Abstract
Links between environmental chemicals and human health have emerged over the last few decades, but the effects from polyaromatic hydrocarbons were less studied, compared to other commonly known environmental chemicals such as heavy metals, phthalates, arsenic, phenols and pesticides. Therefore, it was aimed to study the relationships of urinary polyaromatic hydrocarbons and adult cardiovascular disease and cancer using human sample in a national and population-based study in recent years. Data was retrieved from US National Health and Nutrition Examination Surveys, 2011–2012, including demographics, self-reported health conditions and urinary polyaromatic hydrocarbons. Statistical analyses included chi-square test, t test, survey-weighted logistic regression modeling and population attributable risk (PAR) estimation. Of 5560 American adults aged 20–80 and included in the statistical analysis, urinary polyaromatic hydrocarbons (representatively in one-third sample) were observed to be higher in people with cardiovascular disease and total cancer. In particular, urinary 4-hydroxyphenanthrene was associated with hypertension (odds ratio (OR) 1.33, 95 % confidence interval (CI) 1.00–1.76, P = 0.048, PAR 5.1 %), urinary 1-hydroxypyrene was significantly associated with heart attack (OR 1.47, 95 %CI 1.05–2.06, P = 0.027, PAR 1.7 %), and urinary 2-hydroxynapthalene (2-naphthol) was associated with cancer (OR 1.46, 95 %CI 1.12–1.90, P = 0.008, PAR 3.9 %). Urinary polyaromatic hydrocarbons were associated with adult hypertension, heart attack and cancer, although the causality cannot be established. From the research perspective, future studies with a longitudinal or experimental approach would be suggested. From the law and public health perspectives, regulation on minimizing exposure to polyaromatic hydrocarbons might need to be considered in future health and environmental policies and intervention programs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Links between environmental chemicals and human health in American adults including hypertension, cardiovascular disease, food allergy, oral health, emotional support and cognitive function have emerged (Shiue 2013a, b, c, 2014a, b, 2015a, b), but the effects from polyaromatic hydrocarbons (PAHs) were less studied, compared to other commonly known environmental chemicals such as heavy metals, arsenic, phenols and phthalates. PAHs constitute a group of chemicals that people could be exposed via vehicle exhausts, asphalt, coal tar, wild fires, agricultural burning, soil, charbroiled foods and tobacco smoke (Centers for Disease Control and Prevention 2012). PAH pollution may have significant health implications, and the extent of damage to organisms from PAH exposure could be dependent on several factors including degree and type of PAH exposure (Ball and Truskewycz 2013). The potential for PAHs to adversely affect human immunologic health could have traditionally been evaluated in rodents, under laboratory conditions (Luebke, et al 1997). Providing evidence from human sample might help public health promotion in the next few years. Following this context, therefore, it was aimed to examine the relationships of urinary PAHs and adult cardiovascular disease by subtypes and cancer using a large human sample in a national and population-based setting in recent years.
Methods
Study sample
As described elsewhere (Centers for Disease Control and Prevention 2012), US National Health and Nutrition Examination Surveys (NHANES) has been a national, population-based, multiyear, cross-sectional study since the 1980s. Study sample is representative of the civilian, noninstitutionalized US population. Information on demographics (more details via http://wwwn.cdc.gov/nchs/nhanes/2011-2012/DEMO_G.htm), serum cotinine (more details via http://wwwn.cdc.gov/nchs/nhanes/2011-2012/COTNAL_G.htm), and self-reported health conditions (more details via http://wwwn.cdc.gov/nchs/nhanes/2011-2012/MCQ_G.htm) was obtained by household interview using questionnaires. In the current analysis, the 2011–2012 study cohort as the most recent wave was selected. Informed consents were obtained from the participating subjects by the NHANES researchers.
Biomonitoring
Urines were only collected in a subsample within 10 days of the household interview, being one third of the whole study cohort with representation (more details via http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/homeurine.pdf), to measure environmental chemical concentrations in urines among people aged 6 and above (more details via http://www.cdc.gov/nchs/nhanes/nhanes2011-2012/labdoc_g.htm). Urine specimens from urinary polyaromatic hydrocarbon were processed, stored under appropriate frozen (−20 °C) conditions, and shipped to the Division of Environmental Health Laboratory Sciences, National Center for Environmental Health, Centers for Disease Control and Prevention, for analysis. According to the NHANES website (more details via http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/PAH_G_met.pdf), the procedure involved enzymatic hydrolysis of glucuronidated/sulfated OH-polyaromatic hydrocarbon metabolites in urine, extraction, derivatization, and analysis using isotope dilution capillary gas chromatography tandem mass spectrometry (GC-MS/MS). Ion transitions specific to each analyte and carbon-13-labeled internal standards are monitored, and the abundances of each ion are measured. Since urinary PAH concentrations were highly skewed, they were all log transformed when performing the statistical analyses.
