Abstract
Purpose
This meta-analysis was conducted to assess the effects of telemedicine interventions on continuous positive airway pressure (CPAP) adherence in patients with obstructive sleep apnoea (OSA).
Methods
The PubMed, Cochrane Library, OVID, Web of Science and EBSCO host databases were searched from January 2004 to February 2020 for randomised controlled trials (RCTs) that assessed the effects of telemedicine interventions on CPAP adherence in patients with OSA. The study inclusion criteria were RCTs that compared patients who received telemedicine interventions with a control group and reported a change in CPAP adherence. The primary outcome was the improvement in CPAP adherence.
Results
In total, there were 11 RCTs (n = 1358) with quantitative analyses. Intervention times ranged from 1 to 6 months. Compared to controls, the telemedicine group exhibited better adherence to CPAP therapy (pooled mean difference (MD) = 0.57, 95% CI = 0.33 to 0.80, I2 = 7%, p < 0.00001). We performed sensitivity analyses by the type of telemedicine intervention, comorbidity burden, and OSA severity to explore whether or not their effect sizes may have affected the time of CPAP application. We performed subgroup analyses by follow-up duration, age, and OSA Epworth sleepiness scale (ESS) symptoms to determine if their effect sizes may have affected the time of CPAP application. However, these analyses did not change the statistical significance of the pooled estimate.
Conclusions
The use of telemedicine for up to 6 months may enhance CPAP adherence in patients with OSA, when compared to no intervention. Our study was searched from January 2004 to February 2020 for randomised controlled trials (RCTs) that assessed the effects of telemedicine interventions on CPAP adherence in patients with OSA. Future studies can continue to search for articles after February 2020
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnoea (OSA) refers to repeated episodes of partial or complete upper airway obstruction during sleep, leading to a significant reduction or complete interruption of airflow, which can cause intermittent disturbances of gas exchange such as hypercapnia and hypoxemia, as well as large fluctuations in blood pressure and fragmented sleep [1]. OSA clinical symptoms include snoring, apnoea, morning headache, dry mouth after waking, daytime sleepiness, etc. [2], which may contribute to risk of stroke, coronary heart disease, arrhythmia, hypertension, and increased cardiovascular mortality [3]. Multiorgan damage makes OSA an economic burden for society [1]. One study reported that OSA afflicts nearly 30 million adults in the USA, and its cost in 2015 was approximately $US 12.4 billion [4]. OSA has strong negative effects on families and society, so treating patients with OSA is very important.
Continuous positive airway pressure (CPAP) is the optimal treatment for OSA [5]. A meta-analysis found that CPAP can improve OSA patients’ sleep quality [6]. CPAP may reduce the risk of cardiovascular complications and reduce the mortality of patients with severe obstructive sleep apnoea-hypopnoea syndrome (OSAHS) [7, 8]. Some studies have defined good CPAP adherence as use for at least 4 h per night and for more than 70% of nights [9] for the average daily CPAP treatment time within 1 month [10]. However, adherence to CPAP in patients with OSA is low. One study indicated that 25–50% of patients with OSAH patients had poor adherence to CPAP [11]. Another study reported that at 3 months of treatment, the rate of adherence was only 60% [12]. Lack of adherence to CPAP may cause complications that affect patients’ quality of life and put great pressure on healthcare workers. A solution to this problem is needed. Some studies have found that telemedicine improves adherence to treatment in patients with chronic diseases [13, 14].
Telemedicine is defined as using telecommunications technology (such as a wireless modem, computer-based telecommunications system, or smartphone application) to provide health service information remotely and achieve remote communication between patients and medical staff [15]. The use of telemedicine to manage patients with OSA has been reported [16, 17]. However, the effects of telemedicine interventions on CPAP use in patients with OSA remain controversial. Some studies have reported that telemedicine interventions improve CPAP adherence in these patients [18,19,20], while other studies have found that they do not [21,22,23].
