Abstract
Background
Cardiovascular diseases (CVDs) are highly prevalent in obstructive sleep apnea (OSA), and dyslipidemia is an important factor. Atherogenic index of plasma (AIP, log[TG/HDL-C]) and apolipoproteinB to apolipoproteinAI ratio (apoB/apoAI ratio) are considered high quality predictors of cardiovascular risk. However, the associations between OSA severity and AIP and apoB/apoAI ratio remained unclear.
Methods
A retrospective study was performed in 284 patients. Subjects were assessed with polysomnography (PSG) test, and OSA severity was defined by AHI. Data collected included anthropometric measurements, medical history, sleep parameters, fasting plasma lipids, fasting blood glucose, and insulin.
Results
Participants were classified based on AHI into the following groups: control group (n = 28), mild group (n = 52), moderate group (n = 53), and severe group (n = 151). Triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), apoAI, AIP, apoB/apoAI ratio (low-density lipoprotein cholesterol), LDL-C/HDL-C ratio, and HDL-C/apoAI ratio showed statistical significance among AHI subgroups (P < 0.05). The Pearson correlation analysis revealed that AIP (r = 0.32, P < 0.001) and apoB/apoAI ratio (r = 0.24, P < 0.001) were positively related to AHI. By multivariate linear regression analysis, we found that AHI was independently related to AIP (β = 0.24, P = 0.001), apoB/apoAI ratio (β = 0.24, P<0.001).
Conclusion
AHI was independently correlated with AIP and apoB/apoAI ratio in OSA. Our findings suggested that AIP and apoB/apoAI ratio increased with OSA severity, which might be partly responsible for the high risk of CVDs in OSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA), a prevalent sleep related respiratory disorder, is caused by recurrent collapse of the upper airway, which can cause nocturnal hypoxia and sleep disruption, as well as daytime sleepiness [1]. It is well known that OSA is closely correlated with metabolic syndrome including dyslipidemia. Several mechanisms such as chronic intermittent hypoxia, oxidative stress, insulin resistance, sympathetic activation, and systemic inflammation may explain the dyslipidemia in OSA [2]. Cardiovascular diseases (CVDs) are highly prevalent in OSA patients, and dyslipidemia is considered to be an important factor for CVDs [3]. In recent years, AIP (atherogenic index of plasma) and apoB/apoAI indicators are believed to be better predictors for CVDs compared with isolated lipid parameters [4, 5]. The cutoff points of AIP and apoB/apoAI that define a high CVDs risk are 0.24 and 0.9, respectively [6, 7]. These two novel indicators could better reflect the lipid metabolism and serve as sensitive indexes for CVDs risk. However, they are underused in OSA. Therefore, the aim of the current research was to explore the relationship of OSA severity (in terms of apnea hypopnea index, AHI) with AIP and apoB/apoAI ratio.
Materials and methods
Subjects
A retrospective research of 284 participants in the sleep center was conducted between January 2014 and November 2018. Dates were extracted from the medical record system in a retrospective manner, including sex, age, height, weight, case history, medication use, sleep parameters, fasting plasma lipids, fasting blood glucose, and insulin. Patients with history of OSA therapy, lipid lowering therapy, alcohol abuse, taking psychoactive medications or corticosteroids, liver or kidney disease, type 2 diabetes, CVDs (including coronary artery disease, heart failure, stroke, and peripheral vascular diseases), malignant tumor, hyperthyroidism, or hypothyroidism were excluded. Patients who were younger than 18 years old were also excluded.
Polysomnography
Overnight in-laboratory PSG was carried out at the sleep center of NanFang Hospital. Apnea were defined as a ≥ 90% drop in flow for more than 10 s. Hypopnea was defined as a 30% or greater drop in breathing amplitude lasting for more than 10 s and accompanied with an oxyhemoglobin desaturation greater than 3% or an ECG arousal. OSA severity was determined based on AHI, which was calculated as the sum of apnea and hypopnea per hour of sleep time.
Biochemical parameters
Fasting plasma lipids were obtained from patients’ medical record, including total cholesterol (TC), triglycerides (TG), apolipoprotein B (apoB), apolipoprotein AI (apoAI), apolipoprotein E (apoE), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and very low-density lipoprotein (VLDL). Based on isolated lipid parameters, the following clinical indicators were calculated: AIP, apoB/apoAI ratio, LDL-C/apoB ratio, HDL-C/apoAI ratio, and LDL-C/HDL-C ratio. In order to calculate LDL-C/apoB and HDL-C/apoAI index, the concentration of LDL-C and HDL-C was converted from millimoles/l to milligrams/l, respectively. AIP value was computed as follows: the logarithm of TG/HDL-C ratio (log[TG/HDL-C]) [8]. The homeostasis model (HOMA-IR) was applied to estimate glycometabolism, and the calculation method was as follows: fasting insulin× fasting glucose / 22.5 [9].
