Abstract
Organotin compounds, such as tributyltin (TBT), are environment contaminants that induce bioaccumulation and have potential toxic effects on marine species and mammals. TBT have been banned by the International Maritime Organization in 2003. However, the assessment of butyltin and metal contents in marine sediments has demonstrated high residual levels of TBT in some cases exceeding 7000 ng Sn g−1. The acceptable daily intake (ADI) level for TBT established by the World Health Organization is 0.5 μg/kg bw/day is based on genotoxicity, reproduction, teratogenicity, immunotoxicity, and mainly neurotoxicity. However, their effect on the cardiovascular system is not well understood. In this study, female rats were exposed to 0.5 μg/kg/day of TBT for 15 days with the goal of understanding the effect of TBT on vascular function. Female Wistar rats were treated daily by gavage and divided into control (n = 10) and TBT (n = 10) groups. The aortic rings were incubated with phenylephrine in both the presence and absence of endothelium. The phenylephrine concentration–response curves were generated by exposing endothelium-intact samples to NG-nitro-l-arginine methyl ester (L-NAME), apocynin, superoxide dismutase (SOD), catalase, tiron, and allopurinol. Acetylcholine (ACh) and sodium nitroprusside (SNP) were used to evaluate the relaxation response. Exposure to TBT reduced serum 17β-estradiol E2 levels and increased vascular reactivity. After incubation with L-NAME, the vascular reactivity to phenylephrine was significantly higher. Apocynin, SOD, catalase, and tiron decreased the vascular reactivity to phenylephrine to a significantly greater extent in TBT-treated rats than in the control rat. The relaxation induced by ACh and SNP was significantly reduced in TBT rats. Exposure to TBT induced aortic wall atrophy and increased superoxide anion production and collagen deposition. These results provide evidence that exposing rats to the current ADI for TBT (0.5 μg/kg) for 15 days induced vascular dysfunction due to oxidative stress and morphological damage and should be considered an important cardiovascular risk factor.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tributyltin (TBT) is an organotin (OT) compound used in the antifouling of ship paints and as an agricultural fungicide (Bryan et al. 1986; Hoch 2001). OTs such as TBT are widely distributed in the oceans, and its high hydrophobicity in the environment promotes bioaccumulation that can result in toxic effects within food webs (Galloway 2006; Antizar-Ladislao 2008).
Although TBT use in paints has been banned by the International Maritime Organization and European Union since 2003, it is still found at high levels that exceed toxicity limits in certain ecosystems and seafood (Antizar-Ladislao 2008). Studies have reported that the toxicological effect of TBT can be expected to persist for years after exposure (Kotrikla 2009; Morton 2009), as TBT is a highly persistent chemical. Assessments of butyltins and metals in marine sediments have demonstrated high levels of TBT that can exceed of 7000 ng Sn g−1 (Costa et al. 2014; Hartwell et al. 2016).
OTs have been reported to impair growth, development, reproduction, and survival of marine species with the decline of mollusks in coastal areas due to imposex marine species. This phenomenon occurs when male sex characteristics are superimposed on normal female gastropods (dos Santos et al. 2016; Costa et al. 2014; Konstantinou and Albanis 2004; Cooke 2006; Antizar-Ladislao 2008). Consumption of contaminated drinking water and marine food has been reported as an important human exposure pathway to TBT, causing possible harmful effects on human health. OTs have been detected in human blood at levels ranging from 64 to 155 ng/mL, which leads to TBT tissue accumulation and dysfunction (Whalen et al. 1999). However, despite the evidence that such sources expose humans to OT, limited data on the effects of TBT on humans are available, and several animal model studies and estimates of marine food intake are required (Kannan et al. 1999; Takahashi et al. 1999; Nielsen and Strand 2002; Cooke 2006; Nakanishi 2007; Antizar-Ladislao 2008).
It is known that the chronic exposure to TBT at concentrations between 0.5 and 50 μg/kg can result in obesity in male mice as a result of increased adiposity and hepatic steatosis along with insulin and leptin resistance (Zuo et al. 2011). TBT was administered by gavage at a dose of 25 μg/kg/day/bw to male and female mice for 4 weeks and interfered with the neural circuit involved in the stimulation of food intake and led to abnormal in the leptin system (Bo et al. 2016). Toxic effects occurred at different levels on the hypothalamus–pituitary–adrenal axis in female rats leading to inflammation, oxidative stress, and fibrotic processes after exposure to TBT (Merlo et al. 2016). Toxic effects on the cardiovascular system have also been reported following TBT exposure in female rats (dos Santos et al. 2012; Rodrigues et al. 2014; Ribeiro Junior et al. 2016).
In some short- and long-term studies, the critical effect of TBT was the immunotoxicity. A tolerable daily intake (TDI) of 0.25 mg/kg/day/bw was established based on reductions in lymphoid organ weights or lymphoid function when TBT was included in male rat diets (Penninks 1993). The no-observed-adverse-effect level (NOAEL) for immunosuppression in rats, following long-term exposure, was 25 μg/ kg/day/bw (WHO 1999). A lack of human data regarding the toxic effects of TBT resulted in a safety factor of 100 that means a TDI of 0.25 μg/kg bw/day appropriate for TBT when expressed as Sn content and, 0.27 μg/kg bw, when it is expressed as TBT (EFSA 2004; Penninks 1993). The acceptable daily intake (ADI) of TBT established by the World Health Organization (WHO) and based on a 200-fold multiplication of the NOAEL is 0.1 mg/kg/day/bw, and in a 2-year study in rats, this level was 0.5 μg/kg/day/bw.
The main cardiovascular risk factors including smoking, aging, hypercholesterolemia, hypertension, hyperglycemia, and atherosclerotic disease are associated with alteration in endothelial function (Sorensen et al. 1994). However, epidemiological and experimental studies have suggested a connection between exposure to metal components in the environment and endothelium dysfunction (Wiggers et al. 2008; Fiorim et al. 2012; Almenara et al. 2013). The deleterious alterations of vascular endothelial function is considered a key early step in the development of atherosclerosis being involved in the occurrence of atherosclerotic complications representing an important risk factor for cardiovascular disease (Anderson et al. 1995; Kinlay and Ganz 1997).
