Abstract
There is an abundance of epidemiological evidence and animal experiments concerning the correlation between cadmium exposure and adverse male reproductive health outcomes. However, the evidence remains inconclusive. We conducted a literature search from PubMed, Embase, and Web of Science over the past 3 decades. Pooled r and 95% confidence intervals (CIs) were derived from Cd levels of the type of biological materials and different outcome indicators to address the large heterogeneity of existing literature. Cd was negatively correlated with semen parameters (r = − 0.122, 95% CI − 0.151 to − 0.092) and positively correlated with sera sex hormones (r = 0.104, 95% CI 0.060 to 0.147). Among them, Cd in three different biological materials (blood, semen, and urine) was negatively correlated with semen parameters, while among sex hormones, only blood and urine were statistically positively correlated. In subgroup analysis, blood Cd was negatively correlated with semen density, sperm motility, sperm morphology, and sperm count. Semen Cd was negatively correlated with semen concentration. As for serum sex hormones, blood Cd had no statistical significance with three hormones, while semen Cd was negatively correlated with testosterone. In summary, cadmium exposure might be associated with the risk of a decline in sperm quality and abnormal levels of sex hormones.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cadmium (Cd), a toxic heavy metal (HMs), is ubiquitously used in the commercial production of several commonly used electronic products, such as television screens, lasers, and batteries, as well as paint pigments, cosmetics, and galvanizing solutions (Cui et al., 2021). Cd, one of the most dangerous endocrine-disrupting chemicals (EDCs), is widely spread in the environment and has been found to be associated with a wide range of health hazards (Cullen & Maldonado, 2013; Sabir et al., 2019). Cd ranks seventh according to the Agency for Toxic Substances and Disease Registry (ATSDR) (Latif et al., 2020) and is classified as a human carcinogen (Group I) by the International Agency for Research on Cancer (IARC) (Humans, 1993). Industrial and mining enterprises, especially non-ferrous metal enterprises, have been the main contributors to soil Cd pollution (Liu et al., 2016; Wang et al., 2019; Zhang et al., 2015). It has been found that fossil fuel combustion, landfill leachate, and excessive use of phosphorus fertilizer are the main sources of Cd pollution (Genchi et al., 2020; Malin & Wright, 2018; Srivastava et al., 2017). Humans are exposed to Cd through the consumption of Cd-contaminated food, inhalation of cigarette smoke, and industrial processes such as smelting and electroplating (Kumar et al., 2019). About 90% of the Cd exposure was in the diet of those who had not been exposed through smoking or occupation (Vacchi-Suzzi et al., 2016). Cd concentrations in blood and urine were significantly higher in smokers compared to non-smokers (Bochud et al., 2018; Heitland & Koster, 2006), in which the burden of Cd in smokers may be about twice as high as that in nonsmokers (Freire et al., 2015). For occupationally exposed people, higher levels of Cd have been detected that are twice the Occupational Safety and Health Administration class C limit of 10 μg/L (Bulat et al., 2009; Wittman & Hu, 2002).
Due to the rapid population growth, urbanization, industrialization, and the long half-life of Cd about 10–30 years, HMs pollution has caused serious persistent effects on the environment and humans. Urinary excretion of Cd is the most reliable exposure biomarkers using to exposure assessment in most epidemiological studies, while difficult degraded to non-toxic or less toxic substances (Suhani et al., 2021). The cumulative effect of Cd is associated with the dysfunction of multiple organs with aging (Akhtar et al., 2021; La-Up et al., 2021; Xu et al., 2021). Although the liver and kidneys are the accumulate and target organs of Cd gradually, the female reproductive organs (such as ovaries and placenta) and the male reproductive organs (such as testis, epididymis, and seminal vesicle) are also the main target organs (Akinloye et al., 2006; Danielsson et al., 1984; Nordberg, 2009; Ronco et al., 2005; Swiergosz-Kowalewska, 2001; Varga et al., 1993). In addition, epidemiological and animal studies showed Cd accumulation not only damages multiple systems, including immune, respiratory, reproductive, endocrine, cardiovascular, digestive, urinary, nervous systems, causes carcinogenesis (such as breast cancer) in humans (Grioni et al., 2019; Suhani et al., 2021), but also induced atherosclerotic cardiovascular disease (ASCVD), including coronary heart disease and stroke (Fagerberg & Barregard, 2021). Moreover, increased dietary Cd intake was also significantly associated with an increased risk of breast cancer (Grioni et al., 2019). A meta-analysis demonstrated a positive association between Cd exposure and the risk of type 2 diabetes and prediabetes, with dose–response relationships and moderate-quality evidence (Filippini et al., 2022).
Observational studies on the effects of Cd exposure on human male reproductive function focused on semen quality and endocrine function (de Angelis et al., 2017). The deterioration of semen quality is one of the major contributing factors to the infertility in human over the past decades (Carlsen et al., 1992; Murawski et al., 2007; Sokol et al., 2006; Templeton, 1995). Previous studies have described the effects of Cd (4.07–5.92 μg/dL) on semen profile, including total sperm count, sperm concentration, motility, and sperm morphology (Kumar & Sharma, 2019; Ventimiglia et al., 2017). Sera sex hormones are essential for initiating and maintaining human reproductive health. Cd may interfere with hormone levels by affecting hormone synthesis, metabolism, and transport (Knazicka et al., 2015; Lewis & Meeker, 2015) between Cd exposure and serum T (Qiu et al., 2022), whereas negative association or no association were observed in others study (Chen et al., 2016; Menke et al., 2008; Rotter et al., 2016). Cd can also induce various abnormalities of the male reproductive system, such as testicular cancer (TC), prostate cancer, hypospadias, and cryptorchidism, which might related to endocrine disorders (Guillette & Edwards, 2008). In recent decades, incidence of male reproductive disorders gradual increased. These reproductive disorders appeared as cryptorchidism and hypospadias in male neonates, while as spermatogenesis dysfunction and testicular germ cell carcinoma in young adult men (Mitchell et al., 2013). Testicular dysgenesis syndrome(TDS) is thought to be mainly caused by environmental exposure and heredity, with little influence from lifestyle (Xing & Bai, 2018). The development of testicular dysgenesis syndrome (TDS) is associated with potential entities, including cryptorchidism, hypospadias, spermatogenesis disorder, and testicular germ cell carcinoma (Thorup et al., 2010). However, the association between Cd exposure and sperm parameters is controversial, and which positive association (Li et al., 2016) and no association (Jeng et al., 2015; Zagreb et al., 2000) between Cd exposure with decline sperm quality risk were observed at the same time.
After acknowledging the opposite conclusion and high heterogeneity of the previous two meta-analysis on cadmium (Cd) and male fertility (Sun et al., 2017; Zhang et al., 2019), we aimed to comprehensively and systematically appraise the all available epidemiological evidence on the association of environmental and occupational exposure to Cd and risk of male reproductive health including human semen parameters, sera sex hormones levels, and TDS.
Materials and methods
Research design and search strategy
Research questions followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Page et al., 2021) for literature search, research selection, data extraction, and synthesis.
At the same time, we followed the prescribed PECOS statement (Population, Exposure, Comparators, Outcomes, and Study design). The target population was adult males of childbearing age. Exposures were environmental or occupational exposures to Cd and its compounds, and comparators were adult males of reproductive age with low levels of Cd and its compounds exposure. Outcomes we brought into human sperm quality parameters (semen concentration, semen viability, semen morphology, semen volume, etc.), sera sex hormones levels, namely clinical sex hormone five (such as T, E2, luteinizing hormone [LH], follicle-stimulating hormone [FSH], and progesterone), TDS (including TC, cryptorchidism, hypospadias, subfertility, and testicular germ cell cancer) three categories. That was, “For adult males of reproductive age (P), was higher Cd and its compounds exposure (E) associated with increased risk to male reproductive health (O) compared with lower levels of Cd and its compounds exposure (C)?”(Supplementary Material 1).
Eligibility and exclusion criteria
See Supplementary Materials 2 for details. In summary, the included studies were in English for cohort, case–control, or cross-sectional studies that provided Cd and outcome variables, including OR, RR, HR, 95% confidence intervals (95% CIs), and correlation coefficients.
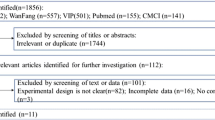
Selection of relevant articles
First, duplicate articles were excluded using EndNote X9. The titles and abstracts of the remaining articles were next carefully reviewed to exclude some irrelevant articles. The full text of the retrieved articles was then carefully reviewed by two independent reviewers (Guangying Li and Jiajia Xia) for eligibility testing. Finally, selected articles were carefully evaluated to extract predetermined information and data. In case of any disagreement between the two examiners, a third independent examiner (Xin Gao) assisted before making a final decision.
Data extraction
One author (Xiang Ruan) independently performed data extraction according to a predesigned table, and any disagreements between them were resolved by discussion with a third author. If possible, the authors of the study were asked for missing data. Data extracted from the study included the following: first author and year, study design, location, time period, sample size, age (year), biomaterials, method of measurement, outcome definition, main finding. Data from all studies that met the inclusion criteria were extracted and tabulated.
Assessment of risk of bias
We assessed the methodological quality of the included articles using the Newcastle–Ottawa Scale (NOS) (Stang, 2010; Tang et al., 2020), including case–control and cohort studies (9 points) and cross-sectional studies (10 points). The original version was used to assess case–control and cohort studies, and the adapted version was used to assess cross-sectional studies. Through different items, three dimensions were assessed: selection of case–control studies, comparability, and exposure; selection, comparability, and outcomes of cohort and cross-sectional studies. Specific items, divided into three more general quality parameters (selection, comparability, and outcome). Typically, a maximum of one point is scored for each individual item, but a maximum of two points is scored for comparability. NOS scores of 0–3 were considered as low quality, 4–6 as moderate quality, and 7–9 as high quality studies (Xing et al., 2016). According to the NOS scoring criteria, cross-sectional studies can be classified as low quality (0–4 points), moderate quality (5–6 points), and high quality (score ≥ 7 points). In the case of a sufficient number of included literature, we will delete the literature with low quality for further analysis. Overlap risk (inclusion of the same patient in different papers) was assessed by means of manual searches. This step was carried out by two authors (Di Yan and Guangying Li).
Data measurement
The meta-analysis was made with r (Pearson correlation coefficient) and its 95% CI (confidence interval), but the articles we extracted in the article had only r. Based on the following formula (a–d), we could be able to get the 95% CI of r. The transformation of the data and the basic data extracted from the previous extraction were included in the meta-analysis.
-
a.
the correlation coefficient r is converted to Fisher’s Z: Z = 0.5 × ln((1 + r)/(1 − r)), equivalent to r = (e2z − 1)/(e2z + 1) (Fisher, 1932)
-
b.
Calculate the variance (V) of Z: V(Z) = 1/(n − 3)
-
c.
Calculate the standard error (SE) of z: SE(Z) = V(Z)^0.5
-
d.
