Abstract
Purpose
Gastroesophageal reflux disease (GERD) often occurs in patients with obstructive sleep apnea (OSA). Although continuous positive airway pressure (CPAP) is considered to be the preferred treatment for OSA, the effect of CPAP therapy on reflux events remains controversial. In this study, we utilized meta-analysis to investigate whether or not CPAP treatment reduces the incidence of reflux.
Methods
Two independent reviewers obtained the data sources from the database of PubMed, Elsevier, Cochrane library, and CNKI using search terms, and then filtered the target articles based on the inclusion and exclusion criteria. RevMan (version 5.3) and STATA (version 12.0) were used for data synthesis. The effect of CPAP treatment on GERD was studied by calculating the weighted mean difference (WMD) and standard deviation (SD) before and after CPAP treatment.
Results
Ten studies involving a total of 272 participants were included in this study. The results showed that the total of WMD before and after CPAP was − 17.68 (95% CI − 30.67 to − 4.69) for percentage time pH < 4, − 24.66 (95% CI − 36.15 to − 13.18) for the longest reflux duration, − 27.53 (95% CI − 49.53 to − 5.52) for number of reflux events, − 49.76 (95% CI − 60.18 to − 39.35) for DeMeester score, − 1.85 (95% CI − 3.00 to − 0.71) for reflux diseases questionnaire (RDQ) score, and − 8.95 (95% CI − 16.00 to − 1.89) for reflux symptom index (RSI). The subgroup analysis demonstrated that the improvement of reflux symptoms was more obvious with the extension of treatment time.
Conclusions
This meta-analysis showed that CPAP treatment significantly reduces the incidence of reflux events in patients with OSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) refers to the apnea and lack of ventilation caused by the collapse of the upper airway during sleep, also known as obstructive sleep apnea hypopnea syndrome (OSAHS). It is mainly manifested as snoring, asphyxiation, daytime sleepiness, and memory decline, which can cause cardiovascular and cerebrovascular diseases and cognitive dysfunction in the long term. OSA can occur in a variety of populations, most of which are middle-aged and elderly. OSA affects a significant number of people worldwide each year. It has been estimated that approximately 1 billion adults aged 30 to 69 years had obstructive sleep apnea, and 425 million of them had moderate to severe obstructive sleep apnea [1], even with an incidence of up to 50% in some countries [2]. With the increase of obesity rate, patients with OSA present an increasing trend [3]. OSA is considered to be a systemic problem and a high-risk factor for many common conditions, such as hypertension, diabetes, and cardiovascular and cerebrovascular accidents, which can lead to sudden death and increase the likelihood of traffic accidents. In addition, studies have shown that OSA is associated with gastroesophageal reflux disease (GERD) [4, 5].
Gastroesophageal reflux disease can be defined as troublesome symptoms that result from the reflux of gastric contents into the esophagus, throat, mouth, or lungs, such as regurgitation, heartburn, and belching. It can also cause a series of long-term complications and end-organ effects, such as vocal cord leucorrhea, reflux asthma, arrhythmia, and sleep disorders [6, 7]. The diagnosis of GERD may involve symptom and sign scale, endoscopic examination, pH-metric criteria, and other indicators. PH-metry ambulatory reflux monitoring is the only test that can evaluate reflux symptom association, including the following indicators commonly used: percentage time pH < 4, the longest reflux duration, number of reflux events, and the DeMeester score. And reflux diseases questionnaire score (RDQ score) and reflux symptom index (RSI) are commonly used clinical scores for symptoms and signs. RDQ score is scored by investigating heartburn, chest pain, acid reflux, and food loss in the past 4 weeks. RSI contains nine items of reflux symptoms. Improvement of life style and acid inhibition therapy are main treatments at present. The frequent co-occurrence of OSA and GERD may be explained by the following mechanisms. Firstly, GERD and OSA patients had similar risk factors: age, obesity, smoking, and alcohol consumption [8, 9]. In addition, strong protective mechanisms for swallowing and esophageal peristalsis decline during sleep, which may delay esophageal acid clearance, thereby increasing acid-mucosal contact time [10]. Most importantly, the negative intrathoracic pressure during inspiratory efforts against the occluded airway and the repetitive arousals to counter obstruction events are responsible for the increased incidence of regurgitation [11, 12].
