Abstract
Purpose
Falls are common events in institutionalized elderly. Recent evidence suggests that several risk factors (FRFs) may be related to these falls. The aim of this study was to elucidate if some demographic and clinical factors are associated with the risk of falls in institutionalized elderly. The role of adapted physical activity (APA) in the risk of falls was also assessed.
Methods
With a Kaplan–Meier statistical model, the mean survivor time (MST) to a fall event was recorded for 6 months in 128 new-admitted patients to nursing home. Demographic factors such as sex, age, stature, body mass or other FRFs such as fall recidivism, gait and balance performance, cognitive impairment, activity of daily living (ADL) levels, Parkinson’s disease, utilization of gait assistant devices, and the employment of a program of APA were considered potential co-variants.
Results
Thirty patients experienced a fall during the observation period (6 months) with an overall MST of 154.8 ± 4.6 (range 2–167) days. Moreover, history of previous fallen, reduced gait capacity, poor cognitive function, limited performance in the ADL, and Parkinson’s disease were associated with a reduced MST to a fall event. While at contrary, the employment of the APA significantly reduced the fall-risk.
Conclusions
Our results suggest the effectiveness of an APA program for the prevention of falling in institutionalized elderly. Moreover, new-admitted patients to nursing homes with a history of previous fallen, reduced gait capacity, poor cognitive function, limited performance in the ADL, and Parkinson’s disease are associated with an increased risk of fallen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fall sequels are the fifth cause of death in the elderly [1]. In nursing homes and long term-facilities, number of falls is double in comparison to non-institutionalized older adults [2, 3]. Amount of literature has underlined that this phenomenon is also associated with elevated rate of mortality [4], deeply affects families, and increases society financial burden [5, 6]. Most of the recognized fall-risk factors (FRFs) are usually higher in elderly hospitalized patients [7–10]. For instance, reduced gait and balance performance, asthenia, cognitive impairment, and augmented dependence in the execution of activities of daily living (ADL) are recognized FRFs [2, 11–13]. Age-related pathologies such as Alzheimer’s disease, Parkinson’s disease, stroke, and arthritis seem equally associated with this clinical phenomenon [3, 11, 14]. Despite the recognition of this problem in the clinical milieu and several interventional studies aimed to prevent falls in care homes, the literature provides inconsistent results on FRFs. This heterogeneity is likely associated with a large difference in interventions and levels of patient’s dependency [15, 16].
Besides the objective of interventional studies, research needs also to investigate which are the potential detectable FRFs in a multifaceted clinical setting, such as the standard nursing homes. In particular, the early recognition of patients of high risk of falls would be of crucial importance to start specific treatments. In this scenario, adapted physical activity (APA) is becoming a useful means by which institutionalized elderly individuals may gain muscular strength, enhance ADL performance, and reduce the natural progression of cognitive and physical impairment [17–27]. However, the role of APA in the incidence of falls in nursing home residents is still a matter of debate [15]. Moreover, the risk of falling associated with the recognized FRFs in the specific time frame starting from the admission of the patient to the nursing home is not fully elucidated.
Therefore, the aim of this study was to clarify whether some demographic factors such as sex, age, stature, body mass, fall recidivism, gait and balance performance, cognitive impairment, ADL level, Parkinson’s disease, utilization of gait assistant devices, and the employment of a program of APA are associated with the risk of falls in institutionalized elderly individuals.
Methods
Study design
This observational prospective-cohort study compared fallen and not fallen patients, stratified by their demographic, physical, and pathological characteristics. Kaplan–Meier estimate was used to measure the fraction of subjects not incurred in a fall the first 6 months from the admission to a nursing home. The time from admission (days) to an occurrence of the fall, or to the end of follow-up (censored), were the main variables. Moreover, to compare potential difference among sub-groups of the selected patients a Kaplan–Meier estimate was performed by stratifying the group by sex, age, stature, body mass, recidivism, gait and balance performance, cognitive impairment, ADL levels, Parkinson’s disease, utilization of gait assistant device, and the employment of a program of APA during the observed 6 months.
The study was carried out in accordance with the Declaration of Helsinki (2013) of the World Medical Association for experiments involving humans.
