Abstract
Purpose
To provide updated evidence on the association of obstructive sleep apnoea (OSA)/sleep-disordered breathing (SDB) with risk of all-cause cognitive impairment/dementia and Alzheimer’s disease (AD).
Methods
A systematic literature search was done in PubMed, EMBASE and Scopus databases for cohort studies (retrospective or prospective) that documented the association of SDB/OSA with the risk of cognitive impairment or all-cause dementia or AD. Only studies that were published in the year 2000 and onwards were included. The random-effects model was used for all the analyses and effect sizes were reported as hazards ratio (HR) with 95% confidence intervals.
Results
Of 15 studies were included in the meta-analysis, SDB/OSA was diagnosed with at-home polysomnography in six studies, while five studies relied on self-report or questionnaires. In the remaining studies, International Classification of Diseases (ICD) codes determined the diagnosis of SDB. The overall pooled analysis showed that patients with SDB/OSA had higher risk of cognitive impairment and/or all-cause dementia (HR 1.52, 95% CI: 1.32, 1.74), when compared to patients without SDB/OSA. However, when studies with diagnosis of SDB based on polysomnography were pooled together, the strength of association for all-cause cognitive impairment was weaker (HR 1.32, 95% CI: 1.00, 1.74).
Conclusion
Findings suggest a possible association of SDB/OSA with risk of all-cause cognitive impairment and/or dementia. However, careful interpretation is warranted as the majority of the studies did not rely on objective assessment based on polysomnography.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Current evidence indicates that around 2 to 4% of the middle-aged population may be affected by obstructive sleep apnoea/hypopnea (OSA) syndrome [1]. OSA is more prevalent in men and in individuals who are older than 65 years [1]. There is a recent interest in this potentially treatable condition because of its potential association with disorders such as hypertension, diabetes and cardiovascular diseases [2, 3]. A meta-analysis of 17 prospective cohort studies found a link between OSA and a higher risk of cardiovascular diseases (2.48 times higher) and stroke (2 times higher) [2]. Although recent studies suggest the association of OSA with cognitive decline in the elderly, the evidence is still inconclusive. There have been systematic reviews and meta-analyses conducted on the association of sleep disturbances, including OSA or sleep-disordered breathing (SDB), with cognitive decline or dementia but there has been no consistent methodology [4,5,6,7]. Some reviews included cross-sectional studies, which may be potentially biased, whereas others used a combination of all study designs (cross-sectional, case-control, data from randomized controlled trials and cohort-based studies) [4,5,6,7].
A study by Emamian et al. included prospective cohort studies (n = 5) and showed that patients with Alzheimer’s disease (AD) have 5 times higher risk of having OSA than cognitively normal subjects of the same age [5]. Another review by Leng et al. included both prospective and cross-sectional studies and documented, through pooled analysis of prospective studies, that patients with sleep-disordered breathing (SDB) have higher risk of cognitive impairment that those without SDB [4]. Findings from pooled analysis of cross-sectional studies indicated that patients with SDB had lower executive function but there was no effect of SDB on cognition [4]. Furthermore, there are reviews that have proposed an association between OSA/SDB and cognitive decline/dementia based on studies using blood and cerebrospinal biomarkers and brain pathology-based diagnosis. Cui et al. in their meta-analysis indicated abnormal biomarkers of AD in cerebrospinal fluid (CSF) and on brain positron emission tomography (PET) scans in patients with OSA [8]. Their overall analysis showed significantly reduced levels of amyloid-β 42 (Aβ42) and increased total tau (t-tau) levels in cerebro-spinal fluid (CSF), as well as amyloid burden on PET scans in OSA patients, compared to normal subjects [8].
Studies have also differed in their method of diagnosis of OSA/SDB as well as the tools used for cognitive assessments. In view of this significant and substantial heterogeneity between different studies, this review and meta-analysis aimed to provide updated and reliable evidence on the association between SDB/OSA with a cognitive decline and/or a risk of AD. We purposefully decided to include only cohort-based studies and studies that used validated psychometric tools, instead of blood or cerebrospinal fluid or brain tissue related parameters, to assess cognitive decline or dementia or AD.