It is well known that continuous positive airway pressure (CPAP) can significantly improve the hypoxic status and symptoms of OSA and reduce the incidence of related complications, so it is the preferred treatment for patients with OSA. However, whether or not CPAP can improve reflux symptoms in patients with GERD is still controversial. Studies have suggested that CPAP can reduce reflux events in patients with OSA, and even alleviate reflux symptoms in patients without sleep disorders [13, 14]. However, some studies have suggested that the use of CPAP can lead to gastric distension, which can aggravate symptoms such as reflux [15]. The inconsistency of results have been due mainly to small sample sizes and differences in study design. In this study, by integrating changes in reflux symptoms and parameters before and after CPAP treatment documented in previous studies, we attempted to clarify whether or not CPAP treatment is beneficial for GERD in patients with OSA.
Methods
Search strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used. We searched PubMed, Elsevier, Cochrane library, and CNKI database to obtain the targeted articles. The retrieval time of the article is up to March 2020, with no language restrictions. Search terms included “OSAHS or OSA or obstructive sleep apnea hypopnea syndrome or obstructive sleep apnea or Sleep Apnea, Obstructive”, “gastroesophageal reflux or esophageal Reflux or reflux or GER or GERD,” and “continuous positive airway pressure ventilation or CPAP or Ventilation Modes, APRV.” Computer retrieval was combined with manual retrieval of bibliographies of all retrieved articles. Articles that were potentially relevant were evaluated for inclusion according to pre-specified inclusion and exclusion criteria.
Inclusion and exclusion criteria of literature
-
1.
All subjects in this study were adults with OSAHS and reflux symptoms. OSA was diagnosed by polysomnography with apnea hypopnea index (AHI) ≥ 5, and GERD patients were mainly diagnosed on the basis of reflux parameters and symptoms.
-
2.
All patients did not take acid-suppressing drugs and did not receive CPAP treatment for 1 month prior to the trial to prevent their results from being affected.
-
3.
The study must include reflux-relevant values on pre-CPAP and post-CPAP. If the study data could not be provided, or the data was not expressed in the form of WMD and SD, the study was excluded.
-
4.
Research is limited to humans.
-
5.
Abstracts, review, editorials, and case reports were deleted.
Statistical analysis
Review Manager 5.3 and STATA (version 12.0) were used for statistical analysis. The statistical results of continuous outcomes were expressed by weighted mean difference (WMD) and 95% confidence interval (CI), while dichotomous outcomes were expressed by risk ratio (RR) and 95% CI. The Mantel-Haenszel analysis was suitable for dichotomous variables, while the inverse variance method was utilized for continuous variable [16]. The statistical significance level was P < 0.05. Statistical heterogeneity was evaluated according to the I-square (I2) value. Heterogeneity is high when I2 > 75%, moderate when I2 = 50–75%, and low when I2 = 25–50%, and no heterogeneity when I2 < 25% [17]. If I2 < 50%, the study is considered low in heterogeneity, and fixed effects models are used to aggregate the results. If I2 > 50%, the study is considered to be moderately or highly heterogeneous, and the random effects model is used to aggregate the data [18, 19].
Considering the effect of CPAP therapy duration on the outcome, we performed a subgroup analysis (CPAP therapy duration < 1 week and ≥ 1 week). Sensitivity analysis was used to assess the stability of the results. The possible sources of heterogeneity were identified by exploiting meta-regression. We obtained the forest map through Review Manager synthesis. The funnel plot, the Begg test, and the Egger test were used to assess potential publication bias [20, 21]. We also used pruning and filling methods to identify and correct the asymmetry of funnel plot caused by publication bias [22].
Results
Search results
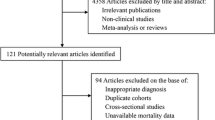
The search and screening of the literature was carried out by two reviewers independently. We initially screened 66 articles from the database, then roughly screened the abstracts or titles of these articles and identified 28 relevant articles. And 5 articles were excluded because of data duplication. We further screened the full text of 23 articles according to the inclusion and exclusion criteria; since there were not enough data or there was a lack of the mean and standard deviation of pre-CPAP and post-CPAP reflux-related indicators, 13 articles were excluded. In the end, a total of 10 studies were included for further research. The steps of document retrieval are displayed in Fig. 1.
