Abstract
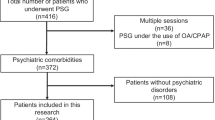
Sleep complaints are commonly encountered in psychiatric clinics. Underlying medical disorders or sleep disorders need to be identified and treated to optimize treatment of the mental illness. Excessive daytime sleepiness, which is the main symptom of obstructive sleep apnea (OSA), overlaps with those of many severe mental illnesses. Medication side effects or the disorder itself maybe account for daytime sleepiness but comorbid OSA is a possibility that should not be overlooked. The diagnosis of OSA is straightforward but treatment compliance is problematic in psychiatric patients. This article summarizes studies concerning comorbid OSA in patients with severe mental illness and includes suggestions for future investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive Sleep Apnea (OSA) is a chronic disorder characterized by repetitive upper airway obstruction during sleep leading to apneic or hypopneic episodes, hypoxemia, and recurrent arousals from sleep [1]. The prevalence rate of OSA with daytime sleepiness has been estimated at 2 %–4 % of middle-aged men and 1 %–2 % of middle-aged women [2]. OSA is associated with considerable morbidity and mortality, particularly from hypertension, cardiovascular disease, and insulin resistance [3]. In addition, the excessive daytime sleepiness related to OSA decreases quality of life [4] and increases risk for motor vehicle accidents [5]. Clinically, OSA is most often treated with continuous positive airway pressure (CPAP) [6], or with an oral appliance [7].
People with severe mental illness have shorter life spans (by 25 years or more) compared with the general population. Much of the excess mortality is due to the high prevalence of physical illness, such as cardiovascular disease, rather than suicide [8]. Despite improvement in mental health services for decades, the mortality rate remains elevated in people with schizophrenia [9]. Optimizing the general health of people with severe mental illness warrants urgent attention. Identifying and treating OSA in these patients is important.
Patients with OSA have substantial comorbidity with severe psychiatric disorders such as depression, anxiety, bipolar disorder, schizophrenia, post traumatic stress syndrome (PTSD), panic disorders, and substance use disorder. In a large cohort study of 4,060,504 subjects from the Veterans Health Administration databases in which 2.9 % were identified as having sleep apnea, psychiatric comorbid diagnoses in the OSA group included depression (21.8 %), anxiety (16.7 %), PTSD (11.9 %), psychosis (5.1 %), and bipolar disorders (3.3 %) [10]. In this manuscript, we will review the literature regarding OSA and these severe mental illnesses to address the importance of identifying OSA in psychiatric patients, discuss shared consequences of the 2 disorders, and assess the effect of treatment of OSA on comorbid psychiatric disorders.
OSA and Depression
Depression is the most common mood disorder in patients with OSA [11]. The prevalence rate of depression in OSA ranges from 7 % to 63 % depending upon the study [12]. Most studies that evaluated the association between OSA and depression were conducted on relatively small clinical populations of patients; fewer were performed in the general, non-clinical populations. A large telephone survey of 18,980 subjects representative of the general population aged 15 to 100 years in 5 European countries found that 17.6 % of subjects with a Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) breathing related sleep disorder diagnosis (without sleep study performed) had major depressive disorder (MDD) [13]. Depressed participants were 5 times more likely to have a DSM-IV breathing related sleep disorder. A recent epidemiological study of 9714 adults from the National Health and Nutrition Examination Survey (NHANES) for the years 2005–2008 demonstrated that sleep apnea was associated with probable major depression, which was diagnosed via a questionnaire [14•]. It also found snoring was not associated with depression but snorting/stopping breathing more than 5 times a week compared with never having these symptoms was strongly associated with probable major depression.
A number of earlier studies did not find an association between the 2 disorders. One study that examined a large male population (n = 1977) found that depression was not associated with either existence or the severity of OSA [15]. Other studies observed that patients with sleep apnea did not have clinically significant levels of depression, nor did they have higher levels of depressive symptoms than normal controls [16, 17]. However, a recent study demonstrated a dose-response association between OSA severity (apnea-hypopnea index, AHI, number of apneas, and hypopneas per hour of sleep) and depression [18], such that the prevalence of depression was increased with increasing severity of OSA.
These variable findings may stem from several reasons. First, OSA and depression share some common symptoms such as sleepiness, fatigue, sleep disturbance, psychomotor retardation, poor concentration, low sexual drive, and irritability. Thus, it may be difficult to distinguish these 2 disorders (particularly in questionnaire-based studies) and researchers have used different measurements, cut-points, or psychiatric interviews to evaluate depression in OSA. This might lead to a reduced reliability of psychiatric diagnoses and confound the association between OSA and depression. Second, although OSA is diagnosed by nocturnal polysomnography (PSG), epidemiological surveys of large populations have used questionnaires to make this diagnosis, often using alternative diagnoses such as sleep related breathing disorders or DSM-IV breathing related sleep disorders. This diagnostic limitation is one of the fundamental difficulties in this area. Third, OSA is most common in the elderly, obese, and those with medical comorbidities, factors that are also more common in depression and may confound the relationship between OSA and depression. In fact, one study suggested that depression in OSA patients may be determined by confounding factors such as age, body mass, and hypertension [19]. The authors also argued that depression may account for the fatigue seen in OSA, after controlling for OSA severity [20]. Due to the complex relationship between OSA and depression, evaluation of the bidirectional relationship between mood disorder and OSA in the clinical setting and in future research efforts is essential.