Methods
Selection of studies
The protocol of the current study was registered at PROSPERO (CRD42023393558). PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed [9]. Table 1 summarizes the search strategy used to systematically search for studies in three databases, i.e. PubMed, EMBASE and Scopus. English language studies published until the 15th of January 2023 were eligible for inclusion.
Studies that documented the association of SDB/OSA with risk of cognitive impairment or all-cause dementia or AD were eligible for inclusion. Specifically, we wanted to include only studies that reported on a clinical diagnosis of cognitive decline or dementia or AD. Therefore, all studies that reported blood or cerebrospinal fluid or brain tissue-related parameters were not considered. We were only interested in studies that had a cohort design. Studies with matched case-control and cross-sectional designs were excluded. We also excluded studies that used data collected as part of a randomized controlled trial. To provide contemporary evidence, we included only those studies that were published in the year 2000 and onwards.
The total number of studies in each of the three databases were identified and duplicates were removed. The title and abstract of the remaining unique studies were reviewed by two study authors independently and further exclusions were made. Following this, the full texts were reviewed by the two authors independently and decisions were made for the final inclusion in the meta-analysis. Any discrepancies were resolved with the help of a senior author.
Data extraction and analysis
Data extraction was done using pre-tested electronic sheet. The extracted data included study identifiers (name of the author, study setting and year of publication), study design, ways in which data on exposure and outcome(s) of interest were collected, characteristics of the study subjects, sample size and key findings. All analyses were conducted using STATA 16 software (TX, USA). We reported pooled effect sizes as hazards ratio (HR) along with 95% confidence intervals. It is important to mention that not all studies reported their effect sizes as hazards ratio and in such instances, we converted the reported effect sizes (either as odds ratio or relative risk) into HR based on the methods reported previously [10, 11]. As an a priori decision, we used random effects model for all analyses. This was done because the included studies differed in the characteristics of the subjects; study setting and design; definitions of SDB/OSA adopted; tools used for exposure and outcomes assessment and duration of follow-up. These differences would have led to substantial heterogeneity in the reported findings.
The Newcastle-Ottawa Scale was used for assessment of the risk of bias [12]. We used Egger’s test along with visual inspection of funnel plot to assess for publication bias [13]. A p-value of less than 0.05 was considered to denote statistical significance. Post hoc subgroup analysis was conducted based on the study design (prospective and retrospective cohort), sex (male and female) and age of the subjects (< 60 years and ≥ 60 years) and assessment method for SDB/OSA (polysomnography and self-reported/ICD coding based).
Results
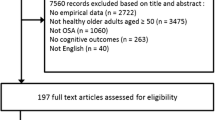
Our search strategy resulted in retrieval of a total of 3726 studies. Duplicates (n = 1386) were removed. Additional studies (n = 2205) were excluded after the title and abstract review. A total of 135 studies were excluded after the full-text review, as summarized in Fig. 1. A total of 15 studies were considered for this meta-analysis [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28].
Characteristics of the included studies
Table 1 presents the specific details of the included studies. Out of included studies (n = 15), seven were prospective cohort and remaining (n = 8) were retrospective cohort studies. The majority of the studies were done in the USA (n = 9). Two each were conducted in Taiwan and the Republic of Korea. Out of the remaining two studies, one was conducted in France and the other one was multicentric. In most of the studies, there were significant differences in baseline characteristics between patients with sleep-disordered breathing (SDB) and those without SDB. Subjects with SBD had higher mean body mass index and increased prevalence of comorbidities such as coronary artery disease, hypertension, diabetes, previous history of stroke, depression and anxiety. The mean follow-up period ranged from 3.4 to 15 years in all included studies. There were significant variations in the tools used for neuropsychological/cognitive assessments, specific aspects that were assessed (e.g., logical memory, global cognition, dementia, language, executive functions), and in the way, cognitive impairment was defined (Table 2). At-home polysomnography was used for establishing the diagnosis of SBD/sleep apnoea in six studies. Apnoea was self-reported or assessed using questionnaire in five studies. In the remaining studies, diagnosis of SDB was based on the International Classification of Diseases (ICD) codes (Table 2). The quality assessment has been presented in supplementary tables 2 and 3. All studies were of good quality.