Endothelial dysfunction is characterized by reduction of the bioavailability of vasodilators, mainly nitric oxide (NO), an increase in endothelium-derived contracting factors (EDCF) and vascular oxidative stress. Considering TBT toxic effects in female rats lead to inflammation, oxidative stress, and fibrotic processes (Merlo et al. 2016; dos Santos et al. 2012), we will test the hypothesis that animal exposure to TBT may present endothelial dysfunction, being a risk factor to develop atherosclerotic disease. In this study, we investigated the effects of exposure to TBT, at the ADI of 0.5 μg/kg/day/bw for 15 days, on the aortic endothelial function of female rats.
Materials and methods
Drugs and reagents
The following materials were used for the experiments: l-phenylephrine hydrochloride, acetylcholine chloride (ACh), NG-nitro-l-arginine methyl ester hydrochloride (L-NAME), apocynin, catalase, tiron, allopurinol, superoxide dismutase, and tributyltin chloride (TBT, 96%). All of these materials were purchased from Sigma (St. Louis, MO, USA). In addition, thiobarbituric acid (Alfa Aesar, USA), sodium nitroprusside (SNP) (Merck & Co., Inc., Rahway, NY, USA), and sodium phenobarbital (Fontoveter, Brazil) were used. The chemicals were dissolved in distilled water except for TBT, which was dissolved in 0.4% ethanol. Analytical grade salts and reagents were used.
Animals and treatment
The studies were performed with 12-week-old female Wistar rats (250–300 g). All experiments were conducted in accordance with the guidelines for biomedical research as stated by the Brazilian Societies for Experimental Biology and with the approval of the Local Ethics Committee for Animals (CEUA-UFES 020/2009). All rats had access to water and rodent chow ad libitum. The rats were randomly divided into two groups: control animals that received 100 μL of 0.4% ethanol daily as a vehicle (control, n = 10), and TBT-exposed rats that received 0.5 μg kg−1 day−1 TBT diluted in 0.4% ethanol by gavage for 15 days. Each group consisted of 10 rats. This TBT concentration was chosen because it represents the ADI established by the World Health Organization (IPCS 1999a).
After 15 days, rats were anesthetized with pentobarbital (35 mg/kg, i.p.), the thoracic aorta was carefully dissected, and the connective tissue was removed. The aortas were divided into 4-mm cylindrical segments. To analyze protein expression, the arteries were stored at − 80 °C for future analysis.
Hormonal measurement
Serum 17β-estradiol (E2) levels were measured from female rats blood samples (n = 5 per group) after euthanasia. Serum E2 levels were measured using an ELISA assay (no. 42K034 DRG Instruments GmbH, Germany) on an ELx808™ Absorbance Microplate Reader (BioTek Instruments, Inc., Winooski, VT, USA). A standard curve was generated using sixfold serial dilutions of the hormone reference provided by Diagnostic Systems Laboratories. Low- and high-quality controls were run on each assay to assess the coefficient of variation. The assay detection limit for E2 was 9.71 pg/mL. The intra-assay coefficient of variation for each assay was between 4 and 7%. The inter-assay coefficient of variation for each assay was between 6 and 9% (Coutinho et al. 2016; Ribeiro Júnior et al. 2016).
Homogenate preparation and measurement of thiobarbituric acid-reactive substances
Lipid peroxidation was evaluated by measuring the level of thiobarbituric acid-reactive substances (TBARS). Were used from 5 animals per treatment group. Aortic tissue was collected, and adipose tissue was manually removed. The samples were then transferred to 1.5-mL Eppendorf tubes containing an extraction buffer (ice-cold 50 mM sodium phosphate buffer, pH 7.4) with a protease inhibitor. The homogenates were centrifuged at 825×g at 4 °C for 15 min. The supernatants were stored at − 80 °C until the lipid peroxidation assay was performed.
Aliquots (0.05 mL) of each homogenate were mixed with 0.25 mL of a 1% solution of thiobarbituric acid, heated at 90 °C for 2 h, and then subjected to absorption measurement at 532 nm (Ma et al. 2003). The final TBARS values were expressed as nM/mg of protein using an extinction coefficient of 156 mM−1 cm−1 (Hermes-Lima et al. 1995). The homogenate protein concentration was determined by a Bradford assay (Sigma-Aldrich) using bovine serum albumin as the standard.
Vascular reactivity measurements
Thoracic aorta segments were mounted between two parallel wires in an isolated tissue chamber in Krebs-Henseleit buffer (125 mM NaCl, 4.6 mM KCl, 2.5 mM CaCl2, 1.2 mM MgSO4, 1.2 mM KH2PO4, 11.0 mM glucose, 0.01 mM EDTA, and 23 mM NaHCO3) with a 95% O2 and 5% CO2 atmosphere (pH 7.4). The aortas were maintained at a resting tension of 1 g at 37 °C. The isometric tension was recorded using an isometric force transducer (TSD125C, BIOPAC Systems, CA, USA) connected to an acquisition system (MP100, BIOPAC Systems). Were used from 10 animals per treatment group.
After 45 min of stabilization, the aortic rings were exposed to 75 mM KCl. The endothelial integrity was then assessed with ACh (10 μM) in the segments that had been previously treated with phenylephrine (1 μM). A relaxation equal to or greater than 90% represented functional integrity of the endothelium. At the plateau contraction, a single dose of 2 × 10–6 M ACh was given to test the endothelial integrity of each isolated aortic ring. The rings with relaxation less than 85% were discarded and the rings without endothelium relaxed at most 10% or even contracted. Another situation in which the ring was discarded was when the response varied more than two deviations from the Gaussian curve.
After a 45-min washout period, phenylephrine concentration–response curves were generated. One single concentration–response curve was generated for each segment.
After 30 min, cumulative concentration–response curves were generated for phenylephrine (0.1 nM to 300 μM). In other experiments, the phenylephrine concentration–response curve was established using endothelium-denuded rings. The endothelium was mechanically removed. Endothelium removal effectiveness was confirmed by the absence of the relaxation induced by ACh (10 μM) in aortas pre-contracted with phenylephrine in each group. Phenylephrine curves were generated in endothelium-intact aortic rings in the presence of a solution containing a non-specific nitric oxide synthase (NOS) inhibitor, (L-NAME; 100 μM), a nicotinamide adenine dinucleotide phosphate (NADPH) oxidase inhibitor (apocynin, 30 μM), an enzymatic superoxide anion scavenger (SOD, 150 U/ml), a scavenger of hydrogen peroxide (catalase, 1000 U/ml), a superoxide anion scavenger (tiron, 1 mM), and a selective inhibitor of xanthine oxidase (allopurinol, 100 μM).
