days (47.8%), and for cardiovascular admissions were 0.0% in all but lag 5 (25.4%).
Sensitivity analyses that changed measure of temperature (maximum, minimum) and excluding temperature below 24°C did not substantially influence the estimates of mean temperature effects on hospitalizations (data not shown).
Discussion
Our research presents the short-term effects of temperatures on risk of hospitalizations across multiple provinces in northern Vietnam adding to the understudied body of evidence in LMICs and sub-tropical environments; (Campbell et al. 2018; Green et al. 2019). Overall, pooled estimates for all the study provinces in northern Vietnam indicate a significant effect of same day rise in temperature above 24°C on hospital admissions for all cause, infectious, respiratory, and cardiovascular admissions. A previous study in a single city in northern Vietnam reported an increased risk of cardiovascular hospitalizations from cold temperatures among the older population (Giang et al. 2014). Similarly cold temperature was associated with mortality in an elderly population in Hanoi, Vietnam (Xuan et al. 2014a). However our multi-province study in the same northern region of Vietnam did not find any adverse health effect of cold temperatures, which could indicate that populations are more adapted to low temperatures rather than higher temperatures in this setting. A temporal study in Queensland, Australia representing both sub-tropical and tropical climates showed a decrease in cardiovascular disease admissions from cold temperature and an increased risk from the heat effect (Lu et al. 2020). Although these two study areas differ in sociodemographic characteristics and economic development status, it could be that heat exposure is more detrimental to health in sub-tropical settings. Therefore, further exploration of temperature-morbidity effects in the local context of similar global settings would be useful for designing geographically targeted adaptation strategies. Recent research argues the co-benefits in investing in mitigating emissions and increasing expenditure to incentivize adoption of sustainable production methods, therefore, reducing health risks, delivering a healthy workforce, and contributing to health and economic benefits (Ahmad et al. 2021).
Similar to mortality, the temperature–morbidity relationship is generally nonlinear and shows U-, V-, or J-shaped patterns, where a certain temperature or temperature range (threshold temperature) is associated with minimum morbidity and temperature below and above the threshold increased morbidity (Zhai et al. 2021; Lu et al. 2020; Phung et al. 2016c; Turner et al. 2012). One recent study from a sub-tropical climate has demonstrated an unusual L-pattern, with the steeper mortality effect of lower temperature and flat effect of higher temperature (Dang et al. 2016). Elsewhere a few studies also showed clear threshold temperatures based on model fit (Turner et al. 2012). However, the temperature threshold appears to vary by study location. For example, in the tropical Mekong Delta Region of Vietnam, Phung et al. (2016b) has reported that a 1°C increase in average minimum temperature above 21°C was significantly associated with 1.3% increase in risk of all-causes hospital admissions, 2.2% increase of risk for infectious disease admission, and 1.1% increase of risk for respiratory disease admissions (Phung et al. 2016b). In contrast, a study in a single city of Thailand representing a tropical climate did not show any significant increase in all-cause admissions (overall 5.3%, 95% CI − 0.2%, 11.1%) per 1°C increase in temperature above 29 °C (Pudpong and Hajat 2011). Moreover, this study showed a significant increase in admissions (5.8% increase, 95% CI: 2.3–9.3%) due to intestinal infectious disease with each 1 °C increase in temperature. In sub-tropical Hong Kong, Chan et al. (2013) reported that hospitalizations increased by 4.5% for every 1 °C increase in mean daily temperature above 29.0 °C as well as a significant association between increased average temperature and respiratory and infectious hospital admissions. Such differential temperature thresholds for health effects could be due to differences in population characteristics and activity patterns in different settings, socioeconomic status, adaptive capacity, and lower acclimatization to higher temperatures in cooler climates (Green et al. 2010; Hondula and Barnett 2014). Previous research in the MDR by Phung et al. (2016b) did not observe significant modifying effects of socio-demographic factors on temperature–morbidity relationship. However, further research, especially applying a prospective study design, is recommended to better explore the factors related to adaptive capacity in tropical/sub-tropical climates.
Spatiotemporal difference in temperature-health effects have been clearly demonstrated in several studies (Phung et al. 2015a; Hondula and Barnett 2014; Guo et al. 2014) suggesting that location-specific studies are critical to inform local policies, provide an evidence-base for appropriate climate change and health adaptation strategies and identify climate sensitive and vulnerable population sub-groups. Vietnam’s northern region has the highest poverty and the highest proportion of ethnic minorities compared to other locations (Quyen 2019). Studies across different settings have shown that people with low socio-economic status are particularly vulnerable to heat effects (Xu et al. 2020; Green et al. 2019). This has also been the case in northern Vietnam as demonstrated by health vulnerability assessment studies to climate change that have shown high health sensitivity to temperatures in northern Vietnam (Tran et al. 2020; WHO 2011). Future research to undertake assessment of health adaptive capacity for ambient temperature change with current and future projections is important.
