Abstract
Guanosine, the endogenous guanine nucleoside, prevents cellular death induced by ischemic events and is a promising neuroprotective agent. During an ischemic event, nitric oxide has been reported to either cause or prevent cell death. Our aim was to evaluate the neuroprotective effects of guanosine against oxidative damage in hippocampal slices subjected to an in vitro ischemia model, the oxygen/glucose deprivation (OGD) protocol. We also assessed the participation of nitric oxide synthase (NOS) enzymes activity on the neuroprotection promoted by guanosine. Here, we showed that guanosine prevented the increase in ROS, nitric oxide, and peroxynitrite production induced by OGD. Moreover, guanosine prevented the loss of mitochondrial membrane potential in hippocampal slices subjected to OGD. Guanosine did not present an antioxidant effect per se. The protective effects of guanosine were mimicked by inhibition of neuronal NOS, but not of inducible NOS. The neuroprotective effect of guanosine may involve activation of cellular mechanisms that prevent the increase in nitric oxide production, possibly via neuronal NOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke as a result from cerebral ischemia (an obstruction of blood flow causing an impairment of providing metabolic substrates) can cause severe degeneration of central nervous system (CNS) cells and consequent loss of brain functions [1]. Stroke is the third leading cause of death and a major cause of long-lasting disability worldwide [2].
During cerebral ischemia, the excitatory amino acid glutamate is released at high concentrations within the core of the infarction area and in the penumbra tissue. In these areas, glutamate promotes overactivation of its receptors, mainly the N-methyl-D-aspartate (NMDA) subtype, leading to ionic unbalance, mitochondrial Ca2+ overload, inhibition of ATP production, and breakdown of biomolecules [3]. Increased intracellular Ca2+ levels further promotes glutamate release and this event amplifies the spread of neuronal excitotoxicity [4].
The degree of cell injury in ischemic events depends on the time and intensity of blood flow obstruction. In this regard, the most effective therapies are reperfusion strategies used to reestablish tissue perfusion, in order to reduce neurological deficits and improve functional outcome [5]. However, reperfusion of ischemic brain tissue can also have harmful consequences, as it is characterized by the significant increase in reactive oxygen species (ROS) and nitrogen reactive species (RNS) levels, including nitric oxide (NO) [4, 6, 7].
NO is a physiological messenger in the CNS and is synthesized by the nitric oxide synthases (NOS) from L-arginine, forming L-citrulline and NO [8]. All brain cells are able to synthesize NO, from different isoforms of NOS, following different types of stimulus. In neurons, NO is synthesized primarily by the neuronal isoform of NOS (nNOS or NOS1), a Ca2+-dependent and constitutively expressed enzyme. In glial cells, NO is synthesized by a Ca2+-independent inducible NOS (iNOS or NOS2), which is upregulated after the increase in proinflammatory cytokines. In contrast, endothelial cells produce NO by a constitutive pathway via Ca2+-dependent activity of endothelial NOS (eNOS or NOS3) [4, 9].
Nitric oxide (NO) can exert both protective and deleterious effects, depending on its cellular source, NOS isoform, and the temporal injury stage. Immediately after brain ischemia, NO released from eNOS is protective by promoting vasodilation and inhibiting microvascular aggregation and adhesion. However, the hyperactivation of NMDA receptors in postsynaptic neurons produces excessive nNOS activity and subsequently inflammatory reactions inducing iNOS expression at glial cells, allowing massive and uncontrolled NO release that may be damaging for the neighboring neurons [8]. Furthermore, the negative effects of excessive NO generation are caused by the endogenous formation of the peroxynitrite anion (ONOO−) rather than NO itself [10]. ONOO− is formed by the spontaneous reaction of NO with superoxide anion (O2 −) [9].
An endogenous neuroprotective agent that had been considered as a putative anti-ischemic strategy is guanosine (GUO), the guanine-derived nucleoside. GUO presents neuroprotective effect in in vivo and in vitro experimental models of brain diseases associated with glutamatergic excitotoxicity [11, 12]. It was showed that after focal stroke in rats, GUO levels are elevated within 2 h and remain high for 7 days in the brain tissue [13]. In oxygen/glucose deprivation (OGD) protocol, an in vitro model for ischemia, we showed that GUO is protective by improving extracellular glutamate uptake [14]. Moreover, GUO is effective in reducing ROS production, iNOS expression and NF-kB activation, and preventing the loss of mitochondrial membrane potential. Additionally, it decreased cells membrane permeability and glutamate release, and recovered glutamine synthetase activity in slices subjected to OGD [12, 15].