Treatment options for OSA include weight loss, positional therapy, mandibular advancement devices, surgery to remove soft tissues causing upper airway obstruction, and continuous positive airway pressure (CPAP) [21]. The gold standard treatment of OSA currently is CPAP, but compliance may be problematic. One study reported that lower pretreatment depressive symptoms may predict better compliance [22]. A number of studies have examined whether CPAP treatment improved depressive symptoms; although numerous studies reported a positive effect of CPAP on mood, the evidence is not consistent. An anecdotal report described resolution of untreated depressed OSA patient’s depression and suicidal ideation promptly after initiation of CPAP treatment [23]. One previous study demonstrated that OSA patients with more severe depressive symptoms responded better to CPAP, whereas patients with less severe or no mood symptoms may benefit less from CPAP treatment [24]. Long-term follow-up studies in patients with various severity of OSA and a broader range of depressive symptoms are needed to examine whether CPAP is beneficial to mood in OSA patients with depression and how to improve depressed OSA patients’ compliance to CPAP.
There are some suggestions from basic studies in animals that antidepressants may have value in the treatment of OSA through their effects on upper airway dilator motor neurons [25, 26]. Furthermore, antidepressants may exert some beneficial effect in OSA by their REM sleep suppression since OSA symptoms tend to worsen in REM sleep when muscle tone is lowest. In clinical studies, several serotonergic medications such as protryptiline, fluoxetine, paroxetine, and mirtazapine have been examined in the treatment of OSA with limited benefit but significant side-effects [27, 28•]. When treating depressed OSA patients, SSRIs are generally well tolerated but other sedating antidepressants with side-effects of weight gain (mainly with H1 receptor blockade properties) may exacerbate OSA.
In the clinical setting, when depressed patients present with symptoms such as excessive daytime fatigue and sleepiness and/or snoring, clinicians should suspect OSA [29]. Refractory depression may be akin to refractory hypertension, in that both instances may possibly denote occult OSA [30]. Identifying OSA in patients with depression is important since some pharmacological treatments of depression may exacerbate OSA; some sedating antidepressants or atypical antipsychotics may produce weight gain, and benzodiazepines may exacerbate daytime sedation. Furthermore, benzodiazepines produce mild respiratory suppression and may blunt the arousal response, both of which could inhibit resumption of breathing effort and further increase the severity of OSA.
OSA and Anxiety Disorder
Although less common than depression, the prevalence of anxiety ranges from 11 % to 70 % in OSA patients [12]. One study found higher level of anxiety in OSA patients than in healthy controls [31]. Another later study found that severity of OSA is not associated with the severity of depression and anxiety symptoms [32]. A recent paper indicated that more severe OSA symptoms are related to a more severe oxidative stress state, which they proposed could be responsible for the daytime symptoms such as sleepiness, depression, and anxiety [33]. OSA patients with comorbid MDD and anxiety had higher C-reactive protein (CRP) level, which indicates systemic inflammation [34]. Two studies found that anxiety or depression is related to poor compliance with CPAP treatment [35, 36]. Such non-adherence to treatment may be related to comorbid insomnia, which is more common in OSA patients with anxiety [37]. Hence, treatment of the anxiety symptoms in OSA patients may be necessary to insure CPAP compliance and prevent other physical and psychological sequelae.
OSA and Bipolar Disorder
Few studies have investigated OSA and bipolar disorder. All of them are anecdotal reports, which describe that CPAP treatment might switch depressed patients to mania [38, 39]. Just as refractory depression might be associated with undiagnosed OSA, refractory mania may also related to untreated underlying OSA, since sleep disruption and reduction may cause mania [40•]. The prevalence rate of comorbid OSA and bipolar disorder is not clear. To treat bipolar patients with underlying OSA is a clinical challenge. Many mood stabilizers such as anticonvulsants or antipsychotics may produce weight gain. Furthermore, heavy sedative administration, which is often administered to manic patients, may exacerbate OSA or even cause respiratory failure [41].