Because of these different findings, it is difficult to judge whether or not telemedicine interventions can improve CPAP adherence in patients with OSA. Therefore, we conducted a meta-analysis of randomised controlled trials (RCTs) to evaluate if telemedicine can improve CPAP compliance.
Methods
Our study had registered with the International Prospective Register of Systematic Reviews (PROSPERO), number CRD42020201043.
Literature search strategy
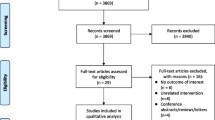
An electronic database search (including web platforms for registration of clinical trials) from January 2004 to February 2020 was performed using PubMed, the Cochrane Library, OVID, Web of Science, and EBSCO host. The following search terms were used: telemedicine OR telehealth OR e-health OR mobile health OR mobile application OR mobile apps OR Internet OR computer OR videoconferencing OR video recording OR telecommunication OR tele-management OR remote OR and sleep disordered breathing OR sleep apnea syndromes OR obstructive sleep apnea, sleep disordered breathing (OSA) and continuous Positive Airway Pressure OR CPAP and Random OR Randomized controlled trials (RCTs) (Fig. 1).
Study selection
Inclusion criteria were as follows:
-
(1)
Patients were adults (age 18 years or older).
-
(2)
Patients could use telemedicine intervention equipment (such as telephone, computerised systems for information exchange, Internet, etc.).
-
(3)
Patients had been diagnosed with OSA [24], mainly based on medical history, signs, and polysomnography (PSG) results. Symptoms such as characteristic sounds, repeated sleep apnoea, superficial breathing, intermittent hypoxemia, and daytime sleepiness were present. PSG monitoring revealed that during 7 hours of sleep, incidents of apnoea were repeated ≥ 30 times, or the apnoea-hypopnoea index (AHI) was greater than or equal to 5 times/h.
-
(4)
Patients were initiating or using CPAP therapy for OSA.
-
(5)
Data were available on CPAP average usage per day (time/night) or mean adherence (minute per day).
-
(6)
The study design was a randomised control trial and follow-up time was greater or equal to 1 month.
Exclusion criteria were as follows:
-
(1)
The study design was not a randomised controlled trial (RCT).
-
(2)
Patients could not use the telemedicine system and CPAP equipment.
-
(3)
Duplicate publications.
-
(4)
Incomplete data or no related outcomes.
Assessment of risk of bias
Two researchers independently screened the articles for inclusion and exclusion criteria. When there were differences of opinion, a third researcher was consulted to resolve disagreements. The Cochrane Collaboration’s tool [25] was used to evaluate the quality of the screened articles. If the study fully met the standard content of 7 items, the quality level was A; if the standards were partially met, the quality level was B; and if the standards were not at all met, the quality level was C.
Statistical analyses
The primary outcome was the improvement in CPAP adherence. Review Manager 5.3 software was used for this study for statistical analyses. The mean difference (MD) with 95% CI was used to pool continuous variable outcomes. Study heterogeneity was evaluated using the Cochran Q statistic and I2 statistic. When the p value was > 0.05 and I2 was < 50%, a fixed effects model was used; otherwise, a random effects model was used. When the value of I2 was > 50% which is considered highly heterogeneous, subgroup analyses and sensitivity analyses will be used to analyze heterogeneity.
Results
Search results
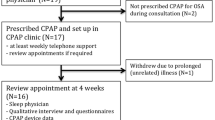
Figure 1 presents the process of search and selection. In total, 1067 articles were found: 66 from the Cochrane Library, 4 from Web of Science, 43 from Ovid, 930 from PubMed and 24 from the EBSCO host. Only 11 articles met the inclusion and exclusion criteria [26,27,28,29,30,31,32,33,34,35,36] (Fig. 1).