Participants
Eligible volunteers were selected at the admission to the geriatrics care units at the Mons. Mazzali Geriatric Institute in Mantua, Italy. Inclusion criteria were an age greater than 65 years old. No exclusion criteria related to chronic diseases were applied.
Screening
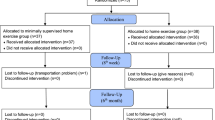
128 patients (37 men and 91 women) were selected for the study. Baseline characteristics of the participants are reported in Table 1.
Test procedures
Number of fallen were recorded during the first 6 months from the admission of the patients to the geriatric care unit. Potential co-variants were assessed at the admission to the geriatric care unit.
APA program
During the 6-month of standard geriatric care, a program of APA (5 times/week) was offered to the participants. Noticeably, APA program was not mandatory and employed by the selected patients according their preferences. Specifically, the APA program included circuit-training exercises as described by Venturelli et al. [17]. Each exercise session lasted approximately 60 min: 5 min of warm-up, 30 min of aerobic exercise, 20 min of resistant circuit training, and 5 min of cool-down. Exercising tools used in the study were cycle ergometers (Bike-Race Technogym SpA, Gambettola, Italy), resistance elastic bands, dumbbells from 0.5 to 3 kg, sticks, and sponge balls. The warm-up program comprised active arm and shoulder mobilization by sponge balls and sticks. Aerobic exercise was performed on a cycle ergometer at a workload corresponding to the 60% of the maximal predicted heart rate. Resistance circuit-training exercises for the upper limbs and trunk were performed at 50% of 1RM of the arm curl test, and subsequently enhanced by increasing the number of repetitions and/or load. The initial work load for resistance training by the elastic band was set according to the 1RM arm curl test: subjects with low maximal strength (1st and 2nd quartiles of 1RM) used the yellow Theraband, whereas patients with high maximal strength (3rd and 4th quartiles of 1RM) used the red Theraband. The elastic band work load was increased during the training period only by augmenting the number of repetitions. During the cool-down phase, subjects performed static stretching exercises for legs, arms, shoulders, and neck, keeping the maximal muscle elongation for 30 s, and increasing the range of motion. The exercises were performed under the supervision of a kinesiologist. Adherence to the APA program was recorded into a log.
Baseline assessment
Fasted body mass and stature were measured with a professional mechanical scale fitted with a stadiometer (Seca mod. 713; III-M; Seca Medical Scales and Measuring Systems, Birmingham, UK). History of previous falls was documented with a standard form. Nursing home residents’ gait and balance performance were assessed by POMA scale [28]. The Mini Mental State Examination (MMSE) [29] was utilized to determinate cognitive performance. Independence and level of ADL were evaluated by Barthel Index [30]. Confirmed diagnosis of Parkinson’s disease was also documented during the physical medical evaluation.
Statistical methods
Kaplan-Mayer survival analysis estimated the proportion of not fallen patients from admission to nursing home. The time from assessment (days) to an occurrence of falling, or to the end of follow-up (6 months—censored), was the main variable. The difference in the mean survivor time (MST) between each parameter assessed at the admission of the patient has been tested with a Log Rank (Mantel-Cox) model. Sex, history of previous falling, Parkinson’s disease, and the utilization of gait assistant devices have been treated as dichotomous variables. Age, POMAb, POMAg, MMSE, ADL, stature, body mass, the adherence to the APA program have been distributed according the higher (Ht), middle (Mt), and lower (Lt) tertile.
Results
The participants’ characteristics are summarized in Table 1. Thirty falls have been documented during the 6 months of observation period.
Overall survivor analysis
The proportion of not fallen patients in the 180 days following the admission to the nursing home is represented in Fig. 1. Specifically, the overall MST to a fall event was 154.8 ± 4.6 days.
Survivor analysis and demographic factors
Female and male patients exhibited similar MST to a fall event 156.4 ± 5.5 and 150.7 ± 9.1 days (p = 0.309), respectively. No difference was detected in the MST to a fall event among the three age-tertile groups (p = 0.070; Table 2). Patients’ stature and body mass were not associated with an increased risk of falling (p = 0.071 and 0.122, respectively Table 2).