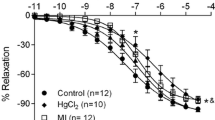
In another set of experiments following the 45-min stabilization period, aortic rings were incubated with phenylephrine (1 μM) until a plateau was reached (approximately 15 min), and the responses to ACh (0.01 nM to 30 μM) or SNP (0.01 nM to 30 μM) were observed in both groups.
Measurement of reactive oxygen species generation in the aortic wall
O2 − levels were detected in aortic artery cryosections (8 μm) in the presence or absence of the mechanically removed endothelium. A Tissue-Tek (no. 4589, Sakura Finetek, CA, USA)-optimized cutting temperature medium was allowed to thaw and was then incubated with 2 μM dihydroethidium (DHE) and an O2 −-sensitive fluorescent dye at 37 °C for 30 min in the dark (Merlo et al. 2016). Images were analyzed using a confocal fluorescence microscope (Leica DM 2500) at 585 nm. The signal intensity was measured in the whole circumference of three sections in the vessel in a blinded experiment. For quantification, 8–10 frozen tissue segments per animal were used from five animals per treatment group. The fluorescence was calculated using ImageJ software (Life Technologies, Rockville, MD).
Histomorphometry
A histomorphometric image analysis system was used with a digital camera (Axio-Cam ERc 5S) coupled to a light microscope (Olympus AX70; Olympus, Center Valley, PA). High-resolution images (2048 × 1536 pixels) were captured using Carl Zeiss AxioVision Rel. 4.8. Photomicrographs and were analyzed using a ×20 objective. The aortic wall thickness (which included all vascular tunicas/field) was calculated using ImageJ software. The thickness and area of the aortic wall were expressed as the mean ± SEM. Were used from 5 animals per treatment group.
Collagen density surface
Picrosirius red-stained aorta sections were used to obtain 15 aortic tissue photomicrographs with a ×20 objective lens. All areas analyzed were randomly chosen, and areas without vascular tunics were avoided. Were used from 5 animals per treatment group. The images were converted to high-contrast black and white images to visualize stained collagen fibers and analyzed with ImageJ software. The results represent the relative amount of collagen in the aortic wall and are expressed as the mean ± SEM as previously described (dos Santos et al. 2012).
Scanning electron microscopy
Aortas from control and TBT rats were collected, washed, opened longitudinally for 10 min with PBS, and fixed with 2.5% glutaraldehyde. The aortas were then post-fixed in 1% osmium tetroxide, 3.8% potassium ferricyanide, and 2.5 mM CaCl2, dehydrated in acetone and embedded in Epon 812. Ultra-thin sections were examined under a Zeiss EM 10C microscope. For scanning electron microscopy, spheroids were dried using the critical point method and coated with a 20-nm layer of gold and examined under a Zeiss 940 DSM microscope (dos Santos et al. 2012). Were used from 4 animals per treatment group.
Statistical analyses
Contractile responses are presented as a percentage of maximum response to 75 mM KCl. Relaxation responses to ACh and SNP were shown as a percentage of relaxation of the maximum contractile response. For each concentration–response curve, the maximum effect (Emax) and the concentration of the agonist that produced 50% of the maximal response (log EC50) were calculated using non-linear regression analysis (GraphPad Prism Software, USA). The agonist efficiency was reported as pD2 (− log EC50). The results are represented as the mean ± SEM. Comparisons between experimental groups were analyzed using Student’s t test (unpaired), and p ≤ 0.05 was considered significant. To compare the effects of the drugs on the contractile responses to phenylephrine, the data were reported as the differences in the area under the concentration–response curve (dAUC) to phenylephrine between the control and experimental conditions. dAUC was calculated from the individual curve plots (GraphPad Prism Software), and the difference was reported as a percentage of the dAUC of the corresponding control condition.
Morphometric analyses were also reported as the mean ± SEM. The data were tested for normality using Kolmogorov–Smirnov tests. Comparisons between groups were also performed using Student’s t test (unpaired), as described above. The results were considered significant at p < 0.05. The measurement of ROS generation in the aorta was reported as the mean ± SEM. The results were tested using a one-way ANOVA and Tukey’s post-test.
Results
Serum 17β-estradiol (E2) and TBARS levels
The TBT group displayed a significant decrease in serum E2 levels compared with the control group (control: 35.10 ± 4.5; TBT: 20.6 ± 1.8 pg/ml, n = 5, p < 0.05).
Furthermore, exposure to TBT for 15 days resulted in a significant increase in aortic wall lipid peroxidation as demonstrated by the TBARS assay (control: 7.53 ± 1.26; TBT: 12.33 ± 0.81, n = 3–5 nM/mg protein, p < 0.05).
Tributyltin exposure on aortic
The contractility response to 75 mM KCl was significantly increased in the TBT group compared with the control group (control: 2.34 ± 0.06 g; TBT: 3.48 ± 0.17 g, n = 10, p < 0.05). The contractility responses induced by phenylephrine were also increased in the TBT group compared with the control group (Emax, control: 104.6 ± 4.36; TBT: 151.3 ± 9.15, n = 10, p < 0.05; pD2, control: − 6.33 ± 0.09; TBT: − 6.98 ± 0.09, n = 10, p < 0.05, Fig. 1a). The endothelium-dependent relaxation induced by ACh was significantly reduced in the TBT compared with the control group (Emax, control: − 105.3 ± 0.15%; TBT: 91.26 ± 0.92%, n = 10; pD2, control: − 6.07 ± 0.01, n = 10; TBT: − 5.79 ± 0.02, n = 10, p < 0.05, Fig. 1b). The endothelium-independent relaxation induced by SNP was also reduced in the TBT compared with the control group (Emax, control: − 99.37 ± 1.65, n = 9; TBT: − 80.68 ± 2.78%, n = 10; pD2, control: − 7.64 ± 0.08, n = 9; TBT: 3.63 ± 0.57, n = 10; p < 0.05, Fig. 1c).