Statistical analysis
Statistical analyses of all data in this study were conducted in SPSS 22.0. Quantitative data were given as the mean ± standard deviation, and their comparisons were analyzed by using analysis of variance (ANOVA). Categorical data were presented as counts (percentage), and their comparisons were tested with chi-square test. Pearson correlation analysis was applied to determine the relationship between AHI and lipid profile. Multiple linear regression analysis was applied to identify the correlation between AHI and nontraditional lipid profile. If a P value was < 0.05, statistical significance was determined.
Results
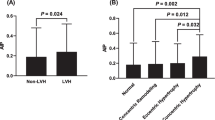
The clinical and biochemical data are shown in Table 1. There are 284 subjects, with an average age of 45.28 ± 11.12 years. Based on AHI, 28 subjects were divided into control group (AHI < 5 events), 52 subjects in mild group (AHI 5–15 events), 53 subjects in moderate group (AHI ≥ 15 and < 30 events), and 151 subjects in severe group (AHI ≥ 30 events). For lipid profile, our research showed significant differences in TG, apoAI, HDL-C, AIP, apoB/apoAI ratio, HDL-C/apoAI ratio, and LDL-C/HDL-C (P < 0.05). However, we did not find statistical differences in TC, LDL-C, apoB, VLDL-C, and LDL-C/apoB (P > 0.05) (Table 1). In addition, the percentage of patients with the AIP exceeding 0.24 was 49.6%. For the apoB/ apoAI ratio, 45.1% of the subjects had values above 0.9. In the Pearson correlation analysis, TG (r = 0.22, P < 0.001), TC (r = 0.13, P = 0.03), apoAI (r = − 0.16, P = 0.006), HDL-C (r = −0.26, P < 0.001), AIP (r = 0.32, P < 0.001), apoB/apoAI ratio (r = 0.24, P < 0.001), LDL-C/HDL-C ratio (r = 0.24, P = 0.001), and HDL-C/apoAI ratio (r = − 0.24, P < 0.001) were significantly associated with AHI (Table 2). Moreover, stepwise linear multivariate regression model revealed that AHI was independently correlated with AIP (β = 0.24, P = 0.001), apoB/apoAI ratio (β = 0.24, P<0.001) (Table 3). Figs. 1–2 showed the correlations between AHI and AIP (Fig. 1, R2 = 0.101) and apoB/apoAI ratio (Fig. 2, R2 = 0.059), respectively.
Discussion
This study explored the relationships between AHI and AIP and apoB/apoAI ratio in OSA patients. Our results revealed that AHI was independently associated with AIP and apoB/apoAI ratio. As far as we know, this was the first study that showed independent association of OSA severity with lipid metabolism of AIP and apoB/apoAI ratio.
AIP
AIP indicator reflected the association between protective factors and atherogenic factors [8]. Previous studies have demonstrated that OSA was correlated with low HDL-C levels and high TG levels [10,11,12] and thus an increase in AIP parameter. Accordingly, our data also showed that AHI was positively related to TG levels, while HDL-C levels decreased as AHI value increased. Moreover, AHI was independently associated with AIP after adjusting for confounding factors. We speculated that the following mechanisms may explain the relationship between OSA severity and AIP index. First, chronic intermittent hypoxia (CIH) could increase TG levels by promoting the production of enzymes and proteins related to TG synthesis in the liver [13]. At the same time, increased sympathetic tone in OSA patients could change the body’s endocrine hormone level, which might affect the production of lipoprotein lipase and lead to the reduction of serum HDL-C concentration [14], thus increasing AIP levels. In addition, previous studies have indicated that block alpha-1 receptor could elevate serum HDL-C and reduce TG level [15]. Therefore, hypersympathetic tone presented in patients with OSA [16] might be another factor increased AIP levels.
The present study had an important clinical implication. Recently, a large number of research evidence have shown that AIP was a powerful indicator to evaluate the risk of CVDs [5, 6, 17, 18]. For example, Cai’s research [5] demonstrated that AIP was an independent risk predictive index for coronary heart disease. Compared with conventional single lipid parameters, AIP was highly valuable for detecting CVDs risk [5]. The following reasons may explain the great predictive power of AIP. First, AIP was a comprehensive clinical indicator, indicating the relationship between protective and atherogenic lipoprotein. And it seemed that using both lipid indices simultaneously provided more accurate information [8]. Second, AIP was believed to have similar clinical significance to sdLDL (small dense LDL), which was believed to be highly atherogenic [19]. In our study, we found that AHI was strongly and independently associated with AIP in OSA patients. Furthermore, the percentage of subjects with AIP ratio above 0.24 was 49.6%. The increase of AIP was proportional to OSA severity, which might partly elucidate why OSA patients have high risk of CVDs, especially in patients with severe OSA [20].