The pooled effect of high temperature on cardiovascular admission on the same day in our research corroborates with results reported elsewhere (Zhai et al. 2021; Tian et al. 2019). However, a recent meta-analysis of estimates from systematic reviews indicated a non-significant effect of high temperature on cardiovascular morbidity (Song et al. 2017). In our research, overall temperature effect on cardiovascular admissions was the weakest among other disease categories, and none of the province specific estimates for temperature effect on cardiovascular admissions was found statistically significant. Previous research among elderly people in Thai Nguyen province of Northern Vietnam reported a non-significant association between hot temperature and CVD admission (RR 1.17, 95% confidence interval: 0.90–1.52) (Giang et al. 2014). Non-significant association between temperature and CVD has also been reported from studies in the MDR (Phung et al. 2016b). As explained in previous research, the differential effects of temperature on cardiovascular morbidity and mortality could be due to increased number of temperature-related cardiovascular deaths before seeking care at the hospital (Michelozzi et al. 2009; O'Neill et al. 2003). However, several studies have reported about the significant effects of extreme temperatures (heatwaves) on increased cardiovascular hospitalizations (Lin et al. 2009), especially in the elderly (Bunker et al. 2016). Different age structures across the provinces could also contribute to such differential health effects as areas with high elderly populations are more likely to be sensitive to high temperatures (Tran et al. 2020). Therefore, age-stratified analysis to elicit temperature and health effects is recommended to identify vulnerable populations and their adaptive capacity. Given projections of high burden of CVD deaths in high-, middle-, and low-income countries (Rehman et al. 2021), it is important that climate change and health adaptation strategies also focus on prevention of non-communicable diseases including CVD.
Some limitations are noted for interpreting our research findings. First, severe admission cases are more likely to be included in the analyses as the hospital data were obtained from the largest public referral hospital at the provincial level, thus the study might have missed the minor cases that were admitted to lower level hospitals (i.e., district hospitals). However, our results still reflect effects on severe admissions. Second, due to small number, the individual-specific cause could not be studied for each province. We recommend future studies in a larger population to look at some heat sensitive individual diseases. Third, although we could not examine the modification effects of socioeconomic factors (e.g., age, occupation) due to lack of data, these factors are less likely to play important role in temperature-hospitalization relationship because they do not change within a short period of time (i.e., day).
Conclusions
The results of this multi-province study enhance the evidence that high temperature is associated with increased risk of morbidity, as measured by hospitalizations in sub-tropical northern Vietnam. As temperature is projected to continue to rise in this region due to climate change, our findings have important implications for public health interventions and adaptation strategies. However further research is recommended focusing on health vulnerability assessment using prospective data in order to better account for variability in temperature, exposure to different temperature thresholds and individual factors relating to age, economic status, etc.
Data availability
The data that support the findings of this study are obtained from Health and Environment Management Agency, Vietnam but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
References
Ahmad M, Akram W, Ikram M, Shah AA, Rehman A, Chandio AA, Jabeen G (2021) Estimating dynamic interactive linkages among urban agglomeration, economic performance, carbon emissions, and health expenditures across developmental disparities. Sustain Prod Consum 26:239–255
Bai L, Li Q, Wang J, Lavigne E, Gasparrini A, Copes R, Yagouti A, Burnett RT, Goldberg MS, Cakmak S, Chen H (2018) Increased coronary heart disease and stroke hospitalisations from ambient temperatures in Ontario. Heart 104(8):673–679. https://doi.org/10.1136/heartjnl-2017-311821
Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B (2013) Time series regression studies in environmental epidemiology. Int J Epidemiol 42(4):1187–1195
Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S, Sauerborn R (2016) Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6:258–268
Campbell S, Remenyi TA, White CJ, Johnston FH (2018) Heatwave and health impact research: a global review. Health Place 53:210–218