Survivor analysis and FRFs
As expected, a history of previous falls significantly affected the MST to a fall event (Fig. 2e; Table 2). Interestingly, patients with a reduced balance performance, assessed by the POMAb test, did not demonstrate an increased risk of falling (p = 0.661). Contrarily, patients in the Lt of gait capacity (POMAg) showed a significant reduction in MST to a fall event (Fig. 2a; Table 2). Patients in the Lt of cognitive capacity, assessed with the MMSE, demonstrated a worsen MST to a fall event (Fig. 2c; Table 2). Similarly, patients with Parkinson’s disease and lower levels of ADL showed an increased risk of falling (Fig. 2b, f). Interestingly, the utilization of gait assistant devices did not seem to affect MST to a fall event (Table 2). However, in the group that did not attend the proposed APA program (Lt), the risk of falls was significantly increased (Fig. 2d; Table 2).
Kaplan–Meier estimation models of the fraction of not fallen patients (proportion/months). a–d Represents Kaplan-Meier curves of the recruited 128 new-admitted patients distributed in higher (Ht), middle (Mt), and lower (Lt) tertiles. d, e Represents dichotomous variables (yes–no). POMAg, gait performance test [28]; ADL, Barthel Index [30]; MMSE, the Mini Mental State Examination [29]; APA, adapted physical activity. *MST significant shorter
Subject’s characteristics according their adherence of APA program
As reported in Table 3, the adherence to the proposed AFA program varied among the institutionalized patients. Indeed, 30 of the fifty-three patients that did not attended (Lt) the APA program have incurred in a fall during the first 6 months of hospitalization. However, their physical characteristics and medical status tended, without reaching a significant difference, to be lower in comparison to the patients that attended APA.
Discussion
Although FRFs have been already investigated in clinics, the influence of these factors on the MST to a fall event from the patient’s admission to a nursing home facility has received so far only little attention. The main finding of this study was that history of previous falls, reduced gait capacity, poor cognitive function, limited performance in the ADL, and Parkinson’s disease were associated with an increased risk of falling. Conversely, patients that, during this 6-month observation period, were involved in an APA program exhibited a significant reduction in the risk of falling.
Incidence of falling and demographic risk factors
In a recent study, the incidence of falling among 230,730 individuals newly admitted to nursing homes was examined [3]. The 21% of this cohort had experienced at least one fall. In another cohort study among institutionalized elderly individuals [13], several demographic FRFs have been studied such as age, sex, and body mass index (BMI). Interestingly, only smaller BMI values were associated with an increased risk of falling. Data from the present study are partially in agreement with these previous reports. In fact, the percentage of patients recruited for this study that incurred in a fall during the first 6 months of hospitalization was very similar (about 23%) to that previously reported [3]. Moreover, in agreement with Diaz Gravalos and co-workers [13], age and sex did not appear to be associated with an elevated risk of falls. Noticeably, alterations in the anthropometric parameters, such as lower body mass and stature, were not associated with an increased risk of falling [13].
Fall-risk factors in hospitalized elderly
It has been recently highlighted that most of the recognized FRFs are elevated in hospitalized elderly individuals [7–10]. Therefore, specific investigations are strongly recommended to prevent this clinical phenomenon. Previous studies involving hospitalized elderly people revealed that the most important FRFs were: history of previous falls, reduced gait and balance capacity, reduced muscular force, cognitive impairment, and difficulties in the execution of activities of daily living [2, 11–13]. Moreover, an increased risk of falling is also associated with the severity of pathologies such as Alzheimer and Parkinson’s disease, stroke, and arthritis [3, 11, 14]. Data from the present study are in agreement with this literature as history of previous falls, reduced gait capacity, poor cognitive function, limited performance in the ADL, and Parkinson’s disease were associated with an increased risk of falling in our cohort of institutionalized elderly.
The role of APA in the risk of falling
During the last decade, APA is becoming a useful approach through which institutionalized elderly individuals may gain muscular strength, enhance independence, and contrast cognitive and physical deterioration [17–20, 25–27, 31]. However, it has been recognized that APA interventions for preventing falls in care facilities remain uncertain due to conflicting results, possibly associated with differences in interventions and levels of patient’s dependency [15]. While many co-factors are likely associated with the adherence to an APA program (Table 3), data from the present study suggest that the participation to an APA program may help to decrease the risk of falling among hospitalized elderly individuals. This result is extremely important because it indicates the effectiveness of APA as a successful and tailored treatment for the patients at high risk of falling.
