Abstract
For the first time, the National Health and Nutrition Examination Survey (NHANES) released data on hemoglobin adducts of formaldehyde (HCHO) in public domain for US children aged 6–11 years, adolescents aged 12–19 years, and adults aged > = 20 years for 2015–2016. This study was undertaken to evaluate the associations between concentrations of HCHO in whole blood and smoking, exposure to environmental tobacco smoke (ETS), and self-reported diagnoses of cancers and asthma. Adult smokers were found to have higher adjusted concentrations of HCHO than nonsmokers (127.7 vs. 125.1 pmol/g Hb, p = 0.02). Exposure to ETS was not found to affect the adjusted concentrations of HCHO. No associations were observed between HCHO concentrations and self-reported diagnosis of “ever” cancer as well as self-reported presence of asthma at the time of participation in NHANES. HCHO concentrations were not found to differ across genders and racial/ethnic groups for children and adolescents. Among adults, non-Hispanic blacks (120.0 pmol/g Hb) had lower adjusted concentrations (p < = 0.01) of HCHO than non-Hispanic whites (128.8 pmol/g Hb), Mexican Americans (129.4 pmol/g Hb), other Hispanics (130.3 pmol/g Hb), and non-Hispanic Asians (127.9 pmol/g Hb). In conclusion, self-reported diagnoses of cancer and asthma were not found to be associated with observed concentrations of HCHO in whole blood.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Formaldehyde (HCHO), at room temperature, is a flammable gas that may cause burning sensation to the eyes, nose, and lungs at high concentrations (https://www.atsdr.cdc.gov/ToxProfiles/tp111-c1-b.pdf). HCHO is produced both by human activity and natural sources. Primary source of exposure to HCHO is by breathing air that contains HCHO. Automobile exhaust and cigarette smoke are predominant sources of HCHO air contamination. HCHO may also occur naturally in foods such as fruits.
Saccharides used as tobacco ingredients are responsible for generating HCHO in tobacco smoke (Baker 2006). HCHO is present in both mainstream and side-stream cigarette smoke. Smith et al. (2000) lists the presence of HCHO in mainstream cigarette smoke to be in the range of 3.4–283 μg/cig. Presence of HCHO in vaping products has been documented by Nicol et al. (2020), Gillman et al. (2020), and Cirillo et al. (2019). Aljadani et al. (2020) reported on the contents of water pipe smoke including genotoxic carcinogens such as HCHO.
International Agency for Research on Cancer (IARC) has classified HCHO as a human carcinogen (https://monographs.iarc.fr/wp-content/uploads/2018/06/mono100F-29.pdf, https://publications.iarc.fr/106). HCHO may be associated with cancers of nasopharynx, nasal sinuses, and others as well as leukemia. The US National Toxicology Program also listed HCHO as a known human carcinogen (https://ntp.niehs.nih.gov/whatwestudy/assessments/cancer/roc/index.html?utm_source=direct&utm_medium=prod&utm_campaign=ntpgolinks&utm_term=roc12). In a recent study of exposure to HCHO and other volatile organic compounds indoor environments in China, Zhang et al. (2020) described the predicted carcinogenic risk of formaldehyde to be greater than the threshold value of 1E-06. Kwak et al. (2020) reviewed 31 studies and based on the meta-analysis did not find strong evidence in HCHO being a risk factor for lung cancer among workers occupationally exposed to HCHO. However, significantly increased risk estimates were obtained for the recent studies. In another meta-analysis of 12 reports among those who were occupationally exposed to HCHO, Catalani et al. (2019) did not find an association between exposure to HCHO and non-Hodgkins lymphoma. However, higher risks were observed by in studies published prior to 1986. Allegra et al. (2019), based on a review of 81 articles, did not find exposure to HCHO to be a cause of acute myeloid leukemia. Masjedi et al. (2019), based on the air quality in water pipe and cigarette cafes in Tehran, Iran, estimated the lifetime risk of cancer due to HCHO exposure for water pipe and cigarette smokers. The average of lifetime cancer risk due to formaldehyde exposure through inhalation in water pipe, cigarette, water pipe and cigarette, and none-smoking cafés in weekday and weekend sessions was estimated to be 111 × 10−5 and 61.2 × 10−5, 33.7 × 10−5 and 39.4 × 10−5, 271 × 10−5 and 322 × 10−5, and 4.80 × 10−5 and 5.90 × 10−5, respectively, which, authors reported exceed the maximum limits established by the US EPA and WHO. Delikhoon et al. (2018) reported mean inhalation lifetime cancer risk for formaldehyde and acetaldehyde in summer and winter of 2017 to range between 7.55 × 10−6 and 9.25 × 10−5 in Shiraz, Iran. Based on a review of 14 studies, a majority of which were conducted in Europe, Awan et al. (2018) reported a significant association between exposure to HCHO and risk of developing oral and pharyngeal cancers.