Chan EY, Goggins WB, Yue JS, Lee P (2013) Hospital admissions as a function of temperature, other weather phenomena and pollution levels in an urban setting in China. Bull World Health Organ 91(8):576–584
Chen R, Yin P, Wang L, Liu C, Niu Y, Wang W, Zhou M (2018) Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ 363:k4306
Dang TN, Seposo XT, Duc NH, Thang TB, An DD, Hang LT, Long TT, Loan BT, Honda Y (2016) Characterizing the relationship between temperature and mortality in tropical and subtropical cities: a distributed lag non-linear model analysis in Hue, Viet Nam, 2009-2013. Glob Health Action 9:28738. https://doi.org/10.3402/gha.v9.28738
Eckstein D, Künzel V, Schäfer L, Winges M (2020) Global Climate Risk Index 2020, who suffers most from extreme weather events? Weather-related loss events in 2018 and 1999 to 2018. Germanwatch, Bonn, p 2020
Giang PN, Dung DV, Giang KB, Vinhc HV, Rocklöv J (2014) The effect of temperature on cardiovascular disease hospital admissions among elderly people in Thai Nguyen Province, Vietnam. Glob Health Action 7(1):23649
Green RS, Basu R, Malig B, Broadwin R, Kim JJ, Ostro B (2010) The effect of temperature on hospital admissions in nine California counties. Int J Public Health 55:113–121
Green H, Bailey J, Schwarz L, Vanos J, Ebi K, Benmarhnia T (2019) Impact of heat on mortality and morbidity in low and middle income countries: a review of the epidemiological evidence and considerations for future research. Environ Res 171:80–91
Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, Williams G (2014) Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology (Cambridge, Mass) 25(6):781
Hashizume M, Armstrong B, Wagatsuma Y, Faruque ASG, Hayashi T, Sack DA (2008) Rotavirus infections and climate variability in Dhaka, Bangladesh: a time-series analysis. Epidemiol Infect 136(9):1281–1289
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Hijioka Y, Lin E, Pereira JJ, Corlett RT, Cui X, Insarov GE, Lasco RD, Lindgren E, Surjan A (2014) Asia. In: Barros VR, Field CB, Dokken DJ, Mastrandrea MD, Mach KJ, Bilir TE, Chatterjee M, Ebi KL, Estrada YO, Genova RC, Girma B, Kissel ES, Levy AN, MacCracken S, Mastrandrea PR, White LL (eds) Climate change 2014: impacts, adaptation, and vulnerability. part b: regional aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press, Cambridge and New York, pp 1327–1370
Hondula DM, Barnett AG (2014) Heat-related morbidity in Brisbane, Australia: spatial variation and area-level predictors. Environ Health Perspect 122:831–836
Institute of strategy and policy on natural resources and environment (ISPONRE) (2009) Viet Nam Assessment Report on Climate Change https://wedocs.unep.org/bitstream/handle/20.500.11822/7940/VTN_ASS_REP_CC.pdf?sequence=3&isAllowed=y
Katzfey JJ, McGregor JL, Suppiah R (2014) High-resolution climate projections for Vietnam: technical report. CSIRO, Australia, p 266
Lin S, Luo M, Walker RJ, Liu X, Hwang SA, Chinery R (2009) Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 20(5):738–746
Lu P, Xia G, Zhao Q, Xu R, Li S, Guo Y (2020) Temporal trends of the association between ambient temperature and hospitalisations for cardiovascular diseases in Queensland, Australia from 1995 to 2016: a time-stratified case-crossover study. PLoS Med 17(7):e1003176
Luong LMT, Phung D, Sly PD, Dang TN, Morawska L, Thai PK (2019) Effects of temperature on hospitalisation among pre-school children in Hanoi, Vietnam. Environ Sci Pollut Res Int 26(3):2603–2612
Michelozzi P, Accetta G, De Sario M, D'Ippoliti D, Marino C, Baccini M, Biggeri A, Anderson HR, Katsouyanni K, Ballester F, Bisanti L, Cadum E, Forsberg B, Forastiere F, Goodman PG, Hojs A, Kirchmayer U, Medina S, Paldy A et al (2009) High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med 179(5):383–389
Mui N T, 2006. Country pasture/forage resource profile https://ees.kuleuven.be/klimos/toolkit/documents/661_Vietnam.pdf
Nguyen DQ, Renwick J, Mcgregor J (2014) Variations of surface temperature and rainfall in Vietnam from 1971 to 2010. Int J Climatol 34:249–264
O’Neill MS, Zanobetti A, Schwartz J (2003) Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol 157(12):1074–1082
Phung DT, Huang C, Rutherford S, Chu C, Wang X, Nguyen M (2015a) Climate change, water quality, and water-related disease in the Mekong Delta Basin: a systematic review. Asia Pac J Public Health 27:176–265
Phung D, Huang C, Rutherford S, Chu C, Wang X, Nguyen M, Nguyen NH, Manh CD, Nguyen TH (2015b) Association between climate factors and diarrhoea in a Mekong Delta area. Int J Biometeorol 59(9):1321–1331
Phung D, Huang C, Rutherford S, Chu C, Wang X, Nguyen M, Nguyen NH, Do CM, Nguyen TH (2015c) Temporal and spatial patterns of diarrhoea in the Mekong Delta area, Vietnam. Epidemiol Infect 143(16):3488–3497
Phung D, Rutherford S, Chu C, Wang X, Nguyen M, Nguyen NH, Manh Do C, Nguyen TH, Huang C (2015d) Temperature as a risk factor for hospitalisations among young children in the Mekong Delta area, Vietnam. Occup Environ Med 72(7):529–535