Findings from pooled analysis
The pooled findings indicate that patients with sleep-disordered breathing (SDB) had higher risk of all-cause cognitive impairment and/or all-cause dementia (HR 1.52, 95% CI: 1.32, 1.74; N = 15, I2 = 71.9%), when compared to patients without SDB (Figure 2). No publication bias was detected on Egger’s test (P = 0.37) or on the visual inspection of the funnel plot (Supplementary figure 1). SDB patients had higher risk of AD (HR 1.39, 95% CI: 1.17, 1.66; N = 6, I2 = 21.4%), compared to those without SDB (Figure 3). There was no publication bias (P = 0.83) (Supplementary figure 2).
The risk of all-cause cognitive impairment and/or all-cause dementia was higher in both males (HR 1.38, 95% CI: 1.15, 1.66; N = 6, I2 = 82.3%) and females (HR 2.08, 95% CI: 1.57, 2.76; N = 4, I2 = 0.0%) with SDB, compared to males and females without SDB (Table 2). Pooling of findings from both prospective cohort (HR 1.31, 95% CI: 1.06, 1.61; N = 7, I2 = 51.1%) and retrospective cohort studies (HR 1.74, 95% CI: 1.42, 2.12; N = 8, I2 = 80.8%) showed a higher risk of SDB with all-cause cognitive impairment and/or all-cause dementia (Table 2). A higher risk of all-cause cognitive impairment with SDB was observed among patients younger than 60 years (HR 3.30, 95% CI: 1.68, 6.48; N = 2, I2 = 15.3%) and for those ≥ 60 years (HR 2.40, 95% CI: 1.65, 3.48; N = 2, I2 = 37.2%) (Table 2). When studies with diagnosis of SDB based on polysomnography were pooled together, the strength of association between SDB and all-cause cognitive impairment was weaker (HR 1.32, 95% CI: 1.00, 1.74; N = 6, I2 = 60.1%) compared to studies with diagnosis of SDB based on patient reports or ICD based codes (HR 1.65, 95% CI: 1.39, 1.96; N = 2, I2 = 37.2%) (Table 2).
Discussion
Meta-analysis found that presence of SDB/OSA was significantly associated with the risk of all-cause cognitive impairment and/or all-cause dementia and AD. The risk of cognitive impairment and/or all-cause dementia was higher in both men and women with SDB/OSA, compared to men and women without SDB/OSA. Studies with polysomnography-based diagnosis of SDB/OSA had a weaker strength of association with cognitive impairment compared to studies with diagnosis of SDB based on patient reports or ICD based codes. The findings are similar to those of previous reviews. Leng et al., through pooled analysis of prospective studies, observed that patients with SDB had 26% higher chance of developing cognitive impairment compared to patients without SDB [4]. Emamian et al. included prospective cohort studies (n = 5) with a sample size of 236 subjects and that found that patients with AD were 5 times more at risk of having OSA than cognitively normal subjects of the same age [5].
Our current limited understanding on the factors linking SDB/OSA with cognitive decline and/or dementia suggests a multi-factorial causation [29]. The current view is that the immediate effects of SDB/OSA such as hypoxemia and sleep fragmentation may cause neuronal injury and thereby affect memory, attention and executive functions [29,30,31,32]. Hypoxemia is also proposed to accelerate cognitive ageing [30, 32]. Brain hypoperfusion, commonly seen in SDB/OSA, has also been linked to the underlying pathological process leading to dementia/AD [33] through mechanism that involves hypoperfusion-induced chronic hypoxemia that accelerates the progression of cerebral small vessel disease [34, 35]. This, in turn, leads to lesions in white matter, lacunar infarcts, loss of grey matter and white matter fibre abnormalities [32,33,34,35,36,37]. Additional concern is the development of intermittent hypoxaemia and altered sleep architecture (such as sleep fragmentation and adverse impact on REM sleep) that lead to metabolic derangements, oxidative stress, inflammation and blood-brain barrier dysfunction [32]. These processes together lead to reduced neurogenesis, decreased plasticity, development of microinfarcts, changes in grey and white matter and cerebral neuronal networks [32, 38, 39]. Studies have also shown increased accumulation of amyloid plaques and hyperphosphorylated tau protein in brain of patients with SDA/OSA [40, 41].
