Abstract
For the first time, National Health and Nutrition Examination Survey released data on ethylene oxide (ETO) into public domain for US children aged 6–11 years, adolescents aged 12–19 years, and adults aged ≥ 20 years for 2013–2016. This study was undertaken to evaluate the associations between concentrations of ETO in whole blood and smoking, exposure to environmental tobacco smoke (ETS), and self-reported diagnosis of cancers including breast cancer. Both adolescent (29.6 vs. 49.6 pmol/g Hb, p < 0.01) and adult smokers (31.5 vs. 142.7 pmol/g Hb, p < 0.01) were found to have substantially higher adjusted levels of ethylene oxide than nonsmokers. Non-Hispanic blacks had higher levels of ethylene oxide than other race/ethnicities for children and adolescents. Non-Hispanic Asians had higher levels of ethylene oxide than other race/ethnicities for adults. Exposure to ETO measured by the number of smokers smoking inside the home (p < 0.01) and number of days smokers smoked inside the home (p = 0.03) during the prior week was found to be associated with elevated levels of ETO (p < 0.01) among US adults. Increased age was associated with elevated levels of ETO among adolescents (p = 0.02) and adults (p < 0.01) but the reverse was true for children (p = 0.04). For the general US population, levels of ETO were not found to be associated with cancers including breast cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ethylene oxide (ETO), produced for commercial use by catalytic oxidation of ethylene, is a flammable gas which easily dissolves in water, alcohol, and most organic solvents (ATSDR 1990). Produced in large quantities, it is used to make various organic chemicals such as ethylene glycol, ethanolamines, simple and complex glycols, and polyglycol ethers. In small quantities, it is also used to sterilize medical equipment and supplies in hospitals. It is also used as a fumigant to spray agricultural products. It is emitted from fossil fuels such as petroleum, natural gas, and coal, and from tobacco products (NIH, US Library of Medicine, 2019). People may be exposed to ETO if they work in industries that produce or use ETO. Nurses, doctors, and others who work in hospitals may also be exposed to ETO. ETO can be inhaled from cigarette smoke, environmental tobacco smoke (ETS), and vehicle exhaust.
According to a document (USEPA 2016) by US Environmental Protection Agency “… in EtO-manufacturing facilities and in sterilizing facilities, there is a strong evidence of an increased risk of cancer of the lymphohematopoietic system and of breast cancer in females…” and there is a “…clear evidence that EtO is genotoxic and sufficient weight of evidence to support a mutagenic mode of action for EtO carcinogenicity ...” As per USEPA, “… concentration of ethylene oxide associated with 1-in-a-million cancer risk, for a life time of continuous exposure, is 0.0002 μg/m3” (https://www.epa.gov/il/ethylene-oxide-emissions-frequent-questions). According to a 2018 document of International Agency for Cancer Research (IARC 2018), “there is limited evidence in humans for a causal associations of ethylene oxide with lymphatic and haematopoietic cancers … and breast cancer.” In a very recent review article, however, Vincent et al. (2019) concluded that USEPA’s classification of ETO as a human carcinogen overstates the underlying evidence and grossly overstates the risk. Olaguer et al. (2019) reported on an air quality modeling study in neighborhoods of a sterilization facility in Michigan and concluded the peak 24-h exposure to ETO to be “… 1.83 μg/m3 above the background level, corresponding to an additional cancer risk of approximately one in one hundred…” Bogen et al. (2019) questioned USEPA’s reliance to compute risk estimates on National Institute of Occupational Safety And Health’s epidemiological studies on sterilization facility workers exposed to ETO between 1938 and 1986. Marsh et al. (2019) executed a meta-analysis of 13 studies that reported on lympho-hematopoietic cancers and breast cancer risk among persons occupationally exposed to ETO. According to these authors (Marsh et al. 2019), based on epidemiological studies published between 2000 and 2010, exposure to ETO among ETO production and sterilization workers was not found to carry an increased risk of lympho-hematopoietic and breast cancers.
