Abstract
Purpose
The objective of this pilot study was to compare the effects of water-based exercise to conventional land-based exercise on postural sway and quality of life in people with Parkinson’s disease.
Methods
Twenty people (male) with Parkinson’s disease were randomly divided into two groups of ten. Both groups carried out an 8-week (three sessions per week) physical exercise protocol. Postural sway and quality-of-life parameters of two groups were measured in pre- and post-intervention sessions.
Results
The between-group analyses indicate a greater reduction and thus improvement in the mean velocity of sway (p = 0.01) and an increase in the quality-of-life scores (p < 0.001) in the water-based group compared to land based.
Conclusions
Water-based exercises were more beneficial than land-based exercises when considering improvements to postural stability and the quality of life of those with Parkinson’s disease. The aquatic therapy is a promising intervention in the rehabilitative care of people with Parkinson’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
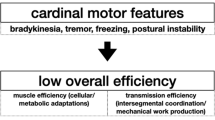
Parkinson’s disease (PD) is a degenerative neurological disorder affecting between 1 and 3% of older people [1]. Bradykinesia, muscle weakness, and poor motor control have been identified as the causes of movement disabilities and have, therefore, been the focus of the training exercises in the past research [2]. Physical exercise is essential for restoring joint mobility, muscle strengthening, and whole-body coordination and, therefore, is an integral part of a specific rehabilitation program to restore mobility and increase QoL in people with PD [3].
Postural instability is frequently demonstrated in people with PD [4] that contributes to their risk of falling [5] and poor quality of life (QoL) [6]. The ability to control standing postural sway is a prerequisite for many functional activities of daily life and for safe mobility; thus, it is commonly measured as a main parameter of human balance [7]. Using objective and precise measurements is essential in clinical and research evaluations. A force plate is an instrument that measures the ground reaction force and is used to quantify the postural sway in upright standing. Previous studies have demonstrated that the sensitivity and reliability of the Centre of Pressure (CoP) parameters measured with a force plate are sufficient to differentiate people with PD from their healthy peers of similar age [8]. Furthermore, the force plate data can also be used to show the changes of dyskinesia-induced postural instability [9] and predict postural instability in people with PD [10]. People with PD have shown less body sway in standing and a reduced limit of stability in dynamic tasks, and a higher risk of falling [11, 12].
Physical exercises that address deficits in postural stability have shown positive effects to increase motor function and independence in people with PD [13, 14]. Equipment-based resistance trainings have shown beneficial effects on balance, gait, and function in people with PD [15, 16]. The alternative forms of physical training that could retard balance deficits and prolong individual independence have recently gained more attention in research [17,18,19,20]. Aquatic training is currently used as a treatment method for people with PD [21, 22]. Emerging anecdotal results have indicated that this modality has beneficial effects on balance and an individual’s ability to complete exercise activities when used in conjunction with existing land-based exercises [22,23,24]. Aquatic training has previously been reported to be a useful treatment that improves postural stability for a variety of health conditions [25,26,27,28,29]. There is still limited scientific evidence about the potential benefits of aquatic training on the postural stability of people with PD [22]. Laboratory-based parameters of balance, measured using a force plate, have gained less attention than clinical outcome measures in studies of the effects of aquatic therapy in people with PD. A thorough search of the relevant literature yields no related study which has reported the effects of aquatic therapy on postural sway of people with PD during standing. The purpose of this study was to investigate the effects of aquatic exercise on standing postural sway, as well as quality of life in individuals with PD.
Method
Twenty males with PD volunteered in a randomized parallel-group controlled clinical trial. Participants were initially assessed by a neurological specialist to check their eligibility to take part in this study and then subsequently referred to the study. The referred subjects were diagnosed to be in stage II or III according to the “Hoehn and Yahr Scale” [30] and scored 22.5 ± 7.9 according to UPDRS III (Unified Parkinson’s Disease Rating Scale, Part III) at screening [31]. All participants had been taking dopaminergic medication (Levodopa) as a part of their therapeutic program. Participants had a freezing gait pattern (but were able to walk unaided) and had experienced at least one fall in the last 6 months. They had no signs of dementia (Mini-Mental Examination Scores more than 24) and gave informed consent. Participants were excluded if they had a history of fracture or have had orthopedic surgery within the last year. Participants were allocated to one of two groups: (1) water-based exercise group and (2) land-based exercise group (Fig. 1) via random allocation. To ensure both the comparison groups consisted of the same number of Hohen and Yahr stage-matched participants (four people were at stage II and six people at stage III), the random allocation was determined by selecting a sealed envelope, by the participant, from a bag. Medication dose in the two groups was controlled. Each participant took about 50 ± 10 ml/h of oral levodopa and no participant had any change in their medication during the study period. Ethical approval was obtained from the University’s Research Committee. The assessment sessions were carried out in the University’s facilities and the exercise programs (including both land and aquatic training) took place in a city gym/pool complex. This study only included men, because a male trainer was responsible for the participants’ exercise therapy and the lack of gender compatibility is a cultural concern, where this study was carried out. All participants completed their exercise programs and testing procedures.