Studies have shown that obstructive sleep apnoea could be associated with higher scores on depression and anxiety scales when compared to individuals without this condition [42,43,44]. It is crucial to recognize that these mood changes can have significant repercussions on cognitive performance. These mood disturbances may result in difficulties with concentration, memory and decision-making, all of which are essential components of cognitive functioning. Moreover, individuals experiencing depression and anxiety often report reduced motivation and energy levels, further contributing to cognitive impairment. Therefore, consideration of the possible presence of affective disorders, such as depression and anxiety, among OSA patients and their potentially adverse impact cognitive performance is important.
SDB/OSA is a potentially treatable condition. Therefore, its timely management can potentially lead to a reduced risk of cognitive decline. Sonia et al. conducted a randomized controlled trial to examine whether the treatment with continuous positive airway pressure (CPAP) leads to better cognitive function in AD patients with OSA [45]. The study found an improvement in the neuropsychological scores in intervention group that received therapeutic CPAP, compared to those that received placebo CPAP. However, the study was small and involved only 52 mild to moderate AD/OSA patients. Similarly, Troussiere et al. evaluated annual mini-mental state examination (MMSE) score decline in patients with mild to moderate AD (n = 23), based on whether the subjects received CPAP therapy or not [46]. The study found significantly lower decline in the group of patients that received CPAP therapy. Kushida et al. conducted a two arm, double-blinded randomized controlled (RCT) with the aim to understand the cognitive effects of CPAP therapy in patients with documented OSA [47]. The authors found a small and transient improvement in some measures of executive function with the use of CPAP, especially in cases of severe OSA. A meta-analysis of RCTs (n = 14) by Wang et al. demonstrated partial improvement of cognitive impairment in patients with severe OSA after the CPAP treatment [48]. In a large retrospective study that utilized Medicare claims, data of around 50,0000 beneficiaries that were aged older than 65 years found CPAP treatment to be associated with lower risk of incident AD [49]. However, there are studies that have also shown no beneficial effect of CPAP on cognitive scores [50, 51]. Furthermore, while CPAP is the most widely used management for SDB/OSA and evidence is overall supportive of its role in reducing the risk of cognitive impairment, there is still a need to identify and test other treatment modalities and their effect on cognitive performance in patients with SDB/OSA.
There are certain limitations of the current review. First, in some of the studies, either ICD-based codes for SDB/OSA were employed, or self-reported and questionnaire-based assessments of apnoea were utilized. The absence of a direct, objective assessment method in these instances may have introduced bias into the analysis. For the same reason, we were also unable to conduct stratified analysis based on the severity of SDB. Second, we acknowledge that deriving hazard ratios (HR) from either odds ratios or relative risks using statistical methods may entail some degree of imprecision. Nevertheless, our primary objective was to maximize the utilization of available data and extract the most insights possible. Third, our findings were only focused on the risk of cognitive impairment/decline (as categorical/dichotomous outcome) and we were unable to analyse continuous cognitive scores. The main reason was that the included studies considered different cognitive outcomes and used different tools for assessment, thereby posing challenge to derive meaningful estimates. Even for the risk of cognitive impairment/decline, the studies used different cutoffs that corresponded to a wide range of interpretation, i.e. from mild to severe cognitive impairment. Therefore, we presented our findings as risk of all-cause cognitive impairment/decline. Fourth, in most of the included studies, there were baseline differences in the characteristics of subjects with and without SDB/OSA. We think that the associations observed in our analysis may be influenced by these differences, to some extent. Fifth, there were some studies in our review that had retrospective cohort designs and therefore may not have collected data to allow for adjustment for important confounders.