US National Health and Nutrition Examination Survey (NHANES, CDC 2020a) conducted by Centers for Disease Control and Prevention collected data on US non-institutionalized residents and released these data into public domain every 2 years. In addition to collecting data on personal and health attributes, urine and blood samples were also collected for NHANES participants. Starting 2011–2012 cycle of NHANES, data on over 30 metabolites of volatile organic compounds in urine were made available for public use for one-third of NHANES participants aged ≥ 6 years. Among the metabolites for which data were made available was N-ace-S-(2-hydroxyethyl)-l-Cys (ng/mL) or HEMA which is a metabolite of ETO and acrylonitrile as well as vinyl chloride. Jain (2015) showed children aged 6–11 years exposed to ETS to have higher levels of HEMA than nonsmoker adults aged ≥ 20 years (1.3 vs. 0.8 ng/mg creatinine, p < 0.01). Among adolescents aged 12–19 years, smokers were found to have higher adjusted levels of HEMA than nonsmokers (1.5 vs. 1.0 ng/mL, Jain 2016). St Helen et al. (2014) showed a threefold increase in the levels of HEMA among 14 nonsmokers exposed to 8 h of smoke in an automobile from a smoker in the driver’s seat. Among 17 smokers who stopped smoking, decrease in the levels of HEMA was 81–90% after 3 days (Carmella et al. 2009). Starting 2013–2014 cycle of NHANES, data were made available for ETO in whole blood. Consequently, this study was undertaken to evaluate the associations between observed concentrations of ETO and mainstream smoking, ETS, and self-reported diagnosis of cancers including breast cancer. Data for NHANES for 2013–2016 will be used for this purpose.
While link between breast and other cancers and ETO exposure has been suggested for those working in ETO manufacturing and sterilization facilities, the availability of data on ETO for general population does provide an opportunity to assess if there may be a link between cancer and ETO exposure in general population.
NHANES did not directly collect data on physician diagnoses but it did collect data on self-reported physician diagnoses including cancer diagnosis. The NHANES participants aged ≥ 20 years were asked if they have ever been told by a doctor or other health care professionals that they had cancer or a malignancy of any kind (CDC 2017a). The participants may answer yes or no, refuse to answer the question, or may say they do not know if they have ever been told about the cancer diagnoses. Follow-up questions were asked about what types of cancer they have been diagnosed with. While it was of substantial importance to know if ETO exposure and presence of cancer among NHANES participants were linked but in the absence of historical data on both cancer and ETO exposure, this possible association could not be established. Even if the participants admitted to having been diagnosed with cancer at any time in the past, without the availability of historical ETO exposure data, it was not possible to establish an association. However, in spite of this and other limitations, self-reported cancer diagnosis was included as an independent variable in the model fitted for those aged ≥ 20 years. In addition, for female data, diagnosis of breast cancer was also used as an independent variable in the model fitted for females aged ≥ 20 years.
The aim of this study was to evaluate the associations between observed concentrations of ETO and mainstream smoking, ETS, and self-reported diagnosis of cancers including breast cancer. Data will be separately analyzed for US children, adolescents, and adults.
Materials and methods
NHANES data for 2013–2016 on ETO, demographics, serum cotinine, body measures, medical questionnaire, and exposure to environmental tobacco smoke (ETS) in home were downloaded for US residents aged ≥ 6 years. Three databases, one each for children aged 6–11 years, adolescents aged 12–19 years, and adults aged ≥ 20 years were generated. Age-specific body mass index percentiles (BMIPCT) using the growth curves for US children and adolescents (CDC 2020b) were generated using the software provided by the US Centers for Disease Control and Prevention (CDC 2020c). Using recommendations provided by Jain (2018), adolescents with serum cotinine levels ≥ 0.765 ng/mL and adults with serum cotinine ≥ 3.3 ng/mL were classified as smokers. All children were assumed to be nonsmokers. Data on exposure to ETS at home were estimated by the number of smokers smoking inside home (N_SMK) and the number of days smokers smoked (D_SMK) inside during the last 7 days (CDC 2017b).
