Abstract
Purpose
The symptoms of sleep apnea, such as sleep fragmentation and oxygen desaturation, might be risk factors for subsequent mood disorder (MD), but associations between sleep apnea and MD remain unclear. This nationwide population-based study thus aimed to identify the risk of MD in patients with vs. without sleep apnea.
Methods
This cohort study used data from the National Health Insurance database. In total, 5415 patients diagnosed with sleep apnea between 2000 and 2010 were evaluated, and 27,075 matched non-sleep apnea enrollees were included as a comparison cohort. All subjects were followed until 2011. The Cox proportional hazard ratio (HR) was used to investigate the relationship between MD and sleep apnea while controlling covariates and comorbidities of sleep apnea.
Results
Of 5415, 154 patients with sleep apnea (2.84 %) were diagnosed with MD during the follow-up period in comparison with 306 of 27,075 individuals (1.13 %) without antecedent sleep apnea. After adjusting for the selected factors and comorbidities, we found that patients with sleep apnea were from 1.82- to 2.07-fold greater risk of MD than the comparisons. Of the three subcategories of MD (major depressive disorder, bipolar disorder, and unspecified MD), sleep apnea had the highest predisposing risk with respect to major depressive disorder (adjusted HR from 1.82 to 2.07) and bipolar disorder (adjusted HR from 2.15 to 3.24).
Conclusions
There is a greater likelihood of MD manifesting in patients with a history of sleep apnea. Health professionals are thus advised to carefully monitor the psychological impacts of sleep apnea.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sleep apnea is a type of sleep disorder characterized by complete or partial cessation of breathing during sleep. There are three specific forms of sleep apnea, central sleep apnea, obstructive sleep apnea, and complex or mixed sleep apnea [1]. Obstructive sleep apnea is one of the best known and most prevalent sleep disorders. A previous study reported that the prevalence of sleep apnea is currently estimated between 5 and 10 % [2]. Sleep apnea can cause serious disturbances, such as increased sympathetic activity and intermittent hypoxemia. Previous studies have revealed that sleep apnea can influence the quality of life and is associated with a number of serious consequences, including fatigue and excessive daytime sleepiness, endocrine and metabolic derangements [3], hearing loss [4], and cardiovascular disease [5]. Besides these physical effects, sleep apnea is associated with a higher prevalence of psychiatric comorbidities [6–8].
In biomechanism research, sleep fragmentation and oxygen desaturation during sleep are suspected to be responsible for mood disorder (MD) [9]; however, studies of sleep apnea and MD remain unclear. A study found that women with severe sleep apnea had higher anxiety and depression scores than women with mild sleep apnea [10]. In addition, depression has been reported to be associated with not only sleep apnea-related symptoms (such as sleep problems, irritability, social withdrawal, and sleepiness) but also the most common MDs in sleep apnea [11]. The previous study showed that the patients with obstructive sleep apnea experienced a higher risk of depressive disorder than comparison group [12]. However, there are two opinions regarding MD and sleep apnea in previous studies; some scientists considered that there is strong correlation between MD syndrome and obstructive sleep apnea [7, 13, 14], whereas other scientists advocated that although patients with obstructive sleep apnea may clinically have depression-related symptoms, they are not always related to MDs [15–17].
According to the previous studies, we found that MD and sleep apnea might have some relevance as well as have causal relationship, but the evidence is far from conclusive. However, the inconclusive results with respect to non-significant correlations might be because of the small sample size, sample characteristics, lack of control groups, and the respondents’ reaction bias [17]. The previous study only investigates the association between depressive disorder and sleep apnea [12]. Considering this, a longitudinal study regarding the development of MDs in patients with sleep apnea is required because such a study is currently lacking in the literature. Therefore, this study aimed to investigate the risk of MD (i.e., major depressive disorder, bipolar disorder, and unspecified MD) for patients with sleep apnea using a nationwide population-based dataset in Taiwan. In this study, patients with sleep apnea in the follow-up longitudinal National Insurance database were compared with the matched control subjects during the same period, and adjustment several comorbidities, such as psychiatric disorders, cardiovascular morbidities, and insomnia.
