Key Summary Points
To measure the effects of home exercises complemented with supervision on fall-related variables in older people.
AbstractSection FindingsSupervised home exercise seems superior only on functional mobility (TUGT).
AbstractSection MessageOlder individuals who do not have exercise habits should be motivated to exercise training in daily life.
Abstract
Purpose
The aim was to measure the effects of the home exercises supported with supervision on the fall-related variables in older people.
Methods
Seventy-five individuals over the age of 65 were enrolled. They were allocated to a “minimally supervised home exercise group” (group 1) or a “home exercise group” (group 2). Falls efficacy, fear of falling (FOF), fall risk, functional mobility, balance performance, and depression were assessed using the Falls Efficacy Scale International (FES-I), visual analog scale (VAS-FOF), the Elderly Falls Screening Test (EFST), the Timed Up and Go Test (TUGT), Tinetti’s Balance Performance Oriented Mobility Assessment (BPOMA), and the Geriatric Depression Scale Short Form (GDS-SF), respectively. Participants performed a four-day weekly exercise program for eight weeks. Group 1 was supervised one day per week on a group basis.
Results
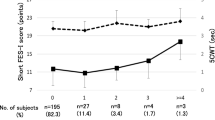
Results are based on 75 subjects (group 1 n = 37, group 2 n = 38). Analysis of variance revealed significant interactions only for FES-I, VAS-FOF, TUGT, and BPOMA. The difference between groups was significant only for TUGT score; group 1 had better scores at 8 weeks and 6 months. FES-I, VAS-FOF, and BPOMA were significantly improved in both groups. EFST and GDS improved in the total sample but not at the group level.
Conclusion
Supervised home exercise seems to be superior only for functional mobility (TUGT). Further studies with a larger sample are needed to draw conclusions about depression and fall risk. The intervention was feasible and atendible.
Trial registration
ClinicalTrials.gov" NCT05337839. Retrospectively registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative processes that occur with increasing age lead to an increase in the risk of falls [1]. Even if they do not result in injury, the main consequences of falls are fear of falling (FOF), activity restrictions, loss of mobility, and loss of independence. With aging, the rate of falls has been reported to increase by up to 60% [2]. Rapp reported an annual fall rate of 29.7% in community-dwelling men and 38.7% in women aged 65–90 years in Germany [3]. In a cross-sectional study conducted in Turkey, 28.5% of 2322 participants aged 65 years and older reported falling in the past year [4]. As a result, falls are a serious and important public health problem [5,6,7].
In older adults, muscle weakness, lack of flexibility, deficiencies in maintaining balance, and unconfident walking are the main causes of falls [1, 5, 6]. These can be treated by implementing various measures, including exercise programs [1, 5, 6, 8]. On the other hand, fall prevention programs are expected to improve both physical and psychosocial functioning [7, 9, 10]. Prevention of sedentary lifestyle is possible as long as outcome measures related to psychosocial function improve [11, 12]. Among these variables FOF, depression and falls efficacy take place considerably [7, 9]. A systematic review reported the prevalence of FOF to range from 3 to 85% in community-dwelling older adults [13]. Reducing FOF and improving fall-related self-efficacy are expected to have positive effects on the health of older adults. [14]. Tinetti concluded that the association between falls efficacy and function is stronger than the association between fall history and function [15]. In 2003, Stel reported the predictive ability of balance and mobility performance for recurrent falling [7].
There are few studies reporting positive effects of an exercise program on psychosocial functions such as depression and falls efficacy. These studies are designed to compare a fully supervised experimental group with a control group receiving usual care [5, 16, 17]. In only one study, supervision was minimal and delivered via home visit. However, no psychosocial function-related outcome measure was evaluated [18]. The need for balance supervision, especially when supervising is complemented with home exercises, has been pointed out by Ng et al. [19]. The present study meets this need by providing minimally supervision to experimental group.
Thus, the aim was to measure the effects of the balanced supervised intervention on the abovementioned physical and also psychosocial fall-related variables immediately after the withdrawal of the intervention and 6 months later in community-dwelling older adults. In fall prevention studies, especially in the assessment of fear of falling and self-efficacy, a follow-up period of at least 6 months is recommended to detect positive changes [12, 20]. Based on this suggestion, a follow-up period of 6 months was chosen.