Separate regression models were fitted for children, adolescent, and adults to estimate factors affecting observed levels of ETO. University Edition SAS (www.sas.com) Procs FREQ, UNIVARIATE, and SURVEYREG were used to analyze data. Since data on ETO have been positively skewed, log10 transformed values of ETO were used as dependent variables for each of the three regression models fitted to estimate factors affecting observed levels of ETO. Independent variables used in all three models were gender (male, female), race/ethnicity (non-Hispanic white or NHW, non-Hispanic black or NHB, Mexican Americans or MA, Hispanics other than Mexican Americans or OHISP, non-Hispanic Asians or NHAS, and other unclassified race and ethnicities or OTH), age in years, poverty income ratio, N_SMK, and D_SMK. Models for children and adolescents used BMIPCT and models for adults used log10 transformed values of body mass index as independent variables to evaluate the effect of body habitus. In order to estimate the effect of smoking, smoking status (nonsmoker, smoker) was also used as an independent categorical variable for the models fitted for adolescents and adults. Self-reported diagnoses of cancers were included as an ordinal variable for the models fitted for adults. All models used sampling weights and sampling design information on strata and clustering.
Sample sizes used for the analysis are given in Table 1. Table 2 provides data on unadjusted geometric means (UGM) and Table 3 provides data on adjusted geometric means (AGM). Table 4 provides data on associations as regression slopes between log10 transformed values of ETO and selected independent variables.
Results
Male adults had higher UGM for ETO than female adults (44.7 vs. 39.0 pmol/g Hb, p < 0.01; Table 2). NHB had the highest UGMs for ETO among various other race/ethnicities. The order of UGMs by race/ethnicity for children was NHB (41.4 pmol/g Hb) > NHAS (39.8 pmol/g Hb) > MA (32.3 pmol/g Hb) > OTH (31.6 pmol/g Hb) > OHISP (31.2 pmol/g Hb) > NHW (30.6 pmol/g Hb). For adolescents, this order was as follows: NHB (37.9 pmol/g Hb) > OTH (33.9 pmol/g Hb) > NHAS (31.6 pmol/g Hb) > NHW (30.8 pmol/g Hb) > OHISP (29.5 pmol/g Hb)) > MA (28.8 pmol/g Hb). The order of UGMs by race/ethnicity for adults was NHB (59.4 pmol/g Hb) > OTH (44.8 pmol/g Hb) > NHW (40.4 pmol/g Hb) > NHAS (39.8 pmol/g Hb) > OHISP (39.4 pmol/g Hb) > MA (35.3 pmol/g Hb). Adolescent smokers had more than twice the UGM for ETO than adolescent nonsmokers (55.9 vs. 27.2 pmol/g Hb, p < 0.01, Table 2). Adult smokers had more than five times the UGM for ETO than adult nonsmokers (141.0 vs. 26.4 pmol/g Hb, p < 0.01, Table 2).
While adjusted ETO levels were almost similar for children and adolescents at 34.2 and 38.3 pmol/g Hb, the adjusted levels were substantially higher among adults at 67.1 pmol/g Hb (Table 3). AGMs for ETO did not differ by gender for children, adolescents, and adults (Table 3). NHB children had statistically significantly higher AGMs for ETO (41.4 pmol/g Hb, Table 3) than NHW (30.1 pmol/g Hb, Table 3, p < 0.01), MA (32.4 pmol/g Hb, Table 3, p < 0.01), and OHISP (31.8 pmol/g Hb, Table 3, p < 0.01). AGMs for ETO for adolescents did not differ by race/ethnicity (Table 3). NHB adults had higher AGMs (68.8 pmol/g Hb, Table 3) than NHW (60.0 pmol/g Hb, Table 3, p = 0.03). NHAS adults had higher AGMs for ETO than NHW (74.6 vs. 60.0 pmol/g Hb, Table 3, p < 0.01) and MA (74.6 vs. 63.9 pmol/g Hb, Table 3, p = 0.04). Adolescent smokers had higher ETO than nonsmokers (49.6 vs. 29.6 pmol/g Hb, Table 3, p < 0.01). Adjusted levels of ETO for adult smokers were more than four times the levels for adult nonsmokers (142.7 vs. 31.5 pmol/g Hb, Table 3, p < 0.01).