Methods
Database
The National Health Insurance (NHI) program was launched by the Taiwanese government on March 1, 1995. The Taiwan NHI database contains data related to prescriptions, diseases, outpatient visits, vital status, and hospital admissions of 1 million beneficiaries randomly drawn from the national population of 23 million. The data used in this study were retrieved from the Taiwan Longitudinal Health Insurance Database 2000 (LHID2000), which is a subset of the Taiwan NHI Research Database (NHIRD) and contains complete records of all medical services provided to one million randomly selected individuals from the national population. The Taiwan National Health Research Institute confirmed that there was no significant difference in population distribution between the LHID2000 and NHIRD and that the LHID2000 is representative of the Taiwanese population of 23.3 million people. The study protocol was approved by the Chia-Yi Christian General Hospital Research Ethics Committee.
Study sample
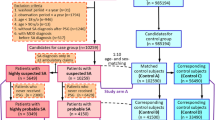
The database used in this study contains detailed inpatient and outpatient records on every visit for each patient. Data from the study cohort was identified by International Classification of Diseases, 9th Revision Clinical Modification (ICD-9-CM) codes registered in patient medical records. The medical records between 2000 and 2010 were used to recruit the sample, which consisted of two cohorts, one is sleep apnea cohort and the other is comparison cohort. The study flowchart is shown in Fig. 1. For the sleep apnea cohort, individuals older than 18 years of age who received a major diagnosis of sleep apnea (ICD-9-CM codes 780.51, 780.53, or 780.57) [12] as newly diagnosed on two separate outpatient visits in 1 year, or one diagnosis of sleep apnea during one session of inpatient care, were recruited. To estimate the validation of ICD-9-CM codes for the identification of sleep apnea, we recruited 50 participants who had of sleep apnea in claim database. In our previous study [18], the results found that the diagnosis of sleep apnea is similar in our clinical database and NHIRD, a positive predictive value of 88 % (95 % confidence interval (CI) 79.0–97.0) for sleep apnea.
The comparison cohort was randomly selected from the remaining insurants who were matched with the study subjects across three age groups (18–34, 35–54, and >55 years), sex, and index year in which the study case was first diagnosed as sleep apnea, with a comparison-to-case ratio of 5:1. None of the comparison individuals received a diagnosis of sleep apnea since the initiation of the NHI program in 1995.
MD was the main outcome followed by this study that was identified based on the diagnosis codes presented in outpatient or inpatient records in the following three categories: major depressive disorders (ICD-9-CM codes 296.2 and 296.3), bipolar disorders (ICD-9-CM codes 296.0, 296.1, and 296.4–296.8), and unspecified episodic MD (ICD-9-CM code 296.9). Subjects diagnosed with MD before being diagnosed with sleep apnea or those with dubitable basic data, such as incorrect subject ID and erroneous gender, were excluded from analysis. Each case in the study cohort was followed until 2011 or until a diagnosis of MD.
Covariates
We used living area, enrollee category (EC), monthly income, and urbanization level as proxy measures representing health care affluence and socioeconomic status in NHI database. In living area, there are four geographic groups, north, central, south, and east and offshore. In Taiwan, the rural-urban disparity exists in health care and social resources; northern Taiwan is the most abundant area than other areas. The EC is divided into the following four subgroups: EC I consisted of governmental servants and public school teachers; EC II, employees of private enterprises or institutions; EC III, the fishing and agrarian populace or self-employed; and EC IV, low-income earners or unemployed pensioners. In general, the familial house income and social position are highest in EC I and lowest in EC IV. The urbanization levels were into the following three categories: urban, suburban, and rural areas. The categories were based on the following five indices: population density, percentages of residents who were agricultural workers, the number of physicians per 100,000 people, percentages of residents with college or higher education, and percentages of residents aged 65 years or older. In general, the inhabitants that live in urban and suburban areas have a higher socioeconomic status.