In the present study, we examine further the mechanisms involved in the neuroprotective effect of GUO in response to OGD/reperfusion damage. Selective inhibition of different NOS isoforms was used to investigate the participation of these enzymes on GUO neuroprotective and antioxidant effects. We also evaluated a putative antioxidant activity of GUO per se.
Materials and methods
Animals
Male adult Wistar rats (60–90 days post-natal) were obtained from our local breeding colony and maintained on a 12 h light–12 h dark schedule at 23 ± 1 °C, with food and water ad libitum. The procedures used in the present study complied with the guidelines on animal care of the UFSC Ethics Committee on the Use of Animals (CEUA), which follows the “Principles of laboratory animal care” from NIH (2011).
Preparation and incubation of hippocampal slices
Rats were killed by decapitation, and hippocampi were rapidly removed and placed in an ice-cold Krebs-Ringer bicarbonate buffer (KRB) of the following composition (in mM): 120 NaCl, 2 KCl, 10 MgSO4, 0.5 CaCl2, 1.18 KH2PO4, 26 NaHCO3, and 10 D-glucose. The buffer was bubbled with 95 % O2–5 % CO2 up to pH 7.4. Slices (400 μm) were prepared using a Mcllwain Tissue Chopper, separated in KRB at 4 ° C and allowed to recover for 30 min in KRB at 37 ° C [16].
Slices corresponding to the control group were incubated throughout the experiment in KRB. Oxygen and glucose deprivation (OGD) was induced by incubating slices for a 15-min period in an OGD buffer with the following composition (in mM): 1.3 CaCl2, 137 NaCl, 5 KCl, 0.65 MgSO4, 1.1 KH2PO4, and 5 HEPES, where 10 mM D-glucose was replaced by 10 mM 2-deoxy-glucose [17], and the buffer was bubbled with nitrogen throughout the incubation period [18]. After the OGD period, slices returned to an oxygenated regular KRB containing glucose for 2 h (reoxygenation period, that mimics the reperfusion after ischemia). These experiments were performed at 37 °C.
Slices treatment
When present, GUO (100 μM, Sigma-Aldrich®), N-3-Aminomethyl-benzyl-acetamidine (1400 W) (100 μM, Sigma-Aldrich®, iNOS inhibitor), 7-nitroindazole (7-NI) (50 μM, Sigma-Aldrich®, nNOS inhibitor), or L-N G-nitro-L-arginine methyl ester (L-NAME) (1 mM, Sigma-Aldrich®, non-selective NOS inhibitor) were added in the reoxygenation period. When the treatment was realized with GUO plus NOS inhibitors, the NOS inhibitors were pre-incubated for 15 min before adding GUO and they were kept together during the 2 h of reoxygenation. As a positive control for ROS production, we used hydrogen peroxide (H2O2, Vetec®). Hippocampal slices were incubated for 2 h with H2O2, at a concentration of 1 mM [19].
Evaluation of cell viability
Cell viability was determined through the ability of cells to reduce 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) (Sigma-Aldrich®) as previously described [20]. After the reoxygenation period, hippocampal slices were incubated with MTT (0.5 mg/mL) in KRB for 20 min at 37 °C. The tetrazolium ring of MTT can be cleaved by active dehydrogenases to produce a precipitated formazan. The precipitated formazan was solubilized with 200 μL of dimethyl sulfoxide (DMSO), and the optical density quantified spectrophotometrically at a wavelength of 550 nm was considered as a parameter of cellular viability.
Propidium iodide staining
Cell damage was assessed by using the uptake of the fluorescent exclusion dye propidium iodide (PI) (Sigma-Aldrich®), which is a polar compound that enters only dead or dying cells with damaged membranes. Once inside the cells, PI complexes with DNA and emits an intense red fluorescent [21]. After the reoxygenation period, hippocampal slices were incubated with 7 μg/mL of PI for 30 min at 37 °C. PI fluorescence was measured in a fluorescence microplate reader. Peak excitation and emission wavelengths for IP occur at 535 and 617 nm, respectively [22].
Measurement of reactive oxygen and nitrogen species
To measure cellular reactive oxygen and nitrogen species production, the molecular probe 2′,7′-dichlorofluorescein diacetate (DCFH-DA) (Sigma-Aldrich®) was used. After the reoxygenation period, hippocampal slices were loaded with 80 μM of DCFH-DA for 30 min at 37 °C. DCFH-DA is deacetylated by intracellular esterases to form non-fluorescent form 2′,7′-dichlorodihydrofluorescein (DCFH), which is rapidly oxidized by reactive oxygen and/or nitrogen species present in samples, producing the highly fluorescent compound desterified 2′,7′-dichlorofluorescein (DCF). Peak excitation and emission wavelengths for DCF occur at 480 and 525 nm, respectively [23].