Phung D, Chu C, Rutherford S, Nguyen HLT, Do CM, Huang C (2016a) Heatwave and risk of hospitalization: a multi-province study in Vietnam. Environ Pollut 220(Pt A):597–607
Phung D, Guo Y, Nguyen HT, Rutherford S, Baum S, Chu C (2016b) High temperature and risk of hospitalizations, and effect modifying potential of socio-economic conditions: a multi-province study in the tropical Mekong Delta Region. Environ Int 92-93:77–86
Phung D, Guo Y, Thai P, Rutherford S, Wang X, Nguyen M, Chu C (2016c) The effects of high temperature on cardiovascular admissions in the most populous tropical city in Vietnam. Environ Pollut 208:33–39
Phung D, Chu C, Tran DN, Huang C (2018) Spatial variation of heat-related morbidity: a hierarchical Bayesian analysis in multiple districts of the Mekong Delta Region. Sci Total Environ 1(637-638):1559–1565
Pudpong N, Hajat S (2011) High temperature effects on out-patient visits and hospital admissions in Chiang Mai, Thailand. Sci Total Environ 409(24):5260–5267
Quyen NH (2019) Rural poverty reduction in Vietnam 2019. Mekong Delta Research Institute Available online at https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2019/03/pdfresizer.com-pdf-resize-4.pdf, accessed on May 2021
Rehman S, Rehman E, Ikram M, Jianglin Z (2021) Cardiovascular disease (CVD): assessment, prediction and policy implications. BMC Public Health 21:1299
Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, Tian J, Shang K (2017) Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ 586:241–254
Tian Y, Liu H, Si Y, Cao Y, Song J, Li M, Wu Y, Wang X, Xiang X, Juan J, Chen L, Wei C, Gao P, Hu Y (2019) Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: a national time-series study. PLoS Med 16(1):e1002738
Tran DN, Doan VQ, Nguyen VT, Khan A, Thai PK, Cunrui H, Chu C, Schak E, Phung D (2020) Spatial patterns of health vulnerability to heatwaves in Vietnam. Int J Biometeorol 64:863–872
Turner LR, Barnett AG, Connell D, Tong S (2012) Ambient temperature and cardiorespiratory morbidity: a systematic review and meta-analysis. Epidemiology 23(4):594–606
Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, Cox PM (2015) Health and climate change: policy responses to protect public health. Lancet 386(10006):1861–1914
WBG and ADB. (2021). Climate risk country profile: Vietnam 2021: The World Bank Group and the Asian Development Bank.
WHO (2011) Mapping out vulnerable areas and population due to adverse health impacts of climate change in Viet Nam. Hanoi, Vietnam Health Environment Management Agency
Wu Y, Xu R, Wen B, Coelho MSZS, Saldiva PH, Li S, Guo Y (2021) Temperature variability and asthma hospitalisation in Brazil, 2000-2015: a nationwide case-crossover study. Thorax 76(10):962–969
Xu R, Zhao Q, Coelho MSZS, Saldiva PHN, Abramson MJ, Li S, Guo Y (2020) Socioeconomic level and associations between heat exposure and all-cause and cause-specific hospitalization in 1,814 Brazilian cities: A nationwide case-crossover study. PLoS Med 17(10):e1003369
Xuan LTT, Egondi T, Ngoan LT, Toan DTT, Huong LT (2014a) Seasonality in mortality and its relationship to temperature among the older population in Hanoi, Vietnam. Glob Health Action 7(1):23115
Xuan LTT, Van Hau P, Thu DT, Toan DTT (2014b) Estimates of meteorological variability in association with dengue cases in a coastal city in northern Vietnam: an ecological study. Glob Health Action 7(1):23119
Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S (2012) Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect 120(1):19–28
Zhai G, Zhang K, Chai G (2021) Lag effect of ambient temperature on the cardiovascular disease hospital admission in Jiuquan, China. Air Qual Atmos Health 14:181–189
Acknowledgements
DP was supported by the Research Start-up Fund of School of Medicine, Griffith University.
Author information
Authors and Affiliations
Contributions
M.R.T. conceptualized, curated data, performed data analysis and drafted the manuscript; D.P. assisted with data analysis, writing methods, and drafting the manuscript; S.R. reviewed and edited the manuscript; all the authors (M.R.T., C.C, S.R., C.H., and D.P.) contributed to review and draft of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study is one of a bigger research project in climate change and health in the Mekong Delta Region. The project was approved by the ethical committee of Griffith University (GU Ref No: ENV/23/15/HREC) and Health and Environment Management Agency, the leading agency of the health sector responsible for climate change and health in Vietnam (1290/MT-SKCD).
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Talukder, M.R., Chu, C., Rutherford, S. et al. The effect of high temperatures on risk of hospitalization in northern Vietnam. Environ Sci Pollut Res 29, 12128–12135 (2022). https://doi.org/10.1007/s11356-021-16601-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16601-8