Evaluations
All evaluation sessions ran between 8 a.m. and 11 a.m. to control the possible confounding effects of PD symptoms on the study outcomes. All participants were instructed not to take the anti-PD medications during the 8-h period before the evaluation sessions. The primary outcome measure was posturographic evaluation. Each participants’ ability to keep balance was tested by measuring postural sway, while bilaterally standing on a Kistler® force plate (Model: 9260AA6, Kistler instrument AG, Sweden), and mounted in the floor of the gait laboratory. During postural sway testing, the participants stood barefoot (feet were placed shoulder width apart and were slightly externally rotated) on the force platform, and they were unassisted and were required to put their feet within a marked area. Their arms were relaxed by their sides and they were required to look straight forward at a reference cross (X) that was placed 10 cm lower than their height on the wall in front of them. The participants were asked to maintain a quiet standing position for 90 s. The sampling rate of the force plate was set at 100 Hz. Three trials were recorded for each participant and averaged to produce a representative value for their postural sway. The force plate was calibrated and reset before each trial to remove the offset signals. Between each repetition, the participants were allowed to have a 2-min break to prevent fatigue.
The Parkinson’s Disease Quality-of-Life (PDQL) questionnaire was used to measure the participants’ quality of life [32]. This self-administered instrument had 37 questions which were classified into four scales. The different scales were: Parkinson’s disease symptoms (PS) with 14 questions, systematic symptoms (SS) with 7 questions, emotional functioning (EF) with 9 questions, and social functioning (SF) with 7 questions. The score for each scale ranged from 1 to 5, designed as a Likert-scale questionnaire. A high score implied favourable quality-of-life measurements. The original (English) questionnaire was translated into Farsi (Persian language) and its validity (the range of convergent validity: 0.42–0.8; discriminate validity: 0.15–0.7) and reliability (Cronbach alpha: 0.95) have been reported to be acceptable [33]. The Farsi version of PDQL was used in this study.
Exercise program
Both land and water-based protocols consisted of a 24-session program. The program lasted 8 weeks (three sessions per week) and was conducted under the supervision of an expert physical trainer. The aquatic program had the same design as the land program in terms of session-lengths and exercise manoeuvres. All sessions for both comparison groups started with 10 to 15-min warm-up phase specifically designed for each participant’s walking ability. During warm-up, the participants in the aquatic group were asked to walk across the pool, waist-deep, in water that was 30 °C. The non-aquatic group walked across a basketball court. After the warm-up period, a 40-min exercise program (primary treatment exercise period) was completed, which was tailored to each individual’s ability. The treatment exercises included stepping forward and backward, walking in a straight line, walking in alternating directions, walking on tiptoes, walking on the heels of the feet, passing a Swiss ball to the trainer (stood in front of them), catching the ball (passed by the trainer), and catching then passing the ball to and from alternate sides. The last 5-min phase was a cooling-down period that consisted of gentle stretching exercises. This exercise protocol was developed based on the guideline of the American College of Sports Medicine (ACSM) for physical exercise of the elderly with chronic conditions [34]. As recommended by ACSM, each exercise was initially started with two sets of ten repetitions for each manoeuvre [34] and was increased by approximately two repetitions, depending on each participant’s tolerance, every 2 weeks until 20 repetitions was achieved. Progression began mostly in the second and third weeks when participants found the task less difficult in the determined level of repetition and velocity.