Conclusion
The findings of the current meta-analysis indicate a possible association of SDB/OSA with risk of all-cause cognitive impairment and/or dementia. However, it is important to note that the majority of the studies in our review did not rely on objective assessment of SDB/OSA based on polysomnography. Therefore, careful interpretation regarding the strength and significance of the observed association is advised. Furthermore, there is a possibility that unmeasured confounders may influence or mediate this association. Consequently, future studies should identify and consider adjustments for important confounders such as hypertension, diabetes, obesity, low physical activity, history of traumatic brain injury or respiratory diseases, smoking, alcohol use and depression.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
None.
References
Jennum P, Riha RL (2009) Epidemiology of sleep apnoea/hypopnoea syndrome and sleep-disordered breathing. Eur Respir J 33:907–914. https://doi.org/10.1183/09031936.00180108
Dong J-Y, Zhang Y-H, Qin L-Q (2013) Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis 229:489–495. https://doi.org/10.1016/j.atherosclerosis.2013.04.026
Fallahi A, Jamil DI, Karimi EB et al (2019) Prevalence of obstructive sleep apnea in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab Syndr 13:2463–2468. https://doi.org/10.1016/j.dsx.2019.06.030
Leng Y, McEvoy CT, Allen IE, Yaffe K (2017) Association of sleep-disordered breathing with cognitive function and risk of cognitive impairment: a systematic review and meta-analysis. JAMA Neurol 74:1237–1245. https://doi.org/10.1001/jamaneurol.2017.2180
Emamian F, Khazaie H, Tahmasian M et al (2016) The association between obstructive sleep apnea and Alzheimer’s disease: a meta-analysis perspective. Front Aging Neurosci 8:78. https://doi.org/10.3389/fnagi.2016.00078
Shi L, Chen S-J, Ma M-Y et al (2018) Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev 40:4–16. https://doi.org/10.1016/j.smrv.2017.06.010
de Almondes KM, Costa MV, Malloy-Diniz LF, Diniz BS (2016) Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res 77:109–115. https://doi.org/10.1016/j.jpsychires.2016.02.021
Cui W, Duan Z, Li Z, Feng J (2022) Assessment of Alzheimer’s disease-related biomarkers in patients with obstructive sleep apnea: a systematic review and meta-analysis. Front Aging Neurosci 14:902408. https://doi.org/10.3389/fnagi.2022.902408
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71. https://doi.org/10.1136/bmj.n71
Tierney JF, Stewart LA, Ghersi D et al (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16. https://doi.org/10.1186/1745-6215-8-16
Parmar MK, Torri V, Stewart L (1998) Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 17:2815–2834. https://doi.org/10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8
Ottawa Hospital Research Institute. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 8 Feb 2023
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Tsai M-S, Li H-Y, Huang C-G et al (2020) Risk of Alzheimer’s disease in obstructive sleep apnea patients with or without treatment: real-world evidence. The Laryngoscope 130:2292–2298. https://doi.org/10.1002/lary.28558
Lee JE, Yang SW, Ju YJ et al (2019) Sleep-disordered breathing and Alzheimer’s disease: a nationwide cohort study. Psychiatry Res 273:624–630. https://doi.org/10.1016/j.psychres.2019.01.086
Blackwell T, Yaffe K, Laffan A et al (2015) Associations between sleep-disordered breathing, nocturnal hypoxemia, and subsequent cognitive decline in older community-dwelling men: the Osteoporotic Fractures in Men Sleep Study. J Am Geriatr Soc 63:453–461. https://doi.org/10.1111/jgs.13321
Chang W-P, Liu M-E, Chang W-C et al (2013) Sleep apnea and the risk of dementia: a population-based 5-year follow-up study in Taiwan. PLoS One 8:e78655. https://doi.org/10.1371/journal.pone.0078655