Measurement of nitric oxide production
NO production in hippocampal slices was estimated from the increase in the fluorescence intensity of the NO-sensitive dye 4,5-diaminofluorescein diacetate (DAF-2 DA) (Sigma-Aldrich®). Hippocampal slices were loaded with 10 μM of DAF-2 DA for 60 min at 37 °C, during the reoxygenation period. DAF-2 DA is taken up by cells where it is esterified by intracellular esterases to form the relatively non-fluorescent compound 4,5-diaminofluorescein (DAF-2). In the presence of O2, NO combines with DAF-2 to form the highly fluorescent triazolofluorescein (DAF-2T). Peak excitation and emission wavelengths for DAF-2T occur at 485 and 515 nm, respectively [24]. As a positive control for this assay, we used S-nitroso-N-acetyl-DL-penicillamine (SNAP, Sigma-Aldrich®), a nitric oxide donor. Hippocampal slices were incubated for 2 h with SNAP, at a concentration of 1 mM [25].
Measurement of peroxynitrite production
Dihydrorhodamine-123 (DHR-123) (Sigma-Aldrich®) oxidation was used to evaluate peroxynitrite (ONOO−) production in the hippocampal slices. Non-fluorescent DHR 123 is oxidized to rhodamine 123, a fluorescent lipophilic cationic dye in the presence of ONOO−. After the reoxygenation period, hippocampal slices were loaded with 15 μM of DHR 123 for 30 min at 37 °C. Peak excitation and emission wavelengths for rhodamine 123 occur at 485 and 525 nm, respectively [26].
Evaluation of in vitro scavenger activity by guanosine
Measurement of a putative GUO scavenger activity against the 2,2-diphenyl-1-picrylhydrazyl (DPPH) (Sigma-Aldrich®) radical was performed in accordance with the procedure described previously [27]. DPPH solution (500 μM) was added to a medium containing different concentrations of the GUO (10, 100, 500, or 1000 μM) and incubated at room temperature for 30 min. The decrease in the absorbance measured at 518 nm depicted the scavenger activity of drugs against DPPH radical [28]. Ascorbic acid (10 μM) was used as a positive control of scavenger activity.
Nitric oxide scavenging activity by GUO was determined using the Griess reagent (Sigma-Aldrich®) [29]. Sodium nitroprusside (SNP, 5 mM) (Sigma-Aldrich®) was incubated at 25 °C with different concentrations of GUO (10, 100, 500, or 1000 μM). After 2 h, 500 μL of incubation solution was mixed with 500 μL of the Griess reagent. The absorbance was measured at 550 nm [28]. The values were compared with the control to determine the percentage of inhibition of the nitrite (NO2 −) reaction with the Griess reagent, which gave an index for the NO scavenger activity.
Measurement of mitochondrial membrane potential
After the reoxygenation period, hippocampal slices were loaded with the mitochondrial selective dye fluorescent tetramethylrhodamine ethyl ester (TMRE, 100 nM) (Sigma-Aldrich®) for 30 min at 37 ° C. TMRE is a cationic lipophilic dye that accumulates in the negatively charged mitochondrial matrix according to the Nernst equation potential [30]. Peak excitation and emission wavelengths for TMRE occur at 550 and 590 nm, respectively [31].
To interpret the results obtained with the TMRE probe, we use the protonophore carbonyl cyanide 4-(trifluoromethoxy) phenylhydrazone (FCCP, Sigma-Aldrich®) at a concentration of 10 μM. FCCP has the capacity to depolarize the mitochondria [32].
Statistical analysis
For statistical analysis, we used the software GraphPad Prism 5.0®. Results are expressed as means + standard deviation (SD) of percentages related to control groups. Statistical significance was determined using one-way ANOVA followed by Tukey’s post hoc test for comparisons among multiple groups. Statistical differences were accepted at P < 0.05. For the linear correlation analysis, we used the software GraphPad Prism 5.0®.
Results
Guanosine prevents increased NO and ONOO− production in rat hippocampal slices subjected to OGD
We previously showed that in hippocampal slices subjected to OGD occurs an excessive ROS production, which is prevented by GUO [33]. We found that hippocampal slices subjected to OGD also presented an increase in NO production, as measured by an increase in the fluorescence emission from DAF-2-DA (Fig. 1a). SNAP (1 mM) used as a positive control for this assay also showed increased fluorescence intensity (224 ± 16 % related to the control; not shown).