Data processing
The CoP signals were passed through a second-degree curve filter with a 10 Hz cut-off frequency (Qualysis® software, Qualysis Inc., Sweden). The first and last 15 s of each trial were cropped (remaining 60 s). This was to limit the effect of possible adjustments, and the participant might have carried out to find a comfortable position over the force plate at the beginning of tests or when anticipating the end of recording time. The acquired CoP time series had two components, anteroposterior (AP) and mediolateral (ML) in a coordinated system. The 2D resulting distance (RD) was calculated from these two point measures as follows:
The range and mean velocity of CoP were computed using Microsoft Excel. The CoP-based parameters of body sway were:
The sway range (R) was the maximum distance between two points of the CoP path [35]:
Mean velocity (\( \bar{V} \)) was the average velocity that CoP moves and is calculated by dividing total excursion of the CoP by the recording time [35]:
Sway area (SA) was the area covered by CoP excursion per unit of time [36]:
Mean frequency (\( \bar{F} \)) was the frequency of the CoP trajectory if it had travelled in a circle with the radius of mean distance [36]:
In these equations, T stands for trial duration, n is data points to be calculated, and N is the total number of data points.
Statistical analysis
Two separate one-way between-group analyses of covariance (ANCOVA) were conducted to compare the effectiveness of aquatic and land-based exercises on postural sway and QoL outcomes. The independent variable was the type of exercise (aquatic- and land-based) and the dependant variables consisted of postural sway and QoL parameters recorded after the exercise protocols were completed. The participants’ baseline measures of postural sway and QoL were used as the covariant in these statistical analyses. Preliminary statistics were conducted to check that there was no violation of the assumption of normality, linearity, homogeneity of variances, homogeneity of regression slopes, and reliable measurement of covariate. Upon demonstration of a significant difference between two intervention groups on post-intervention parameters, post hoc tests were conducted to identify the source of any significant difference between- or within-group comparisons. Between-group differences were analyzed using independent and paired t tests. The paired t test was used to compare pre- and post-intervention results within each group. Statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS) version 16 software. The level of significance was set at 0.05 for all tests.
A power analysis was performed using the G.Power software (V.3.1, Heinrich Heine, University of Dusseldorf, Germany) to check the impact of a small sample size on the results. The CoP velocity of the post-intervention session was selected for this analysis, because this parameter has been reported as the best representative parameters of CoP that has a high correlation with clinical balance performance [37]. The calculated power of this study was 0.65. Fifteen participants in each group should be recruited to obtain the acceptable power at the 0.8. In this calculation, the adjusted level of alpha (0.15) was used as advised for the studies with a small group size [38].
Results
Twenty-two participants initially volunteered and 20 people completed the interventions (see Fig. 1 for dropouts) after attending over 80% of the sessions. None of the people that completed the trial had taken part in other exercise activities while involved in the study. The participants in the aquatic group were 60.5 ± 5.44 years, 72.55 ± 3.07 kg, and 168.1 ± 4.7 cm and those in the land group were 63.2 ± 4.94 years, 71.25 ± 28.6 kg, and 165.7 ± 4.07 cm. The t test showed no significant difference for these parameters between the two groups (p > 0.05).
ANCOVA analyses showed significant differences between two exercise groups on the post-intervention measures of: the mean velocity of CoP excursion [F (1, 17) = 8.02, p = 0.01, ƞ 2 = 0.32] and PDQL scores [F(1, 17) = 155.2, p < 0.001, η 2 = 0.9]. The results indicated that the two groups were similar at baseline (pre-intervention) parameters (p > 0.05). Within-group comparisons (paired t test) showed some significant changes in postural sway and QoL parameters after the exercises. The aquatic group showed significant improvements in mean velocity [p < 0.01; 95% CI (3.3, 9.8)], sway area [p < 0.01; 95% CI (5.6, 16.6)], and mean frequency [p < 0.01; 95% CI (0.05, 0.17)] of the CoP in the post-intervention session. Both groups showed improved sway range [land: p = 0.03; 95% CI (1.87, 23); aquatic: p = 0.05; 95% CI (−0.61, 43.3)]. In post-intervention results, the mean velocity of postural sway and PDQL score (including all the sub-divisions but the EF) were significantly different between aquatic and land groups (details in Tables 1, 2). The aquatic group showed a higher improvement in mean velocity of CoP [p = 0.01; 95% CI (−5.2, −0.66)] and PDQL scores [p < 0.001; 95% CI (8.1, 16.7)].
Discussion
The results of this study showed that a program consisting of thrice-weekly exercise therapy, for 8 weeks, improved the postural sway and QoL parameters in people with mild-to-moderate PD. Water-based exercise was more effective in improving the postural control and QoL parameters when compared with the same exercise protocol performed on land. The results of this study were in agreement with previous research [22, 23, 39,40,41], which showed that water-based exercise has a better improvement of balance in people with PD compared to that of land-based exercise. Previous research has mainly measured the effects of physical activity “subjectivity” through clinical assessment tools; this study assessed such an effect “objectivity” using instrumented measurements.