Calculate the 95% CI of Z: (Upper CI of Z = Z + SE(Z) × 1.96, Lower CI of Z = Z − SE(Z) × 1.96) (Nissensohn et al., 2016)
Data analysis
Heterogeneity statistics (I2) were used to test the consistency of the cumulative evidence across studies. I2(%) was calculated as 100%* (Q − df)/Q and used to determine the degree of heterogeneity and consistency of the studies. If I2 is less than 25%, heterogeneity is low, between 25 and 50% is moderately heterogeneous, and higher than 50% heterogeneity is high. In the Cochrane systematic review, the heterogeneity was acceptable as long as I2 was not greater than 50%. For those with high heterogeneity, that is, I2 > 50%, we will adopt the random effect model; otherwise, we will use the fixed effect model for analysis.
To assess publication bias, funnel plots and the Egger’s test (Egger et al., 1997) were performed for all primary outcomes. If the funnel plot forms a symmetric "funnel" shape, there is no bias. Publication bias exists if many points fall outside the pseudo-95% CI and the funnel is clearly asymmetric. Egger’s test is used to detect asymmetry in the funnel plot, with P < 0.05 in the Egger’s test indicating publication bias.
Besides, the one-by-one elimination method, which is also the most commonly used method, was used to analyze the sensitivity of each article. The effect sizes were pooled after deleting each single included article, and the newly obtained effect was compared with the effect before deletion. If there were no significant differences before and after exclusion studies, the sensitivity of the study was considered low and the results stable. In contrast, significant differences in post-exclusion effects indicate higher sensitivity of exclusion studies. Sensitivity analysis can identify studies with abnormal effect sizes.
Subgroup analyses were also performed to explore sources of heterogeneity. Each individual study was divided into different groups, and then pooled analysis was performed to compare the significant difference between each group and the total pooled effect.
Meta-analysis was performed by Stata software (version 11.0), and P < 0.05 (α = 0.05) was considered statistically "significant".
Results
Study selection and included studies
Finally, 15 articles (3 additional articles by reviewing the references of the included articles) were included in the quantitative analysis (Fig. 1). Among them, 27 articles still could not find the full text after sending an email to the author without a response, so these articles were not included in this study. We summarized the characteristics of included literature (Table 1 and Supplementary Materials 3).
Risk of bias
According to the NOS checklist, all scores were between 5 and 7, and one case–control study was considered as moderate quality and the other as high quality. So did two cohort studies. In the cross-sectional study, 5 studies were considered as moderate quality and 6 studies were considered as high quality. Overall, these articles had a low risk of bias (Fig. 2).
Overall analysis of semen parameters
Semen parameters in 13 articles were pooled and analyzed and divided into three subgroups based on biological material (Supplementary Material 4). The overall results showed that there was a negative correlation between Cd exposure and semen parameters (r = − 0.122, 95% CI − 0.151 to − 0.092, P < 0.05) (all P values of data analysis could be found in Table S1). And the results of three subgroups showed that blood Cd (BCd), semen Cd, and urine Cd (UCd) were negatively correlated with semen parameters. The values of r and 95% CI were r = − 0.176, 95% CI − 0.219 to − 0.132, r = − 0.062, 95% CI − 0.112 to − 0.011, r = − 0.087, 95% CI − 0.160 to − 0.015, respectively (Fig. 3). The forest plots showed high heterogeneity and then we carried out sensitivity analysis, which showed that the results were robust (Table S2). Asymmetrical funnel plot suggested that there might be publication bias (Fig S1). Subsequently, we took BCd, semen Cd, and UCd as variables to carry out Egger's test. From three subgroups, only the BCd group had publication bias (Table S3).
Overall analysis of sera sex hormones
Sex hormones in 6 articles were pooled and analyzed and divided into three subgroups based on biological material (Supplementary Material 5). The forest plot showed that Cd was positively correlated with sex hormones (r = 0.104, 95% CI 0.060 to 0.147, P < 0.05) (all P values of data analysis could be found in Table S4). In the three subgroups, there was no statistical significance between semen Cd and sex hormones, while BCd and UCd were positively correlated with sex hormone. The values of r and 95% CI were r = 0.132, 95% CI 0.084 to 0.180, r = 0.405, 95% CI 0.189 to 0.620, respectively (Fig. 4) There was also high heterogeneity in sex hormones. Sensitivity analysis showed robust results. Asymmetric funnel plot suggested possible publication bias (Fig. S2). Egger's test verified its existence (Table S5). But in Egger's test with BCd, semen Cd, and UCd as three variables, there was no publication bias in semen Cd (Table S6).
BCd concentration and semen parameters
Immediately, we made a meta-analysis of BCd and semen parameters by taking semen parameters as subgroups from 8 articles (Supplementary Material 6). By analysis, we found that the concentration of BCd was negatively correlated with semen parameters (r = − 0.182, 95% CI − 0.230 to − 0.135, P < 0.05) (all P values of data analysis could be found in Table S7). In various subgroup analysis, semen density (r = − 0.137, 95% CI − 0.190 to − 0.084, P < 0.05), sperm motility (r = − 0.220, 95% CI − 0.315 to − 0.125, P < 0.05), sperm morphology (r = − 0.315, 95% CI − 0.462 to − 0.167, P < 0.05), and sperm count (r = − 0.238, 95% CI − 0.397 to − 0.079, P < 0.05) four subgroups were statistically significant with BCd (Fig. 5a). There was also a high degree of heterogeneity in the forest plot. Right after, results of sensitivity showed that the results were robust (Table S8). Funnel plots suggested that there might be publication bias (Fig. S3). Egger's test found there was publication bias, with a value of less than 0.05 (Table S9). The four groups of sensitivity analysis results showed that the results are robust. However, different from the total value, Egger's test of these four subgroups showed no publication bias, with P values of 0.093, 0.115, 0.172, and 0.060, respectively. Generally, the heterogeneity of this group of data was very high, but due to insufficient data, it was impossible to analyze the source of heterogeneity.
Forest plots for subgroup analysis. a Forest plot of the correlation between blood cadmium concentration and semen parameters with semen density, sperm motility, sperm morphology, semen volume, sperm count as subgroups. b Forest plot of the correlation between semen cadmium concentration and semen parameters with semen density, sperm motility, sperm morphology, semen volume, semen concentration, sperm count as subgroups. c Forest plot of the correlation between blood cadmium concentration and sera sex hormones with testosterone, luteinizing hormone (LH), follicle-stimulating hormone as subgroup. d Forest plot of the correlation between semen cadmium concentration and sera sex hormones with testosterone, luteinizing hormone (LH), follicle-stimulating hormone as subgroup
Semen Cd concentration and semen parameters
Next, we analyzed the relationship between semen Cd and semen parameters from 10 articles (Supplementary Material 7). Forest plot showing the concentration of semen Cd was negatively correlated with semen parameters (r = − 0.062, 95% CI − 0.112 to − 0.011, P < 0.05) (all P values of data analysis could be found in Table S10). In subgroup analysis, only the semen concentration group had a statistically negative correlation (r = − 0.186, 95% CI − 0.231 to − 0.140, P < 0.05). The forest plot also showed high heterogeneity but in the subgroup of seminal Cd and semen concentration, the heterogeneity was 0% (Fig. 5b). In the sensitivity analysis, the results show robustness (Table S11). The asymmetric distribution of the funnel plot suggested possible bias (Fig. S4), and Egger's test showed that there was no publication bias (Table S12). At the same time, we also quantified the publication bias between semen Cd and semen concentration, and the results showed that without publication bias, P was 0.459.
BCd concentration and sera sex hormones
From 5 articles, we analyzed the relationship between BCd and sex hormone levels (Supplementary Material 8). Forest map demonstrated BCd was positively correlated with sera sex hormones (r = 0.132, 95% CI 0.084 to 0.180, P < 0.05). However, subgroup analyses of the three hormones showed no statistical significance (all P values of data analysis could be found in Table S13) (Fig. 5c). Sensitivity analysis showed that the results were stable (Table S14), and the asymmetric forest plot suggested that there might be bias (Fig. S5), which Egger's test also confirmed, that is, P was 0.001 (Table S15). High heterogeneity also occurred in this group, and we were also unable to analyze the source of heterogeneity.
Semen Cd concentration and sera sex hormones
From 3 articles, we analyzed the relationship between semen Cd and sex hormone levels (Supplementary Material 9). However, the overall results were not statistically significant, and only T was negatively associated with seminal Cd in the subgroup (r = − 0.109, 95% CI − 0.157 to − 0.061, P < 0.05) (all P values of data analysis could be found in Table S16). Moreover, the heterogeneity was 0% in the T and seminal Cd subgroup (Fig. 5d). Sensitivity results showed moderate robustness (Table S17). However, sensitivity analysis of statistically significant subgroups showed robust results. Funnel showed that there might be publication bias (Fig. S6). Egger's test showed that there was no publication bias, i.e., P = 0.146 (Table S18). Similarly, quantification of publication bias in the seminal Cd and T subgroups revealed no publication bias, i.e., P = 0.249.
Cd and spermatogenesis
Cd was testicular toxicant to male animals and humans, which could cause great changes in testicular morphology and histopathology, such as abnormality of Leydig cells, atrophy of seminiferous tubules, fibrosis, and decrease in testicular size (Babaknejad et al., 2018; Siu et al., 2009), Cd decreased sperm motility in a dose-dependent manner (Wang et al., 2020).