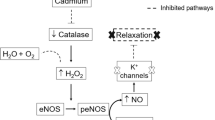
Vasoconstriction and the role of NO in vascular responses
The influence of the endothelium on the vasoconstrictor effect to phenylephrine was investigated in aortic rings following endothelial removal. Endothelial removal increased the phenylephrine responses in both groups, but this increase was significantly greater in the TBT group by 1.6-fold (Fig. 2a, b) as shown by dAUC values (control = 65.1 ± 5.7 vs. TBT = 105.4 ± 12.9 01%, p < 0.01) (Fig. 2c). To determine whether TBT exposure altered the NO-induced modulation of phenylephrine-induced contractile responses, aortic rings were incubated with the NOS inhibitor L-NAME (100 μM). The NO-induced modulation of the phenylephrine response was increased in the aortic rings of the TBT group (Fig. 2d, e). In the presence of L-NAME, the phenylephrine concentration–response curves shifted to the left in both groups, but this effect was greater in the TBT group than in the control group as shown by the dAUC values (Fig. 2f). The results suggested that the negative endothelial modulation was larger in the TBT group.
Effects of 15 days of exposure to 0.5 μg/Kg TBT on the NO-mediated vascular response in aortic arteries. The effect of the endothelial removal (E−) on the concentration–response curve of phenylephrine in a control and b TBT aortic rings. c A comparison of the percent difference (area under the curve). d The effect of a NOS blocker (L-NAME) on the concentration–response curve of phenylephrine in rat aortic rings from control and e TBT rats. f A comparison of the percent difference (area under the curve). Symbols represent the mean ± SEM. * pD2 and # Emax with p < 0.05, unpaired t test, n = 7–9
Reactive oxygen species production and the participation of reactive oxygen species in vascular responses
Apocynin (Fig. 3a, b) and tiron (Fig. 3d, e) significantly reduced vascular reactivity in the aortas of the TBT group, as shown by the dAUC values (apocynin, control = 44.7 ± 7.2 vs. TBT = 72.7 ± 4.1% (1.6-fold) p < 0.05 and tiron, control = 14.0 ± 3.0 vs. TBT = 65.2 ± 4.1%, p < 0.0001 (4.4-fold)) (Fig. 2c–f). Incubation with SOD (Fig. 3g) reduced vascular reactivity only in the TBT group, whereas catalase (Fig. 3j–l) reduced vascular reactivity in both experimental groups. However, this effect was significantly greater in the TBT group (control = 14.0 ± 6.4 vs. TBT = 48.3 ± 3%, p < 0.0003 (3.4-fold) (Fig. 3m). Incubation with allopurinol increased vascular reactivity only in the TBT group by 5.0-fold (control = 6.3 ± 4.5 vs. TBT = 31.7 ± 4.1%, p < 0.001) (Fig. 3n–p).
ROS effects on phenylephrine-induced contraction in aortic rings. Apocynin (specific NADPH oxidase inhibitor) effects in the a control and b TBT groups. c A comparison of the percent difference (area under the curve). Effects of tiron (superoxide anion scavenger) in the d control and e TBT groups. f A comparison of the percent difference (area under the curve). SOD (superoxide anion scavenger) effects in the g control and h TBT groups. i A comparison of the percent difference area under the curve. Effects of catalase (hydrogen peroxide scavenger) in the j control and l TBT groups. m A comparison of the percent difference (area under the curve). Effects of allopurinol (selective inhibitor of xanthine oxidase) in the n control and o TBT groups. p A comparison of the percent difference area under the curve represented as the mean ± SEM, n = 8–9. * pD2 and # Emax with p < 0.05, unpaired t test
Aorta superoxide anion detection
The O2− level in the aorta was detected using the O2−-sensitive fluorescent dye DHE. The signal strength in the aorta was significantly higher for the TBT group in the presence (E+) (Fig. 4B–B1) and absence of the endothelium (E−) (Fig. 4D–D1) when compared with the control group also in the presence (Fig. 4A–A1) or absence of endothelium (Fig. 4C–C1) (p < 0.01).
Superoxide anion production in the aortic ring in the (A and A1) control and (B1 and B2) TBT groups with the endothelium and (C and C1) the control and (D and D2) TBT groups without the endothelium. Fluorescence labeling with the oxidative dye hydroethidine and vascular superoxide anion. Symbols represent the mean ± SEM. **p < 001, one-way ANOVA
Vascular atrophy and collagen density
The aortic rings were atrophied 15 days after TBT exposure. The thickness of the aortic wall was significantly decreased in the TBT group compared with the control group (control: 133.24 ± 5.29 μm; TBT: 87.29 ± 0.75 μm, n = 5, p < 0.05, Fig. 5a–c). In addition, the development of fibrotic processes was assessed in the control and TBT groups. Collagen deposition in the aortas was significantly higher in the TBT group than in the control group, as shown by the Picrosirius red staining (control: 84.27 ± 2.32; TBT: 103.87 ± 1.93, n = 5, p < 0.001, Fig. 5d–f).
Photomicrography of H&E-stained aortic ring sections from control and TBT (0.5 μg/kg) female Wistar rats treated for 15 days. a Aortic ring section from control rats showing normal morphology. b Aortic ring section from the TBT group showing signs of vascular atrophy. c Aorta wall thickness (mean ± SEM). Representative image of collagen density in the control group (d) and the TBT group (e). Collagen surface density (mean ± SEM) with an increase in the aortic wall area from the TBT group (f). ***p < 0.001 vs. control. Bar = 50 μm
Aorta ultrastructure
Scanning electron microscopy (SEM) of rat aortic arteries revealed that the endothelial surface of the control group had a normal squamous appearance (Fig. 6A). TBT exposure denuded the surface endothelium in the rat aorta (Fig. 6B–B2) leading to an irregular aortic endothelium surface with an accumulation of red blood cells with platelets and fibrin on the denuded endothelial surface (Fig. 6B2).
SEM photomicrographs showing the endothelial surface of control rat aortas with a normal squamous appearance (A). TBT rats exhibited a denuded surface endothelium in the rat aortic artery (asterisk), leading to an irregular surface in the aortic endothelium with an accumulation of red blood cells, platelets and fibrin on the denuded endothelial surface (arrow) (B, B1, and B2). (Arrowhead: endothelial cell, Bar = 10 μm)
Discussion
Results of the current study showed that oral exposure of female rats for 15 days to the ADI of TBT of 0.5 μg/kg/day/bw recommended by the WHO (IPCS 1999a) lead to significant aortic vascular abnormalities such as increased vasoconstrictor responsivity and decreased, both endothelium-dependent and independent, vasorelaxation. Additionally, our results demonstrated an increased endothelial release of NO as well as a reduction in NO bioavailability and greater free radical production. Irregular morphology of aortic rings was also observed after exposure to TBT showing increases in collagen density and a denuded endothelial surface and fibrin accumulation.