Effects of guanosine on NO (a) and ONOO− (b) production in hippocampal slices subjected to OGD/reoxygenation and evaluation of antioxidant properties of guanosine on DPPH radical reduction (c) and NO radicals scavenging (d). Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h. Guanosine (GUO, 100 μM) was added during the reoxygenation period and NO (a) and ONOO− (b) production were measured by incubation with fluorescent probes, as described in the “Materials and methods” section. A concentration curve of GUO (10 μM to 1 mM) was used to assess the putative antioxidants properties of guanosine. Results are expressed as percentage of increase of relative fluorescence units (RFU) (a and b), absorbance of DPPH radical (c), and as percentage of inhibition of NO radicals (d) in relation to the control values, which were 24.56 ± 0.3 μM to nitrite absorbance (d). Data correspond to means + SD of five experiments performed in triplicates. * P < 0.05 as compared to the control group. # P < 0.05 as compared to the OGD-control group (ANOVA followed by Tukey’s test)
As GUO is capable to prevent the increased ROS and NO production in hippocampal slices subjected to OGD, we analyzed the RNS production measured by ONOO− levels in rat hippocampal slices subjected to OGD. A significant increase in ONOO− levels was observed in hippocampal slices subjected to OGD and GUO was capable to prevent the enhanced ONOO− levels (Fig. 1b). We are here firstly showing that GUO decreased the generation of NO and ROS (mainly O2 − and H2O2) and the consequent production of ONOO− in hippocampal slices subjected to OGD.
Evaluation of putative antioxidant properties of guanosine
Considering that GUO prevented the increase in ROS, NO, and ONOO− levels caused by OGD, we analyzed whether GUO presents antioxidant properties per se. As expected, incubation of DPPH radical with ascorbic acid (used as a positive control) resulted in a marked decrease in the absorbance values emitted by DPPH, confirming the antioxidant properties of ascorbic acid. However, when incubated with GUO, no reduction in DPPH absorbance was observed, indicating that GUO does not present antioxidant properties per se (Fig. 1c). We then evaluated whether guanosine presents NO scavenging activity. Evaluation of inhibition of NO radicals formation showed that guanosine has a small, but significant NO scavenging activity (less than 10 % at the concentration used to afford neuroprotection, 100 μM) (Fig. 1d).
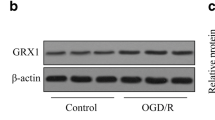
Effects of NOS isoforms inhibition on cellular viability and cell membrane permeability of hippocampal slices
GUO treatment prevented iNOS expression in hippocampal slices subjected to OGD and to an in vitro glutamate challenge [33, 34]. Here, we used NOS activity inhibitors to understand the involvement of the NOS isoforms in the mechanism of OGD-induced cell damage and in the neuroprotective effect of GUO. The non-selective NOS inhibitor L-NAME (1 mM), the selective iNOS inhibitor 1400 W (50 μM), and the selective nNOS inhibitor 7-NI (100 μM) were used [10, 35].
GUO prevented cell viability decrease in hippocampal slices subjected to OGD, similarly to L-NAME (Fig. 2a). However, simultaneous incubation of L-NAME + GUO inhibited the recovery in cellular viability induced by GUO or L-NAME alone (Fig. 2a). Incubation of 1400 W or 7-NI did not recover cellular viability in hippocampal slices subjected to OGD, but simultaneous incubation with 1400 W + 7-NI was protective (Fig. 2d). iNOS or nNOS inhibitors did not interfere on GUO effect of recovering cellular viability (Fig. 2b–d).
Evaluation of effects of NOS enzymes inhibition on cell viability of hippocampal slices subjected to OGD/reoxygenation. Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h (OGD). Guanosine (GUO, 100 μM) was added during the reoxygenation period in the presence or not of L-NAME (1 mM, a), 1400 W (50 μM, b), 7-NI (100 μM, c), or 1400 W + 7-NI (d). Data are expressed as percentage of the control group and correspond to the means + SD of five experiments performed in triplicates. * P < 0.05 as compared to the control group; # P < 0.05 as compared to the OGD-control group (ANOVA followed by Tukey’s test)
PI staining in hippocampal slices subjected to OGD was used to assess an increase in cell membrane permeability. Hippocampal slices subjected to OGD presented an increased PI incorporation. Incubation with GUO, L-NAME (Fig. 3a), 1400 W (Fig. 3b), 7-NI (Fig. 3c), or 1400 W + 7-NI (Fig. 3d) prevented PI staining. Co-incubation of NOS inhibitors and GUO did not significantly modify GUO effect in preventing cell damage (Fig. 3).
