Abstract
Meta-analysis with high-quality studies can provide superior evidence. In this paper, we use meta-analysis to analyze the relationship between cadmium (Cd) content in semen and male infertility, and then objectively evaluate the effect of Cd on sperm quality. The objectives of this study were to update our understanding of infertility and to provide evidence to treat and prevent the infertility. We searched potentially relevant studies that were published from establishing database data to April 2018. Articles came from the databases of CNKI, Wanfang, VIP, PubMed, CMCI, and EMBASE. A total of 11 articles were included. We gathered the mean and variance of the infertility group and the control group to compare the Cd content in two groups. In total, the 11 studies include 1707 subjects, 1093 of which were in the infertility group and 614 of which were in the control group. We can get some information from this meta-analysis: SMD = 0.50 (95% Cl 0.39–0.61), Z = 8.92, P < 0.05; the funnel plot of the meta-analysis shows incomplete symmetry, which may have the publication bias. Therefore, the high content of Cd in semen is a causative factor of infertility. The Cd content in semen can be used as an indicator of sperm quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infertility generally refers to the couples of childbearing age who do not have contraception, but have no kids of their own for 1 year or longer after marriage (Agarwal et al. 2010). According to WHO’s findings in 2008, the incidence rate of infertility was about 15% in childbearing couples all over the world; the incidence of male infertility accounts for 30% in infertility couples (Pritts et al. 2009). Male infertility is divided into sexual dysfunction and normal sexual function in clinical; the latter can be further divided into azoospermia, asthenospermia, and sperm number normal infertility according to the result of semen analysis (Frühmesser et al. 2013; Lotti and Maggi 2018). Today, male infertility can be cured and multiple pathogenic factors of infertility have been found, but infertility still exists (Kefer et al. 2010). Therefore, it is important to update our understanding of the infertility etiology, which can be used to prevent and treat this disease. In these hypotheses, trace element plays an important role in reproductive system diseases (Saglam et al. 2015). After searching for a series of literatures on trace element and reproductive system, we decided to study the association between Cd content in semen and infertility.
Cd is a kind of rare element in nature, which was first found by F. Strohmaier in 1817. Cd was mainly applied in the nickel-cadmium battery, pigment, painting, and plastic production since 1960 (Bulat et al. 2009; Chen et al. 2018). Although Cd plays an important role in industry, it is a toxic metal; excess Cd in the human body will lead to chronic poisoning. Usually, we believe that when the concentration of cadmium in the blood of patients is greater than 30 μg/L, it is chromium poisoning (Li et al. 2017; Semczuk and Semczuksikora 2001) (Yang et al. 2013). Today, with the strong demand for pollution control and health, more and more researches on Cd have been carried out. In some animal experiments, male rats were exposed to Cd by feeding or injecting different doses of chromium chloride; these rats were used to compare their Cd content, enzyme activity, and the amount of spermatogenesis in the testis. Stained histological sections of testes and epididymis of the CdCl2-treated group reveal a degradation of the seminiferous tubules and deformity in spermatogenesis as well as absence of spermatozoa; a decrease in the seminal vesicular secretion was noted in CdCl2-treated mice (Bataineh et al. 1997; Oguzturk et al. 2012) (Ponnapakkam et al. 2003). In some regional surveys, the size of the testicles, the amount of semen, the percentage of immature spermatocyte, and other data were measured as reproductive parameters by controlling the physical condition and diet (Laskey et al. 1986). These findings suggest that the rise of Cd content in semen can lead to infertility. Therefore, we made a systematic analysis of these findings to illustrate the reliability of this result. Meta-analysis is a kind of systematic review and a research process (Keene et al. 2012; DerSimonian and Laird 1986). It combines the results of several studies in the same subject, determines the average level of different studies, evaluates the conclusion of different researches, and casts about for new hypotheses and research ideas (HM et al. 2014). So far, no one has discussed Cd content and infertility from the perspective of meta-analysis. In this paper, we reported a meta-analysis of published articles to assess the association between Cd and infertility, which was based on the definition of causation in evidence-based medicine to update our understanding of Cd and the etiology of infertility and provide quality evidence for Cd surveillance, prevention, and infertility treatment.
Data acquisition
Data sources
Meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. We searched for potentially relevant studies that were published from establishing database data to April 2018. Articles came from the databases of CNKI (China National Knowledge Infrastructure), Wanfang (Wanfang Data Knowledge Service Platform), VIP (Database for Chinese Technical Periodicals), PubMed (Public Medline), CMCI (Chinese Medical Citation Index), and EMBASE (Excerpt Medical Database). Keywords were as follows: cadmium, infertility, human, semen, reproductive system.