Characteristics of included studies
Ten studies involving a total of 272 participants were included in this review [17, 23, 24]. Our review incorporated 6 sets of data representing reflux parameters: percentage time pH < 4, the longest reflux duration, number of reflux events, DeMeester score, RDQ score, and RSI. One study provided 4 sets of data, and 3 studies provided 3 sets of data. The analysis of percentage with time pH < 4 included 5 studies, the longest reflux duration included 6 studies, the number of reflux events included 4 studies, and the DeMeester score, RDQ score, and RSI respectively included 2 studies. All the included self-controlled trials were level 2, and the design of randomized controlled trials was level 1. The authors, year of publication, national sources, sample sizes, duration of treatment, study design, and level of research evidence are shown in Table 1.
Pooled analysis
We obtained a forest map that reflected the relationship between CPAP and percentage time pH < 4, the longest reflux duration, number of reflux events, DeMeester score, RDQ score, and RSI. We summarize the key information of the forest map in Table 2, including reflux parameters, subgroup, studies included, sample size, χ2 (df), P value, mean difference (95% CI), and heterogeneity (I2). The analysis shows that the I2 values of the indicators in the study are 95%, 85%, 97%, 0, 31%, and 82% respectively, and the heterogeneity varies greatly. Therefore, we use the random effects model to combine the effect size. The results illustrated that the total of WMD was − 17.68 (95% CI − 30.67 to − 4.69, P = 0.008) for percentage time pH < 4, − 24.66 (95% CI − 36.15 to − 13.18, P < 0.0001) for the longest reflux duration, − 27.53 (95% CI − 49.53 to − 5.52, P = 0.01) for number of reflux events, − 49.76 (95% CI − 60.18 to − 39.35, P < 0.00001) for the DeMeester score, − 1.85 (95% CI − 3.00 to − 0.71, P = 0.002) for the RDQ score, and − 8.95 (95% CI − 16.00 to − 1.89, P = 0.01) for RSI.
Subgroup analysis
According to the dividing line of treatment time of 1 week, we performed subgroup analysis for three sets of parameters including percentage time pH < 4, the longest reflux duration, and the number of reflux events (Table 2).
Treatment time < 1 week: the analysis of percentage with time pH < 4 included 3 studies, the longest reflux duration included 3 studies, and the number of reflux events included 2 studies. The total of WMD for percentage time pH < 4 was − 12.55 (95% CI − 22.65 to − 2.44, P = 0.01), the corresponding value for the longest reflux duration was − 27.70 (95% CI − 47.67 to − 7.71, P = 0.007), and the corresponding value for the number of reflux events was − 9.57 (95% CI − 12.43 to − 6.71,P < 0.00001).
Treatment time ≥ 1 week: the analysis of percentage with time pH < 4 included 3 studies, the longest reflux duration included 3 studies, and the number of reflux events included 2 studies. The total of WMD for percentage time pH < 4 was − 25.44 (95% CI − 45.45 to − 5.43, P = 0.01), the corresponding value for the longest reflux duration was − 24.77 (95% CI − 36.74 to − 12.80, P < 0.0001), and the corresponding value for the number of reflux events was − 49.27 (95% CI − 60.92 to − 37.63, P < 0.00001).
Sensitivity analysis and quality assessment
Sensitivity analysis showed that the five indicators including percentage time pH < 4, the longest reflux duration, DeMeester score, RDQ score, and RSI would not destroy the current pooled analysis results after removing any study. While one indicator (number of reflux events) showed no significant difference in the pooled analysis results after the deletion of Maroun’s study. After changing the random effects model to the fixed effects model, the analysis results did not change significantly.