OSA and Schizophrenia
The rate of comorbid OSA in schizophrenic patients is not clear. In our previous study done with inpatient psychiatric consultations, schizophrenics had sleep apnea diagnosed on sleep study over 6 times more frequently than patients with other psychiatric diagnoses. Obesity, male gender, and chronic neuroleptic administration were risk factors for OSA in schizophrenic patients [42]. Ancoli-Israel et al found higher rates of OSA (48 % with an RDI > 10 and 20 % with an RDI > 20) in elderly schizophrenic outpatients [43]. They found no relationship between Body Mass Index (BMI) and sleep apnea risk but demonstrated a positive correlation between age and risk of OSA. A Japanese study showed 18.8 % (19/101, men 21.9 %, women 13.5 %) of psychiatric inpatients with schizophrenia had sleep apnea, which was not higher than that of the healthy control group (22.9 %, 11/48, men 30.7 %, women 13.6 %) [44]. However, the mean BMI of the overall sample was 24.0, which is atypically low for many schizophrenic patients, and they evaluated nocturnal respiration with oximetry alone, which may underestimate OSA. Metabolic syndrome is an important side effect of atypical antipsychotics. An 8-year cohort study [45] reported a 28.4 % prevalence rate of metabolic syndrome related to weight gain in schizophrenic patients (n = 189) who had received clozapine treatment. Given that sleep disordered breathing is correlated with metabolic syndrome [46•], clinicians need to focus on both metabolic syndrome and OSA.
Although OSA might contribute to the cardiovascular disease and increased mortality of this population, it is underdiagnosed in schizophrenic patients, as excessive daytime sleepiness, the most common daytime symptom of OSA, may be misattributed to negative symptoms or medication side-effects. A case report described a schizophrenic patient with OSA who received CPAP therapy with resulting AHI reduction from 43.6 to 2.3. Negative symptoms such as blunted affect, psychomotor poverty, and fatigue improved [47].
It may be difficult at times to distinguish whether CPAP improves daytime sleepiness or negative symptoms. In chronic schizophrenic patients, long-term use of antipsychotics can lead to weight gain and metabolic syndrome, both of which are risk factors for cardiovascular disease. Identification of comorbid OSA in schizophrenic patients is valuable and administration of CPAP may reduce the risk of cardiovascular events and might improve psychiatric status [48] although they have poor compliance of CPAP [49].
OSA and Post Traumatic Stress Syndrome (PTSD)
Sleep complaints are critical in the constellation of symptoms in DSM IV-defined PTSD [50]. PTSD diagnostic criterion B includes nightmares, which have been designated the “hallmark symptoms” of PTSD [51] and criterion D includes insomnia and other parasomnias.
Sleep disordered breathing (SDB) has been found in a number of case series of PTSD patients [52, 53]. A recent study [54•] reported 69 % of 105 Vietnam-era veterans with PTSD had an AHI >10. Another study [55] compared symptoms in typical OSA patients with those with comorbid OSA and PTSD. They found that both groups reported high rates of fatigue or sleepiness, nocturia, morning dry mouth, and morning headaches but those with PTSD had more insomnia and nightmares. Furthermore, OSA severity was associated with poor cognitive performance in those with PTSD [56•]. Apnea induced arousals promote sleep fragmentation which can exacerbate nightmares, sleepwalking and sleep terrors, and can be diminished by CPAP therapy [57, 58]. Some reports suggest that treatment of sleep disturbance alleviates PTSD [59]. Therefore, it is reasonable to anticipate that treatment of comorbid OSA in PTSD patients is beneficial for improving both disorders [60]. However, non-adherence of CPAP treatment in PTSD patients is high. Non-adherent patients often endorse more severe nightmares [61]. Alternatively, CPAP related REM sleep rebound may increase nightmares and thereafter discourage patients from use of CPAP. Whether nightmare reducing treatments such as image rehearsal treatment or pharmacotherapy by prazosin can enhance CPAP compliance deserves further investigation.
OSA and Panic Disorder (PD)
Patients with panic disorder (PD) often report having sleep disturbance, predominantly initial insomnia, broken sleep, and nocturnal panic attacks. A prevalence of 68 % for difficulties in falling asleep and of 77 % for disturbed sleep has been reported [62]. Among these sleep complaints, sleep apnea has seldom been reported. In an earlier study, the authors found PD patients have an increased rate of micro-apneas (5–10 seconds) during sleep [63].
Nocturnal panic attacks arise mainly during non-rapid eye movement (NREM) sleep at the late stage 2/3 boundary [64–66]. As with daytime panic attacks, they often occur unexpectedly, without an obvious trigger among 28 %–71 % PD patients [67–69]. One previous study depicted that PD patients with prominent respiratory symptoms have increased rates of spontaneous and nocturnal panic attacks [70]. Another recent study demonstrated that patients with nocturnal panic attacks have more respiratory-related panic symptoms, as well as depressive, and other psychiatric symptoms compared with the no nocturnal panic group [71]. By contrast, 2 other studies found no correlation between respiratory panic symptoms and nocturnal panic attacks [72, 73]. Although none of these studies directly examined the effects of comorbid OSA in PD, an earlier study demonstrated that nocturnal panic symptoms do occur in patients with sleep apnea and mostly decreased after treatment of OSA. The authors suggested that more than 5 % of sleep apnea patients have panic attack symptoms [74]. OSA in children was associated with increased urinary catecholamine [75], and since PD patients have abnormalities in noradrenergic systems [76], these 2 disorders may be related. A study [77] conducted in Japan reported that 1 night of CPAP treatment lowered urinary adrenaline and noradrenaline. Another recent study found that PD patients with OSA can benefit from CPAP treatment to decrease panic attack symptoms and reduce the frequency of alprazolam use [78•]. As there is evidence that sleep deprivation triggers panic attack in sleep [69], CPAP treatment may stabilize sleep and prevent further panic attacks. It is important to diagnose underlying OSA in PD patients, especially with nocturnal panic attacks since proper treatment of OSA might be beneficial for decreasing panic symptoms.