Methods
Design
This was a single-center, randomized and double-blind trial with two parallel arms, namely minimally supervised home exercise group (group 1) and home exercise group (group 2).
Patients and setting
Data were collected at Izmir Bozyaka Training and Research Hospital in Turkey, a tertiary health-care facility where it is difficult to recruit healthy individuals for the studies. For this reason, older people between 65 and 80 years of age who suffered from myalgia for a short period of time (no longer than two weeks) that did not raise doubts about a serious disease were recruited. Participants were not painful along intervention period, and there was no need for treatment. Inclusion criteria were the ability to complete the timed up and go test (TUGT) independently or with the aid of an assistive device, having no regular exercise habits, and a score above 20 on the Mini Mental State Examination (MMSE) [16]. MMSE an 11-item screening test of cognitive function that quantifies orientation to time and place, registration, recall, attention, calculation, language, and praxis. For scoring, the total number of correct answers is added, and the maximum possible score is 30 [21]. A score of 23 or less is considered to indicate cognitive impairment [22]. Excluding criteria were medical conditions impeding to perform exercises such as severe musculoskeletal and neurological disease, severe visual impairment, cardiovascular, pulmonary, or malignant disease. Demographic and medical characteristics of participants, including age, sex, body mass index, education level, number of comorbidities, number of medications taken by participants, and number of fall events, were recorded. Fall history was recorded as the number of fall events in the past twelve months. All eligible participants were informed of the aim of the study and provided written informed consent. The study was approved by the local ethics committee of our hospital and was conducted in accordance with the ethical standards of the Declaration of Helsinki. The study was registered on the ClinicalTrials website under the ID of NCT05337839.
Randomization
The allocation sequence was generated by a statistician with a random block size of 6 and placed in sealed sequential opaque envelopes. An allocation ratio of 1:1 was used. These envelopes were delivered to patients by last two authors after enrollment in the study, and the patients were referred to the first author (supervising physician). She opened the envelopes and assigned the patients to group 1 or group 2.
Blinding
The patients, the outcome assessor, and the statistician were blinded to allocation. The supervising physician was not blinded.
Interventions
Participants were asked to perform the stretching, balance, and strengthening exercises listed in the guide (Exercise & Physical Activity: Your Everyday Guide from the National Institute on Aging) published by the National Institute on Aging (https://healthysd.gov/wp-content/uploads/2015/04/go4life-exercise-guide.pdf). These exercises have been prepared for older people and are suitable for self-implementation at home. Participants received a written exercise booklet with illustrations and simple instructions to help them perform the exercises safely. The booklet included information on the objectives, instructions on how to perform the exercises safely and avoid harmful movements, instructions on the order and frequency of the exercises, and the recommended number of repetitions for each exercise. The stretching exercises included neck, pectoral wall, upper back, shoulder girdle, ankle flexor and extensor, and knee flexor and extensor muscles. Balance exercises consisted of unilateral standing, tandem walking and unilateral knee bending during standing position. The strengthening exercises aimed to train shoulder girdle muscles, abdominal wall, calf muscles, quadriceps, hip abductor and extensor muscles. Balance exercise was defined in a mild intensity so that participants could maintain an upright position throughout the session, consistent with the description in the institutional program that was used. Strength exercise intensity was determined by calculating one repetition maximum (RM), and low level (8–12 RM) was used [23].
The exercise sessions consisted of a 5-min warm-up period at the beginning and a 5-min cool-down period at the end. The exercise program was not tailored to the functional status of the participants at baseline and was not adjusted during the intervention period. This was the case for both groups. The average duration of the exercise sessions was estimated at thirty minutes, as described in the guide, with 10 repetitions for each movement. Participants in group 1 performed all exercises three days per week at home without supervision. They participated in a group exercise program with 6–8 patients per group, which took place once a week in our clinic under supervision. Group 2 was asked to perform the exercises at home four days per week. To perform the exercises properly, they were motivated and encouraged by a phone call one day per week. They also received support and guidance from the first author as needed.