Publication bias
There may be a slight publication bias because the funnel plot was not completely symmetrical. However, we performed the Begg and Egger tests for the three groups of parameters in the study, which were percentage time pH < 4, the longest reflux duration, and number of reflux events. The Begg test showed no publication bias in percentage time pH < 4 (P = 0.806), the longest reflux duration (P = 0.452), and number of reflux events (P = 0.734). In analogy, there was no publication bias in Egger’test for percentage time pH < 4 (P = 0.817), the longest reflux duration (P = 0.482), and number of reflux events (P = 0.833). The pruning and filling methods showed that the symmetry of funnel plots did not require statistical correction.
At the same time, we evaluated bias sources used risk of bias from Cochrane risk-of-bias tool (Fig. 2).
Discussion
It is well known that OSA patients with reflux symptoms are a very common phenomenon. Although CPAP is considered to be the preferred treatment for OSA patients, the influence of CPAP therapy on reflux in OSA patients remains controversial. On the one hand, some studies have suggested that CPAP treatment increases rate of GERD, which may be related to esophageal aerophagia, that is, CPAP tend to move air down to the esophagus and stomach through pressure, causing abdominal distension and further triggering lower esophageal sphincter relaxation [25, 26]. However, Ozcelik H et al. demonstrated that CPAP treatment does not cause reflux through objective parameters of the esophageal manometer and pH meter [27]. On the other hand, unlike the above, studies have demonstrated that after CPAP treatment, the reflux symptoms of OSA patients are alleviated 17,29-31. They believe that CPAP treatment can reduce airway obstruction, relieve inspiratory force, increase esophageal pressure, and lower arousal and movement frequency, all of which are associated with a reduced risk of GERD. In addition, CPAP pressure in severe OSA patients increased lower esophageal sphincter pressure and further decreased GERD [28]. Some researchers deem that improvement of reflux after CPAP treatment is the result of increased esophageal pressure and lower esophageal sphincter pressure [29].
In previous studies, we could perceive that different indicators and test methods were used to evaluate GERD. The diagnosis of GERD requires comprehensive consideration, which may involve symptoms, endoscopic examination, pH-metric criteria, manometry, PPI trail, and detection of helicobacter pylori. A presumptive diagnosis of GERD can be originated in the setting of typical symptoms of heartburn and regurgitation [28]. The reflux diseases questionnaire and the gastroesophageal reflux diseases questionnaire are currently the most widely used epidemiological studies of diagnostic questionnaire tools. “PPI trial” is often used in clinical practice, but is prohibited in our study. Although the pH value criterion, esophageal pressure measurement, and endoscopy are not used in routine clinical diagnosis, they embody a comprehensive feature of GERD, and they are important in intractable and atypical symptoms. PH-metry ambulatory reflux monitoring is the only test that can evaluate reflux symptom association [30], including the following indicators commonly used: percentage time pH < 4, the longest reflux duration, number of reflux events, and the DeMeester score.
Our study combined a number of indicators for evaluating GERD, including symptom scores and pH-metry parameters. The changes in six indicators before and after CPAP treatment showed that CPAP was significantly correlated with reflux index (P < 0.01), which effectively improved reflux symptoms and pH-metry parameters in OSA patients. There was a degree of heterogeneity in this study. Considering the effect of CPAP therapy duration on the outcome, we performed a subgroup analysis based on the treatment time to find the source of heterogeneity. The analysis demonstrated that the results were significant regardless of whether the treatment time was longer or shorter than 1 week, indicating that CPAP treatment can reduce reflux events regardless of duration of treatment. No publication bias was found in the results of Begg’s test and Egger’s test. At the same time, the sensitivity analysis showed that the overall results were basically unchanged after excluding the single study or converting the fixed effects model to the random effects model. Therefore, the outcome of our meta-analysis was strongly convincing.
Although our research acquired meaningful reliable results, it still had some limitations. First of all, the study sample size included in the analysis was too small, so we may need more studies to address the impact of this factor. Secondly, the diagnosis criteria for GERD was partly based on subjective symptoms and empirical PPI therapy (“PPI trial”), but PPI therapy was prohibited in our study, which made the diagnosis challenging. In addition, different studies adopted different indicators and measurement techniques, which may produce inconsistent results to some extent. Finally, some results had a large heterogeneity, but we could not define the source of heterogeneity from the limited research data.