OSA and Substance Use Disorder (SUD)
Sleep problems are common in people with psychiatric disorders including SUD and were significantly related to role impairment .People with SUD have an insomnia complaint over 2.5 times as often as those in the general population [79]. Conversely, adolescents with sleep problems and daytime sleepiness are more likely to use licit or illicit substances [80, 81]. There are few studies regarding SUD and specific sleep disorders though many commonly prescribed medications and substances of abuse can have significant effects on sleep and wakefulness [82]. A study evaluated 30 SUD subjects by questionnaire and found that the majority of them had insomnia, or symptoms consistent with sleep apnea, or restless leg syndrome [83].
Sleep problems are more common among alcoholics, especially elderly alcoholics than among nonalcoholics [84]. As people commonly use alcohol to self-medicate sleep problems, such problems may predispose people to develop alcohol use problems [85] or increase the risk of relapse among abstinent alcoholics [86]. Researchers have long found that alcohol increased the severity of OSA [87] and exacerbated hypoxemia [88]. The possible cause is that alcohol induces oropharyngeal muscle hypotonia and depression of arousal mechanisms as well as weight gain [89]. A recent study depicted that patients with OSA are more vulnerable than healthy persons to the effects of alcohol consumption and sleep restriction on driving performance [90•]. OSA patients should reduce or abstain from alcohol intake, particularly during night-time. Those treating alcoholics should be aware of OSA and offer proper treatment if indicated.
Methadone maintenance therapy (MMT) is an essential therapeutic substitution method of heroin addiction [91]. As a long-acting μ-opioid agonist, methadone has been shown to cause blunted hypercapnic and heightened hypoxic ventilatory responsiveness in patients receiving MMT [92]. In the United States, since methadone prescriptions for pain management grew from about 531,000 in 1998 to about 4.1 million in 2006 [93], methadone-related sleep breathing disorders deserve more attention. A study showed central sleep apnea is not uncommon in MMT patients [94], although obstructive sleep apnea is more common than central sleep apnea in MMT patients with subjective sleep complaints [95]. MMT has been shown to increase sleep apnea [96] and poor sleep quality [97]. However, another study demonstrated that subjective daytime sleepiness and daytime function of patients on stable MMT are not affected by changes in sleep architecture, presence of central sleep apnea, or the blood concentration of methadone [98]. Clinicians should closely monitor sleep-related symptoms and investigate both OSA and CSA (central sleep apnea) in these patients when prescribing and adjusting methadone dosage.
There is only 1 study which investigated methylenedioxymethamphetamine (MDMA, “ecstasy”) and OSA [99]. The authors suggested prior recreational use of MDMA increased the risk of OSA. As a neurotoxin to serotonergic neurons, this finding further suggested that brain serotonergic neuron dysfunction may play a role in the pathogenesis of OSA. Serotonin dysfunction-related impaired chemoreflex or arousal system seems more likely to be the key effects on OSA [100]. It is important to educate people who may be abusing MDMA that this drug may cause OSA, which may contribute to developing cardiovascular sequelae, stroke, and death. As for other recreational drugs, OSA-related investigations are lacking.
Conclusion
Practicing psychiatrists and psychologists must consider OSA in the differential diagnosis in every patient with sleep disturbance and severe mental illness in everyday practice. Patients often come with a variety of sleep complaints such as difficulty falling asleep, broken sleep, and daytime sleepiness. In the short-term, sedating medication effects should be considered, and in the long-term, drug induced weight gain, which can lead to OSA, needs to be taken into consideration. As OSA is associated with a higher prevalence of psychiatric comorbid conditions, patients with psychiatric disorders and coincident symptoms suggesting sleep disordered breathing should be evaluated for OSA. Identifying underlying OSA, which can be easily diagnosed by sleep study, is essential to reduce further psychiatric and cognitive burdens in an already disadvantaged population, and to address significant cardio-vascular, metabolic, and other physiologic morbidity. CPAP compliance is often poor in psychiatric patients, and additional attention to barriers to use is necessary in such patients. Attention to the prescription of medications that can induce weight gain is crucial in patients with a high risk of comorbid OSA such as the obese or elderly. Future studies concerning mutual effects of OSA and psychiatric disorder are indicated.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Gibson GJ. Obstructive sleep apnoea syndrome: underestimated and undertreated. Br Med Bull. 2004;72:49–65.
Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39.
Pack AI. Advances in sleep-disordered breathing. Am J Respir Crit Care Med. 2006;173:7–15.
Jenkinson C, Stradling J, Petersen S. Comparison of three measures of quality of life outcome in the evaluation of continuous positive airways pressure therapy for sleep apnoea. J Sleep Res. 1997;6:199–204.
George CF, Nickerson PW, Hanly PJ, Millar TW, Kryger MH. Sleep apnoea patients have more automobile accidents. Lancet. 1987;2:447.
Suzuki M, Otsuka K, Guilleminault C. Long-term nasal continuous positive airway pressure administration can normalize hypertension in obstructive sleep apnea patients. Sleep. 1993;16:545–9.
Gotsopoulos H, Chen C, Qian J, Cistulli PA. Oral appliance therapy improves symptoms in obstructive sleep apnea: a randomized, controlled trial. Am J Respir Crit Care Med. 2002;166:743–8.
Newcomer JW, Hennekens CH. Severe mental illness and risk of cardiovascular disease. JAMA. 2007;298:1794–6.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–31.
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28:1405–11.
Andrews JG, Oei TP. The roles of depression and anxiety in the understanding and treatment of obstructive sleep apnea syndrome. Clin Psychol Rev. 2004;24:1031–49.
Saunamaki T, Jehkonen M. Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand. 2007;116:277–88.
Ohayon MM. The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry. 2003;64:1195–200. quiz, 274–6.
• Wheaton AG, Perry GS, Chapman DP, Croft JB. Sleep Disordered Breathing and Depression among U.S. Adults: National Health and Nutrition Examination Survey, 2005–2008. Sleep. 2012;35:461–7. This national study found that sleep disordered breathing may be associated with probable major depression..
Pillar G, Lavie P. Psychiatric symptoms in sleep apnea syndrome: effects of gender and respiratory disturbance index. Chest. 1998;114:697–703.
Lee S. Depression in sleep apnea: a different view. J Clin Psychiatry. 1990;51:309–10.
Gall R, Isaac L, Kryger M. Quality of life in mild obstructive sleep apnea. Sleep. 1993;16(8 Suppl):S59–61.
Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med. 2006;166:1709–15.
Bardwell WA, Berry CC, Ancoli-Israel S, Dimsdale JE. Psychological correlates of sleep apnea. J Psychosom Res. 1999;47:583–96.
Bardwell WA, Moore P, Ancoli-Israel S, Dimsdale JE. Fatigue in obstructive sleep apnea: driven by depressive symptoms instead of apnea severity? Am J Psychiatry. 2003;160:350–5.
Caples SM, Gami AS, Somers VK. Obstructive sleep apnea. Ann Intern Med. 2005;142:187–97.
Edinger JD, Carwile S, Miller P, Hope V, Mayti C. Psychological status, syndromatic measures, and compliance with nasal CPAP therapy for sleep apnea. Percept Mot Skills. 1994;78(3 Pt 2):1116–8.
Krahn LE, Miller BW, Bergstrom LR. Rapid resolution of intense suicidal ideation after treatment of severe obstructive sleep apnea. J Clin Sleep Med. 2008;4:64–5.
Millman RP, Fogel BS, McNamara ME, Carlisle CC. Depression as a manifestation of obstructive sleep apnea: reversal with nasal continuous positive airway pressure. J Clin Psychiatry. 1989;50:348–51.
Berger AJ, Bayliss DA, Viana F. Modulation of neonatal rat hypoglossal motoneuron excitability by serotonin. Neurosci Lett. 1992;143:164–8.
Fenik P, Veasey SC. Pharmacological characterization of serotonergic receptor activity in the hypoglossal nucleus. Am J Respir Crit Care Med. 2003;167:563–9.
Veasey SC. Serotonin agonists and antagonists in obstructive sleep apnea: therapeutic potential. Am J Respir Med. 2003;2:21–9.
• Marshall NS, Yee BJ, Desai AV, Buchanan PR, Wong KK, Crompton R, et al. Two randomized placebo-controlled trials to evaluate the efficacy and tolerability of mirtazapine for the treatment of obstructive sleep apnea. Sleep. 2008;31:824–31. This study found that mirtazapine has limited benefit for treatment of OSA.
Kaplan R. Obstructive sleep apnoea and depression–diagnostic and treatment implications. Aust N Z J Psychiatry. 1992;26:586–91.
Farney RJ, Lugo A, Jensen RL, Walker JM, Cloward TV. Simultaneous use of antidepressant and antihypertensive medications increases likelihood of diagnosis of obstructive sleep apnea syndrome. Chest. 2004;125:1279–85.
Munoz A, Mayoralas LR, Barbe F, Pericas J, Agusti AG. Long-term effects of CPAP on daytime functioning in patients with sleep apnoea syndrome. Eur Respir J. 2000;15:676–81.
Asghari A, Mohammadi F, Kamrava SK, Tavakoli S, Farhadi M. Severity of depression and anxiety in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2012.