Inclusion criteria
(1) The randomized controlled trial (RCT) was used in the study. (2) The subjects of the experimental group were infertile patients or the people whose sperm survival rate was less than 40%, while the subjects of the control group were normal male (Liu 1986). (3) The article provides sufficient information such as the title, the name of first author, the journal and the publication year, the sample size of the experimental group and the control group, the number of cases, and the content of Cd.
Exclusion criteria
(1) No RCT tests, repeated documents, individual cases, incomplete information, and animal tests. (2) Experimenters who take medicine that affect sperm activity, or the subjects of the experiments have inherited disease and other unhealed disease.
Cochrane systematic reviews
Cochrane systematic reviews provide information about the effectiveness of interventions by identifying, appraising, and summarizing the results of otherwise unmanageable quantities of primary research to provide valid, reliable evidence for health decision-making and clinical practice (Chandler and Hopewell 2013). They differ from traditional reviews produced by “content experts” in that they use a replicable, scientific, and transparent approach that seeks to minimize bias (Meerpohl et al. 2008). We use the following criteria for evaluation.
-
1.
The generation of random order: in the RCT paper, the method of generating random order should be described in detail, therefore the evaluator can judge whether there are comparable among the groups allocated by this method. Further, the groups were classified according to their description and degree of detail.
-
2.
Allocation concealment for random schemes: in the random distribution scheme test, the random allocation scheme should be assigned to the random allocation scheme, so that the researchers and the research objects cannot predict the order of distribution in the process of grouping. If no allocation concealment is adopted, the possibility of bias will be increased. Therefore, the method of hiding the random allocation scheme should be described in detail. In that case, the assessor can judge the bias risk of the paper.
-
3.
A blind method and a measurement bias for the subjects: in the RCT paper, we should describe whether blindness is applied to research subjects and intervention implementers. In the process of study, if the research object or the intervention implementer knows the group situation and the intervention measures adopted by the group, it will increase the possibility of implementing bias or measuring bias.
-
4.
A blind method and a measurement bias for the result evaluators: it is necessary to describe in detail whether each evaluation index in the study is blind to the outcome evaluator. If the outcome evaluator knows which group the subjects were assigned to and what intervention measures were adopted, it will increase the likelihood of detection/measurement bias. We should evaluate each major outcome indicator in the study.
-
5.
Completeness of outcome index data: incomplete outcome data for each indicator should be described in detail, the number of missing and drop out groups and their reasons need to be reported. The results of the system evaluation should be brought into data analysis again. The quantity, characteristics, and improper handling methods of incomplete outcome data will increase the likelihood of missed visit bias.
-
6.
The possibility of selective reporting of the results: the author of the systematic reviews should explain how to judge the possibility of selective reporting and whether the results of selective reports are available. Selective reporting of the results expected by researchers will lead to reporting bias.
-
7.
Other sources of bias: other factors that may lead to bias in the implementation process should be described, unless there are no other factors leading to bias in the implementation process.
Statistical treatment
All analyses were performed by Review Manager Software (version 5.3). Standard statistical tables and graphs were used to describe the characteristics of the surveyed subjects. We use the mean and variance of these studies to plot. Q test is used to determine whether the result is heterogeneous, if there is no significant difference in Q test (P > 0.10, I2 ≤ 50%), we use fixed effect model to analyze data; if there is a significant difference in Q test (P < 0.10, I2 > 50%), we use a random effect model to analyze data. The result of the meta-analysis has statistical difference if the P value is less than 0.05.
Data analysis
Literature search
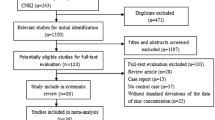
The literature search strategy identified 1856 unique citations, which came from different databases (Fig. 1). After a preliminary inspect of title and abstract, we identified 112 distinct studies as potentially relevant studies for further investigation. In these studies, 82 studies did not have clear experimental background, 16 studies did not have complete data, and 3 studies did not have control groups. Only 11 studies fit with the inclusion criteria and were included in the meta-analysis. The information related to these articles was shown in Table 1. The results of the quality assessment for these articles are shown in Fig. 2.
Meta-analysis
Figure 3 is the forest plot; it has heterogeneity (P < 0.05, I2 = 59%). Thus, we chose random effects models to assess all the studies. In total, the 11 studies included 1707 subjects, 1093 of which were in infertility group and 614 of which were in the control group. We can get some information from this meta-analysis: SMD = 0.50 (95% Cl 0.39–0.61), Z = 8.92, P < 0.05, the funnel plot of meta-analysis shows incomplete symmetry, considering the publication bias (Fig. 4).