Based on the clinicians’ opinions, several comorbidities of sleep apnea were also selected for adjustment, including psychiatric disorders, cardiovascular morbidities, and other comorbidities. The codes are shown as follow: schizophrenia (ICD-9-CM code 295), attention deficit and hyperactivity disorder (ICD-9-CM code 314), alcohol/substance abuse (ICD-9-CM codes 312 and 313), anxiety (ICD-9-CM code 300), conduct disorder (ICD-9-CM codes 303–305), mental retardation (ICD-9-CM codes 317–319), post-traumatic stress disorder (PTSD; ICD-9-CM codes 308 and 309), hypertension (ICD-9-CM codes 401 to 405), diabetes mellitus (ICD-9-CM codes 250), hyperlipidemia (ICD-9-CM code 272), chronic obstructive pulmonary disease (COPD; ICD-9-CM codes 491.xx, 492.xx, 494.xx, 496.xx), obesity (ICD-9-CM code 278.0), asthma (ICD-9-CM code 493), coronary artery disease (CVA; ICD-9-CM codes 430 to 438), heart failure (ICD-9-CM codes 425.4, 425.9, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.xx), and insomnia (ICD-9-CM codes 307.41, 307.42, 780.52). The selected comorbidity condition was defined as a diagnosis within 1 year before or after a diagnosis of sleep apnea.
Statistical analysis
Baseline social demographic characteristics between patients with and without sleep apnea were compared using the chi-squared test. Cox proportional hazard regression analysis was used to calculate both the crude and adjusted hazard ratios (HRs), with 95 % CIs, of developing MD after sleep apnea during the follow-up period. Stratified analysis was performed with respect to age groups, sex, and subcategories of MD. We used two adjustment model; one was made for geographical location, enrollee category, monthly income, urbanization level, and all selected comorbidities, and the other was excluded the study subject with psychiatric comorbidities and adjustments were made for geographical location, enrollee category, monthly income, urbanization level, and other comorbidities. All statistical analyses were conducted with SAS 9.3 statistical software (SAS Institute Inc., Cary, NC, USA).
Sensitivity analysis
To assess the effect of other potential residual confounding factors on the observed results, sensitivity analysis was performed according to the R-package “obsSens” [19]. First, an additional hypothetical unmeasured confounding factor was added to this analytical model. Then, the extent of how the added factor confounded the observations with different prevalences was tested in the case and comparison groups.
Results
The total sample size was 32,490 individuals, which included 5415 patients (3613 men, 67 %) diagnosed with sleep apnea from 2000 to 2010 (Table 1). The 27,075 matched comparison patients were selected from the same LHID2000 database. Almost half (46 %) of the patients with sleep apnea were aged 35–54 years, and 32 % were aged >55 years. In terms of geographical distribution, sleep apnea was more common in the northern area of Taiwan (52 %) than in other areas. A high percentage (48 %) of patients with sleep apnea was classified as EC II. The largest proportion of patients with sleep apnea (50 %) resided in the most urbanized locations in Taiwan. After matching by sex, age group, and index year, the patients with sleep apnea were found to be more likely to have the comorbidities, such as cardiovascular morbidities, insomnia, and some psychiatric disorders. Of the seven selected psychiatric comorbidities of sleep apnea, anxiety was the most prevalent.
Table 2 summarizes the details of a total of 154 (2.84 %) patients with sleep apnea who were subsequently diagnosed with MD during the follow-up period up to 2011. Model 1 was all of the study subjects, and model 2 was excluded the participants with psychiatric comorbidities. In the comparison group, 306 (1.13 %) subjects without antecedent sleep apnea were diagnosed as having MD during the follow-up period. After adjusting for geographical location, monthly income, urbanization level, and comorbidities, sleep apnea remained a significant predisposing factor, with a 1.82-fold (95 % CI of adjusted HR 1.47–2.24) increased risk of MD within the follow-up period in model 1 and with a 2.07-fold (95 % CI of adjusted HR 1.60–2.68) increased risk of MD within the follow-up period in model 2. Figure 2 compares the MD survival rates between the two cohorts. Further stratified by sex, both male and female patients with sleep apnea were 1.55-fold (95 % CI 1.15–2.10) and 2.12-fold (95 % CI 1.58–2.85), respectively, more likely to be diagnosed with MD in model 1. The similar results are shown in model 2. When the subjects were stratified into three age groups, the adjusted HRs of being diagnosed with MD after having sleep apnea were significantly higher than in the comparison cohort in the 18–34-year-old group (model 1 HR 1.93, 95 % CI 1.11–3.34; model 2 HR 2.48, 95 % CI 1.34–4.58) and 35–54-year-old group (model 1 HR 1.72, 95 % CI 1.25–2.35; model 2 HR 2.14, 95 % CI 1.46–3.13; Table 3). In men, the risk of MD associated with sleep apnea was highest in those aged 18–34 years (model 1 adjusted HR 1.76; model 2 adjusted HR 2.28), and the highest HR in women was observed for those aged 35–54 years (model 1 adjusted HR 2.32; model 2 adjusted HR 2.31).