Conclusion
Our study aggregated six indicators, including two symptom scale scores and four indicators related to pH-metry parameters. Our meta-analysis showed that CPAP treatment relieved reflux symptoms and reduced the value of pH-metry. In conclusion, CPAP is beneficial for gastroesophageal reflux in patients with OSAHS. Therefore, in patients with OSAHS who suffer with GERD, CPAP is a considerable option for the treatment of OSA and the improvement of reflux symptoms. However, more prospective data are needed to confirm which patients benefit.
RDQ score, reflux diseases questionnaire score; RSI, reflux symptom index; LOE, level of evidence; RCT, randomized controlled trials; SCT, self-control trials
RDQ score, reflux diseases questionnaire; RSI, reflux symptom index; NA, not appliable; CI, confidence interval
Abbreviations
- OSA:
-
obstructive sleep apnea
- OSAHS:
-
obstructive sleep apnea hypopnea syndrome
- GERD:
-
gastroesophageal reflux disease
- CPAP:
-
continuous positive airway pressure
- CNKI:
-
China National Knowledge Infrastructure
- WMD:
-
weighted mean difference
- SD:
-
standard deviation
- CI:
-
confidence interval
- RDQ:
-
reflux diseases questionnaire
- RSI:
-
reflux symptom index
References
Benjafield Adam V, Ayas Najib T, Eastwood Peter R et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. [J]. Lancet Respir Med 7:687–698. https://doi.org/10.1016/S2213-2600(19)30198-5
Tan A, Yi CY, Jason Y et al (2016) Prevalence of sleep-disordered breathing in a multiethnic Asian population in Singapore: a community-based study. [J]. Respirology 21:943–950. https://doi.org/10.1111/resp.12747
Young T, Peppard PE, Shahrad T (2005) Excess weight and sleep-disordered breathing. [J]. J Appl Physiol 99:1592–1599. https://doi.org/10.1152/japplphysiol.00587.2005
Zanation AM, Senior Brent A (2005) The relationship between extraesophageal reflux (EER) and obstructive sleep apnea (OSA). [J]. Sleep Med Rev 9:453–458. https://doi.org/10.1016/j.smrv.2005.05.003
Elhennawi DM, Ahmed MR, Abou-Halawa AS (2016) Correlation of obstructive sleep apnoea and laryngopharyngeal reflux: phmetry study. [J]. Clin Otolaryngol 41:758–761. https://doi.org/10.1111/coa.12640
Richard H, Eamonn Q, Zaigham A et al (2014) Coping with common gastrointestinal symptoms in the community: a global perspective on heartburn, constipation, bloating, and abdominal pain/discomfort May 2013. [J]. J Clin Gastroenterol 48:567–578. https://doi.org/10.1097/MCG.0000000000000141
Paul M, Talley Nicholas J (2006) Gastro-oesophageal reflux disease.[J]. Lancet 367:2086–2100. https://doi.org/10.1016/S0140-6736(06)68932-0
Marques RM, Silveira DR, Barbosa SVJ et al (2014) Influence of obesity on the correlation between laryngopharyngeal reflux and obstructive sleep apnea. [J]. Braz J Otorhinolaryngol 80:5–10. https://doi.org/10.5935/1808-8694.20140004
Kelly S, William O (2016) Mechanism of gastroesophageal reflux in obstructive sleep apnea: airway obstruction or obesity? [J]. Clin Sleep Med 12:87–94. https://doi.org/10.5664/jcsm.5402
Teramoto S, Haruki K, Yasuyoshi O (2002) Nocturnal gastroesophageal reflux: symptom of obstructive sleep apnea syndrome in association with impaired swallowing. [J]. Chest 122:2266–2267; author reply 2267. https://doi.org/10.1378/chest.122.6.2266
Gislason T, Christer J, Paul V et al (2002) Respiratory symptoms and nocturnal gastroesophageal reflux: a population-based study of young adults in three European countries. [J]. Chest 121:158–163. https://doi.org/10.1378/chest.121.1.158
Freidin N, Fisher MJ, Taylor W, Boyd D, Surratt P, McCallum RW, Mittal RK (1991) Sleep and nocturnal acid reflux in normal subjects and patients with reflux oesophagitis. [J]. Gut 32:1275–1279. https://doi.org/10.1136/gut.32.11.1275
Sadeka T, Douglas C, Richard W et al (2016) Effect of CPAP therapy on symptoms of nocturnal gastroesophageal reflux among patients with obstructive sleep apnea. [J]. J Clin Sleep Med 12:1257–1261. https://doi.org/10.5664/jcsm.6126