ApoB/apoAI ratio
It was well known that apoB was an essential structural constituent of atherogenic lipoproteins and apoAI was main structural component of anti-atherogenic HDL-C [21]. Thus, apoB/apoAI ratio also represented the relationship between atherogenic factors and protective factors [22]. In a large-scale research [23], OSA patients had lower levels of apoAI and higher levels of apoB than non-OSA. Similarly, the current research also shown that OSA was related to elevation in apoB level and reduction in apoA level and thereby an increase in apoB/apoAI ratio. Previous studies reported that apoB/apoAI index was relevant to insulin resistance [24] and apoB was related to inflammatory response [25]. Insulin resistance and systemic inflammation, which were observed in OSA [26], might be the causes of increased apoB/apoAI ratio in OSA.
Several research have revealed that apoB/apoAI indicator was stronger than LDL-C/HDL-C in predicting CVDs risk [27, 28]. Furthermore, Kaneva’s research has observed that the normolipidemia participants, who with a high apoB/apoAI value, had more atherogenic lipid profile [7]. The following explanations may explain the great prediction ability of apoB/apoAI ratio. First, similarly, apoB/apoAI ratio was a comprehensive lipid index, indicating the relationship between atherosclerosis and anti-atherosclerosis lipoprotein [22]. Moreover, each atherogenic lipoprotein particle contained one apoB molecule; thus the serum apoB levels represented the potential atherogenic risk. In addition, it is the apoB in lipoprotein particles that causes these lipoproteins to remain in the arterial wall, which eventually leads to the risk of CVDs [21]. In current research, significant difference in apoB/apoAI ratio was observed, and this indicator was independently related to AHI. In addition, the proportion of participants with apoB/apoAI ratio above 0.9 was high (45.1%) in our study. Similarly, this might partly explain why OSA patients have higher cardiovascular risk than the general population.
However, in current research, we did not observe statistical difference in LDL-C among four groups. Consistent with our results, several previous research [2, 29] also identified no statistical difference in LDL-C. This result might indicated that AIP and apoB/apoAI ratio were more sensitive and accurate CVDs risk predictors than LDL-C and other traditional single lipids, which was consistent with previous research conclusions [6, 22].
There were several limitations in present research. Firstly, it’s a retrospective research. Therefore, the mechanism of dyslipidemia in OSA could not be further explored. Secondly, we failed to study the relationships between oxygen desaturation index (ODI) and AIP and apoB/apoAI ratio. Thirdly, we did not evaluate the influence of CPAP treatment on AIP and apoB/apoAI levels.
Conclusion
In conclusion, we have shown that AHI was independently associated with AIP and apoB/apoAI ratio. Our findings suggested that AIP and apoB/apoAI ratio increased with OSA severity, which might be partly responsible for the high risk of CVDs in OSA. In the future, it is necessary to carry out high quality prospective research to further elaborate the relationships of OSA severity with AIP and apoB/apoAI ratio and to evaluate the clinical value of AIP and apoB/apoAI ratio in identifying OSA patients with high risk of cardiovascular diseases.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Coughlin S (2004) Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J 25:735–741
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. LANCET 364:937–952
Millan J, Pinto X, Munoz A, Zuniga M, Rubies-Prat J, Pallardo LF, Masana L, Mangas A, Hernandez-Mijares A, Gonzalez-Santos P, Ascaso JF, Pedro-Botet J (2009) Lipoprotein ratios: physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag 5:757–765
Cai G, Shi G, Xue S, Lu W (2017) The atherogenic index of plasma is a strong and independent predictor for coronary artery disease in the Chinese Han population. Medicine (Baltimore) 96:e8058
Wu T, Gao Y, Zheng Y, Ma Y, Xie X (2018) (AIP-AI ) Atherogenic index of plasma (AIP): a novel predictive indicator for the coronary artery disease in postmenopausal women. LIPIDS HEALTH DIS 17:197
Kaneva AM, Potolitsyna NN, Bojko ER, Odland JØ (2015) The Apolipoprotein B/Apolipoprotein A-I ratio as a potential marker of plasma atherogenicity. Dis Markers 2015:1–7