A further analysis for MD subgroups stratified by sex revealed HRs across the MD subgroups of major depressive disorder, bipolar disorder, and unspecified MD among patients with sleep apnea (Table 4). The three categories of MD had different risks of being diagnosed after sleep apnea. The sleep apnea group showed significantly higher HRs than the comparison cohort for major depressive disorder (model 1 adjusted HR 1.82; model 2 adjusted HR 2.04) and bipolar disorder (model 1 adjusted HR 2.15; model 2 adjusted HR 3.24). Comparison of the survival rates of different MD subgroups vs. comparison groups is shown in Supplementary Figs. S1, S2, and S3.
We next examined whether there was evidence for synergistic effects of sleep apnea and insomnia on mood disorders (Supplementary Table 1). The evidence of synergy was found. The effect for insomnia alone was 3.15 in model 1 and 3.90 in model 2 and for sleep apnea alone was 1.85 in model 1 and 2.02 in model 2. The combined effect (model 1 adjusted HR 4.31; model 2 adjusted HR 6.34) was greater than the sum of these individual effects. We also considered the interaction for sleep apnea with psychiatric comorbidities (Supplementary Table 2) and with other comorbidities (Supplementary Table 3) on mood disorders. Moreover, we estimated association between treatment of sleep apnea and the risk of mood disorder (Table 5). We observed that the patients without continuous positive airway pressure (CPAP) have higher risk of MD than those with CPAP treatment in both model 1 (HR = 2.02 vs. HR = 0.77) and model 2 (HR = 2.27 vs. HR = 0.98).
Sensitivity analysis was used to investigate the effect of other potential residual confounding factors on the observed results. Considering the estimated trends of the sleep apnea group HR model with the add-on of a residual confounding factor in model 1 (Fig. 3) and in model 2 (Fig. 4), the add-on residual confounder (prevalence of the unmeasured confounder is 1.0), which was characteristic of the non-sleep apnea group (prevalence of the unmeasured confounder is 0.0), the effect of sleep apnea was a risk for MD (HR = 3.61, top line in model 1; HR = 4.12, top line in model 1). It shows that in almost all situations, patients with sleep apnea were at a higher risk of MD occurrence than those without.
Discussion
This population-based cohort study might be the first to reveal causality between sleep apnea and MD using a nationwide dataset, after adjusting for sex, socioeconomic characteristics, and comorbidities. There were several significant findings of this study. First, the HR of patients with sleep apnea diagnosed with MD was significantly higher than that of the comparison cohort. Second, the results indicated a significantly increased risk of MD in patients with sleep apnea aged 18–34 years. Third, major depressive disorder and bipolar disorder were most significantly associated with sleep apnea. These findings may warrant monitoring of the substantial and persistent psychological impact of sleep apnea on adult patients.
The epidemiology study showed that the prevalence of obstructive sleep apnea is approximately 3–7 % [20]. However, the previous NHI database study with 2000–2009 period showed that the incidence of sleep apnea is only 0.7096 % [21], and our study with 2000–2010 period showed that the incidence is 0.7363 %. The incidence rate of our study was similar when compared with the previous study. We found that patients with sleep apnea had a significant higher risk of MD than the comparison cohort in Taiwan. A previous article reported an increased risk of MD (OR 1.85) among patients with obstructive sleep apnea associated with living in a facility and the severity of obesity [22]. Another study also reported that 54.1 % individuals with a diagnosis with bipolar I disorder were at a higher risk for obstructive sleep apnea [23]. In contrast to the aforementioned studies, some previous results found no association between sleep apnea and MD [16, 24]. However, there were some limitations to these two studies, including a high attrition rate, small sample size, and use of a less sensitive tool to predict mood disturbances. Our results and those of most previous studies confirmed the existence of a significant risk of MD in patients with sleep apnea.