Several studies have reported that E2 acts by regulating vascular function in both the vascular smooth muscle cells and endothelial cells, inducing cardiovascular protection of the vessel wall (Cheng et al. 1994; Barbacanne et al. 1999; Tostes et al. 2003). E2, an ovarian steroid hormone, modulates the vascular mechanisms responsible for endothelium-dependent relaxation and contraction (Cheng et al. 1994; Ceravolo et al. 2012). Ceravolo (2012) reported that E2 replacement reduced the O2 − production in ovariectomized rats, leading to improvement in aortic reactivity. Other studies showed that an imbalance in oxidative stress impairs aortic vascular reactivity (Sagredo et al. 2013; Camporez et al. 2011). Similarly, we previously reported exposure of rats to a lower TBT dose (100 ng/kg/day/bw) reduced plasma E2 levels by 32% compared with control group rats (Rodrigues et al. 2014). Consistent with these findings, the present study showed a 38% reduction in E2 serum levels in TBT-treated rats. It is possible that the reduction in E2 could be associated with an impairment in aortic reactivity in our model.
The reaction of free radicals with cell membrane lipids (Janieck et al. 1985; Janero and Burghardt 1989) has been shown to inactivate membrane-bound receptors and enzymes, to increase membrane permeability of several tissues, and to have the potential to damage cells (Poli et al. 1985; Janero and Burghardt 1989). Rakesh et al. (1996) reported an increase in lipid peroxidation in aortas in a diabetic rat model as shown by increased TBARS levels. A dose-dependent increase in brain TBARS levels was observed after 7 days of TBT exposure to a single dose of 10, 20, and 30 mg/kg (Mitra et al. 2015). Consistent with these previous findings, our data revealed higher levels of TBARS in aortic tissues sub-chronically exposed to low concentrations of TBT. Thus, this elevated oxidative stress in aortic tissue could be attributed to exposure to TBT in female rats.
The aorta is a conductance artery, and regulation of its vascular tone is attributed to several factors (Furchgott 1983; Hutchinson et al. 1987; Vanhoutte 1988). Environmental factors also play a role, and epidemiological and experimental studies have suggested a connection between exposure to metal components in the environment and vascular dysfunction (Wiggers et al. 2008; Fiorim et al. 2012; Almenara et al. 2013; Rodrigues et al. 2014). However, to date, few studies have demonstrated the effects of OT on the regulation of aortic reactivity (Solomon and Krishnamurty 1992; Ally et al. 1993; Rodrigues et al. 2014).
Our present findings show that the aortic arteries of TBT-treated rats exhibited a higher contractility response to 75 mM KCl and to phenylephrine. Additionally, increased oxidative stress was observed in TBT rats. Thus, abnormal vascular function in TBT-treated rats could be associated with an increase in oxidative stress caused by TBT. The relaxation induced by ACh and SNP was reduced in TBT-exposed aortic rings in our study. It has been demonstrated that a reduction in ACh-induced relaxation in aortic vessels could be a risk factor associated in cardiovascular disease, such as myocardial infarction (Sartório et al. 2005) and arterial hypertension (Cai and Harrison 2000). Moreover, when comparing the magnitudes of the responses of aortic rings with and without endothelium and after L-NAME treatment, our findings showed that the magnitude of the response increased in the TBT group. These results suggest that the ability of the endothelium to modulate the contractile response induced by phenylephrine was preserved and enhanced regardless of the exposure to TBT. However, ACh- and SNP-induced relaxations were reduced in the TBT group even under an increased NO-dependent negative endothelial modulation.
Our results suggested that at least two factors may be responsible for this phenomenon. The increased oxidative stress in the TBT-treated group without endothelium and increased collagen density may explain our results. Previous studies reported a relationship between increased oxidative stress and collagen production leading to impairment of vascular function, which supports our finding (Wu et al. 2016; Stephen et al. 2014; Chen et al. 2013).
As shown in previous studies, vascular endothelial cells generate NO from the amino acid l-arginine, which induces a relaxation response (Hutchinson et al. 1987). In the current study, after incubation with L-NAME, we also observed that the magnitude of response was higher in aortic rings from the TBT group. Thus, these data suggest an important role for vascular NO as a compensatory mechanism for the increase in the vasoconstrictor pathway activated by TBT. Other cardiovascular studies performed by our group have shown abnormal NO function and/or production after TBT exposure (dos Santos et al. 2012; Rodrigues et al. 2014; Ribeiro Junior et al. 2016).
However, ACh-induced relaxation was reduced in the TBT-treated aortic rings. Several studies have demonstrated that exposure to TBT generates oxidative stress and ROS followed by oxidative vascular damage (Ishihara et al. 2012; Kato et al. 2013; Isomura et al. 2013; Mitra et al. 2015, Rodrigues et al. 2014). NADPH oxidase is the major source of ROS in the vasculature, producing superoxide anions from oxygen using NADPH oxidase as the electron donor (Guzik et al. 2000b). In our study, after incubation with apocynin, the response to phenylephrine was lower in TBT rats compared with control rats, and this could be related to an increase in local NADPH oxidase activity. Similarly, increased superoxide anion production was observed in the mesenteric resistance arteries of TBT rats (Ribeiro Junior et al. 2016).
Similarly, our data showed an increase in ROS production in the TBT-treated aortic rings (see Fig. 4). In addition, SOD, allopurinol, tiron, and catalase all reduced the vasoconstrictor response induced by phenylephrine in the aortas of TBT-treated rats. These findings suggested that the superoxide anions produced by NADPH oxidase and xanthine oxidase and hydrogen peroxide were associated with vascular abnormalities as a result of TBT exposure. In addition, we evaluated the local production of ROS, with and without the endothelium, using a DHE assay. In the presence of intact endothelium, the fluorescence intensity signal in the middle layer was higher in the aortas from the TBT group than that in the aortas of the control group. There was no difference in the fluorescence intensity signal between the rings with or without endothelium suggesting that TBT increased local production of O2 − levels in the aorta and could induce aortic wall and smooth muscle changes. One other study performed by our group showed a higher O2 − level in pituitary and adrenal glands after TBT exposure, leading to apoptosis and fibrosis (Merlo et al. 2016).