To improve compliance, all participants were asked to record each completed exercise session on an attendance card weekly and then submit it. They were also warned and informed about potential adverse events such as pain, fatigue, and injury, as well as the risk of falls. Participants were asked to inform the researchers of any adverse events that occurred during the exercise sessions.
Outcome measures
Assessments were made at baseline, eighth week (at the end of the last session), and sixth month. Falls efficacy was the primary outcome of the present study. The Falls Efficacy Scale International (FES-I) is a self-assessment questionnaire designed to measure concern about the possibility of falling during various activities of daily living. A total of sixteen practices and activities performed at home, such as cooking, dressing, bathing, and outside the home, such as visiting, walking on uneven surfaces, or shopping, are scored from 1 to 4 (1 = not at all concerned, 4 = very concerned). The total score ranges from 16 to 64, and the higher the score, the lower the risk of falling [24]. FOF, functional mobility, balance, fall risk, and depression were the secondary outcomes. A visual analog scale (VAS) was used to subjectively measure FOF. Participants were asked to indicate the degree of fear of falling by marking on a 100-mm line (zero; not at all, 100; maximum fear). A new sheet of paper was used at each visit so that participants could not see their previous response to avoid bias. In clinical settings and trials, VAS has been used to measure FOF with moderate validity, and it is suggested that clinicians may prefer VAS to measure FOF [25]. The Timed up and go test (TUGT) was used to assess functional mobility. Participants were asked to walk at their ordinary walking speed during the test. They were seated at the beginning of the test and were asked to stand up from the chair, walk 3 m, turn around, return to the chair, and sit down again. The duration between rising from the chair and sitting down was measured with a stopwatch [26]. Before the test, participants were instructed about the testing procedure, and a test trial was performed for this purpose. The Balance Performance Oriented Mobility Assessment (BPOMA) of Tinetti was used to evaluate balance performance. This test assesses balance while sitting and standing, turning 360°, and the ability to stand up from a chair and sit down. Eight different tasks are scored between 0 and 2. The maximum possible score is 16, with a higher score associated with better balance performance [27]. The Elderly Falls Screening Test (EFST) was used to assess risk of fall. It consists of two parts, one of which queries the number of falls in the past year, history of injurious falls and near falls; the second part assesses walking speed and walking style. The first part is self-reported and covers three items; the second part is scored by assessor and covers two items. Maximum possible score is five. A score between 0 and 1 indicates low, 2–3 moderate, and 4–5 high fall risk [28]. The Geriatric Depression Scale Short Form (GDS-SF) was used to determine depressive symptoms. It includes fifteen dichotomous questions to which participants are asked to answer yes or no. Of the 15 questions, 10 indicate the presence of depression when answered yes, while the remaining five indicate the presence of depression when answered no. An answer in the direction of depression is assumed as one point. To obtain a final score, all points are added together. The total score ranges from 0 to 15. A score between 0 and 5 is normal, while a score above 5 indicates depression [29].
Sample size
A change by > 3 points in FES- I is considered a minimal clinically important difference in elderly adults [30]. Data from independent functionally ambulatory patients in the Turkish FES-I validation study were used to calculate the sample size [31]. We found that a difference of 4 units or more for the FES- I could be detected between two groups of 35 subjects with 80% power and a two-sided type 1 error rate of 0.05% using the values of 26.7 for the mean score and 6.62 for the standard deviation.
Data analyses
IBM SPSS 26.0 Version (IBM Corp., Armonk, NY, USA) was used for data analysis. Descriptive statistics of the study were reported as mean (standard deviation) and median (interquartile range) for normally and nonnormally distributed continuous data, respectively, and as frequencies for categorical variables. The differences between and within groups for primary and secondary outcome scores were tested via type 3 mixed design analysis of variance (ANOVA) using single “between subject” (group) and single “within subject” (time) factors. When the sphericity was violated, the degrees of freedom were corrected using either Huynh–Feldt or Greenhouse and Geisser estimates of sphericity [32]. If a significant effect was found, post hoc tests for pairwise comparisons were performed. Effect sizes were interpreted according to Cohen’s partial eta-squared (ηp2) cut of values; 0.14 or more are large effects, 0.06 or more are medium effects, and 0.01 or more are small effects [33]. Intention-to-treat analysis included all randomized patients. Missing data that occurred in only one patient were imputed by assigning the mean of the series. In addition, per-protocol analysis was performed for sensitivity analysis. Significance was set as p < 0.05.