Franco CM, Lima AM, Ataide L, Jr., Lins OG, Castro CM, Bezerra AA, et al. Obstructive sleep apnea severity correlates with cellular and plasma oxidative stress parameters and affective symptoms. J Mol Neurosci. 2012.
Einvik G, Hrubos-Strom H, Randby A, Nordhus IH, Somers VK, Omland T, et al. Major depressive disorder, anxiety disorders, and cardiac biomarkers in subjects at high risk of obstructive sleep apnea. Psychosom Med. 2011;73:378–84.
Kjelsberg FN, Ruud EA, Stavem K. Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med. 2005;6:341–6.
Chasens ER, Pack AI, Maislin G, Dinges DF, Weaver TE. Claustrophobia and adherence to CPAP treatment. West J Nurs Res. 2005;27:307–21.
Yang CM, Liao YS, Lin CM, Chou SL, Wang EN. Psychological and behavioral factors in patients with comorbid obstructive sleep apnea and insomnia. J Psychosom Res. 2011;70:355–61.
Berge D, Salgado P, Rodriguez A, Bulbena A. Onset of mania after CPAP in a man with obstructive sleep apnea. Psychosomatics. 2008;49:447–9.
Hilleret H, Jeunet E, Osiek C, Mohr S, Blois R, Bertschy G. Mania resulting from continuous positive airways pressure in a depressed man with sleep apnea syndrome. Neuropsychobiology. 2001;43:221–4.
• Plante DT, Winkelman JW. Sleep disturbance in bipolar disorder: therapeutic implications. Am J Psychiatry. 2008;165:830–43. This is a thorough review about bipolar disorder and sleep disorders..
Bastiampillai T, Khor LJ, Dhillon R. Complicated management of mania in the setting of undiagnosed obstructive sleep apnea. J ECT. 2011;27:e15–6.
Winkelman JW. Schizophrenia, obesity, and obstructive sleep apnea. J Clin Psychiatry. 2001;62:8–11.
Ancoli-Israel S, Martin J, Jones DW, Caligiuri M, Patterson T, Harris MJ, et al. Sleep-disordered breathing and periodic limb movements in sleep in older patients with schizophrenia. Biol Psychiatry. 1999;45:1426–32.
Takahashi KI, Shimizu T, Sugita T, Saito Y, Takahashi Y, Hishikawa Y. Prevalence of sleep-related respiratory disorders in 101 schizophrenic inpatients. Psychiatry Clin Neurosci. 1998;52:229–31.
Bai YM, Lin CC, Chen JY, Chen TT, Su TP, Chou P. Association of weight gain and metabolic syndrome in patients taking clozapine: an 8-year cohort study. J Clin Psychiatry. 2011;72:751–6.
• Hall MH, Okun ML, Sowers M, Matthews KA, Kravitz HM, Hardin K, et al. Sleep is associated with the metabolic syndrome in a multi-ethnic cohort of midlife women: The SWAN Sleep Study. Sleep. 2012;35:783–90. This cohort study found that sleep disordered breathing is associated with metabolic syndrome in women..
Sugishita K, Yamasue H, Kasai K. Continuous positive airway pressure for obstructive sleep apnea improved negative symptoms in a patient with schizophrenia. Psychiatry Clin Neurosci. 2010;64:665.
Strakowski SM, Hudson JI, Keck Jr PE, Wilson DR, Frankenburg FR, Alpert JE, et al. Four cases of obstructive sleep apnea associated with treatment-resistant mania. J Clin Psychiatry. 1991;52:156–8.
Cunningham SL, Ellsworth SD, Winkelman JW, Dorsey CM, Ford AR, Lukas SE. Compliance with nasal continuous positive airway pressure in psychiatric patients with obstructive sleep apnea. Sleep Res. 1994;23:192.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washinton, DC: American Psychiatric Press; 1994.
Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989;146:697–707.
Krakow B, Melendrez D, Pedersen B, Johnston L, Hollifield M, Germain A, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry. 2001;49:948–53.
Krakow B, Haynes PL, Warner TD, Santana E, Melendrez D, Johnston L, et al. Nightmares, insomnia, and sleep-disordered breathing in fire evacuees seeking treatment for posttraumatic sleep disturbance. J Trauma Stress. 2004;17:257–68.
• Yesavage JA, Kinoshita LM, Kimball T, Zeitzer J, Friedman L, Noda A, et al. Sleep-disordered breathing in Vietnam veterans with posttraumatic stress disorder. Am J Geriatr Psychiatry. 2012;20:199–204. This study found high prevalence of sleep breathing disorder in patients with PTSD..
Krakow B, Melendrez D, Warner TD, Clark JO, Sisley BN, Dorin R, et al. Signs and symptoms of sleep-disordered breathing in trauma survivors: a matched comparison with classic sleep apnea patients. J Nerv Ment Dis. 2006;194:433–9.