Conclusion
In nursing homes, number of falls is double in comparison to non-institutionalized older adults, causing an elevated rate of mortality and society financial-burden. Results of this study indicate that history of previous falls, reduced gait capacity, poor cognitive function, limited performance in the ADL, and Parkinson’s disease are associated with an increased risk of falling. Therefore, particular attention has to be payed to these fall-predictors in institutionalized elderly. Even though the adherence to a program of APA in the clinical setting is potentially affected by confounding factors such as the cognitive level of the patients, their functional capacity, and health status, our data seem to suggest the effectiveness of an APA program in the prevention of falls.
References
Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 35(Suppl 2):ii37–ii41. doi:10.1093/ageing/afl084
Fonad E, Wahlin TB, Winblad B, Emami A, Sandmark H (2008) Falls and fall risk among nursing home residents. J Clin Nurs 17(1):126–134. doi:10.1111/j.1365-2702.2007.02005.x
Leland NE, Gozalo P, Teno J, Mor V (2012) Falls in newly admitted nursing home residents: a national study. J Am Geriatr Soc 60(5):939–945. doi:10.1111/j.1532-5415.2012.03931.x
Nurmi IS, Luthje PM, Kataja JM (2004) Long-term survival after falls among the elderly in institutional care. Arch Gerontol Geriatr 38(1):1–10
Carroll NV, Delafuente JC, Cox FM, Narayanan S (2008) Fall-related hospitalization and facility costs among residents of institutions providing long-term care. The Gerontologist 48(2):213–222
Stevens JA, Corso PS, Finkelstein EA, Miller TR (2006) The costs of fatal and non-fatal falls among older adults. Inj Prev 12(5):290–295. doi:10.1136/ip.2005.011015
Becker C, Rapp K (2010) Fall prevention in nursing homes. Clin Geriatr Med 26(4):693–704. doi:10.1016/j.cger.2010.07.004
Handoll H (2010) Prevention of falls and fall related injuries in older people in nursing homes and hospitals. Inj Prev 16(2):137–138. doi:10.1136/ip.2010.026625
Heinrich S, Rapp K, Stuhldreher N, Rissmann U, Becker C, Konig HH (2013) Cost-effectiveness of a multifactorial fall prevention program in nursing homes. Osteoporos Int J Estab Result Coop Euro Found Osteoporos Nat Osteoporos Found USA 24(4):1215–1223. doi:10.1007/s00198-012-2075-x
Vlaeyen E, Coussement J, Leysens G, Van der Elst E, Delbaere K, Cambier D, Denhaerynck K, Goemaere S, Wertelaers A, Dobbels F, Dejaeger E, Milisen K, Center of Expertise for F, Fracture Prevention F, (2015) Characteristics and effectiveness of fall prevention programs in nursing homes: a systematic review and meta-analysis of randomized controlled trials. J Am Geriatr Soc 63(2):211–221. doi:10.1111/jgs.13254
Alvarez Barbosa F, Del Pozo-Cruz B, Del Pozo-Cruz J, Alfonso-Rosa RM, Sanudo Corrales B, Rogers ME (2016) Factors associated with the risk of falls of nursing home residents aged 80 or Older. Rehabil Nurs Off J Assoc Rehabil Nurses 41(1):16–25. doi:10.1002/rnj.229
da Silva Borges EG, de Souza Vale RG, Cader SA, Leal S, Miguel F, Pernambuco CS, Dantas EH (2014) Postural balance and falls in elderly nursing home residents enrolled in a ballroom dancing program. Arch Gerontol Geriatr 59(2):312–316. doi:10.1016/j.archger.2014.03.013
Diaz Gravalos GJ, Gil Vazquez C, Andrade Pereira V, Alonso Payo R, Alvarez Araujo S, Reinoso Hermida S (2009) Risk factors for falls amongst older people living in nursing home. A cohort study. Rev Esp Geriatr Gerontol 44(6):301–304. doi:10.1016/j.regg.2009.06.013
Nazir A, Mueller C, Perkins A, Arling G (2012) Falls and nursing home residents with cognitive impairment: new insights into quality measures and interventions. J Am Med Direct Assoc 13 (9):819e811–819e816. doi:10.1016/j.jamda.2012.07.018