Dobiásová M, Frohlich J (2001) The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem 34:583
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. DIABETOLOGIA 28:412–419
Roche F, Sforza E, Pichot V, Maudoux D, Garcin A, Celle S, Picard-Kossovsky M, Gaspoz J, Barthélémy JC (2009) Obstructive sleep apnoea/hypopnea influences high-density lipoprotein cholesterol in the elderly. Sleep Med 10:882–886
Nadeem R, Singh M, Nida M, Waheed I, Khan A, Ahmed S, Naseem J, Champeau D (2014) Effect of obstructive sleep apnea hypopnea syndrome on lipid profile: a meta-regression analysis. J Clin Sleep Med 10:475–489
Newman AB, Nieto FJ, Guidry U, Lind BK, Redline S, Pickering TG, Quan SF (2001) (TG)relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol 154:50–59
Adedayo AM, Olafiranye O, Smith D, Hill A, Zizi F, Brown C, Jean-Louis G (2014) Obstructive sleep apnea and dyslipidemia: evidence and underlying mechanism. Sleep Breath 18:13–18
Kawano Y, Tamura A, Kadota J (2012) Association between the severity of obstructive sleep apnea and the ratio of low-density lipoprotein cholesterol to high-density lipoprotein cholesterol. METABOLISM 61:186–192
Marotta T, Ferrara LA, Di Marino L, Mancini M, Annuzzi G, Russo O, D’Orta G, Lucarelli C, Rossi F (1995) Factors affecting lipoprotein lipase in hypertensive patients. METABOLISM 44:712–718
Somers VK, Dyken ME, Clary MP, Abboud FM (1995) Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest 96:1897–1904
Zhan Y, Xu T, Tan X (2016) Two parameters reflect lipid-driven inflammatory state in acute coronary syndrome: atherogenic index of plasma, neutrophil-lymphocyte ratio. BMC Cardiovasc Disord 16:96
Niroumand S, Khajedaluee M, Khadem-Rezaiyan M, Abrishami M, Juya M, Khodaee G, Dadgarmoghaddam M (2015) Atherogenic index of plasma (AIP): a marker of cardiovascular disease. Med J Islam Repub Iran 29:240
Wu TT, Gao Y, Zheng YY, Ma YT, Xie X (2018) Atherogenic index of plasma (AIP): a novel predictive indicator for the coronary artery disease in postmenopausal women. Lipids Health Dis 17:197
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. LANCET 365:1046–1053
Walldius G, Jungner I (2004) Apolipoprotein B and apolipoprotein A-I: risk indicators of coronary heart disease and targets for lipid-modifying therapy. J Intern Med 255:188–205
Walldius G, Jungner I (2006) The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy--a review of the evidence. J Intern Med 259:493–519
Xu H, Guan J, Yi H, Zou J, Meng L, Tang X, Zhu H, Yu D, Zhou H, Su K, Wang Y, Wang J, Yin S, Shanghai SHSR, The SSHS (2016) Elevated low-density lipoprotein cholesterol is independently associated with obstructive sleep apnea: evidence from a large-scale cross-sectional study. Sleep Breath 20:627–634
Sierra-Johnson J, Romero-Corral A, Somers VK, Lopez-Jimenez F, Walldius G, Hamsten A, Hellenius ML, Fisher RM (2007) ApoB/apoA-I ratio: an independent predictor of insulin resistance in US non-diabetic subjects. Eur Heart J 28:2637–2643
Sniderman AD, Faraj M (2007) Apolipoprotein B, apolipoprotein A-I, insulin resistance and the metabolic syndrome. Curr Opin Lipidol 18:633–637
Seetho IW, Wilding JP (2014) Sleep-disordered breathing, type 2 diabetes and the metabolic syndrome. ChroN Resp Dis 11:257–275
Walldius G, Jungner I, Aastveit AH, Holme I, Furberg CD, Sniderman AD (2004) The apoB/apoA-I ratio is better than the cholesterol ratios to estimate the balance between plasma proatherogenic and antiatherogenic lipoproteins and to predict coronary risk. Clin Chem Lab Med 42:1355–1363
Rasouli M, Kiasari AM, Mokhberi V (2006) The ratio of apoB/apoAI, apoB and lipoprotein(a) are the best predictors of stable coronary artery disease. Clin Chem Lab Med (CCLM) 44
Lin Q, Zhang X, Chen G, Huang D, Din H, Tang A (2012) Obstructive sleep apnea syndrome is associated with some components of metabolic syndrome in nonobese adults. Sleep Breath 16:571–578
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, B., Fan, Z., Zhang, Y. et al. Independent association of severity of obstructive sleep apnea with lipid metabolism of atherogenic index of plasma (AIP) and apoB/apoAI ratio. Sleep Breath 24, 1507–1513 (2020). https://doi.org/10.1007/s11325-020-02016-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02016-1