People with PD have less body sway in standing and reduced limit of stability in dynamic tasks and higher risk of falling [11, 12]. The reduction of falling after training is reported to be associated with the increased area and range of body sway in those with PD [12]. The increased range and area of CoP excursion could, therefore, be interpreted as improved balance in the participants. The CoP parameters used in this study are commonly used outcomes and have been shown to have a good association with the clinical parameters of balance [42, 43]. The velocity of CoP excursion is reported to be the most sensitive parameter to predict the risk of falls and balance performance in clinical evaluations [37, 42]. The reduction in mean velocity of CoP excursion suggests that training improves postural control [42]. As reported in previous research, the average value of the mean velocity of CoP is about 20 mm/s in people with PD, 13 mm/s in healthy aged-matched (older), and 10 mm/s in healthy young people [44]. Comparison of the data recorded can help us to recognize that training can improve outcomes towards normative values of healthy people.
The reduced QoL in people with PD is associated with deterioration in physical activity [45]. The participants’ improvement in QOL in both exercise groups was significant. The improvement in QoL shown in this trial indicates that the rehabilitation program is a useful method of improving the participants’ physical capabilities. Aquatic exercise showed a better improvement of QoL scores than land-based exercise. Considering that many people with PD do not have access to a pool for aquatic therapy; land-based exercise can still be beneficial.
Water-based exercise or aquatic training uses the unique properties of water, such as hydrostatic pressure, to facilitate functional mobility and reduce muscular fatigue during exercise [23, 46]. Efforts were made to control the intensity of protocol throughout both groups; however, participants showed different progressing rates, because their physical fitness were varied at baseline. To ensure that inhibiting conditions of postural stability were addressed by the exercise protocol, a specific therapeutic training was tailored for each participant [47]. Bradykinesia, muscle weakness, and poor motor control were identified as the causes of postural instability and were, therefore, the focus for the training exercises [2]. The applied training included stepping forward (heel-to-toe exercise) and backward (toe-to-heel exercise) to promote ankle sway and the strengthening of the leg muscles that stabilize the ankle. Alternating the direction of walking was a self-induced perturbation to compensate for a shift in the line of gravity, towards the marginal limits of the base of support. The external perturbation (passing and catching the Swiss ball) and the rotational movements were to enhance the control of hip and trunk muscles taking part in the hip strategy movement. These inherent aspects of exercise may have led to improved postural sway, in this study. Although the current findings imply that exercise would be effective in the improvement of postural control, the underlying mechanisms of the therapeutic effects on the motor control system were out of the scope of this study and warrant further investigation.
Study limitations
All the participants had continuous contact with a neurological specialist. This specialist may have used an updated therapy that aided the improvement in physical condition. However, recruitment in this way was necessary to ensure that the condition was correctly diagnosed and specialist care was essential to ensure that the condition was not worsened due to neglect. This study only included men; therefore, these results could not be generalized to women. This study also has some other limitations that restrict the generalizability of the findings in the following ways. First, due to the small sample size, the reported results should be considered as a preliminary finding of an exploratory study. Second, this was not a blind study, since the participants were aware of interventions they received. The participants may have had positive expectations about the benefits of exercise. As a result, individuals who participated in the exercise environment that was new to them (in the water) may have had higher expectations compared with those participating in the more conventional method (the exercise on the land). Third, the non-exercised condition was not included; therefore, the net benefit of each exercise method could not be determined; however, since exercise is known to improve the PD condition, it is arguably unethical to force an individual to not exercise at all. Finally, the follow-up evaluation is missing, which would have investigated how long the effects of the intervention would have lasted. This major limitation could affect the clinical importance of the results.
Conclusion
Findings suggested that aquatic training is a promising therapeutic intervention to improve the postural stability and perception of QoL of males with moderate stage PD who had a history of falling. Further studies with a long-term monitoring period are needed to check whether these improvements persist over time.