Evaluation of effects of NOS enzymes inhibition on cellular membrane damage measured by PI incorporation. Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h (OGD). Guanosine (GUO, 100 μM) was added during the reoxygenation period in the presence or not of L-NAME (1 mM, a), 1400 W (50 μM, b), 7-NI (100 μM, c), or 1400 W + 7-NI (d). Data are expressed as percentage of the control group and correspond to the means + SD of five experiments performed in triplicates. * P < 0.05 as compared to the control group; # P < 0.05 represents different mean compared to the OGD-control group (ANOVA followed by Tukey’s test)
Effects of NOS isoforms on ROS production in hippocampal slices
Incubation with L-NAME prevented ROS production in hippocampal slices subjected to OGD (Fig. 4a). However, incubation with 1400 W or 7-NI was not able to prevent the increase of ROS production in hippocampal slices submitted to OGD (Fig. 4b, c). Interestingly, the simultaneous incubation of 1400 W + 7-NI prevented the increase in ROS production caused by OGD (Fig. 4d). We observed that incubation of L-NAME + GUO, 1400 W + GUO, or 7-NI + GUO did not interfere with the GUO effect of preventing the increase in ROS production induced by OGD (Fig. 4a–c). These results demonstrated that total NOS inhibition prevented ROS production as well as GUO treatment alone, but simultaneous inhibition of different NOS isoforms plus GUO did not presented any additional effect in the prevention of ROS levels increase caused by OGD.
Evaluation of effects of NOS enzymes inhibition on DCF fluorescence in hippocampal slices subjected to OGD/reperfusion. Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h (OGD). Guanosine (GUO, 100 μM) was added during the reoxygenation period in the presence or not of L-NAME (1 mM, a), 1400 W (50 μM, b), 7-NI (100 μM, c), or 1400 W + 7-NI (d). Data are expressed as percentage of increase of relative fluorescence units (RFU) related to the control group and correspond to the means + SD of six experiments performed in triplicates. * P < 0.05 as compared to the control group; # P < 0.05 as compared to the OGD-control group (ANOVA followed by Tukey’s test)
Effect of NOS isoforms inhibition on NO production in hippocampal slices
Hippocampal slices subjected to OGD and incubated with L-NAME presented a decrease in NO production (Fig. 5a). However, incubation of hippocampal slices with 1400 W was unable to prevent the increase in NO, whereas incubation with 7-NI was capable to attenuate the increase in NO synthesis in hippocampal slices subjected to OGD (Fig. 5b, c). These results suggest that the nNOS isoform is more effective than the iNOS isoform in preventing oxidative damage in hippocampal slices subject to in vitro ischemia. Yet, co-incubation of 1400 W + 7-NI prevented NO production in hippocampal slices subjected to OGD (Fig. 5d). Co-incubation of GUO and the inhibitors of NOS enzymes did not potentiated the GUO effect alone in reducing NO production.
Evaluation of effects of NOS enzymes inhibition on NO production in hippocampal slices subjected to OGD/reoxygenation. Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h (OGD). Guanosine (GUO, 100 μM) was added during the reoxygenation period in the presence or not of L-NAME (1 mM, a), 1400 W (50 μM, b), 7-NI (100 μM, c), or 1400 W + 7-NI (d). Data are expressed as percentage of increase of relative fluorescence units (RFU) related to the control group and correspond to the means + SD of five experiments performed in triplicates. * P < 0.05 as compared to the control group; # P < 0.05 as compared to the OGD-control group (ANOVA followed by Tukey’s test)
Effects of NOS isoforms inhibition on ONOO− production in hippocampal slices
Measurement of ONOO− levels in rat hippocampal slices subjected to OGD were also evaluated in the presence of NOS inhibitors. Similarly to the observed in NO levels measurement, hippocampal slices subjected to OGD and incubated with GUO or L-NAME presented a decrease in ONOO− production (Fig. 6a). Incubation of hippocampal slices with 1400 W was unable to prevent the increase in ONOO−, whereas incubation with 7-NI attenuated the increase in ONOO− production in hippocampal slices subjected to OGD (Fig. 6b, c). Co-incubation of 1400 W + 7-NI prevented ONOO− production. Again, the neuroprotective effect of GUO in preventing the increase in ONOO− production is maintained when co-incubated with 1400 W or 7-NI (Fig. 6). Considering ONOO− production showed similar results as observed to NO production, we evaluated if ONOO− synthesis has a positive correlation with NO synthesis. A linear correlation analysis revealed a correlation of R 2 = 0.9309 (data not shown). This data indicates that ONOO− synthesis correlates directly with the NO synthesis.