Study characteristics
Tables 1 and 2 summarise the characteristics of the 11 studies [26,27,28,29,30,31,32,33,34,35,36]. This meta-analysis included study data from 1440 patients (telemedicine group n = 678; control group n = 680). Of the 11 studies, 6 were conducted in the USA, 2 in Spain and 1 each in Canada, France and Belgium. The intervention duration ranged from 1 to 6 months. The total number of participants ranged from 15 to 126 in the telemedicine groups and from 15 to 129 in the control groups. The mode of positive airway pressure was CPAP (see Table 1). Telemedicine interventions included a web platform, a universal telemonitoring unit, a computer-based telecommunications system and others (see Table 2). Most interventions involved patients using a telemedicine device to transmit data (CPAP time, mask leak, apnoea-hypopnoea index (AHI) and other OSA data) to the researchers’ website, with the research team contacting patients to provide appropriate guidance or to set up a visit with a researcher if the data were abnormal (Table 2).
Risk-of-bias assessment
In 11 studies selected for this meta-analysis, 82% (9 of 11) presented adequate random sequence generation; 36% (4 of 11) reported allocation concealment; 0% (0 of 11) met the criteria of blinding of participants and personnel; 9% blinded assessment of outcomes (1 of 11); and 73% presented incomplete outcome data (8 of 11). The methodological quality summary is shown in Table 3.
Meta-analysis of CPAP adherence
CPAP adherence was the main outcome. All 11 studies [26,27,28,29,30,31,32,33,34,35,36] (n = 1358) reported that the use of telemedicine interventions significantly improved CPAP adherence when compared to controls (pooled MD = 0.57; 95% CI = 0.33 to 0.80; I2 = 7%; P < 0.00001; see Fig. 2).
Results of sensitivity analyses
Sensitivity analyses by type of telemedical intervention
Four types of telemedical intervention were used in the 11 studies: computer software (n = 2, 18%), Internet-based monitoring systems (n = 5, 46%), wireless modems (n = 3, 27%) and a smart device (n = 1, 9%). We performed sensitivity analyses to explore if the types of intervention were important in terms of effect sizes on the timing of CPAP use. We sequentially omitted individual studies. The pooled weighted mean difference ranged from 0.52 (95% CI 0.28 to 0.76) to 0.62 (95% CI 0.37 to 0.86). This analysis did not change the statistical significance of the pooled estimate.
Sensitivity analyses by comorbidity burden
Of the 11 studies, 1 [33] described the OSA comorbidities; the other 10 did not. Therefore, we performed sensitivity analyses after omitting that study to explore whether or not heterogeneity was evident. The heterogeneity was MD = 0.52, 95% CI = 0.28 to 0.76; I2 = 0%; p < 0.0001. When we sequentially omitted the other studies individually, the pooled estimate did not affect the statistical significance.
Sensitivity analyses by severity of OSA
The OSA classification of the 2013 American College of Physicians (ACP) adult OSA management guidelines is as follows: no OSA, AHI < 5/h; mild OSA, 5/h < AHI < 15/h; moderate OSA, 15/h < AHI < 30/h; and severe OSA, AHI > 30/h [37]. Of the 11 studies, only one [36] dealt with severe OSA. The other studies did not specify OSA classifications. We performed sensitivity analyses omitting that single study to explore whether or not OSA severity affected CPAP use. The heterogeneity was low (I2 < 50%). The statistical significance of the pooled estimate was not affected.
Results of subgroup analyses
We performed subgroup analyses by follow-up duration, age, and ESS scores.
Subgroup analyses by follow-up duration
When we compared patients on CPAP therapy for 1 to 3 months (8 studies, 751 patients) and 4 to 6 months (3 studies, 607 patients), the heterogeneities were low (MD = 0.61, 95% CI = 0.30 to 0.92; I2 = 25%; p < 0.0001,vs. MD = 0.50, 95% CI = 0.14 to 0.86; I2 = 0%; p = 0.006, Fig. 3). The statistical significance of the pooled estimate was not affected.