Cd could affect spermatogenesis by affecting molecular biology (signaling pathway interference), epigenetic regulation, and cell structure (cell junction and cytoplasmic bridge), thus leading to low fertility/infertility in men. Oxidative stress was caused by various reactive substances indirectly produced by Cd including hydroxyl radical, nitric oxide radical, and superoxide radical (Galán et al., 2001; Winiarska-Mieczan, 2018) It had been found in many studies that Cd affected spermatogenesis and steroid production through oxidative stress (Acharya et al., 2008; Al-Azemi et al., 2010; Arab et al., 2021; Benvenga et al., 2019; Bu et al., 2011; Koriem et al., 2013; Mahmoudi et al., 2018; Pires et al., 2013; Venditti et al., 2021). Studies had shown, for example, that Cd caused oxidative stress in testis through Nrf2-keap1 signal, which weakened spermatogenesis and steroid production (He et al., 2018; Shi & Fu, 2019). In addition, Rictor/mTORC2 signaling could also affect spermatogenesis (Dong et al., 2015). Akt signaling pathway participated in many crucial cellular functions and was proved that Cd caused infertility by affecting Akt and its downstream proteins NF-κB (p50) and COX-2 (Mitra et al., 2022). EGFR stimulated the activity of PI3K/AKT signaling pathway, which was frequently dysregulated in female and male genital tract cancers (Song et al., 2014; Zhong et al., 2000). Cd had also been proved to upregulate p-EGFR and its downstream signal proteins including p-AKT, AKT1/2/3, NF-κβ(p50) and COX-2 (Mitra et al., 2016). Cd had been proved to interact with PI3K/Akt cascade through ROS and non-ROS-mediated pathways (Fresno Vara et al., 2004; Matsuoka & Igisu, 2001). Exposure to Cd would affect the global DNA methylation of mice, reduced the DNA methylation level of LINE-1 in testis, and increased the number of abnormal sperm (Wang et al., 2020). Cd could cause abnormal expression of lncRNAs and mRNA in testis and sperm. Gene ontology and pathway analyses pointed out that the functions of lncRNAs and mRNA were closely related to many processes of spermatogenesis, including the cytoskeleton of intermediate filament and intermediate filament, the metabolism of mRNA and macromolecules, etc (Gao et al., 2017). DAAM 1,which was Dishevelled-associated activator of morphogenesis, had been proven that Cd could inhibit the expression of DAAM 1 in testis and caused changes in sperm quality (Chemek et al., 2018). In the process of spermatogenesis, the demand for cysteine was increasing, which was used for replacing histone with protamine (Conrad et al., 2015). The mRNA expression of cystine/glutamate transporter SLC7A11 was inhibited in Cd-exposed mice, while cysteine/glutathione homeostasis was necessary for Sertoli cells, not glutamate homeostasis (Liu et al., 2022). Serine protease PREP could also be affected by Cd, thus changing the cytoskeleton (Venditti et al., 2020). The other study had found that Cd affected the apical ectoplasmic specialization dynamics during spermatogenesis by affecting intercellular adhesion molecule 2 (ICAM2) and losing ICAM 2-actin interaction might promote the connection reconstruction (Xiao et al., 2013). As a linker, Nectin-2 was found to inhibit its transcription by Cd, leading to male infertility (Zhang & Lui, 2014). Moreover, overexpression of LG3/4/5 in testis could block or rescue Cd-induced BTB destruction and testicular damage, which corrected the spatiotemporal expression of actin and microtubule-based regulatory proteins by maintaining the cytoskeleton in testis (Li et al., 2020). Research had found that Cd could destroy the cell barrier function through p2/MMP4 pathway in TM4 cells as well as p38 signal and ISR regulated by HRI reactive mitochondrial stress (Zhou et al., 2022a, 2022b). Of course, the changes caused by different doses of Cd might also have different responses to different doses. For example, it had been found that in the low and medium concentration group (fed with 2 or 4 mg/kg BW Cd), the increased levels of LHR, 17α- hydroxylase and eNOS might inhibit Cd-induced testicular cell apoptosis, and the decreased expression level of all factors in the high dose group (fed with 8 mg/kg BW Cd) might be the result of increased testicular cell apoptosis (Ren et al., 2019) (Fig. 6). As the testis was strongly sensitive to Cd, it was reflected in the decrease of sperm quantity and quality, which was achieved through a variety of tanglesome pathways to affect the development and meiosis of spermatogenic epithelial cells and so on.
Cd affects spermatogenesis through several pathways. The dashed line is considered a possible pathway. Akt protein kinase B, BTB blood-testis barrier, COX-2 cyclooxygenase-2, DAAM 1 Dishevelled-associated activator of morphogenesis, EGFR epidermal growth factor receptor, eIF2bα eukaryotic translation initiation factor 2, eNOS endothelial nitric oxide synthase, HRI Heme-regulated inhibitor, ICAM2 intercellular adhesion molecule 2, ISR integrated stress response, keap1 Kelch-like ECH-associated protein 1, LG3/4/5 laminin-type globular domains of LG3, 4 and 5, LHR luteinizing hormone receptor, LINE-1 long interspersed nuclear elements-1, lncRNA long non-coding ribonucleic acid, MMP4 matrix metalloproteinase 4, mTORC2 the mammalian target of rapamycin complex 2, NF-κB (p50) nuclear factor-κB, Nrf-2 Nuclear factor erythroid-2-related factor 2, PI3K phosphatidylinositol 3-kinase, PREP prolyl oligopeptidase, Rac1 ras-related C3 botulinum toxin substrate 1, Rictor rapamycin-insensitive companion of mTOR, ROS reactive oxygen species, SLC7A11 cystine/glutamate antiporter solute carrier family 7 member 11
Cd and steroidogenesis
The regulation of spermatogenesis was also carried out by steroids, such as T and E2 (Walker, 2011; Zhang et al., 2010). An in vitro study on Leydig cell culture in rats showed CdCl2 had an adverse effect on cell viability in a dose-dependent and time-dependent manner (Clough et al., 1990). 3β-HSD, cyp11a1, and tex15 played central roles in steroid and spermatogenesis, and the study in vitro found that Cd caused their relative expression downregulation in TM3 cells. Located in the outer membrane of mitochondria, VDAC2 was involved in many ion-dependent processes, such as hormone release and anti-apoptosis pathway, and was related to sperm capacitation and acrosome reaction (Martínez-Abad et al., 2017). Cd activated JNK/p53 signaling pathway, which occurred through downregulation of VDAC2, resulting in downregulation of StAR and decrease of T content, which eventually led to sperm abnormality (Fang et al., 2020). The downregulation of StAR, p450scc and 17β-HSD by Cd had been demonstrated in multiple studies (Abarikwu et al., 2019; Fang et al., 2020; Habib et al., 2019; Ren et al., 2012; Shi & Fu, 2019), including adolescent Cd exposure, thereby leading to the decrease of Leydig cells and T (Ji et al., 2010). During pregnancy, maternal exposure to Cd could downregulate the expression of StAR proteins P450scc and 17β-HSD in male fetal testis (Ji et al., 2011). As an essential limiting factor in T synthesis in testis, StAR was responsible for transporting cholesterol to mitochondria (Miller, 2007). P450scc and 17β-HSD were T synthetases in Leydig cells of testis. A possible relationship existed between cytoskeleton and steroid production. Cd exposure led to the upregulation of CORO1A and Cofilin 1, while the downregulation of p-Cfl 1 and Pfn 1, followed by the destruction of actin polymerization and the decrease of filamentary actin (Wang et al., 2022). Ferroptosis was a newly defined programmed cell death pathway, characterized by iron overload and lipid peroxidation (Dixon et al., 2012; Hassannia et al., 2019). Cd could affect iron homeostasis and lead to ferroptosis, and ultimately reduced the production of T, and the study had revealed that Cd-induced ferroptosis depends on the over-activation of HMOX1 and the release of free iron by heme (Zeng et al., 2021). New research found that father's Cd exposure would reduce the testicular cholesterol pool of offspring mice and affected T synthesis (Zhou et al., 2022a, 2022b). Cholesterol was the direct precursor of T (Hall et al., 1969). Huang et al., (2020) had previously found that exposure to Cd during pregnancy reduced the serum T level of offspring by affecting SF-1 signaling pathway (Fig. 7). Hormonal abnormalities were also one of the outcome variables we collected, and a large number of animal experiments had also proved that Cd did inhibit hormonal generation through a variety of pathways, even paternal Cd exposure, by reducing the number of Leydig cells and the steroidogenic activity in a sophisticated of ways, which in itself further affected sperm parameters.
Steroidogenesis affects spermatogenesis. 3β-HSD 3β-hydroxysteroid dehydrogenase, 17β-HSD 17β-hydroxysteroid dehydrogenase, Cfl-1 Cofilin 1, CORO1A Coronin-1A, cyp11a1 cytochrome P450 side-chain cleavage, HMOX1 heme oxygenase 1, JNK Jun N-terminal kinase, p450scc cytochrome P450 cholesterol side-chain cleavage, Pfn 1 Profilin 1, SF-1 steroid-producing factor 1, StAR steroidogenic acute regulatory, tex15 testis expressed gene 15, VDAC2 voltage dependent anion channel 2
Discussion
This is the first meta-analysis to examine the association of Cd and its compounds exposure with semen quality, sera sex hormones, and TDS based on epidemiological evidence. Some interesting results have been obtained in this study. Firstly, Cd was negatively correlated with semen parameters but positively correlated with sex hormones in the overall analysis. Among them, Cd in three different biological materials (blood, semen and urine) was negatively correlated with semen parameters, while among sex hormones, while only blood and urine were statistically positively correlated with them. In subgroup analysis, BCd concentration was negatively correlated with semen density, sperm motility, sperm morphology and sperm count. The concentration of Cd in semen was negatively correlated with that of semen concentration. In terms of serum sex hormones, the BCd concentration had no statistical significance with the three hormones, while semen Cd concentration was negatively correlated with serum T. Nelson and Bunge first raised the topic of declining global male fertility in 1974 and sparked controversy (Nelson & Bunge, 1974). Over the past 5 decades, male infertility has become a public health issue, due to growing literatures reporting a significant trend of global decline in human male fertility. Environmental exposure and occupational exposure to toxic pollutants have been shown to negatively affect human male fertility (Jenardhanan et al., 2016; Knez, 2013). At present, there are two meta-analyses on Cd and male reproductive health (Sun et al., 2017; Zhang et al., 2019), the results of meta-analysis of 20 case–control studies in 2017 (Sun et al., 2017) showed that the semen concentrations of lead and Cd in normal men were significantly higher than those in low fertility group, while the results of meta-analysis of 11 randomized controlled trials in 2019 (Zhang et al., 2019) showed that high Cd content in semen is one of the pathogenic factors of infertility. In a 2022 study of the effect of metals on semen parameters of domestic ruminants, the result showed that Cd would affect sperm viability and motility (Ribeiro et al., 2022). Therefore, based on the latest evidence, we summarized the relevant literature in the last 3 decades to further explore the relationship between Cd exposure and male reproductive health. In addition, the semen parameters, sera sex hormones levels, as well as TDS were considered as outcome variables, which are directly related to decreased male fertility. Clinical male fertility potential was analyzed by semen analysis. Pregnancy rates increase with sperm morphology and motility (Garrett et al., 2003). Sperm chromatin and DNA damage can provide information on sperm quality and may be a prerequisite for normal sperm function (Venkatesh et al., 2011). Endocrine disorders play a decisive role in the etiology of male infertility (Concepcion-Zavaleta et al., 2022). Spermatogenesis is a complex process involving genetic, hormonal and environmental factors, which dysfunction can induced poorer sperm quality leading to infertility (Pathak et al., 2020). Although a specific endocrine cause of altered sperm production has been identified in only 2% of infertile men, men with clinically abnormal semen analysis still require endocrine evaluation (Practice Committee of the American Society for Reproductive, 2015; Sigman & Jarow, 1997). Fertility likelihood varies according to the type of TDS. Subfertility is common in TC. At presentation, oligospermia was present in 45% of cases and azoospermia in 6–24% (Williams et al., 2009). Men with a history of cryptorchidism are at increased risk of infertility (Thorup et al., 2010). Men diagnosed with TC often have abnormal semen parameters at baseline (Dohle, 2010).