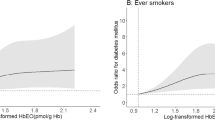
Among adolescents (β = 0.01424, p = 0.02, Table 4) and adults (β = 0.00125, p < 0.01, Table 4), age was positively associated with the levels of ETO meaning adjusted levels of ETO increased as participants became older. When the model for adults was fitted with just the females in the model, age was still positively associated with the levels of ETO (β = 0.00102, p = 0.03). However, among children, younger children had higher ETO levels than older children (β = − 0.01079, p = 0.04, Table 4). Among adults, BMI was negatively associated with the levels of ETO (β = − 0.01853, p < 0.01, Table 4). It was only among adults that exposure to ETS was associated with higher levels of ETO (β = 0.08464, p < 0.01, for the number of smokers smoking inside the home and β = 0.02043, p = 0.021, for the number of days smokers smoked inside the home in the prior week). ETO exposure inside the home was not found to affect ETO levels among children and adolescents (Table 4). Self-reported diagnosis of cancer was not found to affect adjusted levels of ETO (β = − 0.01511, p = 0.34, Table 4). Self-reported diagnosis of breast cancer among females was also not found to affect adjusted levels of ETO (β = 0.02118, p = 0.52, Table 4).
Discussion
There was no evidence of a link between ETO and cancers including breast cancer. Valdez-Flores et al. (2010) reported on the analysis of the updated and pooled studies of over 19,000 workers, examined twelve cancer endpoints and six cohorts or sub-cohorts, and reported none of these 72 combinations resulted in a statistically significant increase in cancer risks including the risks for leukemia, lymphohematopoietic tissue, lymphoid tumors, and breast cancer. Thus, results reported by Valdez-Flores et al. (2010) lend support to the findings in this manuscript.
Kirman and Hays (2017) reported that the levels of endogenous equivalent concentrations in the blood of humans correspond to external exposures of ETO between 0.13 and 6.9 ppb of ETO in the air. These ETO air concentrations are orders of magnitude larger than EPA’s proposed maximum air concentration of 0.0001 ppb and in the range of the Texas Commission on Environmental Quality (TCEQ) proposed maximum air concentration of 4 ppb (TECQ 2020). For this study, smokers were found to have the maximum AGM of 142.7 pmol/g Hb for ETO among adult smokers. In order to convert this AGM into equivalent ETO air concentrations, we divided 142.7 by 10.9 in accordance with Eq. 3 of Kirman and Hays (2017), and this came out to be 13.1 ppb. Thus, it can be stated that ETO air concentration less than 13.1 ppb is not likely to cause any type of cancer including breast cancer.
Smoking was associated with manifold higher levels of ETO among US adults and 68% higher levels among US adolescents compared with nonsmokers. These results are not surprising. Among adults, exposure to ETS was associated with 21.5% higher levels of ETO for every additional smoker smoking inside the house and with 4.8% higher levels of ETO for every additional day smokers smoked inside the house during the prior week. That too should not be surprising. However, exposure to ETS could not be found to be associated with higher levels of ETO even though regression slopes (Table 4) associated with both the number of smokers smoking inside the home and number of days smokers smoked inside the home the prior week were positive for both adolescents and children (Table 4). We do not know the reason for this but relatively small sizes for children and adolescents may be responsible for this. Additional NHANES data in the future may be helpful.
Conclusion
-
There was no association between ETO whole blood concentrations and self-reported diagnosis of cancers including breast cancer.
-
Smoking was associated with elevated concentrations of ETO for both US adults and adolescents.
-
Exposure to ETS was associated with increased levels of ETO among US adults but not among US children and adolescents.