We observed that major depressive disorder and bipolar disorder were most associated with sleep apnea and MD. Major depressive disorder is the most influenced disorder caused by obstructive sleep apnea across all psychiatric disorders [7, 25, 26]. Furthermore, some patients diagnosed with sleep apnea also complain of insomnia, which may lead to significant social and personal problems, resulting in depression [6]. A clinical study found that the presence of depression symptomatology is often associated with obstructive sleep apnea [27]. For bipolar disorder, a large-scale cohort study showed that sleep apnea was associated with some psychiatric comorbidities, including depression (21.8 %) and bipolar disorders (3.3 %) [7]; the study also reported that 54.1 % patients with bipolar I disorder were at a higher risk for obstructive sleep apnea [23]. The present study also found a higher probability of major depressive disorder in both men and women, which was particularly notable in women with sleep apnea. Previous studies reported that women with sleep apnea tended to describe their main presenting symptoms as insomnia, and many had a history of depression. Consistent with the previous findings, our large-scale study implied that major depressive disorder may be more common and more severe in women with sleep apnea than in men.
Potential mechanisms explaining the association between sleep apnea and MD have not been clearly delineated. However, a biological plausibility exists. With respect to clinical symptoms, depression is associated and may manifest as insomnia, snoring, and sleepiness [28]. Moreover, sleep fragmentation or oxygen desaturation during sleep might influence the presentation of mood symptoms in patients with sleep apnea. Treatment studies [29, 30] found that hypoxia or hypoxemia in obstructive sleep apnea might play a key role in affecting mood. On the other hand, differences in underlying mechanisms of sleep apnea between men and women also remain unclear. Sleep apnea has been assumed to be predominantly associated with men, rather than women [31]. However, previous studies showed that women with sleep apnea were at a subsequent risk of depression. Our study also found that women tend to have higher HRs than male in both major depressive disorder and bipolar disorder. Women with obstructive sleep apnea are reportedly more prone to fatigue, tiredness, and lack of energy than men [32]. An obstructive sleep apnea study also found that depression, insomnia, morning headaches, and use of sedatives were more pronounced in women than in men [27].
In general, CPAP is the leading therapy for sleep apnea that is a treatment, which uses mild air pressure to keep the airways open [33]. The previous studies reported that the depression scores are significantly lower after CPAP treatment in patients with sleep apnea than a control group [34–36]. The present study found the similar results, which we observed that the sleep apnea patients without CPAP have higher risk of MD compared with sleep apnea patients with CPAP in both model 1 and model 2. The original experiments with CPAP followed from the concept that closure of the oropharynx in OSA syndrome results from an imbalance of the forces that normally keep the upper airway open. Detailed magnetic resonance imaging has confirmed that CPAP increases airway volume and airway area and reduces lateral pharyngeal wall thickness and the upper airway edema that result from chronic vibration and occlusion of the airway [37]. Clinically, quality of life and psychological status both got improved after CPAP treatment was initiated for OSA patient according to one prospective study [38]. Evidence from meta-analysis article revealed that CPAP might be a useful component of treatment of depressive symptoms in individuals with OSA [39]. Thus, less incidence rate of mood disorder in sleep apnea patient on CPAP treatment in our study corresponded with above study findings.
The present study had some limitations that should be considered when interpreting the results. First, we retrieved information only from insurance claims in the NHI database of Taiwan, which includes only those patients who utilized health care resources. Hence, a selection bias may exist, as those with sleep apnea or mental illness may not access medical services because of various individual factors, such as personal unawareness, economic difficulties, or social stigma. However, the accessibility of medical services has generally improved for such individuals in Taiwan because of the extensive network of these services and the affordable copayment system for medical expenses. Second, the Taiwan NHI database included the treated patients. The MD patients who have minor symptoms or did not seek medical advice may not be included in the database. Thus, the present study investigated the association between sleep apnea and MD that may be severe symptoms. The association between sleep apnea and MD with minor or mild symptoms would be explored further. Third, diagnoses of the conditions examined in this work may often be arbitrarily given by physicians based on their clinical judgment and relevant clinical information, including symptoms and signs, which is not accessible from the delinked NHIRD. Misclassification of cases is possible because of individual variations in diagnoses of psychiatric symptoms. Finally, patients in Taiwan would receive a formal report with apnea–hypopnea index (AHI) score after they had PSG test performed overnight in sleep center. However, the definite AHI score of each patient would be documented only in medical chart but would not be included in NHI database.