Results
Seventy-five of 103 recruited patients enrolled in the study. After allocation, group 1 consisted of 37 and group 2 consisted of 38 patients. Only one person was lost to follow-up after baseline evaluation because of transportation problems. There was no participant that lost to follow-up between 8 weeks and 6 months.
The flowchart of the study is shown in Fig. 1. All patients fully adhered to the exercise program for 8 weeks. Baseline demographics and medical characteristics of groups are provided in Table 1. None of the patients reported any adverse effects.
Analysis of variance revealed significant interactions between group and time as well as main effects of time. A significant interaction was found for FES-I [F (1.74, 127.2) = 9.457, p < 0.01], VAS-FOF [F (1.64, 120.1) = 5.785, p = 0.007], TUGT [F (1.15, 83.9) = 10.712, p = 0.001], and BPOMA [F (1.65, 120.9) = 16.275, p < 0.01]. Follow-up of these interactions showed that FES-I, VAS-FOF, TUGT and BPOMA scores at week 8 and month 6 were better than at baseline in both groups. In addition, FES-I, TUGT, and BPOMA scores at week 8 were better than at month 6 in both groups. A significant difference between groups was found only with respect to TUGT; group 1 had better scores than group 2 at 8 weeks and 6 months. The effect sizes of these differences are large. The primary and secondary outcome scores and mean differences between groups are presented in Table 2. GDS- SF [F (1.45, 106.2) = 13.099, p < 0.01] and EFST [F (1.74, 127.6) = 86.403, p < 0.01] showed significant effects only in the time main factor indicating an improvement for the whole sample but not differing at the group level over time. Per-protocol analysis did not differ from the intention-to-treat analysis (data not shown).
Discussion
According to the results of our study, FES-I at week 8 did not differ between groups. The only superiority of supervision was in the TUGT, and the other secondary outcomes did not differ between groups. At month 6, the results were also the same. On the other hand, the primary outcome (FES-I) and additionally the fear of falling (VAS-FOF) and the balance performance (BPOMA) improved in both groups. These improvements were in effect both immediately after intervention, and at sixth month, although a deterioration occurred at the sixth month, except for VAS-FOF. However, it is not possible to attribute these within-group improvements to the interventions since they are uncontrolled observations.
Due to the usage of distinct concepts of our primary outcome in clinical trials, such as fear of falling, falls efficacy, balance confidence, and concern about falling [34], direct comparison of our results with the literature may not be possible. Thus, falls efficacy and FOF are used interchangeably in the literature. A meta-analysis concluded that falls efficacy and FOF are influenced by both physical and psychological issues [12]. Although fall history affects physical activity and provokes activity avoidance, this effect has been reported to be mediated by falls efficacy and social support [35]. Hence, we have paid special attention to measure the effects of an exercise program on falls efficacy and also on FOF in addition to physical variables. Although the physical and psychological improvements observed in the groups in our study were consistent with previous studies [17], the supervision was not superior in psychological variables. To yield favorable results for falls efficacy and FOF, strengthening exercises or only balance training are reported to be successful [17, 36]. To the best of our knowledge, there is no study evaluating effects of minimally supervised exercise program on psychosocial function in older adults. Since improvement in VAS-FOF and FES-I were observed in both groups, we could not attribute this finding to the supervision. However, maintenance of improvement in VAS-FOF at sixth month is noteworthy. A meta-analysis showed that exercise interventions that reduced FOF failed to carry this effect beyond the end of the intervention [34]. On the contrary, in the present study, improvement in VAS-FOF was maintained at sixth month. To attribute this effect to exercise programs, it would be appropriate to test it in future studies with an inactive control group.
It is interesting that in our study minimally supervision added some more gain only for a physical variable (TUGT). Nelson et al. obtained more improvement related to functional performance after a minimally supervised exercise program in comparison with unsupervised one [18]. Lacroix et al. interpret the greater improvement in balance performance in the supervised group as a result of the motivational effect of supervision [1]. Similarly, functional mobility (TUGT) outcomes in favor of group 1 in our study may be explained by stimulator role of supervision for performing exercises in a more qualified fashion.