Limitations of the study
Data analysis for this study was limited by non-availability of data on occupational exposure to ETO. To what degree this limitation will affect the observed absence of association between cancers including breast cancer and ETO exposure is not known. It will depend on the percent of adults selected for participation in NHANES who actually worked in occupations where they may be exposed to ETO and to what degree they may be exposed to additional levels of ETO in those occupations. This introduces some level of uncertainty about null results obtained for the associations between ETO and cancers. However, in the absence of any other information, the only way to look at it is the R2 of the models that were fitted. A low R2 depicts unexplained variability in the data which may negatively reflect on the model conclusions arrived at. However, for the models fitted for this study for adults, R2 was 57.6% when both males and females were modeled together and 66.3% when only females were modeled. These are considered very healthy R2’s by any statistical standards. Consequently, there does not seem to be any reason that should make observed null association between cancer and ETO levels suspect.
Any statistical analysis, and, in particular, regression analysis with multiple predictors as was the case for this study, is suspected to result in false positives as well as false negatives. False positives meaning falsely detecting statistically significant differences, when, in fact, they do not exist, can be, to some degree, controlled by adjusting p values for the differences for multiple comparisons by using one of the several methods that are available. This was the approach adopted for this study. False negatives meaning declaring null differences when, in fact, the differences do exist, is an issue that may not be that easy to control. However, it should be noted that false positives and false negatives are negatively associated. Unnecessary emphasis or being too conservative about protecting against false positives may lead to false negatives. True protections against both false positives and false negatives can only be achieved by having large enough sample sizes to provide enough power for statistical tests and to have good quality balanced data for analysis. It is in this sense that we look at the results about association of ETS with ETO as depicted in Table 4. While the sample size of 3955 for adults was almost indisputably large and this did result in the expected conclusion that ETS was positively associated with ETO, sample sizes of 650 for children and 776 for adolescents (Table 1) were still large enough by any statistical standards but did not generate the expected positive association between ETS and ETO. However, it may be that ETO and ETS are not positively associated for children and adolescents. But, the slopes for both the number of smokers smoking inside the home and the number of days the smokers smoked in the prior week inside the home were still positive (Table 4), just not statistically significant. Could it be the quality of data? For the adults data, 19.6% (N = 734) reported smoking inside the home, but for the adolescents data, 11.1% (N = 86) reported smoking inside the home, and for children data, 12.3% (N = 80) reported smoking inside the home. Thus, data for children and adolescents were a bit more “imbalanced” than for adults. This may have resulted in association between ETO and ETS being positive but statistically insignificant for both adolescents and children. The message here is as follows: respect the data and do not try to find a statistical method that will generate results to your liking. It may be that parents with children no longer smoke inside the home so as to protect them from ETS.
Data availability
All data used for analysis for this study are in public domain and available free of charge at www.cdc.gov/nchs/nhanes/index.htm
References
ATSDR. Agency for Toxic Substances and Disease Registry. Toxic substances – portal. 1990. Available at https://www.atsdr.cdc.gov/phs/phs.asp?id=732&tid=133. Last accessed on February 23, 20202
Bogen KT, Sheehan PJ, Valdez-Flores C, Li AA (2019) Reevaluation of historical exposures to ethylene oxide among U.S. sterilization workers in the National Institute of Occupational Safety and Health (NIOSH) study cohort. Int J Environ Res Public Health 16(10):E1738. https://doi.org/10.3390/ijerph16101738
Carmella SG, Chen M, Han S, Briggs A, Jensen J, Hatsukami DK, Hecht SS (2009) Effects of smoking cessation on eight urinary tobacco carcinogen and toxicant biomarkers. Chem Res Toxicol 22(4):734–741. https://doi.org/10.1021/tx800479s