Subgroup analyses for ages
The second subgroup analysis stratified ages; in one study, 36 were excluded, because its data cannot be merged. We found that patients less than 50 years old OSA patients use CPAP (3 studies, 398 patients) versus more than 50 years old use CPAP (7 studies, 673patients) demonstrated that the heterogeneity were (MD = 0.47, 95% CI = 0.02 to 0.92; I2 = 13%; p = 0.04, vs. MD = 0.69, 95% CI = 0.36 to 1.02; I2 = 28%; p < 0.0001, Fig. 4). This result found that ages have small heterogeneity (I2 < 50%), and the results did not affect OSA patients use CPAP.
Subgroup analyses by ESS score
Six of the eleven studies used the ESS to evaluate daytime sleepiness. We subjected the ESS scores to subgroup analyses. We found that use/non-use of the ESS (6 studies, 955 patients; 5 studies, 403 patients, respectively) was associated with low heterogeneity (MD = 0.62, 95% CI = 0.34 to 0.91; I2 = 0%; p < 0.0001, vs. MD = 0.45, 95% CI = 0.05 to 0.86; I2 = 30%; p = 0.03, Fig. 5). The use of CPAP therapy was not affected.
Publication bias
A funnel plot showed symmetric distribution of data around the average, which suggested the absence of publication bias (Fig. 6).
Discussion
This meta-analysis of 11 studies [26,27,28,29,30,31,32,33,34,35,36] with 1358 patients revealed that telemedicine interventions may improve CPAP adherence in patients with OSA compared to no intervention.
Using the 11 studies, we performed sensitivity analyses by the type of telemedical intervention, comorbidity burden and OSA severity. We performed subgroup analyses by follow-up duration, age and use of the ESS. We found nothing to suggest that telemedicine was inappropriate. The among-study heterogeneities were small; telemedicine improved adherence with CPAP therapy. Poor adherence with CPAP therapy has been associated with certain patient characteristics (such as age), disease characteristics (symptom severity), side effects of CPAP use (skin irritation, dry nose or mouth), titration procedures and psychosocial factors (mental health issues, self-perceived efficacy and social support) [38,39,40,41]. Faced with these problems, what can physicians and nurses do? Patient characteristics cannot be changed. CPAP side effects, treatment titration procedures and psychosocial factors may receive intervention. A study on the effects of telemedicine intervention on CPAP side effects in patients with OSA found that only dry mouth was statistically significant (p < 0.05) [30]. Other side effects such as frequent awakenings, discomfort, and difficulty falling asleep were not significant (p > 0.05) [30]. The sample sizes were only 28 in the telemedicine group and 26 in the control group. The follow-up time was 3 months. Future studies should enroll larger sample sizes and extend the follow-up time [30]. Gentina found that marriage quality and partner engagement affected nightly CPAP use and, thus, adherence to therapy [42]. One study found that the support of and frequent interaction with a partner improved program satisfaction and increased CPAP use after 90 days of treatment compared to usual care [43].
CPAP can decrease apnoea-hypopnoea index (AHI) and improve sleep quality [44]. One study that analysed the effects of CPAP treatment in patients with OSA with various levels of adherence found that sleep quality and blood pressure improved more with good adherence [45]. Two studies found that OSA patients who used CPAP treatment daily had a significant improved quality of life, less daytime sleepiness and greatly reduced risk factors [46, 47]. Therefore, CPAP adherence can influence the effects of CPAP treatment [18, 48, 49].
Our meta-analysis revealed that telemedicine may improve CPAP adherence in patients with OSA. Telemedicine devices can upload daily data related to factors such as CPAP adherence, CPAP pressure, and mask leaks to the sleep laboratory’s platform. When researchers determine that data are abnormal, they are able to contact patients via the network platform or call them to provide professional guidance for behavioural intervention. These measures can help improve knowledge and confidence in patients, thereby improving their CPAP adherence.