Discussion
Infertility is a disease which concerned all over the world. In infertility, male infertility accounts for a large proportion and was on the rise in recent years (Desai and Sharma 2009). The main reason for male infertility is the decrease of sperm activity and quantity (Du et al. 2010; Kitamura et al. 2015). In recent years, with the aggravation of environmental pollution and the pressure of life, the quality of semen dropped sharply (Wittmaack and Shapiro 1992). In some reports on semen quality testing, we can see that in some work fields of long-term exposure to heavy metals, the probability of male infertility is greatly increased (Ho and Wei 2013; Wirth and Mijal 2010). Although infertility can be treated with surgery and drug method, the cause of the disease is still unclear. An important hypothesis for the etiology of oligoasthenospermia is Cd pollution. It is necessary to clarify whether the increase of Cd in semen is a causative factor of infertility. Therefore, we conducted a study of meta-analysis, which has not been applied to the association between Cd and male infertility in the past.
Cd is a kind of harmful metal element, is widely used in industrial production, and Cd can affect the human body by food, water, dust, and so on (Liu et al. 2007). A major way of Cd poisoning is the Cd inevitably accumulated in the environment and then transfer into the human body through the food chain. In recent years, the number of Cd toxicity reports was increasing. In many studies of Cd, some people found that the reproductive system is one of the target organs that is sensitive to Cd, which reduces the androgen production by injuring the testicles, lowering the androgen secretion, and affecting the sperm production to reduce the male reproductive capacity (Ponnapakkam et al. 2003). In this study, Table 1 shows that the increase of Cd content in semen causes infertility. In addition, the information of the forest graph shows that the difference of Cd content between the infertile group and the control group has a significant quantitative value, which suggests that the incidence of infertility has a causal relationship with Cd content. The funnel plot presents asymmetry, which means that there may be bias. Egger and Begg’s test results show that there is no publication bias in this study. Therefore, we believe that the excessive Cd content in semen is one of the causative factors of infertility.
Importance of the study
The purposes of the etiological study are finding the side effects of the treatment and the causative factors of infertility and providing evidence for practice (Salort-Llorca et al. 2008). According to the fifth edition of the human semen Laboratory Test Manual published by WHO in 2010, “normal semen standard” (Sakai et al. 2011), we can find that the current semen detection standards have nine indicators, including semen appearance, semen volume, pH value, liquefaction time, sperm density, sperm count, sperm motility, normal morphology, and white blood cells. In this study, based on the results of the study, we believe that the Cd content should be included in the semen detection index. High Cd content significantly increases the risk of infertility. As a result, Cd exposure should also be considered as a variable in the reproductive system–related experiments and instructed in the relevant articles on prevention and treatment of infertility to provide more reliable evidence for the detection and evaluation of infertility.
Strengths and limitations
This study has several strengths. Firstly, it is the first article, which uses meta-analysis method to study the relationship between Cd content and infertility in semen. This study is a summary of the relationship between Cd and infertility in the past few decades, which can be used to identify infertility. Secondly, the study updates our understanding of infertility and provides comprehensive evidence for infertility so far. Finally, the result of this study can be applied to the detection of semen quality and increase the standard of semen detection. The main limitation of this article is that there are 11 documents with 1701 cases in this study. These results were published from 1989 to 2012, which is not conducive to our research on male infertility in recent years.
Conclusion
In summary, the high level of Cd in semen is widespread in infertility patients; Cd is a factor leading to low sperm quality. When carrying out semen detection, Cd content should be an index for sperm activity. This study uses evidence-based medicine and systematic analysis to analyze the relationship between Cd and infertility, which is helpful to correctly evaluate the causative factors of infertility and provide clues and ideas for future research.