Yu et al. (2020) reviewed the risk of asthma among children and adults when exposed to HCHO. Based on meta-analysis of 13 studies, they (Yu et al., 2020) reported each 10 μg/m3 increase in HCHO exposure to be significantly associated with a 10% increase in the risk of asthma in children, and among adults with HCHO exposure > 22.5 μg/m3, relative risk of asthma was found to be 1.81. Neamtiu et al. (2019) reported adjusted odds of 2.69 among Romanian school children when exposed to HCHO ≥ 35 μg/m3 during a school week as compared with HCHO exposure < 35 μg/m3. Yao et al. (2015) meta-analyzed data from 8 articles to evaluate association between HCHO exposure among children with and without asthma. Pooled weighted mean difference between the concentrations of HCHO among children with and without asthma was 0.021 (95% CI 0.009–0.033). Formaldehyde pollution and ventilation frequency were identified as risk factors for respiratory system disorders in both adults and children in Shenyang City, China (Zhai et al., 2013).
National Health and Nutrition Examination Survey conducted by US Centers for Disease Control and Prevention (NHANES, https://wwwn.cdc.gov/nchs/nhanes/Default.aspx) among non-institutionalized US population, for the first time, released data on HCHO in public domain for its 2015–2016 cycle. This provided an opportunity to not only study gender and racial/ethnic differences in observed concentration of HCHO but also to evaluate possible associations between HCHO concentrations and prevalence of cancers and asthma among US population. While NHANES does not collect physician diagnosed data on cancers and asthma, it does collect self-reported data on cancers and asthma via medical conditions questionnaires administered to NHANES participants in mobile examination centers. While data on self-reported asthma are collected for all NHANES participants irrespective of their age, data on self-reported cancers are collected for only those who were aged > = 20 years at the time they participated in NHANES. Participants were asked if they have ever been told by a doctor or other health care professional that they had cancer. An affirmative response is followed by asking information on specific cancer sites for up to three cancers. They are also asked the age at which each cancer was first diagnosed. Similarly, participants are asked if they have ever been told they had asthma. An affirmative response is followed by asking if they still had asthma. Data on HCHO are provided as hemoglobin adduct concentrations of HCHO. In summary, the objective of this study was to estimate associations between observed HCHO concentrations and smoking, exposure to environmental tobacco smoke (ETS), cancers, and asthma. In addition, variability in HCHO concentrations across genders and race/ethnicity will also be assessed.
Materials and methods
Data source and description
NHANES 2015–2016 data on demographics, body measures, HCHO, serum cotinine, self-reported data on cancers and asthma, and ETS exposure were downloaded and match merged by the ID of NHANES participants aged > = 6 years. Three databases, one each for children aged 6–11 years, adolescents aged 12–19 years, and adults aged > = 20 years were generated. Thus, data were separately analyzed for children aged 6–11 years, adolescents aged 12–19 years, and adults aged > = 20 years.
Definitions and categorizations
Age specific body mass index percentiles (BMIPCT) using the growth curves for US children and adolescents (https://www.cdc.gov/nccdphp/dnpa/growthcharts/training/modules/module1/text/module1print.pdf) were generated using the software provided by the US Centers for Disease Control and Prevention (https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/cdc-source-code.sas). Adolescents with serum cotinine levels > = 0.765 ng/mL and adults with serum cotinine > = 3.3 ng/mL were classified as smokers as per recommendations by Jain (2018). All children were assumed to be nonsmokers. Data on exposure to ETS at home were estimated by number of smokers smoking inside home (N_SMK) and number of days smokers smoked (D_SMK) inside during the last 7 days (https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/SMQFAM_I.htm).