Several studies have reported that metabolic diseases or xenobiotic exposure could lead to morphological abnormalities of the aorta (Yoshizuka et al. 1992; Aguado et al. 2013; Díaz et al. 2013; Rodrigues et al. 2014). In diabetic rats, morphological irregularities in the aortic arteries were observed, including increased aortic wall thickness and perivascular fibrosis and collagen deposition with fragmentation and disarray of the elastic fibers (Ti et al. 2015). Yoshizuka et al. (1992) observed morphological alterations in the rat aortic artery as marked by swelling of the mitochondria in endothelial cells 4 h after exposure to TBT oxide (0.05 mL/kg). In addition to these previous findings, our results also showed aortic morphological damage. We observed atrophy of the aortic wall, increased collagen deposition, and an irregular endothelial surface as well as an accumulation of red blood cells, platelets, fibrin, and signs of vascular inflammation. These data suggest that TBT produces aortic morphological damage related to vascular dysfunction development. In summary, our results showed that 15 days of exposure to 0.5 μg/kg TBT induced significant vascular abnormalities. This exposure dose is less than the provisional maximum tolerable daily dose for tin of 2 mg/kg bw and the provisional tolerable weekly intake of 14 mg/kg bw as determined by the Joint FAO-WHO Expert Committee on Food Additives. Furthermore, it is less than the TDI of 5 or 0.25 mg/kg bw, which has been described to reduce lymphoid organ weights and thymus, or lymphoid function (Penninks 1993).
Oxidative stress and vascular reactivity to phenylephrine increased, the relaxation induced by ACh and SNP decreased, and abnormalities were produced by oxidative stress. Moreover, these vascular dysfunctions were also related to morphological abnormalities in the aortic wall, such as signs of vascular atrophy, denudation of the endothelium, and increased collagen deposition.
The relevance of this study is based in the fact that female rat exposure to a TBT dose, referred as the ADI by WHO, which is based on a 200-fold multiplication of the NOAEL (0.1 mg/kg/day/bw), induced an important vascular dysfunction in aortic rings. The exposure to TBT by food consumption, ingestion of contaminated soil and sediments, and inhalation and dermal absorption in the environment could be a risk to human health.
In conclusion, this study demonstrated that female rat exposure to TBT 0.5 μg/kg bw/day for 15 days, presented functional and morphological dysfunction of aortic rings as a result of increased oxidative stress and fibrosis and should be considered an important cardiovascular risk factor.

References
Aguado A, Galán M, Zhenyukh O, Wiggers GA, Roque FR, Redondo S, Peçanha F, Martín A, Fortuño A, Cachofeiro V, Tejerina T, Salaices M, Briones AM (2013) Mercury induces proliferation and reduces cell size in vascular smooth muscle cells through MAPK, oxidative stress and cyclooxygenase-2 pathways. Toxicol Appl Pharm 268(2):188–200
Ally A, Buist R, Mills P, Reuhl K (1993) Effects of methylmercury and trimethyltin on cardiac, platelet, and aorta eicosanoid biosynthesis and platelet serotonin release. Pharmacol Biochem Be 44(3):555–563
Almenara CCP, Broseghini-Filho GB, Vescovi VAV, Angeli JK, Faria TO, Stefanon I, Vassallo DV, Padilha AS (2013) Chronic cadmium treatment promotes oxidative stress and endothelial damage in isolated rat aorta. PLoS One 8(7):e68418
Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, Selwyn AP (1995) Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol 26(5):1235–1241
Antizar-Ladislao B (2008) Environmental levels, toxicity and human exposure to tributyltin (TBT)-contaminated marine environment. Environ Int 34(2):292–308
Barbacanne MA, Rami J, Michel JB, Souchard JP, Philippe M, Besombes JP, Bayard F, Arnal JF (1999) Estradiol increases rat aorta endothelium-derived relaxing factor (EDRF) activity without changes in endothelial NO synthase gene expression: possible role of decreased endothelium-derived superoxide anion production. Cardiovasc Res 41(3):672–681
Bo E, Farinetti A, Marraudino M, Sterchele D, Eva C, Gotti S, Panzica G (2016) Adult exposure to tributyltin affects hypothalamic neuropeptide Y, Y1 receptor distribution, and circulating leptin in mice. Andrology 4(4):723–734
Bryan GW, Gibbs PE, Hummerstone LG, Burt GR (1986) The decline of the gastropod Nucella lapillus around South-West England: evidence for the effect of tributyltin from antifouling paints. J Mar Biol Assoc UK 66:611–640
Cai H, Harrison DG (2000) Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res 87(10):840–844
Camporez JP, Akamine EH, Davel AP, Celso, Franci CR, Rossoni LV, Carvalho CRO (2011) Dehydroepiandrosterone protects against oxidative stress-induced endothelial dysfunction in ovariectomized rats. J Physiol 589(10):2585–2596
Ceravolo GS, Filgueira FP, Costa TJ, Lobato NS, Chignalia AZ, Araujo PX, Tostes RC, Dantas AP, Fortes ZB, Carvalho MH (2012) Conjugated equine estrogen treatment corrected the exacerbated aorta oxidative stress in ovariectomized spontaneously hypertensive rats. Steroids 78(3):341–346
Chen QZ, Han WQ, Chen J, Zhu DL, Chen-Yan GPJ (2013) Anti-stiffness effect of apocynin in deoxycorticosterone acetate-salt hypertensive rats via inhibition of oxidative stress. Hypertens Res 36:306–312
Cheng DY, Feng CJ, Kadowitz PJ, Gruetter CA (1994) Effects of 17 beta-estradiol on endothelium-dependent relaxation induced by acetylcholine in female rat aorta. Life Sci 55(10):PL187–PL191