Our results support those of previously published systematic reviews [50]. One previous review found that a web-based patient-facing application (PFA) was associated with improved adherence to PAP therapy. However, that review only included two RCTs focusing on PFA use. In contrast, we included 11 RCTs focusing on telemedicine; our sample was larger than that in the previous analysis, and intervention device content was more varied (including wireless modems, telephone-linked communication (TELE) systems and smartphone applications). Another meta-analysis [51] of five RCTs (n = 269 patients) found that teleconsultation/telemonitoring improved CPAP adherence in two trials (n = 19; n = 75), while no between-group differences were observed in two trials (n = 114; n = 75). Additionally, their search ended with papers published in November 2015. In contrast, our meta-analysis of 11 RCTs extended to February 2020 and included teleconsultation and telemonitoring.
Our meta-analysis had potential limitations. First, none of the 11 RCTs included blinded participants and personnel, which may have led to implementation bias or measurement bias. However, one study noted that lack of blinding was unlikely to affect an objectively assessed outcome [52]. Second, our meta-analysis included different types and durations of interventions, with no long-term follow-up (≥ 1 year), so it is unclear whether or not the results could be generalised to long-term follow-up. Third, we did not search for so-called grey literature; we only searched for published literature starting from January 2004.
Conclusions
This meta-analysis revealed that telemedicine interventions may be successfully used to support CPAP adherence in patients with OSA.
References
Lévy P, Kohler M, McNicholas WT et al (2015) Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 1:15015 Published 2015 Jun 25
Jordan AS, Mcsharry DG, Malhotra A (2014) Adult obstructive sleep apnoea. Lancet 383(9918):736–747
Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G (2017) Redline S; INCOSACT Initiative (International Collaboration of Sleep Apnea Cardiovascular Trialists). Sleep Apnea and Cardiovascular Disease: Lessons From Recent Trials and Need for Team Science. Circulation. 136(19):1840–1850
Watson NF (2016) Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. Clin Sleep Med 12(8):1075–1077 Published 2016 Aug 15
Zhang C, Lv J, Zhou J, Su L, Feng L, Ma J, Wang G, Zhang J (2015) The effect of CPAP treatment on EEG of OSAS patients. Sleep Breath 19(4):1121–1124
Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT (2003) Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med 163(5):565–571
Hussain SF, Irfan M, Waheed Z, Alam N, Mansoor S, Islam M (2014) Compliance with continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea among privately paying patients- a cross sectional study. BMC Pulm Med 14:188 Published 2014 Nov 29
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 365(9464):1046–1053
Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, Redline S, Henry JN, Getsy JE, Dinges DF (1993) Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 147(4):887–895
Sutherland K, Kairaitis K, Yee BJ, Cistulli PA (2018) From CPAP to tailored therapy for obstructive sleep apnoea. Multidiscip Respir Med 13:44. https://doi.org/10.1186/s40248-018-0157-0
Wolkove N, Baltzan M, Kamel H, Dabrusin R, Palayew M (2008) Long-term compliance with continuous positive airway pressure in patients with obstructive sleep apnea. Can Respir J 15(7):365–369
Rosen CL, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, Kapur V, Rueschman M, Zee P, Redline S (2012) A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep. 35(6):757–767
Yuli H, Xiaohong W, Feifei W et al (2019) Effect of telemedicine intervention on hypoglycaemia in diabetes patients: a systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare 25(7):402–413
Fukuoka Y, Gay CL, Joiner KL, Vittinghoff E (2015) A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am J Prev Med 49(2):223–237