Considering objective nature of TUGT, even minimal supervision may be assumed as a successful component of program for achieving better functional status. Falls efficacy is supposed to have a major role in predicting behavior and functionality [15]. However, this was not the case in our study. Balance training is defined as an essential part of the rehabilitation program for older adults [37]. Improvement in balance performance was already expected since balance training was taking part in the exercise program in the current study. However, addition of supervision was not superior to home exercise in this regard either.
Our results showed only time main effect for GDS and EFST which are patient reported outcomes. EFST has been shown to bear predictive power for depression [26]. Exercise program either individually or on a group basis can improve depressive symptoms [38] but this was not the case in our study. Improvement in EFST and GDS in total sample, not regarding groups, revealed a need for conduct further studies with larger sample.
Choosing the duration of intervention was challenging, and there is no consensus on the duration of intervention in studies investigating the effectiveness of exercise interventions on falls efficacy. Duration of intervention ranges from 4 to 96 weeks with the mode of 3 times per week for 12 weeks of exercise in studies with proven efficacy [34, 39]. However, in one study, the authors suggested that applying a similar exercise program for 8 weeks instead of 6 months may be associated with better adherence [40]. Therefore, in this study, the authors chose the 8-week intervention duration considering the 4-day-per-week frequency of application, patient compliance, and feasibility.
Schoenfelder et al. proposed that there are some lasting effects even after cessation of an exercise program [16]. Similarly, in our study, the beneficial effect observed in TUGT continued at sixth month. Moreover, the positive within-group changes in FOF observed in both groups at sixth month suggest possible beneficial effects of the treatments, although these are uncontrolled observations. Hence, to recommend participants exercise continuation after the withdrawal of the intervention on their own at home would be better to maintain positive outcomes.
Strengths and limitations
One of the limitations of our study is lack of a third non-intervention arm. This kind of control design was not preferred because of possible bias with regard to intervention groups [41]. In “no care” group, participants are not blinded, beside “no care” may lead to nocebo effect. On the other hand, “usual care” arm may be valuable in order to reveal placebo effect owing to being under care. In addition, an inactive third control arm (e.g., sham intervention) allows interventions to be compared with each other and the contribution they make on their own to be evaluated. This could be the subject of future work. Second, the high adherence rate achieved in this study is most likely due to the personal dedication of the first author and the motivation she generated in the patients. This frequency is usually problematic to be sustained. Third, it is exactly necessary to carry out this kind of studies with larger sample including individuals at different fall risk.
Strengths were mainly the presence of a control group, good compliance to program, no injury and cardiac or musculoskeletal complaint related to the exercise program.
Conclusion
An exercise program combining unsupervised home exercises and supervised group-based exercises improved functional mobility in a group of community-dwelling older adults. The exercise program undertaken in the present study, seems safe, feasible, and beneficial in order to experience a healthy aging process. It would be better to motivate participants to continue exercising after the intervention ends and to conduct studies in which they are followed up for a slightly longer period of time. To make a comment on depression and fall risk would be possible by carrying out studies with larger sample.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable requests.