• Kinoshita LM, Yesavage JA, Noda A, Jo B, Hernandez B, Taylor J, et al. Modeling the effects of obstructive sleep apnea and hypertension in Vietnam veterans with PTSD. Sleep Breath. 2011. This study found that severity of OSA is correlated with poor cognitive function in PTSD patients.
Carrasco E, Santamaria J, Iranzo A, Pintor L, De Pablo J, Solanas A, et al. Changes in dreaming induced by CPAP in severe obstructive sleep apnea syndrome patients. J Sleep Res. 2006;15:430–6.
Guilleminault C, Kirisoglu C, Bao G, Arias V, Chan A, Li KK. Adult chronic sleepwalking and its treatment based on polysomnography. Brain. 2005;128(Pt 5):1062–9.
Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. 2008;12:169–84.
Krakow B, Lowry C, Germain A, Gaddy L, Hollifield M, Koss M, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for comorbid sleep-disordered breathing. J Psychosom Res. 2000;49:291–8.
El-Solh AA, Ayyar L, Akinnusi M, Relia S, Akinnusi O. Positive airway pressure adherence in veterans with posttraumatic stress disorder. Sleep. 2010;33:1495–500.
Sheehan DV, Ballenger J, Jacobsen G. Treatment of endogenous anxiety with phobic, hysterical, and hypochondriacal symptoms. Arch Gen Psychiatry. 1980;37:51–9.
Stein MB, Millar TW, Larsen DK, Kryger MH. Irregular breathing during sleep in patients with panic disorder. Am J Psychiatry. 1995;152:1168–73.
Hauri PJ, Friedman M, Ravaris CL. Sleep in patients with spontaneous panic attacks. Sleep. 1989;12:323–37.
Mellman TA, Uhde TW. Electroencephalographic sleep in panic disorder. A focus on sleep-related panic attacks. Arch Gen Psychiatry. 1989;46:178–84.
Lesser IM, Poland RE, Holcomb C, Rose DE. Electroencephalographic study of nighttime panic attacks. J Nerv Ment Dis. 1985;173:744–6.
Albert U, Maina G, Bergesio C, Bogetto F. Nocturnal panic and recent life events. Depress Anxiety. 2005;22:52–8.
Craske MG, Barlow DH. Nocturnal panic. J Nerv Ment Dis. 1989;177:160–7.
Mellman TA, Uhde TW. Sleep panic attacks: new clinical findings and theoretical implications. Am J Psychiatry. 1989;146:1204–7.
Biber B, Alkin T. Panic disorder subtypes: differential responses to CO2 challenge. Am J Psychiatry. 1999;156:739–44.
Sarisoy G, Boke O, Arik AC, Sahin AR. Panic disorder with nocturnal panic attacks: symptoms and comorbidities. Eur Psychiatry. 2008;23:195–200.
Lopes FL, Nardi AE, Nascimento I, Valenca AM, Mezzasalma MA, Freire RC, et al. Diurnal panic attacks with and without nocturnal panic attacks: are there some phenomenological differences? Rev Bras Psiquiatr. 2005;27:216–21.
Freire RC, Valenca AM, Nascimento I, Lopes FL, Mezzasalma MA, Zin WA, et al. Clinical features of respiratory and nocturnal panic disorder subtypes. Psychiatry Res. 2007;152:287–91.
Edlund MJ, McNamara ME, Millman RP. Sleep apnea and panic attacks. Compr Psychiatry. 1991;32:130–2.
Alvarenga ME, Richards JC, Lambert G, Esler MD. Psychophysiological mechanisms in panic disorder: a correlative analysis of noradrenaline spillover, neuronal noradrenaline reuptake, power spectral analysis of heart rate variability, and psychological variables. Psychosom Med. 2006;68:8–16.
Sullivan GM, Coplan JD, Kent JM, Gorman JM. The noradrenergic system in pathological anxiety: a focus on panic with relevance to generalized anxiety and phobias. Biol Psychiatry. 1999;46:1205–18.
Sukegawa M, Noda A, Sugiura T, Nakata S, Yoshizaki S, Soga T, et al. Assessment of continuous positive airway pressure treatment in obstructive sleep apnea syndrome using 24-hour urinary catecholamines. Clin Cardiol. 2005;28:519–22.
• Takaesu Y, Inoue Y, Komada Y, Kagimura T, Iimori M. Effects of nasal continuous positive airway pressure on panic disorder comorbid with obstructive sleep apnea syndrome. Sleep Med. 2012;13:156–60. This study found treatment with CPAP may reduce panic symtoms in patients with comorbid panic disorder and OSA.
Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biol Psychiatry. 2006;60:1364–71.
Fakier N, Wild LG. Associations among sleep problems, learning difficulties and substance use in adolescence. J Adolesc. 2011;34:717–26.
James JE, Kristjansson AL, Sigfusdottir ID. Adolescent substance use, sleep, and academic achievement: evidence of harm due to caffeine. J Adolesc. 2011;34:665–73.