Lutsey PL, Bengtson LGS, Punjabi NM et al (2016) Obstructive sleep apnea and 15-year cognitive decline: the Atherosclerosis Risk in Communities (ARIC) Study. Sleep 39:309–316. https://doi.org/10.5665/sleep.5434
Martin MS, Sforza E, Roche F et al (2015) Sleep breathing disorders and cognitive function in the elderly: an 8-year follow-up study. the proof-synapse cohort. Sleep 38:179–187. https://doi.org/10.5665/sleep.4392
Yaffe K, Laffan AM, Harrison SL et al (2011) Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 306:613–619. https://doi.org/10.1001/jama.2011.1115
Yaffe K, Nettiksimmons J, Yesavage J, Byers A (2015) Sleep quality and risk of dementia among older male veterans. Am J Geriatr Psychiatry 23:651–654. https://doi.org/10.1016/j.jagp.2015.02.008
Sharafkhaneh A, Giray N, Richardson P et al (2005) Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 28:1405–1411. https://doi.org/10.1093/sleep/28.11.1405
Lutsey PL, Misialek JR, Mosley TH et al (2018) Sleep characteristics and risk of dementia and Alzheimer’s disease: the Atherosclerosis Risk in Communities Study. Alzheimers Dement 14:157–166. https://doi.org/10.1016/j.jalz.2017.06.2269
Osorio RS, Gumb T, Pirraglia E et al (2015) Sleep-disordered breathing advances cognitive decline in the elderly. Neurology 84:1964–1971. https://doi.org/10.1212/WNL.0000000000001566
Ding X, Kryscio RJ, Turner J et al (2016) Self-reported sleep apnea and dementia risk: findings from the prevention of Alzheimer’s disease with vitamin E and selenium trial. J Am Geriatr Soc 64:2472–2478. https://doi.org/10.1111/jgs.14393
Choe YM, Suh G-H, Kim JW, Alzheimer’s Disease Neuroimaging Initiative (2022) Association of a history of sleep disorder with risk of mild cognitive impairment and Alzheimer’s disease dementia. Psychiatry Investig 19:840–846. https://doi.org/10.30773/pi.2022.0176
Agudelo C, Ramos AR, Sun X et al (2022) Sleep-disordered breathing risk with comorbid insomnia is associated with mild cognitive impairment. Appl Sci 12:2414. https://doi.org/10.3390/app12052414
Bubu OM, Pirraglia E, Andrade AG et al (2019) Obstructive sleep apnea and longitudinal Alzheimer’s disease biomarker changes. Sleep 42:zsz048. https://doi.org/10.1093/sleep/zsz048
Barletta P, Abreu AR, Ramos AR et al (2019) Role of obstructive sleep apnea in cognitive impairment. Int J Head Neck Surg 10:57–61. https://doi.org/10.5005/jp-journals-10001-1373
Jackson ML, Howard ME, Barnes M (2011) Cognition and daytime functioning in sleep-related breathing disorders. Prog Brain Res 190:53–68. https://doi.org/10.1016/B978-0-444-53817-8.00003-7
Rosenzweig I, Williams SCR, Morrell MJ (2014) The impact of sleep and hypoxia on the brain: potential mechanisms for the effects of obstructive sleep apnea. Curr Opin Pulm Med 20:565–571. https://doi.org/10.1097/MCP.0000000000000099
Gosselin N, Baril A-A, Osorio RS et al (2019) Obstructive sleep apnea and the risk of cognitive decline in older adults. Am J Respir Crit Care Med 199:142–148. https://doi.org/10.1164/rccm.201801-0204PP
Yan L, Park HR, Kezirian EJ et al (2021) Altered regional cerebral blood flow in obstructive sleep apnea is associated with sleep fragmentation and oxygen desaturation. J Cereb Blood Flow Metab 41:2712–2724. https://doi.org/10.1177/0271678X211012109
Raptis DG, Sinani O, Rapti GG et al (2021) Clinically silent small vessel disease of the brain in patients with obstructive sleep apnea hypopnea syndrome. Diagnostics (Basel) 11:1673. https://doi.org/10.3390/diagnostics11091673
Kepplinger J, Barlinn K, Boehme AK et al (2014) Association of sleep apnea with clinically silent microvascular brain tissue changes in acute cerebral ischemia. J Neurol 261:343–349. https://doi.org/10.1007/s00415-013-7200-z
Wennberg AMV, Wu MN, Rosenberg PB, Spira AP (2017) Sleep disturbance, cognitive decline, and dementia: a review. Semin Neurol 37:395–406. https://doi.org/10.1055/s-0037-1604351