Kerr P, Shoenut JP, Millar T, Buckle P, Kryger MH (1992) Nasal CPAP reduces gastroesophageal reflux in obstructive sleep apnea syndrome. [J]. Chest 101:1539–1544. https://doi.org/10.1378/chest.101.6.1539
Criner GJ, Brennan K, Travaline JM, Kreimer D (1999) Efficacy and compliance with noninvasive positive pressure ventilation in patients with chronic respiratory failure. [J]. Chest 116:667–675. https://doi.org/10.1378/chest.116.3.667
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. [J]. J Natl Cancer Inst 22:719–748. https://doi.org/10.1093/jnci/22.4.719
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. [J]. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Higgins JPT, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. [J]. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. [J]. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. [J]. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. [J]. Biometrics 50:1088–1101. https://doi.org/10.2307/2533446
Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. [J]. Biometrics 56:455–463. https://doi.org/10.1111/j.0006-341x.2000.00455.x
Zheng S (2012) The Second Xiangya Hospital of Central South University. Observation of the efficacy of nasal continuous positive airway pressure combined with anti-reflux drugs in the treatment of elderly patients with OSAHS and GERD [J]. The 1st China Beijing China Geriatrics and Geriatric Health Industry Conference (in Chinese)
Kerr P, Shoenut JP, Steens RD, Millar T, Micflikier AB, Kryger MH (1993) Nasal continuous positive airway pressure. A new treatment for nocturnal gastroesophageal reflux? [J]. J Clin Gastroenterol 17:276–280. https://doi.org/10.1097/00004836-199312000-00002
Watson NF, Mystkowski SK (2008) Aerophagia and gastroesophageal reflux disease in patients using continuous positive airway pressure: a preliminary observation. [J]. J Clin Sleep Med 4:434–438
Shepherd K, Hillman D, Eastwood P (2013) Symptoms of aerophagia are common in patients on continuous positive airway pressure therapy and are related to the presence of nighttime gastroesophageal reflux. [J]. J Clin Sleep Med 9:13–17. https://doi.org/10.5664/jcsm.2328
Hatice O, Yusuf K, Ahmet D et al (2017) Does CPAP treatment lead to gastroesophageal reflux in patients with moderate and severe OSA? [J]. Eur Arch Otorhinolaryngol 274:1223–1229. https://doi.org/10.1007/s00405-016-4116-0
Moraes-Filho JPP, Ivan C, Joaquim G-R et al (2002) Brazilian consensus on gastroesophageal reflux disease: proposals for assessment, classification, and management. [J]. Am. J Gastroenterol 97:241–248. https://doi.org/10.1111/j.1572-0241.2002.05476.x
Hye-Kyung J, Seon CR, Talley Nicholas J (2010) Gastroesophageal reflux disease and sleep disorders: evidence for a causal link and therapeutic implications. [J]. J Neurogastroenterol Motil 16:22–29. https://doi.org/10.5056/jnm.2010.16.1.22
Hirano I, Richter Joel E (2007) Practice Parameters Committee of the American College of Gastroenterology, ACG practice guidelines: esophageal reflux testing. [J]. Am J Gastroenterol 102:668–685. https://doi.org/10.1111/j.1572-0241.2006.00936.x
Author information
Authors and Affiliations
Contributions
L.C, W.Z.H, and P.X.L designed the research study and wrote the manuscript; Y. K wrote and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Cheng Li, Zeng-hong Wu, and Xiao-ling Pan contributed to this work equally and are listed as co-first authors.
Rights and permissions
About this article
Cite this article
Li, C., Wu, Zh., Pan, Xl. et al. Effect of continuous positive airway pressure on gastroesophageal reflux in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath 25, 1203–1210 (2021). https://doi.org/10.1007/s11325-020-02224-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02224-9