Obermeyer WH, Benca RM. Effects of drugs on sleep. Neurol Clin. 1996;14:827–40.
Mahfoud Y, Talih F, Streem D, Budur K. Sleep disorders in substance abusers: how common are they? Psychiatry (Edgmont). 2009;6:38–42.
Brower KJ, Hall JM. Effects of age and alcoholism on sleep: a controlled study. J Stud Alcohol. 2001;62:335–43.
Weissman MM, Greenwald S, Nino-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. Gen Hosp Psychiatry. 1997;19:245–50.
Drummond SP, Gillin JC, Smith TL, DeModena A. The sleep of abstinent pure primary alcoholic patients: natural course and relationship to relapse. Alcohol Clin Exp Res. 1998;22:1796–802.
Le Bon O, Verbanck P, Hoffmann G, Murphy JR, Staner L, De Groote D, et al. Sleep in detoxified alcoholics: impairment of most standard sleep parameters and increased risk for sleep apnea, but not for myoclonias–a controlled study. J Stud Alcohol. 1997;58:30–6.
Vitiello MV, Prinz PN, Personius JP, Vitaliano PP, Nuccio MA, Koerker R. Relationship of alcohol abuse history to nighttime hypoxemia in abstaining chronic alcoholic men. J Stud Alcohol. 1990;51:29–33.
Issa FG, Sullivan CE. Alcohol, snoring and sleep apnea. J Neurol Neurosurg Psychiatry. 1982;45:353–9.
• Vakulin A, Baulk SD, Catcheside PG, Antic NA, van den Heuvel CJ, Dorrian J, et al. Effects of alcohol and sleep restriction on simulated driving performance in untreated patients with obstructive sleep apnea. Ann Intern Med. 2009;151:447–55. This study found that patients with OSA have poorer driving performance than normal people under effects of alcohol and sleep restriction.
Effective medical treatment of opiate addiction. National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. JAMA. 1998;280(22):1936–43.
Teichtahl H, Wang D, Cunnington D, Quinnell T, Tran H, Kronborg I, et al. Ventilatory responses to hypoxia and hypercapnia in stable methadone maintenance treatment patients. Chest. 2005;128:1339–47.
Methadone-associated overdose deaths: factors contributing to increased deaths and efforts to prevent them. GAO-09-34126 Available at: http://wwwgaogov/products/GAO-09-341. Acessed June 30, 2012.
Wang D, Teichtahl H, Drummer O, Goodman C, Cherry G, Cunnington D, et al. Central sleep apnea in stable methadone maintenance treatment patients. Chest. 2005;128:1348–56.
Sharkey KM, Kurth ME, Anderson BJ, Corso RP, Millman RP, Stein MD. Obstructive sleep apnea is more common than central sleep apnea in methadone maintenance patients with subjective sleep complaints. Drug Alcohol Depend. 2010;108:77–83.
Wang D, Teichtahl H. Opioids, sleep architecture and sleep–disordered breathing. Sleep Med Rev. 2007;11:35–46.
Peles E, Schreiber S, Adelson M. Variables associated with perceived sleep disorders in methadone maintenance treatment (MMT) patients. Drug Alcohol Depend. 2006;82:103–10.
Wang D, Teichtahl H, Goodman C, Drummer O, Grunstein RR, Kronborg I. Subjective daytime sleepiness and daytime function in patients on stable methadone maintenance treatment: possible mechanisms. J Clin Sleep Med. 2008;4:557–62.
McCann UD, Sgambati FP, Schwartz AR, Ricaurte GA. Sleep apnea in young abstinent recreational MDMA ("ecstasy") consumers. Neurology. 2009;73:2011–7.
Chamberlin NL, Saper CB. The agony of the ecstasy: serotonin and obstructive sleep apnea. Neurology. 2009;73:1947–8.
Disclosure
W.-C. Lin: none; J. W. Winkelman: has served as a board member of Zeo; has served as a consultant to Pfizer, UCB, Zeo, and Sunovion; has provided expert testimony for AVH; has received research support from National Institute of Mental Health, GlaxoSmithKline, and Impax Pharmaceuticals; and has received stock/stock options from Zeo.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, WC., Winkelman, J.W. Obstructive Sleep Apnea and Severe Mental Illness: Evolution and Consequences. Curr Psychiatry Rep 14, 503–510 (2012). https://doi.org/10.1007/s11920-012-0307-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-012-0307-6
Keywords
- Sleep disorders
- Sleep apnea
- Obstructive sleep apnea
- OSA
- Daytime sleepiness
- Psychiatric comorbidities
- Depression
- Bipolar disorder
- Schizophrenia
- Post-traumatic stress disorder
- PTSD
- Panic disorder
- Substance use disorder
- Antidepressants
- Selective serotonin reuptake inhibitor
- SSRI
- Antipsychotics
- Continuous positive airway pressure
- CPAP
- Psychiatry
- Diagnosis
- Treatment
- Treatment compliance