Evaluation of effects of NOS enzymes inhibition on ONOO− production in hippocampal slices subjected to OGD/reoxygenation. Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h (OGD). Guanosine (GUO, 100 μM) was added during the reoxygenation period in the presence or not of L-NAME (1 mM, a), 1400 W (50 μM, b), 7-NI (100 μM, c), or 1400 W + 7-NI (d). Data are expressed as percentage of increase of relative fluorescence units (RFU) related to the control group and correspond to the means + SD of five experiments performed in triplicates. * P < 0.05 as compared to the control group; # P < 0.05 as compared to the OGD-control group (ANOVA followed by Tukey’s test)
Effects of NOS isoforms inhibition on mitochondrial membrane potential in hippocampal slices
We also previously showed that hippocampal slices subjected to OGD presented a loss in mitochondrial membrane potential (ΔΨmit) [33]. Hippocampal slices incubated with the protonophore FCCP (10 μM for 2 h) showed a decrease in the fluorescence emission from TMRE (37 ± 8 %) indicating a depolarization of the mitochondrial membrane, similar from observed to slices subjected to OGD. GUO was able to prevent the loss of the mitochondrial membrane potential in hippocampal slices subjected to OGD (Fig. 7).
Evaluation of effects of NOS enzymes inhibition on the mitochondrial membrane potential (ΔΨmit) in hippocampal slices subjected to OGD/reoxygenation. Slices were incubated for 15 min in ischemic buffer and reoxygenated for 2 h (OGD). Guanosine (GUO, 100 μM) was added during the reoxygenation period in the presence or not of L-NAME (1 mM, a), 1400 W (50 μM, b), 7-NI (100 μM, c), or 1400 W + 7-NI (50 μM; 100 μM, respectively, d). Data are expressed as percentage of increase of relative fluorescence units (RFU) related to the control group and correspond to the means + SD of five experiments performed in triplicates. * P < 0.05 as compared to the control group; # P < 0.05 as compared to the OGD-control group (ANOVA followed by Tukey’s test)
Incubation of hippocampal slices with the non-selective NOS inhibitor, L-NAME, prevented the mitochondrial membrane depolarization (Fig. 7a). The selective iNOS (1400 W) or nNOS (7-NI) inhibitors per se did not recover the mitochondrial membrane potential (Fig. 7b, c), although co-incubation with 1400 W + 7-NI showed a recovery of the mitochondrial membrane potential (Fig. 7d). Again, the presence of NOS inhibitors did not interfere with the GUO effect of preventing the loss of mitochondrial membrane potential in hippocampal slices subjected to OGD (Fig. 7).
Discussion
Purine nucleosides have been identified as neuroprotective agents [36]. Here, we confirm and extend the knowledge related to the mechanisms involved in the neuroprotective effects of guanosine (GUO) in neurotoxicity and neurodegenerative rodent models [5, 12, 33, 37–39]. In previous studies from our group, the neuroprotective effect of GUO was shown in hippocampal slices subjected to the OGD/reoxygenation protocol. GUO prevents the decrease in cell viability, by increasing glutamate uptake and glutamine synthetase activity, decreasing glutamate release, ROS production and inflammatory mediators expression, including reduction of iNOS expression [14, 15, 33, 40]. The exact interaction site of GUO in cellular membranes is still unknown, although it has been suggested [41, 42]. GUO effects over adenosinergic system are controversial [43], but we have shown that neuroprotective effects of GUO depend on adenosine receptors modulation [33] and on activation of a calcium-dependent potassium channel [14]. It has also recently been shown that GUO may regulate the extracellular disposition of adenosine in some cell types by an unknown mechanism, but this effect seems not to occur in neuronal cells [44]. Therefore, this putative guanosine-adenosine interaction in the brain must be further characterized.
In the present study, we showed that GUO provides neuroprotection to hippocampal slices subjected to OGD also by reducing cell membrane permeability; attenuating the increase in ROS, NO, and ONOO− production; and preventing the loss of mitochondrial membrane potential. These protective effects were also observed by inhibiting NOS isoforms activity, indicating the neuroprotective effect of guanosine also involves modulation of NOS activity.