In conclusion, this population-based, retrospective, follow-up study demonstrated that sleep apnea is associated with MD, and a causal correlation between sleep apnea and subsequent MD was clearly evident. According to the results, the adverse psychological effects of sleep apnea should not be overlooked. Health professionals should also carefully monitor and provide care for both the physical and psychological outcomes of patients with sleep apnea, and such efforts may need to continue for many years, possibly even until old age.
References
Morgenthaler TI, Kagramanov V, Hanak V, Decker PA (2006) Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep 29(9):1203–1209
Lee W, Nagubadi S, Kryger MH, Mokhlesi B (2008) Epidemiology of obstructive sleep apnea: a population-based perspective. Expert Rev Respir Med 2(3):349–364
Tasali E, Mokhlesi B, Van Cauter E (2008) Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest 133(2):496–506
Sheu JJ, Wu CS, Lin HC (2012) Association between obstructive sleep apnea and sudden sensorineural hearing loss: a population-based case-control study. Arch Otolaryngol Head Neck Surg 138(1):55–59
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373(9657):82–93
Baran AS, Richert AC (2003) Obstructive sleep apnea and depression. CNS Spectr 8(2):128–134
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M (2005) Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 28(11):1405–1411
Lin WC, Winkelman JW (2012) Obstructive sleep apnea and severe mental illness: evolution and consequences. Curr Psychiatry Rep 14(5):503–510
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep. Apnea Physiological Reviews 90(1):47–112
Kjelsberg FN, Ruud EA, Stavem K (2005) Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med 6(4):341–346
Saunamäki T, Jehkonen M (2007) Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand 116(5):277–288
Chen YH, Keller JK, Kang JH, Hsieh HJ, Lin HC (2013) Obstructive sleep apnea and the subsequent risk of depressive disorder: a population-based follow-up study. J Clin Sleep Med 9(5):417–423
Ohayon MM (2003) The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry 64(10):1195–1200
El-Sherbini AM, Bediwy AS (2011) Association between obstructive sleep apnea (OSA) and depression and the effect of continuous positive airway pressure (CPAP) treatment. Neuropsychiatr Dis Treat 7(7):715–721
Hattori M, Kitajima T, Mekata T, Kanamori A, Imamura M, Sakakibara H, Kayukawa Y, Okada T, Iwata N (2009) Risk factors for obstructive sleep apnea syndrome screening in mood disorder patients. Psychiatry Clin Neurosci 63(3):385–391
Bliwise DL, Yesavage JA, Sink J, Widrow L, Dement WC (1986) Depressive symptoms and impaired respiration in sleep. J Consult Clin Psychol 54(5):734–735
Bardwell WA, Ancoli-Israel S, Dimsdale JE (2001) Response bias influences mental health symptom reporting in patients with obstructive sleep apnea. Ann Behav Med 23(4):313–317
Lee YC, Hung SY, Wang HK, Lin CW, Wang HH, Chen SW, Chang MY, Ho LC, Chen YT, Liou HH, Tsai TC, Tseng SH, Wang WM, Lin SH, Chiou YY (2014) Sleep apnea and the risk of chronic kidney disease: a nationwide population-based cohort study. Sleep 38(2):213–221
Lin DY, Psaty BM, Kronmal RA (1998) Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics 54(3):948–963
Bresnitz EA, Goldberg R, Kosinski RM (1993) Epidemiology of obstructive sleep apnea. Epidemiol Rev 16(2):210–227
Shiao TH, Liu CJ, Luo JC, Su KC, Chen YM, Chen TJ, Chou KT, Shiao GM, Lee YC (2013) Sleep apnea and risk of peptic ulcer bleeding: a nationwide population-based study. Am J Med 126(3):249–255
Babson KA, Del Re AC, Bonn-Miller MO, Woodward SH (2013) The comorbidity of sleep apnea and mood, anxiety, and substance use disorders among obese military veterans within the veterans health administration. J Clin Sleep Med 9(12):1253–1258