Study design, software, and statistical analysis
Design and statistical analysis of this study were similar to the study by Jain (2020). Regression models stratified by children, adolescent, and adults were fitted to estimate factors affecting observed levels of HCHO. All data were analyzed by University Edition SAS (www.sas.com) Procs FREQ, UNIVARIATE, and SURVEYREG. Since data on HCHO were positively skewed, log10 transformed values of HCHO were used as dependent variables for each of the three regression models fitted to estimate factors affecting observed levels of HCHO. Independent variables used in all three models were gender (male, female), race/ethnicity (non-Hispanic white or NHW, non-Hispanic black or NHB, Mexican Americans or MA, Hispanics other than Mexican Americans or OHISP, non-Hispanic Asians or NHAS, and other unclassified race and ethnicities or OTH), age in years, poverty income ratio, N_SMK, and D_SMK. Models for children and adolescents used BMIPCT and models for adults used log10 transformed values of body mass index as independent variables to evaluate the effect of body habitus. In order to estimate the effect of smoking, smoking status (nonsmoker, smoker) was also used as an independent categorical variable for the models fitted for adolescents and adults. Self-reported diagnoses of “ever” cancer and self-reported diagnoses of asthma “now” were included as ordinal variables for the models fitted for children, adolescents, and adults. All models used sampling weights and sampling design information on strata and clustering.
Sample sizes used for the analysis are given in Table 1. Table 2 provides data on unadjusted geometric means (UGM) and Table 3 provides data on adjusted geometric means (AGM). Table 4 provides data on associations as regression slopes between log10 transformed values of HCHO and selected independent variables.
It certainly would have been appropriate to model the associations between HCHO exposure and cancers of lung and nasopharynx, leukemias, and lymphomas. However, self-reported “ever” diagnoses of these site specific cancers were too low to model the associations between HCHO exposure and these site specific cancers. Number of adult participants self-reporting lung cancer, leukemia, and lymphoma was 4, 1, and 5, respectively. Additional NHANES data in future cycles may provide large enough N to model these important associations.
Laboratory methods
Laboratory methodology to measure hemoglobin adducts of HCHO is available at https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/labmethods/FORMAL_I_MET.pdf.
Results
Prevalence of cancers and asthma
Prevalence of self-reported “ever” cancer was 9.4% among US adults (Table 1). Prevalence of self-reported “ever” asthma was 16.7% among children, 18.7% among adolescents, and 13.7% among US adults. Prevalence of self-reported asthma “now” was 12.9% among children, 11.4% among adolescents, and 7.9% among US adults (Table 1).
Unadjusted geometric means (UGM)
UGMs for HCHO were computed to be 126.6 pmol/g Hb for children, 127.7 pmol/g Hb for adolescents, and 127.8 pmol/g Hb for adults (Table 2). HCHO UGMs for children, adolescents, and adults did not vary by gender. For both children and adolescents, HCHO UGMs did not vary across various racial/ethnic groups. Smoking did not affect the HCHO concentrations for either adolescents or adults (Table 2). For adults, NHW had higher HCHO UGM than NHB (129.1 vs. 120.1 pmol/g Hb, p < 0.01), and NHB had lower HCHO UGM than MA, OHISP, and NHAS (120.1 pmol/g Hb vs. 128.4, 129.6, and 127.7 pmol/g Hb, p < =0.02, Table 2).
Adjusted analysis
Neither gender nor race/ethnicity affected the adjusted geometric means (AGM) for HCHO for children and adolescents (Table 3). Smoking did not affect AGMs for HCHO for adolescents. For adults, NHW had higher HCHO AGM than NHB (128.8 vs. 120.0 pmol/g Hb, p < 0.01), and NHB had lower HCHO AGM than MA, OHISP, and NHAS (120.0 pmol/g Hb vs. 129.4, 130.3, and 127.9 pmol/g Hb, p < =0.01, Table 2). Adult smokers had higher AGMs for HCHO than nonsmoker adults (127.7 vs. 125.1 pmol/g Hb, Table 3, p = 0.02).
Exposure to ETS was not found to affect the levels of HCHO for either children or adolescents (Table 4). However, among adults, a number of smokers smoking inside home were negatively associated with HCHO concentrations with a borderline statistical significance (p = 0.047). Neither ‘ever” diagnosis of cancer nor self-reported asthma “now” affected the HCHO concentrations for either children, adolescents, or adults (Table 4).
Discussion
NHB adults were found to have lower adjusted concentrations of HCHO than any other racial/ethnic group (Table 4). While there may be other reasons, one of the reasons may be that NHB smoke lower number of cigarettes on a daily basis than other racial/ethnic groups and thus may be exposed to lower levels of HCHO from tobacco smoke. For example, in a study about daily cigarettes smokers, Jain (2014) reported average number of cigarettes smoked by NHB, NHW, MA, and other racial/ethnic adults to be 11.4, 18.6, 10.4, and 13.7, respectively.