Regarding metals and metalloid species, blood, urine, and hair are the most widely accepted biological substrates to measure their cumulative body burden (Gil & Hernandez, 2015). Metal levels in blood are suggestive of short-term exposure. In contrast, urinary levels of HMs may suggest long-term exposure to HMs (Deng et al., 2019). Urinary Cd appears to be an ideal biomarker for the physical burden of Cd. In contrast to BCd, UCd can reflect cumulative exposures, including exposures that occurred several years ago (Zeng et al., 2004). The long-term exposure and accumulation of Cd are the direction of public concern, unfortunately, the current data on Cd exposure in urine do not support a meta-analysis of its association with semen quality and sera sex hormones levels. Saaranen et al., (1989) suggested that Cd in seminal plasma may be increased by high local nutritional and industrial exposure, which has a direct impact on testicular function and hormonal changes. Meeker et al., (2010) suggested that although the number was rather limited, there was some consistency in the positive association between Cd exposure and circulating T based on all human studies, which is consistent with our study. Leydig cells are the main source of T in men (Chen et al., 2009), and the testicles are very sensitive to Cd toxicity. Cd in semen may have a more immediate and direct effect on hormones.
There are several risk factors that can influence sperm parameters, such as age, genetic background, environmental, occupational and lifestyle factors (Bonde, 2013; Jurewicz et al., 2014; Knez, 2013; Sharma et al., 2013). In addition, a study pointed out that the decrease of spermatogenesis function may be an early sign of toxic effects of Cd pollution (Caprio et al., 2015). The regulation of hormones begins in the perinatal period, and it plays a key role in spermatogenesis and sperm maturation. In adult men, gonadal T acts on the male neural circuit to stimulate behavior. Compared with the permanent tissue changes induced by development and puberty, this activation of T is short-lived (Mhaouty-Kodja et al., 2018). Regarding sera sex hormones, we included the five clinical male sera sex hormones without considering SHBG. The effects of Cd on sera sex hormones levels are controversial, with results showing that changes in sera sex hormones levels are only associated with UCd but not BCd (Zeng et al., 2004). Others have concluded that Cd is only associated with SHBG, but not with T or E2 or free levels of these hormones (Kresovich et al., 2015). Then our study showed that BCd was positively correlated with FSH levels, and semen Cd concentration was negatively correlated with T, which is an interesting finding. One population-based study (Zhao et al., 2020) found that elevated LH levels were associated with poor sperm motility and morphology, and the use of LH for risk stratification and tail prevention in men may become a new focus of research. Data on TDS are insufficient for meta-analysis. Over the past decades, the incidence of TC is growing probably due to the increasing exposure to its risk factors and improving detection of the disease. The trend of a significant increase in incidence was seen mainly in European countries. Shockingly, however, the most significant increasing trends were found in Asian countries such as Kuwait, Japan, and Thailand. This increasing trend is also more prominent among the younger population (Huang et al., 2022). Although overall mortality rates have decreased globally, there have been significant increases in Thailand and Colombia (Huang et al., 2022). The presence of cancer itself may affect the levels of reproductive hormones. For example, prostate cancer is commonly associated with low T concentrations, while its association with decreased serum LH and increased FSH has also been suggested (Mearini et al., 2008). In addition to direct toxicity, reduced sperm quality may be the result of altered testicular or reproductive tract function. There is growing evidence that pollutants act as endocrine disruptors, leading to genital disorders (impaired spermatogenesis and reproductive defects) and disorders driven by antiandrogens (TDS) (Acerini et al., 2009; Skakkebaek et al., 2001) TDS, sera sex hormones, and semen quality seem to be closely linked, but the exact role of Cd is unknown.
Like other meta-analyses, there are some limitations in this study. First, this study only included English articles, and the analysis of non-Western countries was lacking. Second, this study included data from the last 3 decades, during which there have been changes in semen assessment reference ranges and laboratory methods. In 2010, the WHO issued the first semen criteria for population-based study of fertile men (Cooper et al., 2010). Subsequently, the WHO published the latest Laboratory Manual for the Examination of Human semen, 5th edition, which also includes significant changes in the methods used to perform such analyses compared with the previous version (Special Programme of Research Development and Research Training in Human Reproduction (World Health Organization), 1992; World Health Organization., 1999, 2010). Third, except for semen Cd and T, there was great heterogeneity in our study, which could not be further analyzed due to insufficient data, which may be due to different study populations, different research protocols, different time and place, and different research methods. We suspected that in each hormone subgroup, the results were not statistically significant due to the small number of studies and the large number of cross-sectional studies.
The potential mechanism of Cd detrimental impacts on semen quality remains unclear. The exact contribution of Cd toxicity to reproductive function is difficult to determine due to differences in Cd sensitivity, tissue concentration, and duration of exposure (Wu et al., 2008). Few experimental clinical studies of contaminants on sperm have been conducted in humans, and conducting clinical studies in humans is challenging, mainly due to the dose and duration of exposure and the assessment of other variables, including alcohol use, overweight, obesity, social pressure, and other diseases (Pizzol et al., 2021). Therefore, more high-quality research is needed to address this issue and provide much needed knowledge for the occupational and environmental fields. It has been found that metals (lead and Cd) do not directly affect T or E2 synthesis because no association was detected between lead or Cd and androsterone-glucuronide (the precursor of T) or E2 (synthesized from T by aromatase) (Kresovich et al., 2015). However, a study in mice has found that Cd treatment disrupts iron homeostasis, ultimately leading to an increase in iron and a decrease in T (Zeng et al., 2021). And a recent study showed that paternal Cd exposure affected T production by reducing the testicular cholesterol pool in offspring mice (Zhou et al., 2022a, 2022b). In the past decade, omics technology has made some progress in various research fields, and further development of omics based biomarkers may help explore the knowledge of potential health effects of Cd on humans (Ventura et al., 2021). There is also a need for new biomarkers to reflect new Cd exposure scenarios. As mentioned earlier, the relationship between TDS and sera sex hormones with semen quality seems to remain a mystery.
Conclusions
According to our systematic review and meta-analysis, the concentration of cadmium in blood and semen affects male reproductive health to some extent, which is reflected in semen quality and sex hormone levels. A better understanding of cadmium exposure is essential for studying men's health, which requires further research based on more precise exposure assessments. Prospective cohort studies are also urgently needed to better explore gaps in the causal relationship between cadmium exposure and semen quality, serum sex hormone levels, and TDS. In addition, different concentrations of cadmium in human semen and blood may help to speculate about some correlation with environmental pollution and dietary intake, which should be further investigated. The presence of other factors that may have a strong impact on men's reproductive health and thus indirectly lead to an increase or decrease in cadmium concentrations is also an issue worth studying.
Availability of data and materials
Data are available from corresponding authors upon a reasonable request.
Abbreviations
- BCd:
-
Blood cadmium
- Cd:
-
Cadmium
- CI:
-
Confidence intervals
- E2 :
-
Estradiol
- FSH:
-
Follicle-stimulating hormone
- HMs:
-
Heavy metal
- LH:
-
Luteinizing hormone
- NOS:
-
Newcastle–Ottawa Scale
- SHBG:
-
Sex hormone-binding globulin
- T:
-
Testosterone
- TC:
-
Testicular cancer
- TDS:
-
Testicular dysgenesis syndrome
- UCd:
-
Urine cadmium
- WHO:
-
World Health Organization
References
Abarikwu, S. O., Wokoma, A. F. S., Mgbudom-Okah, C. J., Omeodu, S. I., & Ohanador, R. (2019). Effect of Fe and Cd Co-exposure on testicular steroid metabolism, morphometry, and spermatogenesis in mice. Biological Trace Element Research, 190(1), 109–123. https://doi.org/10.1007/s12011-018-1536-2
Acerini, C. L., Miles, H. L., Dunger, D. B., Ong, K. K., & Hughes, I. A. (2009). The descriptive epidemiology of congenital and acquired cryptorchidism in a UK infant cohort. Archives of Disease in Childhood, 94(11), 868–872. https://doi.org/10.1136/adc.2008.150219
Acharya, U. R., Mishra, M., Patro, J., & Panda, M. K. (2008). Effect of vitamins C and E on spermatogenesis in mice exposed to cadmium. Reproductive Toxicology, 25(1), 84–88. https://doi.org/10.1016/j.reprotox.2007.10.004
Akhtar, E., Roy, A. K., Haq, M. A., von Ehrenstein, O. S., Ahmed, S., Vahter, M., & Raqib, R. (2021). A longitudinal study of rural Bangladeshi children with long-term arsenic and cadmium exposures and biomarkers of cardiometabolic diseases. Environmental Pollution, 271, 116. https://doi.org/10.1016/j.envpol.2020.116333
Akinloye, O., Arowojolu, A. O., Shittu, O. B., & Anetor, J. I. (2006). Cadmium toxicity: a possible cause of male infertility in Nigeria. Reproductive Biology, 6(1), 17–30.
Al-Azemi, M., Omu, F. E., Kehinde, E. O., Anim, J. T., Oriowo, M. A., & Omu, A. E. (2010). Lithium protects against toxic effects of cadmium in the rat testes. Journal of Assisted Reproduction and Genetics, 27(8), 469–476. https://doi.org/10.1007/s10815-010-9426-3
Arab, H. H., Gad, A. M., Reda, E., Yahia, R., & Eid, A. H. (2021). Activation of autophagy by sitagliptin attenuates cadmium-induced testicular impairment in rats: Targeting AMPK/mTOR and Nrf2/HO-1 pathways. Life Sciences, 269, 119. https://doi.org/10.1016/j.lfs.2021.119031
Babaknejad, N., Bahrami, S., Moshtaghie, A. A., Nayeri, H., Rajabi, P., & Iranpour, F. G. (2018). Cadmium testicular toxicity in male Wistar rats: Protective roles of zinc and magnesium. Biological Trace Element Research, 185(1), 106–115. https://doi.org/10.1007/s12011-017-1218-5
Benoff, S., Hauser, R., Marmar, J. L., Hurley, I. R., Napolitano, B., & Centola, G. M. (2009). Cadmium concentrations in blood and seminal plasma: Correlations with sperm number and motility in three male populations (infertility patients, artificial insemination donors, and unselected volunteers). Molecular Medicine, 15(7–8), 248–262. https://doi.org/10.2119/molmed.2008.00104
Benvenga, S., Micali, A., Pallio, G., Vita, R., Malta, C., Puzzolo, D., Irrera, N., Squadrito, F., Altavilla, D., & Minutoli, L. (2019). Effects of Myo-inositol alone and in combination with Seleno-L-methionine on cadmium-induced testicular damage in mice. Current Molecular Pharmacology, 12(4), 311–323. https://doi.org/10.2174/1874467212666190620143303
Bochud, M., Jenny-Burri, J., Pruijm, M., Ponte, B., Guessous, I., Ehret, G., Petrovic, D., Dudler, V., Haldimann, M., Escher, G., & Dick, B. (2018). Urinary cadmium excretion is associated with increased synthesis of cortico- and sex steroids in a population study. The Journal of Clinical Endocrinology & Metabolism, 103(2), 748–758. https://doi.org/10.1210/jc.2017-01540
Bonde, J. P. (2013). Occupational causes of male infertility. Current Opinion in Endocrinology, Diabetes, and Obesity, 20(3), 234–239. https://doi.org/10.1097/MED.0b013e32835f3d4b
Bu, T., Mi, Y., Zeng, W., & Zhang, C. (2011). Protective effect of quercetin on cadmium-induced oxidative toxicity on germ cells in male mice. Anatomical Record (hoboken), 294(3), 520–526. https://doi.org/10.1002/ar.21317
Bulat, Z. P., Dukic-Cosic, D., Dokic, M., Bulat, P., & Matovic, V. (2009). Blood and urine cadmium and bioelements profile in nickel-cadmium battery workers in Serbia. Toxicology and Industrial Health, 25(2), 129–135. https://doi.org/10.1177/0748233709104488
Caprio, F., Campitiello, M. R., Mele, D., Trotta, C., Mainini, G., Vagnetti, P., & Franciscis, P. D. (2015). Environmental pollution due to cadmium: Measure of semen quality as a marker of exposure and correlation with reproductive potential. Clinical and Experimental Obstetrics & Gynecology, 42(6), 767–770. https://doi.org/10.12891/ceog3029.2015
Carlsen, E., Giwercman, A., Keiding, N., & Skakkebaek, N. E. (1992). Evidence for decreasing quality of semen during past 50 years. BMJ, 305(6854), 609–613. https://doi.org/10.1136/bmj.305.6854.609
Chemek, M., Venditti, M., Boughamoura, S., Mimouna, S. B., Messaoudi, I., & Minucci, S. (2018). Involvement of testicular DAAM1 expression in zinc protection against cadmium-induced male rat reproductive toxicity. Journal of Cellular Physiology, 233(1), 630–640. https://doi.org/10.1002/jcp.25923
Chen, C., Wang, N., Nie, X., Han, B., Li, Q., Chen, Y., Zhai, H., Zhu, C., Chen, Y., Xia, F., & Lu, M. (2016). Blood cadmium level associates with lower testosterone and sex hormone-binding globulin in Chinese men: From SPECT-China study, 2014. Biological Trace Element Research, 171(1), 71–78. https://doi.org/10.1007/s12011-015-0526-x
Chen, H., Ge, R. S., & Zirkin, B. R. (2009). Leydig cells: From stem cells to aging. Molecular and Cellular Endocrinology, 306(1–2), 9–16. https://doi.org/10.1016/j.mce.2009.01.023
Chia, S. E., Xu, B., Ong, C. N., Tsakok, F. M., & Lee, S. T. (1994). Effect of cadmium and cigarette smoking on human semen quality. International Journal of Fertility and Menopausal Studies, 39(5), 292–298.