Organization W. H (2010) Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth. Geneva Switzerland Who
Isetta V, Torres M, Gonzalez K et al (2017) A New mHealth application to support treatment of sleep apnoea patients. J Telemed Telecare 23(1):14–18
Hostler JM, Sheikh KL, Andrada TF, Khramtsov A, Holley PR, Holley AB (2017) A mobile, web-based system can improve positive airway pressure adherence. J Sleep Res 26(2):139–146
Fields BG, Behari PP, Mccloskey S, True G, Richardson D, Thomasson A, Korom-Djakovic D, Davies K, Kuna ST (2016) Remote ambulatory management of veterans with obstructive sleep apnea. Sleep 39(3):501–509. https://doi.org/10.5665/sleep.5514
Sparrow D, Aloia M, Demolles DA et al (2010) A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax 65(12):1061–1066
Smith CE, Dauz ER, Clements F, Puno FN, Cook D, Doolittle G, Leeds W (2006) Telehealth services to improve nonadherence: a placebo-controlled study. Telemed e-Health 12(3):289–296
Anttalainen U, Melkko S, Hakko S, Laitinen T, Saaresranta T (2016) Telemonitoring of CPAP therapy may save nursing time. Sleep Breath 20(4):1209–1215
Chen L, Chapman JL, Yee BJ, Wong KKH, Grunstein RR, Marshall NS, Miller CB (2018) Agreement between electronic and paper Epworth sleepiness scale responses in obstructive sleep apnoea: secondary analysis of a randomised controlled trial undertaken in a specialised tertiary care clinic. BMJ Open 8(3):e019255
Schoch OD, Baty F, Boesch M, Benz G, Niedermann J, Brutsche MH (2019) Telemedicine for continuous positive airway pressure in sleep apnea. A Randomized, Controlled Study. Ann Am Thorac Soc 16(12):1550–1557
Sun J (2012) Effects of CPAP-respiration on serum lipids levels in patients with obstructive sleep apnea syndrome: a systematic review and meta-analysis. ShanDong University. https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD201301&filename=1012464288.nh
Higgins J, Green SE (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. Cochrane Collab 2011(14):S38
Hwang D, Chang J W, Benjafield AV, et al (2017) Effect of telemedicine education and telemonitoring on CPAP adherence: the Tele-OSA randomized trial. Am J Respir Crit Care Med rccm.201703-0582OC
Turino C, De Batlle J, Woehrle H et al (2017) Management of continuous positive airway pressure treatment compliance using telemonitoring in obstructive sleep apnoea. Eur Respir J 49(2):1601128
Stepnowsky CJ, Palau JJ, Marler MR, Gifford AL (2007) Pilot randomized trial of the effect of wireless telemonitoring on compliance and treatment efficacy in obstructive sleep apnea. J Med Internet Res 9(2):e14
Taylor Y, Eliasson A, Andrada T, Kristo D, Howard R (2006) The role of telemedicine in CPAP compliance for patients with obstructive sleep apnea syndrome. Sleep Breath 10(3):132–138
Fox N, Hirschallen A, Goodfellow E et al (2012) The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep 35(4):477–481
Demolles DA, Sparrow D, Friedman GR (2004) A pilot trial of a telecommunications system in sleep apnea management. Med Care 42(8):764–769
Isetta V (2015) Negrín, Miguel A, Monasterio C, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax 70(11):1054–1061
Hoet F, Libert W, Sanida C, van den Broecke S, Bruyneel AV, Bruyneel M (2017) Telemonitoring in continuous positive airway pressure-treated patients improves delay to first intervention and early compliance: a randomized trial. Sleep Med 39:77–83
Stepnowsky C, Edwards C, Zamora T, Barker R, Agha Z (2013) Patient perspective on use of an interactive website for sleep apnea. Int J Telemed Appl 2013:1–10
Munafo D, Hevener W, Crocker M, Willes L, Sridasome S, Muhsin M’ (2016) A telehealth program for CPAP adherence reduces labor and yields similar adherence and efficacy when compared to standard of care. Sleep Breath 20(2):777–785
Pépin JL, Jullian-Desayes I, Sapène M, Treptow E, Joyeux-Faure M, Benmerad M, Bailly S, Grillet Y, Stach B, Richard P, Lévy P, Muir JF, Tamisier R (2019) Multimodal remote monitoring of high cardiovascular risk patients with OSA initiating CPAP: a randomized trial. Chest. 155(4):730–739