The high rate of oxidative metabolism during cerebral ischemia leads to an overproduction of free radicals. This process triggers many cellular events that result in damage to macromolecules and subsequent activation of signaling pathways leading to cell death [6]. Therefore, we investigated whether GUO has antioxidant activity per se, since our and other laboratories have shown that neuroprotection promoted by GUO is related to the modulation of oxidative stress caused by ischemic damage [45, 46]. However, our results showed that this nucleoside cannot reduce the DPPH radical. On the other hand, for the first time, we are showing that guanosine presents a small capacity to scavenge NO molecules besides preventing the increase in NO production. In the concentration used to afford neuroprotection (100 μM), GUO has an effect of 8 % of NO scavenger, which may not be the main mechanism of its neuroprotective effect, although it might contribute to it.
NO is one of the ubiquitous biological mediators in mammalian cells. In low concentrations, this radical induces physiological effects such as vascular relaxation, inhibition of platelet aggregation, and cell proliferation [8]. In the brain, NO has also been associated with synaptic plasticity; however, a full understanding of its role in the CNS is not yet elucidated [47]. However, the increase in NO level leads to pathophysiological effects to cell, such as DNA damage, protein nitration, and ONOO− production [48, 49]. By evaluating the role of NOS enzymes, we found that non-selective inhibition of NOS isoforms with L-NAME provides cellular protection to the hippocampal slices subjected to OGD. However, the selective inhibition of iNOS or nNOS did not provide cellular protection.
Previous studies have shown that the activation of the endothelial NOS (eNOS) isoform has protective effects [50, 51]. In agreement, the use of a selective inhibitor for the eNOS isoform resulted in an increased infarct size, suggesting that inhibition of this isoform caused changes in hemodynamic and platelet functions, which culminated in cell damage [7, 49]. On the other hand, activation of iNOS and nNOS isoforms correlates with pathophysiological effects. In a middle cerebral artery occlusion model, a minor ischemic area in nNOS knockout mice was observed [52]. However, another study showed that an increased number of nNOS immunoreactive neurons is associated with a mild damage and functional recovery after the ischemic event [53]. Thus, we decided to inhibit the iNOS and nNOS isoforms activity and observed that simultaneous inhibition of these enzymes prevented cell damage to hippocampal slices, confirming that these isoforms contribute to the pathophysiological events that occur during an ischemic episode.
The cellular signaling pathways that lead to increase of free radical synthesis include hyperactivation of NOS enzymes and increase in NO production [19]. Here, we found that simultaneous inhibition of iNOS and nNOS isoforms prevented the increase in ROS, NO, ONOO−, and loss of mitochondrial membrane potential. These effects were also observed when hippocampal slices were incubated with L-NAME or GUO. These results indicate that iNOS and nNOS isoforms activation could lead to an increase in ROS synthesis, and suggest that GUO may act through pathways that modulate the activity of these enzymes.
Regarding NO and ONOO− production, a prevention was observed only when the nNOS isoform is inhibited, either by its selective inhibitor 7-NI or by the non-selective inhibitor L-NAME. The use of a selective inhibitor for the iNOS isoform, 1400 W, did not decrease NO and ONOO− levels, although we previously showed GUO was able to decrease the expression of the iNOS isoform induced by OGD [33]. The future evaluation of the expression of the nNOS isoform in ischemic situations and protection by GUO can help to understand the protective mechanisms promoted by GUO. Taken together, these results suggest that not only the iNOS isoform is activated in an ischemic event, but also the nNOS isoform. Additionally, these results suggest that inhibition of NO and ONOO− synthesis may be a cell neuroprotective pathway also induced by GUO.
NO and ONOO− can easily diffuse through cell membranes due to their high solubility and therefore can reach targets far from their production site [4, 9]. ONOO− is implicated in damage to several cellular components, including the irreversible inhibition of mitochondrial electron transfer chain, blocking ATP synthesis, inducing nitration and/or oxidation of lipids, DNA, and mitochondrial and cellular proteins [1, 7]. In this sense, evidence suggests that disruption of mitochondrial bioenergetics and dynamics have a critical role in the pathogenesis of neurological diseases and stroke [54]. Mitochondrial injury affects the maintenance of mitochondrial membrane potential [4]. Indeed, we observed a loss of mitochondrial membrane potential in hippocampal slices subjected to OGD. Interestingly, treatment with GUO, L-NAME, or 1400 W plus 7-NI was able to reverse the loss of mitochondrial membrane potential, pointing to a role of NOS isoforms in the maintenance of mitochondrial dynamics.