Clough, S. R., Welsh, M. J., Payne, A. H., Brown, C. D., & Brabec, M. J. (1990). Primary rat Sertoli and interstitial cells exhibit a differential response to cadmium. Cell Biology and Toxicology, 6(1), 63–79. https://doi.org/10.1007/bf00135027
Concepcion-Zavaleta, M., Paz Ibarra, J. L., Ramos-Yataco, A., Coronado-Arroyo, J., Concepcion-Urteaga, L., Roseboom, P. J., & Williams, C. A. (2022). Assessment of hormonal status in male infertility. An update. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 16(3), 1447. https://doi.org/10.1016/j.dsx.2022.102447
Conrad, M., Ingold, I., Buday, K., Kobayashi, S., & Angeli, J. P. (2015). ROS, thiols and thiol-regulating systems in male gametogenesis. Biochimica Et Biophysica Acta, 1850(8), 1566–1574. https://doi.org/10.1016/j.bbagen.2014.10.020
Cooper, T. G., Noonan, E., Von Eckardstein, S., Auger, J., Baker, H. G., Behre, H. M., Haugen, T. B., Kruger, T., Wang, C., Mbizvo, M. T., & Vogelsong, K. M. (2010). World Health Organization reference values for human semen characteristics. Human Reproduction Update, 16(3), 231–245. https://doi.org/10.1093/humupd/dmp048
Cui, Z. G., Ahmed, K., Zaidi, S. F., & Muhammad, J. S. (2021). Ins and outs of cadmium-induced carcinogenesis: Mechanism and prevention. Cancer Treatment and Research Communications, 27, 100372. https://doi.org/10.1016/j.ctarc.2021.100372
Cullen, J. T., & Maldonado, M. T. (2013). Biogeochemistry of cadmium and its release to the environment. Metal Ions in Life Sciences, 11, 31–62. https://doi.org/10.1007/978-94-007-5179-8_2
Danielsson, B. R., Dencker, L., Lindgren, A., & Tjalve, H. (1984). Accumulation of toxic metals in male reproduction organs. Archives of Toxicology. Supplement, 7, 177–180. https://doi.org/10.1007/978-3-642-69132-4_26
de Angelis, C., Galdiero, M., Pivonello, C., Salzano, C., Gianfrilli, D., Piscitelli, P., Lenzi, A., Colao, A., & Pivonello, R. (2017). The environment and male reproduction: The effect of cadmium exposure on reproductive function and its implication in fertility. Reproductive Toxicology, 73, 105–127. https://doi.org/10.1016/j.reprotox.2017.07.021
Deng, Q., Dai, X., Feng, W., Huang, S., Yuan, Y., Xiao, Y., Zhang, Z., Deng, N., Deng, H., Zhang, X., & Kuang, D. (2019). Co-exposure to metals and polycyclic aromatic hydrocarbons, microRNA expression, and early health damage in coke oven workers. Environment International, 122, 369–380. https://doi.org/10.1016/j.envint.2018.11.056
Dixon, S. J., Lemberg, K. M., Lamprecht, M. R., Skouta, R., Zaitsev, E. M., Gleason, C. E., & Stockwell, B. R. (2012). Ferroptosis: An iron-dependent form of nonapoptotic cell death. Cell, 149(5), 1060–1072. https://doi.org/10.1016/j.cell.2012.03.042
Dohle, G. R. (2010). Male infertility in cancer patients: Review of the literature. International Journal of Urology, 17(4), 327–331. https://doi.org/10.1111/j.1442-2042.2010.02484.x
Dong, H., Chen, Z., Wang, C., Xiong, Z., Zhao, W., Jia, C., Lin, J., Lin, Y., Yuan, W., Zhao, A. Z., & Bai, X. (2015). Rictor regulates spermatogenesis by controlling Sertoli cell cytoskeletal organization and cell polarity in the mouse testis. Endocrinology, 156(11), 4244–4256. https://doi.org/10.1210/en.2015-1217
Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. https://doi.org/10.1136/bmj.315.7109.629
Fagerberg, B., & Barregard, L. (2021). Review of cadmium exposure and smoking-independent effects on atherosclerotic cardiovascular disease in the general population. Journal of Internal Medicine, 290(6), 1153–1179. https://doi.org/10.1111/joim.13350
Famurewa, A. C., & Ugwuja, E. I. (2017). Association of blood and seminal plasma cadmium and lead levels with semen quality in non-occupationally exposed infertile men in Abakaliki, South East Nigeria. Journal of Family and Reproductive Health, 11, 97–103.
Fang, Y., Zhang, L., Dong, X., Wang, H., He, L., & Zhong, S. (2020). Downregulation of vdac2 inhibits spermatogenesis via JNK and P53 signalling in mice exposed to cadmium. Toxicology Letters, 326, 114–122. https://doi.org/10.1016/j.toxlet.2020.03.011
Filippini, T., Wise, L. A., & Vinceti, M. (2022). Cadmium exposure and risk of diabetes and prediabetes: A systematic review and dose-response meta-analysis. Environmental International, 158, 106. https://doi.org/10.1016/j.envint.2021.106920
Fisher, R. A. (1932). Statistical methods for research workers (4th ed.). Oliver & Boyd.
Freire, C., Koifman, R. J., Fujimoto, D., de Oliveira Souza, V. C., Barbosa, F., Jr., & Koifman, S. (2015). Reference values of cadmium, arsenic and manganese in blood and factors associated with exposure levels among adult population of Rio Branco, Acre, Brazil. Chemosphere, 128, 70–78. https://doi.org/10.1016/j.chemosphere.2014.12.083
Fresno Vara, J. A., Casado, E., de Castro, J., Cejas, P., Belda-Iniesta, C., & González-Barón, M. (2004). PI3K/Akt signalling pathway and cancer. Cancer Treatment Reviews, 30(2), 193–204. https://doi.org/10.1016/j.ctrv.2003.07.007
Galán, A., García-Bermejo, L., Troyano, A., Vilaboa, N. E., Fernández, C., de Blas, E., & Aller, P. (2001). The role of intracellular oxidation in death induction (apoptosis and necrosis) in human promonocytic cells treated with stress inducers (cadmium, heat, X-rays). European Journal of Cell Biology, 80(4), 312–320. https://doi.org/10.1078/0171-9335-00159
Gao, F., Zhang, P., Zhang, H., Zhang, Y., Zhang, Y., Hao, Q., & Zhang, X. (2017). Dysregulation of long noncoding RNAs in mouse testes and spermatozoa after exposure to cadmium. Biochemical and Biophysical Research Communications, 484(1), 8–14. https://doi.org/10.1016/j.bbrc.2017.01.091
Garrett, C., Liu, D. Y., Clarke, G. N., Rushford, D. D., & Baker, H. W. (2003). Automated semen analysis: ‘Zona pellucida preferred’ sperm morphometry and straight-line velocity are related to pregnancy rate in subfertile couples. Human Reproduction, 18(8), 1643–1649. https://doi.org/10.1093/humrep/deg306
Genchi, G., Sinicropi, M. S., Lauria, G., Carocci, A., & Catalano, A. (2020). The effects of cadmium toxicity. International Journal of Environmental Research and Public Health. https://doi.org/10.3390/ijerph17113782
Gil, F., & Hernandez, A. F. (2015). Toxicological importance of human biomonitoring of metallic and metalloid elements in different biological samples. Food and Chemical Toxicology, 80, 287–297. https://doi.org/10.1016/j.fct.2015.03.025
Grioni, S., Agnoli, C., Krogh, V., Pala, V., Rinaldi, S., Vinceti, M., & Sieri, S. (2019). Dietary cadmium and risk of breast cancer subtypes defined by hormone receptor status: A prospective cohort study. International Journal of Cancer, 144(9), 2153–2160. https://doi.org/10.1002/ijc.32039
Guillette, L. J., Jr., & Edwards, T. M. (2008). Environmental influences on fertility: Can we learn lessons from studies of wildlife? Fertility and Sterility, 89(2 Suppl), e21-24. https://doi.org/10.1016/j.fertnstert.2007.12.019
Guzikowski, W., Szynkowska, M. I., Motak-Pochrzest, H., Pawlaczyk, A., & Sypniewski, S. (2015). Trace elements in seminal plasma of men from infertile couples. Archives of Medical Science, 11(3), 591–598. https://doi.org/10.5114/aoms.2015.52363
Habib, R., Wahdan, S. A., Gad, A. M., & Azab, S. S. (2019). Infliximab abrogates cadmium-induced testicular damage and spermiotoxicity via enhancement of steroidogenesis and suppression of inflammation and apoptosis mediators. Ecotoxicology and Environmental Safety, 182, 1398. https://doi.org/10.1016/j.ecoenv.2019.109398
Hall, P. F., Irby, D. C., & De Kretser, D. M. (1969). Conversion of cholesterol to androgens by rat testes: Comparison of interstitial cells and seminiferous tubules. Endocrinology, 84(3), 488–496. https://doi.org/10.1210/endo-84-3-488
Hassannia, B., Vandenabeele, P., & Vanden Berghe, T. (2019). Targeting ferroptosis to iron out cancer. Cancer Cell, 35(6), 830–849. https://doi.org/10.1016/j.ccell.2019.04.002
He, L., Li, P., Yu, L.-H., Li, L., Zhang, Y., Guo, Y., Long, M., He, J. B., & Yang, S.-H. (2018). Protective effects of proanthocyanidins against cadmium-induced testicular injury through the modification of Nrf2-Keap1 signal path in rats. Environmental Toxicology and Pharmacology, 57, 1–8. https://doi.org/10.1016/j.etap.2017.11.002
Heitland, P., & Koster, H. D. (2006). Biomonitoring of 37 trace elements in blood samples from inhabitants of northern Germany by ICP-MS. Journal of Trace Elements in Medicine and Biology, 20(4), 253–262. https://doi.org/10.1016/j.jtemb.2006.08.001
Huang, J., Chan, S. C., Tin, M. S., Liu, X., Lok, V. T., Ngai, C. H., & Wong, M. C. S. (2022). Worldwide distribution, risk factors, and temporal trends of testicular cancer incidence and mortality: A global analysis. European Urology Oncology. https://doi.org/10.1016/j.euo.2022.06.009
Huang, Y., Zhu, J., Li, H., Wang, W., Li, Y., Yang, X., Zheng, N., Liu, Q., Zhang, Q., Zhang, W., & Liu, J. (2020). Cadmium exposure during prenatal development causes testosterone disruption in multigeneration via SF-1 signaling in rats. Food and Chemical Toxicology, 135, 1197. https://doi.org/10.1016/j.fct.2019.110897
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. (1993). Cadmium and cadmium compounds. IARC Monogr Eval Carcinog Risks Hum (Vol. 58, pp. 119–237). https://www.ncbi.nlm.nih.gov/pubmed/8022055.