Statistical analysis
Adults aged 20 and above were included in the current statistical analysis since chronic diseases were commonly reported in adults. Associations of urinary PAHs and adult health problems were examined by performing t test and survey-weighted logistic regression model, presenting with mean values, odds ratios (OR), and 95 % confidence intervals (CI). Covariates including urinary creatinine, age, sex, ratio of family income to poverty (proxy of socioeconomic status), body mass index, education level, serum cotinine (biomarker of smoking status), alcohol status and physical activity level were adjusted. In addition, population attributable risks from urinary PAHs, which significant associations were found, were calculated based on the formula introduced by Fleiss (1979). Statistical software Stata version 13.0 (Stata, College Station, Texas, USA) was used to perform all the analyses. Since the present study was only carrying out secondary data analysis by extracting data from the US NHANES website (more details via http://wwwn.cdc.gov/nchs/nhanes/search/nhanes11_12.aspx), no further ethics approval was required.
Results
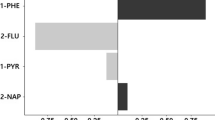
Of 5560 American adults aged 20–80 and included in the statistical analysis, their characteristics are shown in Table 1. The presence of cardiovascular disease and cancer in the American adult population varied. They are shown in Table 2. In Tables 3, 4, 5, 6, 7, 8, 9, 10, 11, and 12, associations of 10 urinary PAHs and adult cardiovascular disease and cancer are presented separately. It was observed that urinary PAHs were higher in people with cardiovascular disease and total cancer. In particular, urinary 4-hydroxyphenanthrene was associated with hypertension (OR 1.33, 95 %CI 1.00–1.76, P = 0.048, population attributable risk (PAR) 5.1 %), urinary 1-hydroxypyrene was significantly associated with heart attack (OR 1.47, 95 %CI 1.05–2.06, P = 0.027, PAR 1.7 %), and urinary 2-hydroxynapthalene (2-naphthol) was associated with cancer (OR 1.46, 95 %CI 1.12–1.90, P = 0.008, PAR 3.9 %). In addition, urinary 2-hydroxynapthalene (2-naphthol) was inversely associated with angina (OR 0.56, 95 %CI 0.33–0.95, P = 0.034).
Discussion
Previous research
Exposure to PAHs has been reported to elevate cardiovascular risk by affecting atherogenesis, thrombosis, or blood pressure regulation (O'Toole, et al 2008; Gentner and Weber 2011). Recently, it was also found that urinary 1-hydroxypyrene is associated with oxidative stress and inflammatory biomarkers in acute myocardial infarction (Freitas, et al 2014; Kraus, et al 2011; Trochimowicz, et al 1976) while 2-naphthol could be linked with lung cancer and breast cancer (Eom, et al 2013; Lee, et al 2010). Consistent with these studies, in the current analysis, adults with hypertension, heart attack and coronary heart disease had higher levels of urinary PAHs. The pathway might go from exposure to PAHs to human biomarkers leading to health conditions presenting. Also consistent with other literature, people with angina and heart failure had lower levels of PAHs (Mendis, et al 1995). However, the mechanism is unknown. As mentioned earlier, the literature on the effects of PAHs on human health is still less than that on other environmental chemicals, such as heavy metals, pesticides, arsenic, phthalates and phenols. Therefore, there is a need to further study with a longitudinal or experimental approach in future research.
Strengths and limitations
The present study has a few strengths. First, this study was conducted in a large and nationally representative human sample with mixed ethnicities and socioeconomic status. Second, this is the first time examining the risk effects of urinary PAHs on adult cardiovascular disease and cancer. Third, population attributable risks from urinary PAHs for cardiovascular disease and cancer were calculated. However, there are also a few limitations that cannot be ignored. First, there could be still other emerging chemicals from the living environments through different channels/vehicles that we might not yet know and would need future research to further identify and examine. Second, it was not possible to examine cancer by subtypes due to small number of disease events. Therefore, it is not possible to compare with the literature directly. Third, causality cannot be established in the present study due to the cross-sectional study design in nature. The significance observed in the present study could be just by chance, but the values in urine were indeed higher in people with these health conditions. Future studies with a longitudinal or experimental approach to confirm or refute the current findings and, if at all, to understand the persisting risk effects along the life course from those environmental chemicals mentioned above would be suggested.
Conclusion
In sum, urinary PAHs were positively associated with adult hypertension, heart attack and cancer while inversely associated with angina. From the research perspective, future studies with a longitudinal or experimental approach would be suggested. From the law and human health perspectives, regulation on minimizing exposure to PAHs for humans might need to be considered in future health and environmental policies and intervention programs.