Daulatzai MA (2015) Evidence of neurodegeneration in obstructive sleep apnea: relationship between obstructive sleep apnea and cognitive dysfunction in the elderly. J Neurosci Res 93:1778–1794. https://doi.org/10.1002/jnr.23634
Meerlo P, Mistlberger RE, Jacobs BL et al (2009) New neurons in the adult brain: the role of sleep and consequences of sleep loss. Sleep Med Rev 13:187–194. https://doi.org/10.1016/j.smrv.2008.07.004
Cirelli C (2013) Sleep and synaptic changes. Curr Opin Neurobiol 23:841–846. https://doi.org/10.1016/j.conb.2013.04.001
Liguori C, Mercuri NB, Izzi F et al (2017) Obstructive sleep apnea is associated with early but possibly modifiable Alzheimer’s disease biomarkers changes. Sleep:40. https://doi.org/10.1093/sleep/zsx011
Sharma RA, Varga AW, Bubu OM et al (2018) Obstructive sleep apnea severity affects amyloid burden in cognitively normal elderly. A longitudinal study. Am J Respir Crit Care Med 197:933–943. https://doi.org/10.1164/rccm.201704-0704OC
Kim J-Y, Ko I, Kim D-K (2019) Association of obstructive sleep apnea with the risk of affective disorders. JAMA Otolaryngol Head Neck Surg 145:1020–1026. https://doi.org/10.1001/jamaoto.2019.2435
Gupta MA, Simpson FC (2015) Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med 11:165–175. https://doi.org/10.5664/jcsm.4466
Li M, Zou X, Lu H et al (2023) Association of sleep apnea and depressive symptoms among US adults: a cross-sectional study. BMC Public Health 23:427. https://doi.org/10.1186/s12889-023-15358-8
Ancoli-Israel S, Palmer BW, Cooke JR et al (2008) Cognitive effects of treating obstructive sleep apnea in Alzheimer’s disease: a randomized controlled study. J Am Geriatr Soc 56:2076–2081. https://doi.org/10.1111/j.1532-5415.2008.01934.x
Troussière A-C, Charley CM, Salleron J et al (2014) Treatment of sleep apnoea syndrome decreases cognitive decline in patients with Alzheimer’s disease. J Neurol Neurosurg Psychiatry 85:1405–1408. https://doi.org/10.1136/jnnp-2013-307544
Kushida CA, Nichols DA, Holmes TH et al (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep 35:1593–1602. https://doi.org/10.5665/sleep.2226
Wang M-L, Wang C, Tuo M et al (2020) Cognitive effects of treating obstructive sleep apnea: a meta-analysis of randomized controlled trials. J Alzheimers Dis 75:705–715. https://doi.org/10.3233/JAD-200088
Dunietz GL, Chervin RD, Burke JF et al (2021) Obstructive sleep apnea treatment and dementia risk in older adults. Sleep 44:zsab076. https://doi.org/10.1093/sleep/zsab076
Skiba V, Novikova M, Suneja A et al (2020) Use of positive airway pressure in mild cognitive impairment to delay progression to dementia. J Clin Sleep Med 16:863–870. https://doi.org/10.5664/jcsm.8346
Schwartz M, Acosta L, Hung Y-L et al (2018) Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath 22:555–568. https://doi.org/10.1007/s11325-017-1590-6
Author information
Authors and Affiliations
Contributions
Q.T. and J.L. designed the project; Q.T., J.S., X.L., J.L., H.Z., J.D. and J.L. were involved in data collection and data analysis; Q.T. and J.L. prepare the manuscript; J.L. edit the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent to participate
None.
Consent to publish
None.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information

Supplementary figure 1
Funnel plot for risk of cognitive impairment and/or all-cause dementia among those with and without sleep disordered breathing (SDB)

Supplementary figure 2
Funnel plot for risk of Alzheimer’s disease among those with and without sleep disordered breathing (SDB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tian, Q., Sun, J., Li, X. et al. Association between sleep apnoea and risk of cognitive impairment and Alzheimer’s disease: a meta-analysis of cohort-based studies. Sleep Breath 28, 585–595 (2024). https://doi.org/10.1007/s11325-023-02934-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02934-w