CDC. Centers for Disease Control and Prevention. Medical conditions. 2017a. Available at https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/MCQ_I.htmAccessed 23 February 2020
CDC. Centers for Disease Control and Prevention. Medical conditions. 2017b. Available at https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/SMQFAM_I.htm. Last accessed on February 23, 2020
CDC. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. 2020a. Available at https://wwwn.cdc.gov/nchs/nhanes/default.aspx. Last accessed on February 23, 2020
CDC. Centers for Disease Control and Prevention. Using the BMI-for-age growth charts. 2020b. https://www.cdc.gov/nccdphp/dnpa/growthcharts/training/modules/module1/text/module1print.pdf. Last accessed on February 23, 2020
CDC. Centers for Disease Control and Prevention. SAS Code for Growth Charts. 2020c. Available at https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/cdc-source-code.sas. Last accessed on February23, 2020
IARC. International Agency for Research on Cancer. Ethylene oxide. 2018. Available at https://monographs.iarc.fr/wp-content/uploads/2018/06/mono100F-28.pdf. Last accessed on February 25, 2020
Jain RB (2015) Levels of selected urinary metabolites of volatile organic compounds among children aged 6-11 years. Environ Res 142:461–470. https://doi.org/10.1016/j.envres.2015.07.023
Jain RB (2016) Levels of selected urinary metabolites of volatile organic compounds in a representative sample of US adolescents. Toxicol Environ Chem 98(8):977–990. https://doi.org/10.1080/02772248.2015.1132319
Jain RB (2018) Revised and extended serum cotinine cut-offs to classify smokers and nonsmokers. Biomarkers. 23:502–507. https://doi.org/10.1080/1354750X.2018.1443516
Kirman CR, Hays SM (2017) Derivation of endogenous equivalent values to support risk assessment and risk management decisions for an endogenous carcinogen: ethylene oxide. Regul Toxicol Pharmacol 91:165–172. https://doi.org/10.1016/j.yrtph.2017.10.032
Marsh GM, Keeton KA, Riordan AS, Best EA, Benson SM (2019 Oct) Ethylene oxide and risk of lympho-hematopoietic cancer and breast cancer: a systematic literature review and meta-analysis. Int Arch Occup Environ Health 92(7):919–939. https://doi.org/10.1007/s00420-019-01438-z
NIH US Library of Medicine. Chemicals and contaminants. What is ethylene oxide? Available at https://toxtown.nlm.nih.gov/chemicals-and-contaminants/ethylene-oxide. 2019. Last accessed on February 23, 2020
Olaguer EP, Robinson A, Kilmer S, Haywood J, Lehner D (2019) Ethylene oxide exposure attribution and emissions quantification based on ambient air measurements near a sterilization facility. Int J Environ Res Public Health 17(1):E42. https://doi.org/10.3390/ijerph17010042
St Helen G, Jacob P r, Peng M, Dempsey DA, Hammond SK, Benowitz NL (2014) Intake of toxic and carcinogenic volatile organic compounds from secondhand smoke in motor vehicles. Cancer Epidemiol Biomark Prev 23(12):2774–2782. https://doi.org/10.1158/1055-9965.EPI-14-0548
TECQ. Texas Commission on Environmental Quality. Ethylene oxide carcinogenic dose-response assessment. Available at https://www.tceq.texas.gov/assets/public/implementation/tox/dsd/proposed/eto.pdf. Last accessed on February 25, 2020
USEPA. United States Environmental Protection Agency. Evaluation of the inhalation carcinogenicity of ethylene oxide. Executive Summary. 2016. Available at https://cfpub.epa.gov/ncea/iris/iris_documents/documents/subst/1025_summary.pdf. Last accessed on February 25, 2020
Vincent MJ, Kozal JS, Thompson WJ, Maier A, Dotson GS, Best EA, Mundt KA (2019 Dec 11) Ethylene oxide: cancer evidence integration and dose-response implications. Dose Response 17(4):1559325819888317. https://doi.org/10.1177/1559325819888317
Valdez-Flores C, Sielken RL Jr, Teta MJ (2010) Quantitative cancer risk assessment based on NIOSH and UCC epidemiological data for workers exposed to ethylene oxide. Regul Toxicol Pharmacol 56(3):312–320. https://doi.org/10.1016/j.yrtph.2009.10.001
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Additional information
Responsible editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jain, R.B. Associations between observed concentrations of ethylene oxide in whole blood and smoking, exposure to environmental tobacco smoke, and cancers including breast cancer: data for US children, adolescents, and adults. Environ Sci Pollut Res 27, 20912–20919 (2020). https://doi.org/10.1007/s11356-020-08564-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-08564-z