Soreca I, Levenson J, Lotz M, Frank E, Kupfer DJ (2012) Sleep apnea risk and clinical correlates in patients with bipolar disorder. Bipolar Disord 14(6):672–676
Phillips BA, Berry DT, Lipke-Molby TC (1996) Sleep-disordered breathing in healthy, aged persons. Fifth and final year follow-up. Chest 110(3):654–658
Yilmaz E, Sedky K, Bennett DS (2013) The relationship between depressive symptoms and obstructive sleep apnea in pediatric populations: a meta-analysis. J Clin Sleep Med 9(11):1213–1220
Ejaz SM, Khawaja IS, Bhatia S, Hurwitz TD (2011) Obstructive sleep apnea and depression: a review. Innov Clin Neurosci 8(8):17–25
Quintana-Gallego E, Carmona-Bernal C, Capote F, Sánchez-Armengol A, Botebol-Benhamou G, Polo-Padillo J, Castillo-Gómez J (2004) Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med 98(10):984–989
Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W (2008) Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep 31(4):473–480
Derderian SS, Bridenbaugh RH, Rajagopal KR (1988) Neuropsychologic symptoms in obstructive sleep apnea improve after treatment with nasal continuous positive airway pressure. Chest 94(5):1023–1027
Bardwell WA, Norman D, Ancoli-Israel S, Loredo JS, Lowery A, Lim W, Dimsdale JE (2007) Effects of 2-week nocturnal oxygen supplementation and continuous positive airway pressure treatment on psychological symptoms in patients with obstructive sleep apnea: a randomized placebo-controlled study. Behav Sleep Med 5(1):21–38
Crocker BD, Olson LG, Saunders NA (1990) Estimation of the probability of disturbed breathing during sleep before a sleep study. Am Rev Respir Dis 142(1):14–18
Chervin RD (2000) Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest 118(2):372–379
Aurora RN, Chowdhuri S, Ramar K, Bista SR, Casey KR, Lamm CI, Kristo DA, Mallea JM, Rowley JA, Zak RS, Tracy SL (2012) The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep 35(1):17–40
Yu BH, Ancoli-Israel S, Dimsdale JE (1999) Effect of CPAP treatment on mood states in patients with sleep apnea. J Psychiatr Res 33(5):427–432
Fidan F, Unlü M, Sezer M, Geçici O, Kara Z (2006) Compliance to CPAP treatment and effects of treatment on anxiety and depression in patients with obstructive sleep apnea syndrome. Tuberk Toraks 55(3):271–277
Sánchez AI, Martínez P, Miró E, Bardwell WA, Buela-Casal G (2009) CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med Rev 13(3):223–233
Schwab RJ, Pack AI, Gupta KB, Metzger LJ, Oh E, Getsy JE, Hoffman EA, Gefter WB (1996) Upper airway and soft tissue structural changes induced by CPAP in normal subjects. Am J Respir Crit Care Med 154(4):1106–1116
Diamanti C, Manali E, Ginieri-Coccossis M, Vougas K, Cholidou K, Markozannes E, Bakakos P, Liappas I, Alchanatis M (2013) Depression, physical activity, energy consumption, and quality of life in OSA patients before and after CPAP treatment. Sleep Breath 17(4):1159–1168
Povitz M, Bolo CE, Heitman SJ, Tsai WH, Wang J, James MT (2014) Effect of treatment of obstructive sleep apnea on depressive symptoms: systematic review and meta-analysis. PLoS Med 11(11):e1001762
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Chia-Yi Christian General Hospital Research Ethics Committee.
Funding
No funding was received for this research.
Additional information
Ming-Kun Lu and Hung-Pin Tan contributed equally to the study.
Electronic supplementary material
Supplementary Fig. 1
(DOCX 58 kb)
Supplementary Fig. 2
(DOCX 52 kb)
Supplementary Fig. 3
(DOCX 55 kb)
Supplementary Table 1
(DOCX 37 kb)
Supplementary Table 2
(DOCX 36 kb)
Supplementary Table 3
(DOCX 36 kb)
Rights and permissions
About this article
Cite this article
Lu, MK., Tan, HP., Tsai, IN. et al. Sleep apnea is associated with an increased risk of mood disorders: a population-based cohort study. Sleep Breath 21, 243–253 (2017). https://doi.org/10.1007/s11325-016-1389-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1389-x