References
Ball A, Truskewycz A (2013) Polyaromatic hydrocarbon exposure: an ecological impact ambiguity. Environ Sci Pollut Res Int 20:4311–4326
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (2012) [http://www.cdc.gov/nchs/nhanes.htm]
Eom SY, Yim DH, Moon SI, Youn JW, Kwon HJ, Oh HC, Yang JJ, Park SK, Yoo KY, Kim HS, Lee KS, Chang SH, Kim YD, Kang JW, Kim H (2013) Polycyclic aromatic hydrocarbon-induced oxidative stress, antioxidant capacity, and the risk of lung cancer: a pilot nested case-control study. Anticancer Res 33:3089–3097
Fleiss JL (1979) Inference about population attributable risk from cross-sectional studies. Am J Epidemiol 110:103–104
Freitas F, Brucker N, Durgante J, Bubols G, Bulcão R, Moro A, Charão M, Baierle M, Nascimento S, Gauer B, Sauer E, Zimmer M, Thiesen F, Castro I, Saldiva P, Garcia SC (2014) Urinary 1-hydroxypyrene is associated with oxidative stress and inflammatory biomarkers in acute myocardial infarction. Int J Environ Res Public Health 11:9024–9037
Gentner NJ, Weber LP (2011) Intranasal benzo[a]pyrene alters circadian blood pressure patterns and causes lung inflammation in rats. Arch Toxicol 85:337–346
Kraus U, Breitner S, Schnelle-Kreis J, Cyrys J, Lanki T, Rückerl R, Schneider A, Brüske I, Gu J, Devlin R, Wichmann HE, Zimmermann R, Peters A (2011) Particle-associated organic compounds and symptoms in myocardial infarction survivors. Inhal Toxicol 23:431–447
Luebke RW, Hodson PV, Faisal M, Ross PS, Grasman KA, Zelikoff J (1997) Aquatic pollution-induced immunotoxicity in wildlife species. Fundam Appl Toxicol, 37:1–15
Lee KH, Shu XO, Gao YT, Ji BT, Yang G, Blair A, Rothman N, Zheng W, Chow WH, Kang D (2010) Breast cancer and urinary biomarkers of polycyclic aromatic hydrocarbon and oxidative stress in the Shanghai Women’s Health Study. Cancer Epidemiol Biomarkers Prev 19:877–883
Mendis S, Sobotka PA, Euler DE (1995) Expired hydrocarbons in patients with acute myocardial infarction. Free Radic Res 23:117–122
O'Toole TE, Conklin DJ, Bhatnagar A (2008) Environmental risk factors for heart disease. Rev Environ Health 23:167–202
Shiue I (2013a) Urine phthalate concentrations are higher in people with stroke: United States national health and nutrition examination surveys (NHANES), 2001-2004. Eur J Neurol 20:728–731
Shiue I (2013b) Association of urinary arsenic, heavy metal, and phthalate concentrations with food allergy in adults: national health and nutrition examination survey, 2005-2006. Ann Allergy Asthma Immunol 111:421–423
Shiue I (2013c) Urinary environmental chemical concentrations and vitamin D are associated with vision, hearing, and balance disorders in the elderly. Environ Int 53:41–46
Shiue I (2014a) Arsenic, heavy metals, phthalates, pesticides, hydrocarbons and polyfluorinated compounds but not parabens or phenols are associated with adult remembering condition: US NHANES, 2011-2012. Environ Sci Pollut Res Int 22:6381–6386
Shiue I (2014b) Higher urinary heavy metal, phthalate, and arsenic but not parabens concentrations in people with high blood pressure, U.S. NHANES, 2011-2012. Int J Environ Res Public Health 11:5989–5899
Shiue I (2015a) Urinary heavy metals, phthalates, phenols, thiocyanate, parabens, pesticides, polyaromatic hydrocarbons but not arsenic or polyfluorinated compounds are associated with adult oral health: USA NHANES, 2011-2012. Environ Sci Pollut Res Int. doi:10.1007/s11356-015-4561-0
Shiue I (2015b) Urinary parabens and polyaromatic hydrocarbons independent of health conditions are associated with adult emotional support needs: USA NHANES, 2005-2008. Environ Sci Pollut Res Int. doi:10.1007/s11356-015-4749-3
Trochimowicz HJ, Reinhardt CF, Mullin LS, Azar A, Karrh BW (1976) The effect of myocardial infarction on the cardiac sensitization potential of certain halocarbons. J Occup Med 18:26–30
Conflict of interest
The author declares that she has no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Philippe Garrigues
Rights and permissions
About this article
Cite this article
Shiue, I. Are urinary polyaromatic hydrocarbons associated with adult hypertension, heart attack, and cancer? USA NHANES, 2011–2012. Environ Sci Pollut Res 22, 16962–16968 (2015). https://doi.org/10.1007/s11356-015-4922-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-015-4922-8