References
Lacroix A, Kressig RW, Muehlbauer T, Gschwind YJ, Pfenninger B et al (2016) Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: a randomized controlled trial. Gerontology 62(3):275–288. https://doi.org/10.1159/000442087
Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 35(Suppl 2):ii37–ii41. https://doi.org/10.1093/ageing/afl084
Rapp K, Freiberger E, Todd C, Klenk J, Becker C et al (2014) Fall incidence in Germany: results of two population-based studies, and comparison of retrospective and prospective falls data collection methods. BMC Geriatr 14:105. https://doi.org/10.1186/1471-2318-14-105
Halil M, Ulger Z, Cankurtaran M, Shorbagi A, Yavuz BB et al (2006) Falls and the elderly: is there any difference in the developing world? A cross-sectional study from Turkey. Arch Gerontol Geriatr 43(3):351–359. https://doi.org/10.1016/j.archger.2005.12.005
Bjerk M, Brovold T, Skelton DA, Bergland A (2017) A falls prevention program to improve quality of life, physical function and falls efficacy in older people receiving home help services: study protocol for a randomised controlled trial. BMC Health Serv Res 17:559. https://doi.org/10.1186/s12913-017-2516-5
Gschwind YJ, Kressig RW, Lacroix A, Muehlbauer T, Pfenninger B et al (2013) A best practice fall prevention exercise program to improve balance, strength / power, and psychosocial health in older adults: study protocol for a randomized controlled trial. BMC Geriatr 13:105. https://doi.org/10.1186/1471-2318-13-105
Stel VS, Smit JH, Pluijm SM, Lips P (2003) Balance and mobility performance as treatable risk factors for recurrent falling in older persons. J Clin Epidemiol 56(7):659–668. https://doi.org/10.1016/s0895-4356(03)00082-9
Howe TE, Rochester L, Jackson A, Banks PMH, Blair VA (2000) Exercise for improving balance in older people. Cochrane Database of System Rev. https://doi.org/10.1002/14651858.CD004963.pub2
Laybourne AH, Biggs S, Martin FC (2008) Falls exercise interventions and reduced falls rate: Always in the patient’s interest? Age Ageing 37(1):10–13. https://doi.org/10.1093/ageing/afm190
Lamb SE, Jørstad-Stein EC, Hauer K, Becker C (2005) Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 53(9):1618–22. https://doi.org/10.1111/j.1532-5415.2005.53455.x
Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ (1997) Fear of fall and restriction of mobility in elderly fallers. Age Ageing 26(3):189–193. https://doi.org/10.1093/ageing/26.3.189
Jung D, Lee J, Lee SMA (2009) meta-analysis of fear of falling treatment programs for the elderly. West J Nurs Res 31(1):6–16. https://doi.org/10.1177/0193945908320466
Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE (2008) Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 37(1):19–24. https://doi.org/10.1093/ageing/afm169
Cumming RG, Salkeld G, Thomas M, Szonyi G (2000) Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol Med Sci 55(5):M299-305. https://doi.org/10.1093/gerona/55.5.m299
Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI (1994) Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol Med Sci 49(3): M140–7. https://doi.org/10.1093/geronj/49.3.m140
Schoenfelder DP, Rubenstein LM (2004) An exercise program to improve fall-related outcomes in elderly nursing home residents. Appl Nurs Res 17(1):21–31. https://doi.org/10.1016/j.apnr.2003.10.008
Thiamwong L, Suwanno J (2014) Effects of simple balance training on balance performance and fear of falling in rural older adults. Int J Gerontol 8(3):143–146. https://doi.org/10.1016/j.ijge.2013.08.011
Nelson ME, Layne JE, Bernstein MJ, Nuernberger A, Castaneda C et al (2004) The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci 59(2):154–160. https://doi.org/10.1093/gerona/59.2.m154
Ng CACM, Fairhall N, Wallbank G et al (2019) Exercise for falls prevention in community-dwelling older adults: trial and participant characteristics, interventions and bias in clinical trials from a systematic review. BMJ Open Sport Exerc Med 5:e000663. https://doi.org/10.1136/bmjsem-2019-000663
Sjösten N, Vaapio S, Kivelä SL (2008) The effects of fall prevention trials on depressive symptoms and fear of falling among the aged: a systematic review. Aging Ment Health 12(1):30–46. https://doi.org/10.1080/13607860701366079
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40(9):922–935. https://doi.org/10.1111/j.1532-5415.1992.tb01992.x
Pollock ML, Gaesser GA, Butcher JD, Despres J-P, Dishman RK, Franklin B, Ewing Garber C (1998) American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 30(6):975–991. https://doi.org/10.1097/00005768-199806000-00032
Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C et al (2005) Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 34(6):614–619. https://doi.org/10.1093/ageing/afi196
Alice C Scheffer, Marieke J Schuurmans, Nynke vanDijk, Truus van der Hooft, Sophia E de Rooij (2010) Reliability and validity of the visual analogue scale for fear of falling in older persons. J Am Geriatr Soc 58(11):2228–30. https://doi.org/10.1111/j.1532-5415.2010.03105.x.