Jenardhanan, P., Panneerselvam, M., & Mathur, P. P. (2016). Effect of environmental contaminants on spermatogenesis. Seminars in Cell & Developmental Biology, 59, 126–140. https://doi.org/10.1016/j.semcdb.2016.03.024
Jeng, H. A., Huang, Y. L., Pan, C. H., & Diawara, N. (2015). Role of low exposure to metals as male reproductive toxicants. International Journal of Environmental Health Research, 25(4), 405–417. https://doi.org/10.1080/09603123.2014.958137
Ji, Y. L., Wang, H., Liu, P., Wang, Q., Zhao, X. F., Meng, X. H., Yu, T., Zhang, H., Zhang, C., Zhang, Y., & Xu, D. X. (2010). Pubertal cadmium exposure impairs testicular development and spermatogenesis via disrupting testicular testosterone synthesis in adult mice. Reproductive Toxicology, 29(2), 176–183.
Ji, Y. L., Wang, H., Liu, P., Zhao, X. F., Zhang, Y., Wang, Q., Zhang, H., Zhang, C., Duan, Z. H., Meng, C., & Xu, D. X. (2011). Effects of maternal cadmium exposure during late pregnant period on testicular steroidogenesis in male offspring. Toxicology Letters, 205(1), 69–78. https://doi.org/10.1016/j.toxlet.2011.05.233
Jurewicz, J., Radwan, M., Sobala, W., Radwan, P., Bochenek, M., & Hanke, W. (2014). Effects of occupational exposure—Is there a link between exposure based on an occupational questionnaire and semen quality? Systems Biology in Reproductive Medicine, 60(4), 227–233. https://doi.org/10.3109/19396368.2014.907837
Knazicka, Z., Forgacs, Z., Lukacova, J., Roychoudhury, S., Massanyi, P., & Lukac, N. (2015). Endocrine disruptive effects of cadmium on steroidogenesis: Human adrenocortical carcinoma cell line NCI-H295R as a cellular model for reproductive toxicity testing. Journal of Environmental Science and Health. Part A Toxic/hazardous Substances & Environmental Engineering, 50(4), 348–356. https://doi.org/10.1080/10934529.2015.987520
Knez, J. (2013). Endocrine-disrupting chemicals and male reproductive health. Reproductive Biomedicine Online, 26(5), 440–448. https://doi.org/10.1016/j.rbmo.2013.02.005
Koriem, K. M., Fathi, G. E., Salem, H. A., Akram, N. H., & Gamil, S. A. (2013). Protective role of pectin against cadmium-induced testicular toxicity and oxidative stress in rats. Toxicology Mechanisms and Methods, 23(4), 263–272. https://doi.org/10.3109/15376516.2012.748857
Kresovich, J. K., Argos, M., & Turyk, M. E. (2015). Associations of lead and cadmium with sex hormones in adult males. Environmental Research, 142, 25–33. https://doi.org/10.1016/j.envres.2015.05.026
Kumar, S., & Sharma, A. (2019). Cadmium toxicity: Effects on human reproduction and fertility. Reviews on Environmental Health, 34(4), 327–338. https://doi.org/10.1515/reveh-2019-0016
Kumar, S., Sharma, A., & Kshetrimayum, C. (2019). Environmental & occupational exposure & female reproductive dysfunction. Indian Journal of Medical Research, 150(6), 532–545. https://doi.org/10.4103/ijmr.IJMR_1652_17
Latif, J., Akhtar, J., Ahmad, I., Mahmood-ur-Rehman, M., Shah, G. M., Zaman, Q., Javaid, T., Farooqi, Z. U. R., Shakar, M., Saleem, A., & Rizwan, M. (2020). Unraveling the effects of cadmium on growth, physiology and associated health risks of leafy vegetables. Brazilian Journal of Botany, 43(4), 799–811. https://doi.org/10.1007/s40415-020-00653-0
La-Up, A., Mahasakpan, P., & Saengow, U. (2021). The current status of osteoporosis after 15 years of reduced cadmium exposure among residents living in cadmium-contaminated areas in northwestern Thailand. Environmental Science and Pollution Research International, 28(16), 20121–20127. https://doi.org/10.1007/s11356-020-12118-8
Lewis, R. C., & Meeker, J. D. (2015). Biomarkers of exposure to molybdenum and other metals in relation to testosterone among men from the United States National Health and Nutrition Examination Survey 2011–2012. Fertility and Sterility, 103(1), 172–178. https://doi.org/10.1016/j.fertnstert.2014.09.020
Li, L., Mao, B., Wu, S., Li, H., Lv, L., Ge, R., & Cheng, C. Y. (2020). Endogenously produced LG3/4/5-peptide protects testes against toxicant-induced injury. Cell Death & Disease, 11(6), 436. https://doi.org/10.1038/s41419-020-2608-8
Li, R., Zhao, L., Li, L., Hou, Z., Zhang, D., Wan, L., Wei, L., Yang, Y., Lv, J., Ma, M., & Zhu, Y. (2017). A preliminary study about the potential effects of heavy metals on the human male reproductive parameters in HIV-infected population in China. Biological Trace Element Research, 180(1), 39–47. https://doi.org/10.1007/s12011-017-0998-y
Li, Y., Wu, J., Zhou, W., & Gao, E. (2016). Association between environmental exposure to cadmium and human semen quality. International Journal of Environmental Health Research, 26(2), 175–186. https://doi.org/10.1080/09603123.2015.1061115
Liu, X., Tian, G., Jiang, D., Zhang, C., & Kong, L. (2016). Cadmium (Cd) distribution and contamination in Chinese paddy soils on national scale. Environmental Science and Pollution Research International, 23(18), 17941–17952. https://doi.org/10.1007/s11356-016-6968-7
Liu, Z., Wang, H., Larsen, M., Gunewardana, S., Cendali, F. I., Reisz, J. A., Akiyama, H., Behringer, R. R., Ma, Q., Hammoud, S. S., & Kumar, T. R. (2022). The solute carrier family 7 member 11 (SLC7A11) is regulated by LH/androgen and required for cystine/glutathione homeostasis in mouse Sertoli cells. Molecular and Cellular Endocrinology, 549, 111641. https://doi.org/10.1016/j.mce.2022.111641
Mahmoudi, R., Azizi, A., Abedini, S., Hemayatkhah Jahromi, V., Abidi, H., & Jafari Barmak, M. (2018). Green tea improves rat sperm quality and reduced cadmium chloride damage effect in spermatogenesis cycle. Journal of Medicine and Life, 11(4), 371–380. https://doi.org/10.25122/jml-2018-0005
Malin, A. J., & Wright, R. O. (2018). The developmental neurotoxicity of cadmium. In Handbook of developmental neurotoxicology (pp. 407–412). https://doi.org/10.1016/b978-0-12-809405-1.00036-5.
Martínez-Abad, S., Castillo-Martín, M., Gadani, B., Rodríguez-Gil, J. E., Bonet, S., & Yeste, M. (2017). Voltage-dependent anion channel 2 is involved in in vitro capacitation of boar sperm. Reproduction in Domestic Animals, 52(Suppl 4), 65–68. https://doi.org/10.1111/rda.13060
Matsuoka, M., & Igisu, H. (2001). Cadmium induces phosphorylation of p53 at serine 15 in MCF-7 cells. Biochemical and Biophysical Research Communications, 282(5), 1120–1125. https://doi.org/10.1006/bbrc.2001.4700
Mearini, L., Costantini, E., Zucchi, A., Mearini, E., Bini, V., Cottini, E., & Porena, M. (2008). Testosterone levels in benign prostatic hypertrophy and prostate cancer. Urologia Internationalis, 80(2), 134–140. https://doi.org/10.1159/000112602
Meeker, J. D., Rossano, M. G., Protas, B., Padmanahban, V., Diamond, M. P., Puscheck, E., Daly, D., Paneth, N., & Wirth, J. J. (2010). Environmental exposure to metals and male reproductive hormones: Circulating testosterone is inversely associated with blood molybdenum. Fertility and Sterility, 93(1), 130–140. https://doi.org/10.1016/j.fertnstert.2008.09.044
Menke, A., Guallar, E., Shiels, M. S., Rohrmann, S., Basaria, S., Rifai, N., Nelson, W. G., & Platz, E. A. (2008). The association of urinary cadmium with sex steroid hormone concentrations in a general population sample of US adult men. BMC Public Health, 8, 72. https://doi.org/10.1186/1471-2458-8-72
Mhaouty-Kodja, S., Naule, L., & Capela, D. (2018). Sexual behavior: From hormonal regulation to endocrine disruption. Neuroendocrinology, 107(4), 400–416. https://doi.org/10.1159/000494558
Miller, W. L. (2007). StAR search—What we know about how the steroidogenic acute regulatory protein mediates mitochondrial cholesterol import. Molecular Endocrinology, 21(3), 589–601. https://doi.org/10.1210/me.2006-0303
Mitchell, R. T., Sharpe, R. M., Anderson, R. A., McKinnell, C., Macpherson, S., Smith, L. B., Wallace, W. H. B., Kelnar, C. J., & van den Driesche, S. (2013). Diethylstilboestrol exposure does not reduce testosterone production in human fetal testis xenografts. PLoS ONE, 8(4), e61726. https://doi.org/10.1371/journal.pone.0061726
Mitra, S., Bhattacharyya, S., Ray, S., Saha, R., Ghosh, P., Rauth, S., Mandal, S., Banerjee, S., & Murmu, N. (2016). Resveratrol alleviates cadmium-induced damage and overexpression of epidermal growth factor receptor and its downstream signaling proteins in the reproductive system of male Swiss albino mice. Jjournal of Environmental Pathology, Toxicology and Oncology, 35(1), 73–90. https://doi.org/10.1615/JEnvironPatholToxicolOncol.2016015298
Mitra, S., Patra, T., Saha, D., Ghosh, P., Mustafi, S. M., Varghese, A. C., & Murmu, N. (2022). Sub-chronic cadmium and lead compound exposure induces reproductive toxicity and development of testicular germ cell neoplasia in situ in murine model: Attenuative effects of resveratrol. Journal of Biochemical and Molecular Toxicology, 36(7), e23058. https://doi.org/10.1002/jbt.23058
Murawski, M., Saczko, J., Marcinkowska, A., Chwilkowska, A., Grybos, M., & Banas, T. (2007). Evaluation of superoxide dismutase activity and its impact on semen quality parameters of infertile men. Folia Histochemica Et Cytobiologica, 45(Suppl 1), S123-126.