References
De Lau LM, Breteler MM (2006) Epidemiology of Parkinson’s disease. The Lancet Neurology. 5(6):525–535
Kwakkel G, de Goede CJ, van Wegen EE (2007) Impact of physical therapy for Parkinson’s disease: a critical review of the literature. Parkinsonism Relat Disord 13(Suppl 3):S478–S487
van der Kolk NM, King LA (2013) Effects of exercise on mobility in people with Parkinson’s disease. Mov Disord 28(11):1587–1596
Jankovic J (2008) Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry 79(4):368–376
Wood BH, Bilclough JA, Bowron A, Walker RW (2002) Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry 72(6):721–725
Lo RY, Tanner CM, Albers KB, Leimpeter AD, Fross RD, Bernstein AL et al (2009) Clinical features in early Parkinson disease and survival. Arch Neurol 66(11):1353–1358
Ruhe A, Fejer R, Walker B (2010) The test-retest reliability of centre of pressure measures in bipedal static task conditions–a systematic review of the literature. Gait Posture 32(4):436–445
Almeida IAD, Terra MB, Oliveira MRD, Silva RAD Jr, Ferraz HB, Santos SMS (2016) Comparing postural balance among older adults and Parkinson’s disease patients. Motriz Rev de Educ Física 22(4):261–265
Chung KA, Lobb BM, Nutt JG, McNames J, Horak F (2010) Objective measurement of dyskinesia in Parkinson’s disease using a force plate. Mov Disord 25(5):602–608
Doná F, Aquino CC, Gazzola JM, Borges V, Silva SM, Ganança FF et al (2016) Changes in postural control in patients with Parkinson’s disease: a posturographic study. Physiotherapy 102(3):272–279
Menant JC, Latt MD, Menz HB, Fung VS, Lord SR (2011) Postural sway approaches center of mass stability limits in Parkinson’s disease. Mov Disord 26(4):637–643
Nonnekes J, de Kam D, Geurts AC, Weerdesteyn V, Bloem BR (2013) Unraveling the mechanisms underlying postural instability in Parkinson’s disease using dynamic posturography. Expert Rev Neurother 13:1303–1308
Dibble LE, Addison O, Papa E (2009) The effects of exercise on balance in persons with Parkinson’s disease: a systematic review across the disability spectrum. J Neurol Phys Ther 33(1):14–26
Tomlinson CL, Herd CP, Clarke CE, Meek C, Patel S, Stowe R et al (2014) Physiotherapy for Parkinson’s disease: a comparison of techniques. Cochrane Database Syst Rev 2014(6):2815
Hass CJ, Buckley TA, Pitsikoulis C, Barthelemy EJ (2012) Progressive resistance training improves gait initiation in individuals with Parkinson’s disease. Gait Posture 35(4):669–673
Lima LO, Scianni A, Rodrigues-de-Paula F (2013) Progressive resistance exercise improves strength and physical performance in people with mild to moderate Parkinson’s disease: a systematic review. J Physiother 59(1):7–13
Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J et al (2012) Tai chi and postural stability in patients with Parkinson’s disease. N Engl J Med 366(6):511–519
de Dreu MJ, van der Wilk AS, Poppe E, Kwakkel G, van Wegen EE (2012) Rehabilitation, exercise therapy and music in patients with Parkinson’s disease: a meta-analysis of the effects of music-based movement therapy on walking ability, balance and quality of life. Parkinsonism Relat Disord 18(suppl 1):S114–S119
Duchesne C, Lungu O, Nadeau A, Robillard ME, Boré A, Bobeuf F et al (2015) Enhancing both motor and cognitive functioning in Parkinson’s disease: aerobic exercise as a rehabilitative intervention. Brain Cogn 99:68–77
Hackney ME, Earhart GM (2009) Effects of dance on movement control in Parkinson’s disease: a comparison of Argentine tango and American ballroom. J Rehabil Med 41(6):475–481
Giladi N (2009) Mobility and exercise in movement disorders. Parkinsonism Relat Disord 15(Suppl 3):S46–S48
Ayán Pérez C, Cancela JM (2013) Effectiveness of water-based exercise in people living with Parkinson’s disease: a systematic review. Eur Rev Aging Phys Act 11:107
Vivas J, Arias P, Cudeiro J (2011) Aquatic therapy versus conventional land-based therapy for Parkinson’s disease: an open-label pilot study. Arch Phys Med Rehabil 92(8):1202–1210
Kargarfard M, Chitsaz A, Azizi S (2012) Effects of an 8-week aquatic exercise training on balance in patients with Parkinson’s disease. J Isfahan Med Sch 30(178):141–150
Suomi R, Koceja DM (2000) Postural sway characteristics in women with lower extremity arthritis before and after an aquatic exercise intervention. Arch Phys Med Rehabil 81(6):780–785