Qaseem A, Holty JE, Owens DK, Dallas P, Starkey M, Shekelle P, Clinical Guidelines Committee of the American College of Physicians (2013) Clinical guidelines committee of the American College of Physicians. Management of obstructive sleep apnea in adults: A clinical practice guideline from the American College of Physicians. Ann Intern Med 159(7):471–483
Weaver TE, Sawyer AM (2010) Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res 131:245–258
Mehrtash M, Bakker JP, Ayas N (2019) Predictors of continuous positive airway pressure adherence in patients with obstructive sleep apnea. Lung 197(2):115–121
Crawford MR, Espie CA, Bartlett DJ, Grunstein RR (2014) Integrating psychology and medicine in CPAP adherence-new concepts? Sleep Med Rev 18(2):123–139
Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE (2011) A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 15(6):343–356
Gentina T, Bailly S, Jounieaux F, Verkindre C, Broussier PM, Guffroy D, Prigent A, Gres JJ, Kabbani J, Kedziora L, Tamisier R, Gentina E, Pépin JL (2019) Marital quality, partner’s engagement and continuous positive airway pressure adherence in obstructive sleep apnea. Sleep Med 55:56–61
Parthasarathy S, Wendel C, Haynes PL, Atwood C, Kuna S (2013) A pilot study of CPAP adherence promotion by peer buddies with sleep apnea. J Clin Sleep Med 9(6):543–550
Randerath WJ, Verbraecken J, Andreas S, Bettega G, Boudewyns A, Hamans E, Jalbert F, Paoli JR, Sanner B, Smith I, Stuck BA, Lacassagne L, Marklund M, Maurer JT, Pepin JL, Valipour A, Verse T, Fietze I, the European Respiratory Society task force on non-CPAP therapies in sleep apnoea (2011) Non-CPAP therapies in obstructive sleep apnoea. Eur Respir J 37(5):1000–1028
Yang MC, Huang YC, Lan CC, Wu YK, Huang KF (2015) Beneficial effects of long-term CPAP treatment on sleep quality and blood pressure in adherent subjects with obstructive sleep apnea. Respir Care 60(12):1810–1818
Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, Barbé F, Vicente E, Wei Y, Nieto FJ, Jelic S (2012) Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 307(20):2169–2176
Sullivan CE, Issa FG, Berthon-Jones M, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1(8225):862–865
Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunström E (2016) Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA Randomized Controlled Trial. Am J Respir Crit Care Med 194(5):613–620
Palm A, Berne C, Igelström H et al (2018) The impact of continuous positive airway pressure on circulating igf-1 in patients with obstructive sleep apnea. J Clin Sleep Med 14(3):385–391 Published 2018 Mar 15
Shaughnessy GF, Morgenthaler TI (2019) The effect of patient-facing applications on positive airway pressure therapy adherence: a systematic review. J Clin Sleep Med 15(5):769–777 Published 2019 February 15
Murphie P, Little S, McKinstry B, Pinnock H (2019) Remote consulting with telemonitoring of continuous positive airway pressure usage data for the routine review of people with obstructive sleep apnoea hypopnoea syndrome: A systematic review. J Telemed Telecare 25(1):17–25
Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, Gluud C, Martin RM, Wood AJG, Sterne JAC (2008) Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 336(7644):601–605
Funding
This research was supported by Shanghai Municipal Commission of Science and Technology (Grant No.18DZ2260200) and Effects of telemedicine system interventions in improving continuous positive airway pressure adherence in patients with obstructive sleep apnoea: a systematic review (Grant No. X Within hospital-2320).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, Y., Su, Y., Hu, S. et al. Effects of telemedicine interventions in improving continuous positive airway pressure adherence in patients with obstructive sleep apnoea: a meta-analysis of randomised controlled trials. Sleep Breath 25, 1761–1771 (2021). https://doi.org/10.1007/s11325-021-02292-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02292-5