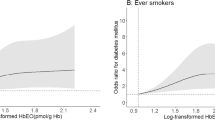
The findings of no associations between exposure to HCHO and prevalence of cancer and asthma observed for this study may be, to a degree, in contradiction to what has been reported by Zhang et al. (2020), Kwak et al. (2020), Yu et al. (2020), Neamtiu et al. (2019), and others. However, this needs to be noted that the results of this study were for the general US population, and not for those who may have been occupationally exposed to HCHO. It is in this context that the results of this study should be viewed. The focus of the analysis of this study was how observed concentrations of HCHO vary across the levels of independent variables including self-reported cancer (no, yes) and asthma (no, yes). In other words, the dependent variable for analysis for this study was the observed concentrations of HCHO. An alternate mode of analysis could have been to model the probabilities of self-reported cancer and asthma meaning analyze data with self-reported cancer (no, yes) and asthma (no, yes) as dependent variables. Then, relative odds of having self-reported cancer and asthma could have been estimated across genders and race/ethnicity as well as “high” versus “low” observed values of HCHO. For example, observed levels of HCHO above 75th percentiles could have been classified as “high” values. In fact, we did re-analyze the data by fitting logistic regression models with self-reported cancer (no, yes) and asthma (no, yes) as dependent variables. However, odds of self-reported cancer as well as asthma were not found to be any higher for those with “high” values of HCHO defined as being > = 75th percentiles of the distributions for HCHO for each age group than those with “low” values of HCHO.
When results look suspicious, there is always a way to go back to the raw data and check for authenticity of the results of statistical analysis to the degree possible. In order to do so, we plotted those who admitted having asthma “now” and cancer “ever” against their observed HCHO concentrations. These results are plotted in supplementary Fig. S1 for asthma “now” and in Fig. S2 for cancer “ever.” An inspection of these two data figures suggests that cases for asthma “now” and cancer “ever” are almost uniformly distributed across the range of observed HCHO concentrations (range for children 59.7–228.0 pmol/g Hb, range for adolescents 57.7–178.0 pmol/g Hb, range for adults: 61.9–214.0 pmol/g Hb). However, we searched for cutoffs for HCHO that will divide cases at 25% below cutoff and 75% > = cutoff. These cutoffs were 119 pmol/g Hb for children and adolescents and 115 pmol/g Hb for adults. With these newly computed cutoffs, probabilities of asthma “now” and “ever” cancer were models by SAS Proc SUYVEYLOGISTIC but relative odds of having asthma “now” and “ever” cancer were no different when HCHO > = cutoffs than HCHO < cutoffs. Hence, we must conclude, there are no associations between HCHO concentrations and self-reported asthma “now” and “ever” cancer among general US populations of children, adolescents, and adults.
References
Aljadani RH, Algabbani AM, Alamir JA, Alqahtani AS, BinDhim NF (2020) Waterpipe tobacco chemical content, microbial contamination, and genotoxic effects: a systematic review. Int J Toxicol 1091581820905108:256–262. https://doi.org/10.1177/1091581820905108
Allegra A, Spatari G, Mattioli S, Curti S, Innao V, Ettari R, Allegra AG, Giorgianni C, Gangemi S, Musolino C (2019) Formaldehyde exposure and acute myeloid leukemia: a review of the literature. Medicina (Kaunas) 55(10):E638. https://doi.org/10.3390/medicina55100638
Awan KH, Hegde R, Cheever VJ, Carroll W, Khan S, Patil S, Warnakulasuriya S (2018) Oral and pharyngeal cancer risk associated with occupational carcinogenic substances: systematic review. Head Neck 40(12):2724–2732. https://doi.org/10.1002/hed.25486
Baker RR (2006) The generation of formaldehyde in cigarettes – overview and recent experiments. Food Chem Toxicol 44:1799–1822
Catalani S, Donato F, Madeo E, Apostoli P, De Palma G, Pira E, Mundt KA, Boffetta P (2019) Occupational exposure to formaldehyde and risk of non hodgkin lymphoma: a meta-analysis. BMC Cancer 19(1):1245. https://doi.org/10.1186/s12885-019-6445-z