Podsiadlo D, Richardson S (1991) The Timed “Up&Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34(2):119–126. https://doi.org/10.1111/j.1532-5415.1986.tb05480.x
Cwikel JG, Fried AV, Biderman A, Galinsky D (1998) Validation of a fall-risk screening test, the Elderly Fall Screening Test (EFST), for community-dwelling elderly. Disabil Rehabil 20(5):161–167. https://doi.org/10.3109/09638289809166077
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al (1982-1983) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17(1):37–49. https://doi.org/10.1016/0022-3956(82)90033-4.
Halvarsson A, Franzén E, Ståhle A (2013) Assessing the relative and absolute reliability of the Falls Efficacy Scale-International questionnaire in elderly individuals with increased fall risk and the questionnaire’s convergent validity in elderly women with osteoporosis. Osteoporos Int 24(6):1853–1858. https://doi.org/10.1007/s00198-012-2197-1
Ulus Y, Durmus D, Akyol Y et al (2012) Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Arch Gerontol Geriatr 54:429–433
Girden ER (1992) ANOVA: repeated measures. Newbury Park: CA: Sage Publications. https://doi.org/10.4135/9781412983419
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences, 2nd edn. Lawrence Erlbaum Associates, Publishers, Hillsdale, NJ
Kumar A, Delbaere K, Zijlstra GA, Carpenter H, Iliffe S et al (2016) Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing 45:345–352. https://doi.org/10.1093/ageing/afw036
Schott N, Tietjens M (2019) Exploring the mediating role of social support and fall efficacy on the association of falls on physical activity: A cross-sectional study in an assisted-living population. J Aging Phys Act 27(1):53–60. https://doi.org/10.1123/japa.2017-0378
Brouwer BJ, Walker C, Rydahl SJ, Culham EG (2003) Reducing fear of falling in seniors through education and activity programs: a randomized trial. J Am Geriatr Soc 51(6):829–834. https://doi.org/10.1046/j.1365-2389.2003.51265.x
Youssef EF, Shanb AA (2016) Supervised versus home exercise training programs on functional balance in older subjects. Malays J Med Sci 23(6):83–93. https://doi.org/10.21315/mjms2016.23.6.9
King LA, Wilhelm J, Chen Y, Blehm R, Nutt J, Chen Z, Serdar A (2015) Does group, individual or home exercise best improve mobility for people with Parkinson’s disease? J Neurol Phys Ther. 39(4):204–212. https://doi.org/10.1097/NPT.0000000000000101
Feng C, Adebero T, DePaul VG, Vafaei A, Norman KE, Auais M (2022) A systematic review and meta-analysis of exercise interventions and use of exercise principles to reduce fear of falling in community-dwelling older adults. Phys Ther 102(1):236
Weber M, Belala N, Clemson L, Boulton E, Hawley-Hague H, Becker C, Schwenk M (2018) Feasibility and effectiveness of intervention programmes integrating functional exercise into daily life of older adults: a systematic review. Gerontology 64(2):172–187. https://doi.org/10.1159/000479965
Hróbjartsson A, Gøtzsche PC (2001) Is the placebo powerless? N Engl J Med 344(21):1594–1602. https://doi.org/10.1056/nejm200105243442106
Acknowledgements
There is no acknowledgment.
Funding
No funding was received for conducting this study. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Ayca Avci Trakyali, Taciser Kaya, and Bugra Ince. Statistical analysis were performed by Bugra Ince. The manuscript was written by Taciser Kaya and Bugra Ince, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval and informed consent
This study was performed in accordance with the ethical standards as laid down in the Declaration of Helsinki. Approval was granted by the Ethics Committee of Izmir Bozyaka Training and Research Hospital (Date: 17 Nov, 2011, Meeting no: 02, Decision No: 03). This study was approved by the local ethics committee of our hospital. All the participants gave signed written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avci Trakyali, A., Kaya, T. & Ince, B. Effects of an exercise program combining unsupervised home exercises and supervised group-based exercises on fall-related variables in older adults: a randomized controlled trial. Eur Geriatr Med 14, 59–67 (2023). https://doi.org/10.1007/s41999-022-00724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00724-3