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, Kerse N (2012) Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database System Rev 12:CD005465. doi:10.1002/14651858.CD005465.pub3
Oliver D, Connelly JB, Victor CR, Shaw FE, Whitehead A, Genc Y, Vanoli A, Martin FC, Gosney MA (2007) Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ 334(7584):82. doi:10.1136/bmj.39049.706493.55
Venturelli M, Lanza M, Muti E, Schena F (2010) Positive effects of physical training in activity of daily living-dependent older adults. Exp Aging Res 36(2):190–205. doi:10.1080/03610731003613771
Venturelli M, Magalini A, Scarsini R, Schena F (2012) From Alzheimer’s disease retrogenesis a new care strategy for patients with advanced dementia. Am J Alzheimer’s Dis Dement 27(7):483–489. doi:10.1177/1533317512459794
Venturelli M, Scarsini R, Schena F (2011) Six-month walking program changes cognitive and ADL performance in patients with Alzheimer. Am J Alzheimer’s Dis Dement 26(5):381–388. doi:10.1177/1533317511418956
Venturelli M, Cè E, Limonta E, Schena F, Caimi B, Carugo S, Veicsteinas A, Esposito F (2015) Effects of endurance, circuit, and relaxing training on cardiovascular risk factors in hypertensive elderly patients. Age 37(5):1–13. doi:10.1007/s11357-015-9835-4
Venturelli Massimo CE, Limonta Eloisa, Muti Ettore, Scarsini Renato, Brasioli Anna, Schena Federico, Esposito Fabio. (2016) Possible predictors of involuntary weight loss in patients with Alzheimer’s disease. PLoS One
Cè E, Rampichini S, Limonta E, Esposito F (2013) Torque and mechanomyogram correlations during muscle relaxation: effects of fatigue and time-course of recovery. J Electromyogr Kinesiol 23(6):1295–1303. doi:10.1016/j.jelekin.2013.09.007
Maggioni MA, Cè E, Giordano G, Bertoli S, Battezzati A, Veicsteinas A, Merati G (2012) Effects on body composition of different short-term rehabilitation programs in long-stay hospitalized elderly women. Aging Clin Exp Res 24(6):619–626. doi:10.3275/8589
Di Tano G, Fulle S, Pietrangelo T, Bellomo R, Fanò G (2005) Sarcopenia: characteristics, genesis, remedies. Sport Sci Health 1(2):69–74. doi:10.1007/s11332-2005-004-0013-4
Gambassi BB, Rodrigues B, de Jesus Furtado Almeida F, Sotão SS, da Silva Souza TM, Chaves LFC, Sauaia BA, Schwingel PA, Pulcherio JOB, Mostarda CT (2016) Acute effect of resistance training without recovery intervals on the blood pressure of comorbidity-free elderly women: a pilot study. Sport Sci Health:1–6. doi:10.1007/s11332-016-0290-0
Lillo N, Palomo-Vélez G, Fuentes E, Palomo I (2015) Role of physical activity in cardiovascular disease prevention in older adults. Sport Sci Health 11(3):227–233. doi:10.1007/s11332-015-0233-1
Pizzigalli L, Ahmaidi S, Rainoldi A (2014) Effects of sedentary condition and longterm physical activity on postural balance and strength responses in elderly subjects. Sport Sci Health 10(2):135–141. doi:10.1007/s11332-014-0184-y
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34(2):119–126
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Mahoney FI, Barthel DW (1965) Functional evaluation: the barthel index. Md State Med J 14:61–65
Massimo Venturelli, Emiliano Cè, Eloisa Limonta, Valentina Bisconti A, Anna Brasioli, Ettore Muti, Fabio Esposito (2016) Effectiveness of exercise- and cognitive-based treatments on salivary cortisol levels and sundowning syndrome symptoms in patients with Alzheimer’s disease. J Alzheimers Dis. doi:10.3233/JAD-160392
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical Standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or compatible ethical Standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Tonni, V., Cè, E., Limonta, E. et al. Fall-risk factors in hospitalized elderly: the role of adapted physical activity. Sport Sci Health 12, 471–477 (2016). https://doi.org/10.1007/s11332-016-0324-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-016-0324-7