Devereux K, Robertson D, Briffa NK (2005) Effects of a water-based program on women 65 years and over: a randomised controlled trial. Aust J Physiother. 51(2):102–108
Arnold CM, Busch AJ, Schachter CL, Harrison EL, Olszynski WP (2008) A randomized clinical trial of aquatic versus land exercise to improve balance, function, and quality of life in older women with osteoporosis. Physiother Can 60(4):296–306
Katsura Y, Yoshikawa T, Ueda SY, Usui T, Sotobayashi D, Nakao H et al (2010) Effects of aquatic exercise training using water-resistance equipment in elderly. Eur J Appl Physiol 108(5):957–964
Elbar O, Tzedek I, Vered E, Shvarth G, Friger M, Melzer I (2013) A water-based training program that includes perturbation exercises improves speed of voluntary stepping in older adults: a randomized controlled cross-over trial. Arch Gerontol Geriatr 56(1):134–140
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17(5):427–442
Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease (2003) The Unified Parkinson’s Disease Rating Scale (UPDRS): status and recommendations. Mov Disorders 18(7):738
De Boer AGEM, Wijker W, Speelman JD, De Haes JCJM (1996) Quality of life in patients with Parkinson’s disease: development of a questionnaire. J Neurol Neurosurg Psychiatry 61(1):70–74
Ghaem H, Haghighi AB, Zeighami B, Dehghan A (2010) Validity and reliability of the Persian version of the Parkinson disease quality of life (PDQL) questionnaire. J Kerman Univ Med Sci 17(1):49–58
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC et al (2007) Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 116(9):1094
Wheat JS, Haddad JM, Fedirchuk K, Davids K (2014) Effects of textured socks on balance control during single-leg standing in healthy adults. Proc Eng 72:120–125
Bigelow KE (2008) Identification of key traditional and fractal postural sway parameters to develop a clinical protocol for fall risk assessment in older adults. The Ohio State University, Columbus
Raymakers JA, Samson MM, Verhaar HJ (2005) The assessment of body sway and the choice of the stability parameter(s). Gait Posture 21(1):48–58
Stevens JP (2009) Applied multivariate statistics for the social sciences. Routledge, New York
Volpe D, Giantin MG, Maestri R, Frazzitta G (2014) Comparing the effects of hydrotherapy and land-based therapy on balance in patients with Parkinson’s disease: a randomized controlled pilot study. Clin Rehabil 28:1210–1217
Brefel-Courbon C, Desboeuf K, Thalamas C, Galitzky M, Senard JM, Rascol O et al (2003) Clinical and economic analysis of spa therapy in Parkinson’s disease. Mov Disord 18(5):578–584
Kawasaki M (2009) The effects of aquatic exercise on balance outcomes in individuals with Parkinson’s disease: 1705: Board# 55 May 27 2: 00 PM-3: 30 PM. Med Sci Sports Exerc 41(5):102
Prieto TE, Myklebust JB, Hoffmann RG, Lovett EG, Myklebust BM (1996) Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Trans Biomed Eng 43(9):956–966
Rocchi L, Chiari L, Cappello A, Horak FB (2006) Identification of distinct characteristics of postural sway in Parkinson’s disease: a feature selection procedure based on principal component analysis. Neurosci Lett 394(2):140–145
Ickenstein GW, Ambach H, Klöditz A, Koch H, Isenmann S, Reichmann H et al (2012) Static posturography in aging and Parkinson’s disease. Front Aging Neurosci 4:20
Chrischilles EA, Rubenstein LM, Voelker MD, Wallace RB, Rodnitzky RL (2002) Linking clinical variables to health-related quality of life in Parkinson’s disease. Parkinsonism Relat Disord 8(3):199–209
Morris DM (2010) Aquatic therapy to improve balance dysfunction in older adults. Topics Geriatr Rehabil 26(2):104–119
Kluding P, McGinnis PQ (2006) Multidimensional exercise for people with Parkinson’s disease: a case report. Physiother Theory Pract 22(3):153–162
Acknowledgements
The work completed here was a Research Project which was co-registered by the Azad University of Khorasgan and Musculoskeletal Research Center, Isfahan University of Medical Sciences, Iran (Registration code: IR.IAU-KH.REC.1392.392345). This Project had no source fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shahmohammadi, R., Sharifi, GR., Melvin, J.M.A. et al. A comparison between aquatic and land-based physical exercise on postural sway and quality of life in people with Parkinson’s disease: a randomized controlled pilot study. Sport Sci Health 13, 341–348 (2017). https://doi.org/10.1007/s11332-017-0363-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-017-0363-8