References
Agarwal A, Makker K, Sharma R (2010) Review article: clinical relevance of oxidative stress in male factor infertility: an update. Am J Reprod Immunol 59:2–11. https://doi.org/10.1111/j.1600-0897.2007.00559.x
Bataineh H, Al-Hamood MH, Elbetieha A, Bani HI (1997) Effect of long-term ingestion of chromium compounds on aggression, sex behavior and fertility in adult male rat. Drug Chem Toxicol 20:133–149. https://doi.org/10.3109/01480549709003875
Bulat ZP, Dukic-Cosic D, Dokic M, Bulat P, Matovic V (2009) Blood and urine cadmium and bioelements profile in nickel-cadmium battery workers in Serbia. Toxicol Ind Health 25:129–135
Chandler J, Hopewell S (2013) Cochrane methods--twenty years experience in developing systematic review methods. Syst Rev 2:76
Chen T et al. (2009) Correlation of trace elements with male infertility. Chin J Health Lab Technol 155–156
Chen M, Li X, Fan R, Yang J, Jin X, Hamid S, Xu S (2018) Cadmium induces BNIP3-dependent autophagy in chicken spleen by modulating miR-33-AMPK axis. Chemosphere 194:396–402. https://doi.org/10.1016/j.chemosphere.2017.12.026
Chia SE, Ong CN, Lee ST, Tsakok FHM (1992) Blood concentrations of lead, cadmium, mercury, zinc, and copper and human semen parameters. Arch Androl 29:177–183. https://doi.org/10.3109/01485019208987722
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Desai N, Sharma RK (2009) Physiologic and pathologic levels of reactive oxygen species in neat semen of infertile men. Fertil Steril 92:1626–1631. https://doi.org/10.1016/j.fertnstert.2008.08.109
Du PS, Cabler S, Mcalister DA, Sabanegh E, Agarwal A (2010) The effect of obesity on sperm disorders and male infertility. Nat Rev Urol 7:153–161. https://doi.org/10.1038/nrurol.2010.6
Frühmesser A, Vogt PH, Zimmer J, Witsch-Baumgartner M, Fauth C, Zschocke J, Pinggera GM, Kotzot D (2013) Single nucleotide polymorphism array analysis in men with idiopathic azoospermia or oligoasthenozoospermia syndrome. Fertil Steril 100:81–87. https://doi.org/10.1016/j.fertnstert.2013.03.016
HM V et al (2014) Meta-analysis of data from animal studies: a practical guide. J Neurosci Methods 221:92–102. https://doi.org/10.1016/j.jneumeth.2013.09.010
Ho HY, Wei HJ (2013) The relationship between heavy metal exposure and risk of infertility in Taiwan. Fertil Steril 100:S12–S12. https://doi.org/10.1016/j.fertnstert.2013.07.160
Hovatta O, Venäläinen ER, Kuusimäki L, Heikkilä J, Hirvi T, Reima I (1998) Aluminium, lead and cadmium concentrations in seminal plasma and spermatozoa, and semen quality in Finnish men. Hum Reprod 13:115–119. https://doi.org/10.1093/humrep/13.1.115
Keck C, Bramkamp G, Behre HM, Müller C, Jockenhövel F, Nieschlag E (1995) Lack of correlation between cadmium in seminal plasma and fertility status of nonexposed individuals and two cadmium-exposed patients. Reprod Toxicol 9(35):35–40. https://doi.org/10.1016/0890-6238(94)00053-Y
Keene DJ, Sajad Y, Rakoczy G, Cervellione RM (2012) Testicular volume and semen parameters in patients aged 12 to 17 years with idiopathic varicocele. J Pediatr Surg 47:383–385. https://doi.org/10.1016/j.jpedsurg.2011.11.035
Kefer JC, Agarwal A, Sabanegh E (2010) Role of antioxidants in the treatment of male infertility. Int J Urol 16:449–457. https://doi.org/10.1111/j.1442-2042.2009.02280.x
Kitamura A, Miyauchi N, Hamada H, Hiura H, Chiba H, Okae H, Sato A, John RM, Arima T (2015) Epigenetic alterations in sperm associated with male infertility. Congenit Anom 55:133–144. https://doi.org/10.1111/cga.12113
Laskey JW, Rehnberg GL, Laws SC, Hein JF (1986) Age-related dose response of selected reproductive parameters to acute cadmium chloride exposure in the male long〦vans rat. J Toxicol Environ Health 19:393–401. https://doi.org/10.1080/15287398609530937
Li X, Xing M, Chen M, Zhao J, Fan R, Zhao X, Cao C, Yang J, Zhang Z, Xu S (2017) Effects of selenium-lead interaction on the gene expression of inflammatory factors and selenoproteins in chicken neutrophils. Ecotoxicol Environ Saf 139:447–453. https://doi.org/10.1016/j.ecoenv.2017.02.017
Liu J (1986) Studies in technic of cryopreservation for human spermatozoa by liquid nitrogen vapor——I. Effects on sperm survival rate of different methods of storage and different times of cold—balance. doi:https://doi.org/10.13361/j.qdyxy.1986.04.003