Cooke GM (2006) Toxicology of tributyltin in mammalian animal models. Immunol, Endocr Metab Agents Med Chem 6:63–71
Costa MB, Zamprogno GC, Pedruzzi FC, Morais L, Tognella MMP, Godoi AFL, Santos DM, Marchi MRR, Fernandez MA (2014) Differential organotionsensitivy in two Leucozonia species from a ship traffic area southeastern Brazil. Mar Biol Res 10(7):712–724
Coutinho JV, Freitas-Lima LC, Freitas FF, Freitas FP, Podratz PL, Magnago RP, Porto ML, Meyrelles SS, Vasquez EC, Brandão PA, Carneiro MT, Paiva-Melo FD, Miranda-Alves L, Silva IV, Gava AL, Graceli JB (2016) Tributyltin chloride induces renal dysfunction by inflammation and oxidative stress in female rats. Toxicol Lett 260(1):52–69
Díaz MFFP, Acosta M, Mohamed FH, Ferramola ML, Oliveros LB, Gimenez MS (2013) Protective effect of soybeans as protein source in the diet against cadmium-aorta redox and morphological alteration. Toxicol Appl Pharm 272(3):806–815
dos Santos RL, Podratz PL, Sena GC, Delgado Filho VS, Lopes PFI, Gonçalves WLS, Alves LM, Samoto VY, Takiya CM, Miguel EC, Moyses MR, Graceli JB (2012) Tributyltin impairs the coronary vasodilation induced by 17 beta-estradiol in the isolated rat heart. J Toxicol Env Heal A 75(16–17):1–13
dos Santos DM, Turra A, de Marchi MR, Montone RC (2016) Distribution of butyltin compounds in Brazil’s southern and southeastern estuarine ecosystems: assessment of spatial scale and compartments. Environ Sci Pollut Res Int 23(16):16152–16163
European Food Safety Authority (2004) Opinion of the scientific panel on contaminants in the food chain on a request from the Commission to assess the health risks to consumers associated with exposure to organotins in foodstuffs. EFSA J 102(1):1–119
Fiorim J, Júnior RFR, Azevedo BF, Simões MR, Padilha AS, Stefanon I, Alonso MJ, Salaices M, Vassallo DV (2012) Activation of K+ channels and Na+/K+ ATPase prevents aortic endothelial dysfunction in 7-day lead-treated rats. Toxicol Appl Pharm 262(1):22–31
Furchgott RF (1983) Role of endothelium in responses of vascular smooth muscle. Circ Res 53(5):557–573
Galloway TS (2006) Biomarkers in environmental and human health risk assessment. Mar Pollut Bull 53(10–12):606–613
Guzik TJ, West NE, Black E, McDonald D, Ratnatunga C, Pillai R, Channon KM (2000) Vascular superoxide production by NAD(P)H oxidase: association with endothelial dysfunction and clinical risk factors. Circ Res 86(9):E85–E90
Hartwell SI, Apeti DA, Mason AL, Pait AS (2016) An assessment of butyltins and metals in sediment cores from the St. Thomas East End Reserves, USVI. Environ Monit Assess 188(11):642
Hermes-Lima M, Willmore WG, Storey KB (1995) Quantification of lipid peroxidation in tissue extracts based on Fe(III)xylenol orange complex formation. Free Radical Bio Med 19(3):271–280
Hoch M (2001) Organotin compounds in the environment—an overview. Appl Geochem 16:719–743
Hutchinson PJ, Palmer RM, Moncada S (1987) Comparative pharmacology of EDRF and nitric oxide on vascular strips. Eur J Pharmacol 141(3):445–451
IPCS (1999) Concise international chemical assessment documents, no.13, Triphenyltin compounds, World Health Organization, Geneva
Ishihara Y, Kawami T, Ishida A, Yamazaki T (2012) Tributyltin induces oxidative stress and neuronal injury by inhibiting glutathione S-transferase in rat organotypic hippocampal slice cultures. Neurochem Int 60(8):782–790
Isomura M, Kotak Y, Masuda K, Miyara M, Okuda K, Samizo S, Sanoh S, Hosoi T, Ozawa K, Ohta S (2013) Tributyltin-induced endoplasmic reticulum stress and its Ca2+−mediated mechanism. Toxicol Appl Pharm 272(1):137–146
Janero DR, Burghardt B (1989) Thiobarbituric acid-reactive malondialdehyde formation during superoxide-dependent, iron-promoted lipid peroxidation: influence of peroxidation conditions. Lipids 24(2):125–131
Janieck MF, Haseltine WA, Henner WD (1985) Malondialdehyde precursors in gamma-irradiated DNA, deoxynucleotides, deoxynucleosides. Nucleic Acids Res 13(24):9011–9029
Kannan K, Senthilkumar K, Giesy JP (1999) Occurrence of butyltin compounds in human blood. Environ Sci Technol 33(10):1776–1779
Kato T, Tada-Oikawa S, Wang L, Murata M, Kuribayashi K (2013) Endocrine disruptors found in food contaminants enhance allergic sensitization through an oxidative stress that promotes the development of allergic airway inflammation. Toxicol Appl Pharm 273(1):10–18
Kinlay S, Ganz P (1997) Role of endothelial dysfunction in coronary artery disease and implications for therapy. Am J Cardiol 80(9A):11I–16I
Konstantinou IK, Albanis TA (2004) Worldwide occurrence and effects of antifouling paint booster biocides in the aquatic environment: a review. Environ Int 30(2):235–248
Kotrikla A (2009) Environmental management aspects for TBT antifouling wastes from the shipyards. J Environ Manag 90:77–85
Ma FX, Liu LY, Xiong XM (2003) Protective effects of lovastatin on vascular endothelium injured by low density lipoprotein. Acta Pharmacol Sin 24(10):1027–1032
Merlo E, Podratz PL, Sena GC, de Araújo JF, Lima LC, Alves IS, Gama-de-Souza LN, Pelição R, Rodrigues LC, Brandão PA, Carneiro MT, Pires RG, Martins-Silva C, Alarcon TA, Miranda-Alves L, Silva IV, Graceli JB (2016) The environmental pollutant tributyltin chloride disrupts the hypothalamic-pituitary-adrenal axis at different levels in female rats. Endocrinology. https://doi.org/10.1210/en.2015-1896
Mitra S, Siddiqui WA, Khandelwal S (2015) Differential susceptibility of brain regions to tributyltin chloride toxicity. Environ Toxicol 30(12):1393–1405
Morton B (2009) Recovery from imposex by a population of the dogwhelk, Nucella lapillus (Gastropoda: Caenogastropoda), on the southeastern coast of England since May 2004: a 52-month study. Mar Pollut Bull 58:1530–1538