Cirillo S, Urena JF, Lambert JD, Vivarelli F, Canistro D, Paolini M, Cardenia V, Rodriguez-Estrada MT, Richie JP Jr, Elias RJ (2019) Impact of electronic cigarette heating coil resistance on the production of reactive carbonyls, reactive oxygen species and induction of cytotoxicity in human lung cancer cells in vitro. Regul Toxicol Pharmacol 109:104500. https://doi.org/10.1016/j.yrtph.2019.104500
Delikhoon M, Fazlzadeh M, Sorooshian A, Baghani AN, Golaki M, Ashournejad Q, Barkhordari A (2018) Characteristics and health effects of formaldehyde and acetaldehyde in an urban area in Iran. Environ Pollut 242(Pt A):938–951. https://doi.org/10.1016/j.envpol.2018.07.037
Gillman IG, Pennington ASC, Humphries KE, Oldham MJ (2020) Determining the impact of flavored e-liquids on aldehyde production during vaping. Regul Toxicol Pharmacol 112:104588. https://doi.org/10.1016/j.yrtph.2020.104588
Jain RB (2014) Trends in serum cotinine concentrations among daily cigarette smokers: data from NHANES 1999–2010. Sc Total Environ 472:72–77
Jain RB (2018) Revised and extended serum cotinine cut-offs to classify smokers and nonsmokers. Biomarkers. 23:502–507. https://doi.org/10.1080/1354750X.2018.1443516
Jain RB (2020. In Press) Associations between observed concentrations of ethylene oxide in whole blood and smoking, exposure to environmental tobacco smoke, and cancers including breast cancer: data for US children, adolescents, and adults. Environ Sc Poll Res Int 27:20912–20919
Kwak K, Paek D, Park JT (2020) Occupational exposure to formaldehyde and risk of lung cancer: a systematic review and meta-analysis. Am J Ind Med 63(4):312–327. https://doi.org/10.1002/ajim.23093
Masjedi MR, Taghizadeh F, Hamzehali S, Ghaffari S, Fazlzadeh M, Jafari AJ, Niazi S, Mehrizi EA, Moradi M, Pasalari H, Arfaeinia H (2019) Air pollutants associated with smoking in indoor/outdoor of waterpipe cafés in Tehran, Iran: concentrations, affecting factors and health risk assessment. Sci Rep 9(1):3110. https://doi.org/10.1038/s41598-019-39684-3
Neamtiu IA, Lin S, Chen M, Roba C, Csobod E, Gurzau ES (2019) Assessment of formaldehyde levels in relation to respiratory and allergic symptoms in children from Alba County schools. Romania Environ Monit Assess 191(9):591. https://doi.org/10.1007/s10661-019-7768-6
Nicol J, Fraser R, Walker L, Liu C, Murphy J, Proctor CJ (2020) Comprehensive chemical characterization of the aerosol emissions of a vaping product based on a new technology. Chem Res Toxicol 33:789–799. https://doi.org/10.1021/acs.chemrestox.9b00442
Smith CJ, Perfetti TA, Rumple MA, Rodgman A, Doolittle DJ (2000) “IARC group 2A carcinogens” reported in cigarette mainstream smoke. Food Chem Toxicol 38(4):371–383
Yao Y, Liang W, Zhu L, Duan Y, Jin Y, He L (2015) Relationship between the concentration of formaldehyde in the air and asthma in children: a meta-analysis. Int J Clin Exp Med 8(6):8358–8362
Yu L, Wang B, Cheng M, Yang M, Gan S, Fan L, Wang D, Chen W (2020) Association between indoor formaldehyde exposure and asthma: a systematic review and meta-analysis of observational studies. Indoor Air 30:682–690. https://doi.org/10.1111/ina.12657
Zhai L, Zhao J, Xu B, Deng Y, Xu Z (2013) Influence of indoor formaldehyde pollution on respiratory system health in the urban area of Shenyang. China Afr Health Sci 13(1):137–143. https://doi.org/10.4314/ahs.v13i1.19
Zhang ZF, Zhang X, Zhang XM, Liu LY, Li YF, Sun W (2020) Indoor occurrence and health risk of formaldehyde, toluene, xylene and total volatile organic compounds derived from an extensive monitoring campaign in Harbin, a megacity of China. Chemosphere 250:126324. https://doi.org/10.1016/j.chemosphere.2020.126324
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
Ram B Jain declares that he had no financial and other conflicts that could have affected the conclusions arrived at in this communication. All data used for analysis for this study are in public domain and available free of charge at www.cdc.gov/nchs/nhanes/index.htm
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Jain, R.B. Associations between observed formaldehyde concentrations and smoking, environmental tobacco smoke, and self-reported cancers and asthma: data for US children, adolescents, and adults. Environ Sci Pollut Res 27, 39180–39185 (2020). https://doi.org/10.1007/s11356-020-10007-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-10007-8