Liu J, Qian M, Cai G, Yang J, Zhu Q (2007) Uptake and translocation of Cd in different rice cultivars and the relation with Cd accumulation in rice grain. J Hazard Mater 143:443–447. https://doi.org/10.1016/j.jhazmat.2006.09.057
Lotti F, Maggi M (2018) Sexual dysfunction and male infertility. Nat Rev Urol 15:287–307. https://doi.org/10.1038/nrurol.2018.20
Meerpohl JJ, Timmer A, Antes G (2008) Evidence-based medicine and systematic reviews. Mmw Fortschr Med 150:41–43. https://doi.org/10.1007/BF03365424
Mendiola J, Moreno JM, Roca M, Vergara-Juárez N, Martínez-García MJ, García-Sánchez A, Elvira-Rendueles B, Moreno-Grau S, López-Espín JJ, ten J, Bernabeu R, Torres-Cantero AM (2011) Relationships between heavy metal concentrations in three different body fluids and male reproductive parameters: a pilot study. Environ Health 10:6. https://doi.org/10.1186/1476-069X-10-6
Oguzturk H, Ciftci O, Aydin M, Timurkaan N, Beytur A, Yilmaz F (2012) Ameliorative effects of curcumin against acute cadmium toxicity on male reproductive system in rats. Andrologia 44:243–249. https://doi.org/10.1111/j.1439-0272.2012.01273.x
Ponnapakkam TP, Bailey KS, Graves KA, Iszard MB (2003) Assessment of male reproductive system in the CD-1 mice following oral manganese exposure. Reprod Toxicol 17:547–551. https://doi.org/10.1016/S0890-6238(03)00101-1
Pritts EA, Parker WH, Olive DL (2009) Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril 91:1215–1223. https://doi.org/10.1016/j.fertnstert.2008.01.051
Saaranen M, Kantola M, Saarikoski S, Vanha-Perttula T (1989) Human seminal plasma cadmium: comparison with fertility and smoking habits. Andrologia 21:140–145
Saglam HS, Altundag H, Atik YT, Dundar MS, Adsan O (2015) Trace elements levels in the serum, urine, and semen of patients with infertility. Turk J Med Sci 45:443–448
Sakai S, Wakasugi T, Yagi K, Ohnishi A, Ito N, Takeda Y, Yamagishi M (2011) Successful pregnancy and delivery in a patient with adult GH deficiency: role of GH replacement therapy. Endocr J 58:65–68. https://doi.org/10.1507/endocrj.K10E-208
Salort-Llorca C, Mínguez-Serra MP, Silvestre FJ (2008) Drug-induced burning mouth syndrome: a new etiological diagnosis. Med Oral Patol Oral Cir Bucal 13:E167–E170
Semczuk M, Semczuksikora A (2001) New data on toxic metal intoxication (Cd, Pb, and Hg in particular) and Mg status during pregnancy. Med Sci Monit 7:332–340
Shaoxian L et al. (1994) Determination of eight elements in semen of infertile patients and normal persons and analysis of zinc to cadmium ratio. J Reprod Med 84–86
Telisman S, Cvitković P, Jurasović J, Pizent A, Gavella M, Rocić B (2000) Semen quality and reproductive endocrine function in relation to biomarkers of lead, cadmium, zinc, and copper in men. Environ Health Perspect 108:45–53. https://doi.org/10.1289/ehp.0010845
Wirth JJ, Mijal RS (2010) Adverse effects of low level heavy metal exposure on male reproductive function. Syst Biol Reprod Med 56:147–167. https://doi.org/10.3109/19396360903582216
Wittmaack FM, Shapiro SS (1992) Longitudinal study of semen quality in Wisconsin men over one decade. Wis Med J 91:477
Xiaojia W, Ziming H, Chunli L (1995) Analysis of trace elements zinc, copper, lead and cadmium in human semen. Reprod Contracept 393–395
Xu Z (2012) Detection and analysis of trace elements of seminal plasma in male infertility. Hainan Med J. https://doi.org/10.3969/j.issn.1003-6350.2012.03.039
Yang Y, Liu H, Xiang XH, Liu FY (2013) Outline of occupational chromium poisoning in China. Bull Environ Contam Toxicol 90:742–749. https://doi.org/10.1007/s00128-013-0998-3
Zheng L, Zhu X, Qin J, Ma N, Luo K (2012) Correlation between sperm quality and trace elements in infertile patients international. J Lab Med 33:659–660. https://doi.org/10.3969/j.issn.1673-4130.2012.06.009
Acknowledgments
The authors thank Heilongjiang Key Laboratory for Laboratory Animals and Comparative Medicine.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 31472161).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Responsible editor: Philippe Garrigues
All authors have read the manuscript and have agreed to submit the manuscript in its current form for consideration for publication in this journal.
Rights and permissions
About this article
Cite this article
Zhang, Y., Li, S. & Li, S. Relationship between cadmium content in semen and male infertility: a meta-analysis. Environ Sci Pollut Res 26, 1947–1953 (2019). https://doi.org/10.1007/s11356-018-3748-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-018-3748-6