Nakanishi T (2007) Potential toxicity of organotin compound via nuclear receptor signalling in mammals. J Health Sci 53(1):1–9
Nielsen JB, Strand J (2002) Butyltin compounds in human liver. Environ Res 88(2):129–133
Penninks AH (1993) The evaluation of data-derived safety factors for bis (tri-n-butyltin) oxide. Food Addit Contam 10(3):351–361
Poli G, Dianzani MU, Cheeseman KH, Staler TF, Lang J, Esterbauer H (1985) Separation and characterization of the aldehydic products of lipid peroxidation stimulated by carbon tetrachloride or ADP-iron in isolated rat hepatocytes and rat liver microsomal suspensions. Biochem J 227(2):629–638
Rakesh K, Subrahmanyam VM, Jawahar K, Kailash P (1996) Time course study of oxidative stress in aorta and heart of diabetic rat. Clin Sci 91(4):441–448 (Printed in Great Britain)
Ribeiro Junior RF, Marques VB, Nunes DO, Ronconi Kde S, de Araújo JF, Rodrigues PL, Padilha AS, Vassallo DV, Graceli JB, Stefanon I (2016) Tributyltin chloride increases phenylephrine-induced contraction and vascular stiffness in mesenteric resistance arteries from female rats. Toxicol Appl Pharmacol 295(1):26–36
Rodrigues SML, Ximenes CF, Batista PR, Simões FV, Coser PHP, Sena GC, Podratz PL, Souza LNG, Vassallo DV, Graceli JB, Stefanon I (2014) Tributyltin contributes in reducing the vascular reactivity to phenylephrine in isolated aortic rings from female rats. Toxicol Lett 225(3):378–385
Sagredo A, Campo L, Martorell A, Navarro R, Martín MC, Rivero JB, Ferrer M (2013) Ovariectomy increases the participation of hyperpolarizing mechanisms in the relaxation of rat aorta. PLoS One 8(9):e73474
Sartório CL, Pinto VD, Cutini S, Vassallo DV, Stefanon I (2005) Effects of inducible nitric oxide synthase inhibition on the rat tail vascular bed reactivity three days after myocardium infarction. J Cardiovasc Pharmacol 45(4):321–326
Solomon R, Krishnamurty V (1992) The effect of tributyltin chloride on vascular responses to atrial natriuretic peptide. Toxicology 76(1):39–47
Sorensen KE, Celermajer DS, Georgakopoulos D, Hatcher G, Betteridge DJ, Deanfield JE (1994) Impairment of endothelium-dependent dilation is an early event in children with familial hypercholesterolemia and is related to the lipoprotein (a) level. J Clin Invest 93(1):50–55
Stephen EA, Venkatasubramaniam A, Good TA, Topoleski LD (2014) The effect of oxidation on the mechanical response and microstructure of porcine aortas. J Biomed Mater Res A 102:3255–3262
Takahashi S, Mukai H, Tanabe S, Sakayama K, Miyazaki T, Masuno H (1999) Butyltin residues in livers of humans and wild terrestrial mammals and in plastic products. Environ Pollut 106(2):213–218
Ti Y, Xie G, Wang Z, Ding W, Zhang Y, Zhong M, Zhang W (2015) Tribbles 3: a potential player in diabetic aortic remodeling. Diabetes Vas Dis Re 13(1):69–80
Tostes RC, Nigro D, Fortes ZB, Carvalho MHC (2003) Effects of estrogen on the vascular system. Braz J Med Biol Res 36(9):1143–1158
Vanhoutte PM (1988) The endothelium-modulator of vascular smooth-muscle tone. N Engl J Med 319(8):512–513
Wiggers GA, Peçanha FM, Briones AM, Pérez-Girón JV, Miguel M, Vassallo DV, Cachofeiro V, Alonso MJ, Salaices M (2008) Low mercury concentrations cause oxidative stress and endothelial dysfunction in conductance and resistance arteries. Am J Physiol Heart Circ Physiol 295:H1033–H1043
Whalen MM, Loganathan BG, Kannan K (1999) Immunotoxicity of environmentally relevant concentrations of butyltins on human natural killer cells in vitro. Environ Res 81(2):108–116
WHO (1999) Concise international chemical assessment document, IPCS-Report No. 14, Tributyltin oxide, World Health Organization, Geneva
Wu J, Saleh MA, Kirabo A, Itani HA, Montaniel KR, Xiao L, Chen W, Mernaugh RL, Cai H, Bernstein KE, Goronzy JJ, Weyand CM, Curci JA, Barbaro NR, Moreno H, Davies SS, Roberts LJ, Madhur MS, Harrison DG (2016) Immune activation caused by vascular oxidation promotes fibrosis and hypertension. J Clin Invest 126(1):50–67
Yoshizuka M, Hara K, Doi Y, Mori N, Yokoyama M, Ono E, Fujimoto S (1992) The toxic effects of bis (tributyltin) oxide on the rat thoracic aorta. Histol Histopathol 7(3):445–449
Zuo Z, Chen S, Wu T, Zhang J, Su Y, Chen Y, Wang C (2011) Tributyltin causes obesity and hepatic steatosis in male mice. Environ Toxicol 26(1):79–85
Acknowledgements
This study was supported by “Coordenação de Aperfeiçoamento de Pessoal de Nível Superior” (CAPES), “Conselho Nacional de Desenvolvimento Científico e Tecnológico” (CNPq 201806/2015-0-455294/2014-3) and “Fundação de Amparo à Pesquisa do Espírito Santo” (FAPES no. 0609-2015) in Brazil. We thank the Laboratory of Cellular Ultrastructure-UFES (grant: MCT/FINEP/CT-INFRA—PROINFRA 01/2006) for the development of the SEM protocols; the Laboratory of Molecular Histology and Immunohistochemistry at UFES for the development of the DHE protocols; and the Laboratory of Biochemistry and Molecular Biophysics of Proteins at UFES for the development of the TBARS protocols. We thank Scott Holt for checking and improving the use of the English language in the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Responsible editor: Markus Hecker
Rights and permissions
About this article
Cite this article
Ximenes, C.F., Rodrigues, S.M.L., Podratz, P.L. et al. Tributyltin chloride disrupts aortic vascular reactivity and increases reactive oxygen species production in female rats. Environ Sci Pollut Res 24, 24509–24520 (2017). https://doi.org/10.1007/s11356-017-0061-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-017-0061-8