Nelson, C. M., & Bunge, R. G. (1974). Semen analysis: Evidence for changing parameters of male fertility potential. Fertility and Sterility, 25(6), 503–507. https://doi.org/10.1016/s0015-0282(16)40454-1
Nissensohn, M., Sánchez-Villegas, A., Fuentes Lugo, D., Henríquez Sánchez, P., Doreste Alonso, J., Peña Quintana, L., Ruano, C., Lowe, N. L., Hall Moran, V., Skinner, A. L., & Warthon-Medina, M. (2016). Effect of zinc intake on growth in infants: A meta-analysis. Critical Reviews in Food Science and Nutrition, 56(3), 350–363. https://doi.org/10.1080/10408398.2013.802661
Noack-Fuller, G., De Beer, C., & Seibert, H. (1993). Cadmium, lead, selenium, and zinc in semen of occupationally unexposed men. Andrologia, 25(1), 7–12. https://doi.org/10.1111/j.1439-0272.1993.tb02674.x
Nordberg, G. F. (2009). Historical perspectives on cadmium toxicology. Toxicology and Applied Pharmacology, 238(3), 192–200. https://doi.org/10.1016/j.taap.2009.03.015
Page, M. J., Moher, D., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., & Chou, R. (2021). PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ, 372, n160. https://doi.org/10.1136/bmj.n160
Pathak, U. I., Gabrielsen, J. S., & Lipshultz, L. I. (2020). Cutting-edge evaluation of male infertility. Urologic Clinics of North America, 47(2), 129–138. https://doi.org/10.1016/j.ucl.2019.12.001
Pires, V. C., Gollücke, A. P., Ribeiro, D. A., Lungato, L., D’Almeida, V., & Aguiar, O., Jr. (2013). Grape juice concentrate protects reproductive parameters of male rats against cadmium-induced damage: A chronic assay. British Journal of Nutrition, 110(11), 2020–2029. https://doi.org/10.1017/s0007114513001360
Pizzol, D., Foresta, C., Garolla, A., Demurtas, J., Trott, M., Bertoldo, A., & Smith, L. (2021). Pollutants and sperm quality: A systematic review and meta-analysis. Environmental Science and Pollution Research International, 28(4), 4095–4103. https://doi.org/10.1007/s11356-020-11589-z
Practice Committee of the American Society for Reproductive, M. (2015). Diagnostic evaluation of the infertile male: A committee opinion. Fertility and Sterility, 103(3), e18-25. https://doi.org/10.1016/j.fertnstert.2014.12.103
Qiu, Y., Lv, Y., Zhang, M., Ji, S., Wu, B., Zhao, F., Qu, Y., Sun, Q., Guo, Y., Zhu, Y., & Lin, X. (2022). Cadmium exposure is associated with testosterone levels in men: A cross-sectional study from the China National Human Biomonitoring. Chemosphere, 307(Pt 2), 135786. https://doi.org/10.1016/j.chemosphere.2022.135786
Ren, X.-M., Wang, G.-G., Xu, D.-Q., Luo, K., Liu, Y.-X., Zhong, Y.-H., & Cai, Y.-Q. (2012). The protection of selenium on cadmium-induced inhibition of spermatogenesis via activating testosterone synthesis in mice. Food and Chemical Toxicology, 50(10), 3521–3529. https://doi.org/10.1016/j.fct.2012.07.021
Ren, Y., Shao, W., Zuo, L., Zhao, W. E., Qin, H., Hua, Y., Lu, D., Mi, C., Zeng, S., & Zu, L. (2019). Mechanism of cadmium poisoning on testicular injury in mice. Oncology Letters, 18(2), 1035–1042. https://doi.org/10.3892/ol.2019.10418
Ribeiro, I. M., Viana, A. G. A., Carvalho, R. P. R., Waddington, B., & Machado-Neves, M. (2022). Could metal exposure affect sperm parameters of domestic ruminants? A meta-analysis. Animal Reproduction Science, 244, 107050. https://doi.org/10.1016/j.anireprosci.2022.107050
Ronco, A. M., Arguello, G., Munoz, L., Gras, N., & Llanos, M. (2005). Metals content in placentas from moderate cigarette consumers: Correlation with newborn birth weight. BioMetals, 18(3), 233–241. https://doi.org/10.1007/s10534-005-0583-2
Rotter, I., Kosik-Bogacka, D. I., Dolegowska, B., Safranow, K., Kuczynska, M., & Laszczynska, M. (2016). Analysis of the relationship between the blood concentration of several metals, macro- and micronutrients and endocrine disorders associated with male aging. Environmental Geochemistry and Health, 38(3), 749–761. https://doi.org/10.1007/s10653-015-9758-0
Saaranen, M., Kantola, M., Saarikoski, S., & Vanha-Perttula, T. (1989). Human seminal plasma cadmium: Comparison with fertility and smoking habits. Andrologia, 21(2), 140–145.
Sabir, S., Akash, M. S. H., Fiayyaz, F., Saleem, U., Mehmood, M. H., & Rehman, K. (2019). Role of cadmium and arsenic as endocrine disruptors in the metabolism of carbohydrates: Inserting the association into perspectives. Biomedicine & Pharmacotherapy, 114, 108802. https://doi.org/10.1016/j.biopha.2019.108802
Sharma, R., Biedenharn, K. R., Fedor, J. M., & Agarwal, A. (2013). Lifestyle factors and reproductive health: Taking control of your fertility. Reproductive Biology and Endocrinology, 11, 66. https://doi.org/10.1186/1477-7827-11-66
Shi, X., & Fu, L. (2019). Piceatannol inhibits oxidative stress through modification of Nrf2-signaling pathway in testes and attenuates spermatogenesis and steroidogenesis in rats exposed to cadmium during adulthood. Drug Design, Development and Therapy, 13, 2811–2824. https://doi.org/10.2147/dddt.S198444
Sigman, M., & Jarow, J. P. (1997). Endocrine evaluation of infertile men. Urology, 50(5), 659–664. https://doi.org/10.1016/S0090-4295(97)00340-3
Siu, E. R., Mruk, D. D., Porto, C. S., & Cheng, C. Y. (2009). Cadmium-induced testicular injury. Toxicology and Applied Pharmacology, 238(3), 240–249. https://doi.org/10.1016/j.taap.2009.01.028
Skakkebaek, N. E., Rajpert-De Meyts, E., & Main, K. M. (2001). Testicular dysgenesis syndrome: An increasingly common developmental disorder with environmental aspects. Human Reproduction, 16(5), 972–978. https://doi.org/10.1093/humrep/16.5.972
Sokol, R. Z., Kraft, P., Fowler, I. M., Mamet, R., Kim, E., & Berhane, K. T. (2006). Exposure to environmental ozone alters semen quality. Environmental Health Perspectives, 114(3), 360–365. https://doi.org/10.1289/ehp.8232
Song, T., Wang, L., Mo, Z., Mao, L., Ma, X., Niu, R., Gu, K., Yan, R., Ma, P., Qi, Y., & Jiao, Q. (2014). Expression of p-Akt in ovarian serous carcinoma and its association with proliferation and apoptosis. Oncology Letters, 7(1), 59–64. https://doi.org/10.3892/ol.2013.1641
Special Programme of Research Development and Research Training in Human Reproduction (World Health Organization). (1992). WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction (3rd ed.). Published on behalf of the World Health Organization by Cambridge University Press.
Srivastava, V., Sarkar, A., Singh, S., Singh, P., de Araujo, A. S. F., & Singh, R. P. (2017). Agroecological responses of heavy metal pollution with special emphasis on soil health and plant performances. Frontiers in Environmental Science. https://doi.org/10.3389/fenvs.2017.00064
Stang, A. (2010). Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. European Journal of Epidemiology, 25(9), 603–605. https://doi.org/10.1007/s10654-010-9491-z
Suhani, I., Sahab, S., Srivastava, V., & Singh, R. P. (2021). Impact of cadmium pollution on food safety and human health. Current Opinion in Toxicology, 27, 1–7. https://doi.org/10.1016/j.cotox.2021.04.004
Sun, J., Yu, G., Zhang, Y., Liu, X., Du, C., Wang, L., Li, Z., & Wang, C. (2017). Heavy metal level in human semen with different fertility: A meta-analysis. Biological Trace Element Research, 176(1), 27–36. https://doi.org/10.1007/s12011-016-0804-2
Swiergosz-Kowalewska, R. (2001). Cadmium distribution and toxicity in tissues of small rodents. Microscopy Research and Technique, 55(3), 208–222. https://doi.org/10.1002/jemt.1171
Tang, X., Tang, S., Ren, Z., & Wong, D. F. K. (2020). Psychological risk and protective factors associated with depressive symptoms among adolescents in secondary schools in China: A systematic review and meta-analysis. Children and Youth Services Review. https://doi.org/10.1016/j.childyouth.2019.104680
Templeton, A. (1995). Infertility-epidemiology, aetiology and effective management. Health Bulletin (edinburgh), 53(5), 294–298.
Thorup, J., McLachlan, R., Cortes, D., Nation, T. R., Balic, A., Southwell, B. R., & Hutson, J. M. (2010). What is new in cryptorchidism and hypospadias—A critical review on the testicular dysgenesis hypothesis. Journal of Pediatric Surgery, 45(10), 2074–2086. https://doi.org/10.1016/j.jpedsurg.2010.07.030
Tuncay, G., Karaer, A., Tanrikut, E., & Ozgul, O. (2021). The effect of seminal plasma cadmium and lead levels on semen parameters in male subjects of infertile couples: A prospective cohort study. Journal of Obstetrics and Gynaecology, 41(6), 946–950. https://doi.org/10.1080/01443615.2020.1820459
Vacchi-Suzzi, C., Kruse, D., Harrington, J., Levine, K., & Meliker, J. R. (2016). Is urinary cadmium a biomarker of long-term exposure in humans? A review. Current Environmental Health Reports, 3(4), 450–458. https://doi.org/10.1007/s40572-016-0107-y
Varga, B., Zsolnai, B., Paksy, K., Naray, M., & Ungvary, G. (1993). Age dependent accumulation of cadmium in the human ovary. Reproductive Toxicology, 7(3), 225–228. https://doi.org/10.1016/0890-6238(93)90228-y
Venditti, M., Ben Rhouma, M., Romano, M. Z., Messaoudi, I., Reiter, R. J., & Minucci, S. (2021). Altered expression of DAAM1 and PREP induced by cadmium toxicity is counteracted by melatonin in the rat testis. Genes (basel). https://doi.org/10.3390/genes12071016
Venditti, M., Chemek, M., Minucci, S., & Messaoudi, I. (2020). Cadmium-induced toxicity increases prolyl endopeptidase (PREP) expression in the rat testis. Molecular Reproduction and Development, 87(5), 565–573. https://doi.org/10.1002/mrd.23345
Venkatesh, S., Singh, A., Shamsi, M. B., Thilagavathi, J., Kumar, R., Mitra, D. K., & Dada, R. (2011). Clinical significance of sperm DNA damage threshold value in the assessment of male infertility. Reproductive Sciences, 18(10), 1005–1013. https://doi.org/10.1177/1933719111401662
Ventimiglia, E., Montorsi, F., & Salonia, A. (2017). Re: Reecha Sharma, Avi Harlev, Ashok Agarwal, Sandro C. Esteves. Cigarette smoking and semen quality: A new meta-analysis examining the effect of the 2010 World Health Organization Laboratory methods for the examination of human semen. Eur Urol 2016;70:63. European Urology, 71(1), e19–e20. https://doi.org/10.1016/j.eururo.2016.05.051
Ventura, C., Gomes, B. C., Oberemm, A., Louro, H., Huuskonen, P., Mustieles, V., Fernández, M. F., Ndaw, S., Mengelers, M., Luijten, M., & Gundacker, C. (2021). Biomarkers of effect as determined in human biomonitoring studies on hexavalent chromium and cadmium in the period 2008–2020. Environmental Research, 197, 110. https://doi.org/10.1016/j.envres.2021.110998
Walker, W. H. (2011). Testosterone signaling and the regulation of spermatogenesis. Spermatogenesis, 1(2), 116–120. https://doi.org/10.4161/spmg.1.2.16956
Wang, P., Chen, H., Kopittke, P. M., & Zhao, F. J. (2019). Cadmium contamination in agricultural soils of China and the impact on food safety. Environmental Pollution, 249, 1038–1048. https://doi.org/10.1016/j.envpol.2019.03.063
Wang, X., Wang, M., Zeng, L., & Su, P. (2020). Hypomethylation of LINE-1 retrotransposons is associated with cadmium-induced testicular injury. Environmental Science and Pollution Research International, 27(32), 40749–40756. https://doi.org/10.1007/s11356-020-10115-5
Wang, Y., Li, T., Li, H., Liang, Y., Mai, W., Liu, C., Chen, H., Huang, Y., & Zhang, Q. (2022). CORO1A regulates lipoprotein uptake in Leydig cells exposed to cadmium. Ecotoxicology and Environmental Safety, 232, 113255. https://doi.org/10.1016/j.ecoenv.2022.113255
Williams, D. H. T., Karpman, E., Sander, J. C., Spiess, P. E., Pisters, L. L., & Lipshultz, L. I. (2009). Pretreatment semen parameters in men with cancer. Journal of Urology, 181(2), 736–740. https://doi.org/10.1016/j.juro.2008.10.023
Winiarska-Mieczan, A. (2018). Protective effect of tea against lead and cadmium-induced oxidative stress-a review. BioMetals, 31(6), 909–926. https://doi.org/10.1007/s10534-018-0153-z
Wittman, R., & Hu, H. (2002). Cadmium exposure and nephropathy in a 28-year-old female metals worker. Environmental Health Perspectives, 110(12), 1261–1266. https://doi.org/10.1289/ehp.021101261
World Health Organization. (1999). WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction (4th edn). Published on behalf of the World Health Organization by Cambridge University Press. Sample text http://www.loc.gov/catdir/samples/cam032/98046890.html. Publisher description http://www.loc.gov/catdir/description/cam029/98046890.html. Table of contents http://www.loc.gov/catdir/toc/cam026/98046890.html.
World Health Organization. (2010). WHO laboratory manual for the examination and processing of human semen (5th edn). World Health Organization.
Wu, H. M., Lin-Tan, D. T., Wang, M. L., Huang, H. Y., Wang, H. S., Soong, Y. K., & Lin, J. L. (2008). Cadmium level in seminal plasma may affect the pregnancy rate for patients undergoing infertility evaluation and treatment. Reproductive Toxicology, 25(4), 481–484. https://doi.org/10.1016/j.reprotox.2008.04.005
Xiao, X., Cheng, C. Y., & Mruk, D. D. (2013). Intercellular adhesion molecule-2 is involved in apical ectoplasmic specialization dynamics during spermatogenesis in the rat. Journal of Endocrinology, 216(1), 73–86. https://doi.org/10.1530/joe-12-0434
Xing, D., Xu, Y., Liu, Q., Ke, Y., Wang, B., Li, Z., & Lin, J. (2016). Osteoarthritis and all-cause mortality in worldwide populations: Grading the evidence from a meta-analysis. Science and Reports, 6, 24393. https://doi.org/10.1038/srep24393
Xing, J. S., & Bai, Z. M. (2018). Is testicular dysgenesis syndrome a genetic, endocrine, or environmental disease, or an unexplained reproductive disorder? Life Sciences, 194, 120–129. https://doi.org/10.1016/j.lfs.2017.11.039
Xu, B., Chia, S. E., Tsakok, M., & Ong, C. N. (1993). Trace elements in blood and seminal plasma and their relationship to sperm quality. Reproductive Toxicology, 7(6), 613–618. https://doi.org/10.1016/0890-6238(93)90038-9
Xu, D.-X., Shen, H.-M., Zhu, Q.-X., Chua, L., Wang, Q.-N., Chia, S.-E., & Ong, C.-N. (2003). The associations among semen quality, oxidative DNA damage in human spermatozoa and concentrations of cadmium, lead and selenium in seminal plasma. Mutation Research/genetic Toxicology and Environmental Mutagenesis, 534, 155–163.
Xu, Y., Mu, W., Li, J., Ba, Q., & Wang, H. (2021). Chronic cadmium exposure at environmental-relevant level accelerates the development of hepatotoxicity to hepatocarcinogenesis. Science of the Total Environment, 783, 146958. https://doi.org/10.1016/j.scitotenv.2021.146958
Zagreb, C., Vrhovac, V., & Zagreb, C. (2000). Semen quality and reproductive endocrine function relation to biomarkers of lead, cadmium, zinc, and copper in men. Environmental Health Perspectives, 108, 45–53.
Zeng, L., Zhou, J., Wang, X., Zhang, Y., Wang, M., & Su, P. (2021). Cadmium attenuates testosterone synthesis by promoting ferroptosis and blocking autophagosome-lysosome fusion. Free Radical Biology & Medicine, 176, 176–188. https://doi.org/10.1016/j.freeradbiomed.2021.09.028
Zeng, X., Jin, T., Buchet, J. P., Jiang, X., Kong, Q., Ye, T., Bernard, A., & Nordberg, G. F. (2004). Impact of cadmium exposure on male sex hormones: A population-based study in China. Environmental Research, 96(3), 338–344. https://doi.org/10.1016/j.envres.2004.02.004
Zhang, Q., Bai, Q., Yuan, Y., Liu, P., & Qiao, J. (2010). Assessment of seminal estradiol and testosterone levels as predictors of human spermatogenesis. Journal of Andrology, 31(2), 215–220. https://doi.org/10.2164/jandrol.109.007609
Zhang, X., & Lui, W. Y. (2014). Dysregulation of nectin-2 in the testicular cells: An explanation of cadmium-induced male infertility. Biochimica Et Biophysica Acta, 1839(9), 873–884. https://doi.org/10.1016/j.bbagrm.2014.07.012
Zhang, X., Zhong, T., Liu, L., & Ouyang, X. (2015). Impact of soil heavy metal pollution on food safety in China. PLoS ONE, 10(8), 35182. https://doi.org/10.1371/journal.pone.0135182
Zhang, Y., Li, S., & Li, S. (2019). Relationship between cadmium content in semen and male infertility: A meta-analysis. Environmental Science and Pollution Research International, 26(2), 1947–1953. https://doi.org/10.1007/s11356-018-3748-6
Zhao, W., Jing, J., Shao, Y., Zeng, R., Wang, C., Yao, B., & Hang, D. (2020). Circulating sex hormone levels in relation to male sperm quality. BMC Urology, 20(1), 101. https://doi.org/10.1186/s12894-020-00674-7
Zhong, H., Chiles, K., Feldser, D., Laughner, E., Hanrahan, C., Georgescu, M. M., Simons, J. W., & Semenza, G. L. (2000). Modulation of hypoxia-inducible factor 1α expression by the epidermal growth factor/phosphatidylinositol 3-kinase/PTEN/AKT/FRAP pathway in human prostate cancer cells: implications for tumor angiogenesis and therapeutics. Cancer Research, 60(6), 1541–1545.
Zhou, G. X., Liu, W. B., Dai, L. M., Zhu, H. L., Xiong, Y. W., Li, D. X., Xu, D. X., & Wang, H. (2022a). Environmental cadmium impairs blood-testis barrier via activating HRI-responsive mitochondrial stress in mice. Science of the Total Environment, 810, 152247. https://doi.org/10.1016/j.scitotenv.2021.152247
Zhou, J., Zhang, Y., Zeng, L., Wang, X., Mu, H., Wang, M., Pan, H., & Su, P. (2022b). Paternal cadmium exposure affects testosterone synthesis by reducing the testicular cholesterol pool in offspring mice. Ecotoxicology and Environmental Safety, 242, 113947. https://doi.org/10.1016/j.ecoenv.2022.113947
Funding
This work was supported by the National Natural Science Foundation of China (Grant numbers [82273598]) and the Nature Science Research Project of Anhui Province (Grant number [2108085MH305]).
Author information
Authors and Affiliations
Contributions
XG and JXZ contributed to the study conception and design. Material preparation, data collection and analysis were performed by XG, GYL, XCP, JJX, DY, YX, and XR. The first draft of the manuscript was written by XG, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, X., Li, G., Pan, X. et al. Environmental and occupational exposure to cadmium associated with male reproductive health risk: a systematic review and meta-analysis based on epidemiological evidence. Environ Geochem Health 45, 7491–7517 (2023). https://doi.org/10.1007/s10653-023-01719-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10653-023-01719-0