Our results show that iNOS and nNOS isoforms contribute significantly to the ROS, NO, and ONOO− production. By inhibiting these enzymes with 1400 W or 7-NI, respectively, or with L-NAME, we observed a significant cellular protection and a decrease in ROS, NO, and ONOO− synthesis and prevention of mitochondrial membrane potential loss, a protective mechanism that is shared by GUO. Particularly, we suggest that NO and ONOO− production are more responsive to nNOS inhibition than eNOS or iNOS in this in vitro ischemia model in hippocampal slices.
Guanosine plays a significant role in the defense mechanisms against cerebral ischemia by inducing key cellular functions in this injury situation, as K+ channels activation [14], glutamate uptake increase, reduction of inflammatory mediators expression [15, 33], and, as firstly shown in this study, reduction of NO and ONOO− production similarly to NOS inhibitors. Although the exact mechanism exerted by GUO on the NO production system is still not completely understood, we reinforce the hypothesis that GUO could be used to devise new strategies for stroke treatment.
Abbreviations
- 1400 W:
-
N-(3-(Aminomethyl)benzyl)acetamidine
- 7-NI:
-
7-nitroindazole
- eNOS:
-
Endothelial nitric oxide synthase
- GUO:
-
Guanosine
- HBSS:
-
Hank’s balanced salt solution
- iNOS:
-
Inducible nitric oxide synthase
- KRB:
-
Krebs-Ringer bicarbonate buffer
- L-NAME:
-
L-N G-nitro-L-arginine methyl ester
- MTT:
-
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- nNOS:
-
Neuronal nitric oxide synthase
- OGD:
-
Oxygen/glucose deprivation
- ONOO− :
-
Peroxynitrite
- ROS:
-
reactive oxygen species
References
Brouns R, De Deyn PP (2009) The complexity of neurobiological processes in acute ischemic stroke. Clin Neurol Neurosurg 111(6):483–95
Donnan GA et al (2008) Stroke. Lancet 371(9624):1612–23
Carden DL, Granger DN (2000) Pathophysiology of ischaemia-reperfusion injury. J Pathol 190(3):255–66
Bolanos JP et al (2009) Mitochondria and reactive oxygen and nitrogen species in neurological disorders and stroke: therapeutic implications. Adv Drug Deliv Rev 61(14):1299–315
Connell BJ et al (2013) Guanosine protects against reperfusion injury in rat brains after ischemic stroke. J Neurosci Res 91(2):262–72
Nanetti L et al (2011) Oxidative stress in ischaemic stroke. Eur J Clin Investig 41(12):1318–22
Moro MA et al (2004) Role of nitric oxide after brain ischaemia. Cell Calcium 36(3–4):265–75
Brown GC (2010) Nitric oxide and neuronal death. Nitric Oxide 23(3):153–65
Bolanos JP, Heales SJ (2010) Persistent mitochondrial damage by nitric oxide and its derivatives: neuropathological implications. Front Neuroenerg 2:1
Kovacs R et al (2009) Endogenous nitric oxide is a key promoting factor for initiation of seizure-like events in hippocampal and entorhinal cortex slices. J Neurosci 29(26):8565–77
Chang R et al (2008) Neuroprotective effects of guanosine on stroke models in vitro and in vivo. Neurosci Lett 431(2):101–5
Lanznaster D et al (2016) Guanosine: a neuromodulator with therapeutic potential in aging-related disorders. Aging Dis 7:5
Uemura Y et al (1991) Neurochemical analysis of focal ischemia in rats. Stroke 22(12):1548–53
Dal-Cim T et al (2011) Guanosine is neuroprotective against oxygen/glucose deprivation in hippocampal slices via large conductance Ca(2) + −activated K+ channels, phosphatidilinositol-3 kinase/protein kinase B pathway activation and glutamate uptake. Neuroscience 183:212–20
Dal-Cim T et al (2016) Neuroprotection promoted by guanosine depends on glutamine synthetase and glutamate transporters activity in hippocampal slices subjected to oxygen/glucose deprivation. Neurotox Res 29(4):460–8
Oliveira IJ et al (2002) Neuroprotective effect of GMP in hippocampal slices submitted to an in vitro model of ischemia. Cell Mol Neurobiol 22(3):335–44
Pocock JM, Nicholls DG (1998) Exocytotic and nonexocytotic modes of glutamate release from cultured cerebellar granule cells during chemical ischaemia. J Neurochem 70(2):806–13
Strasser U, Fischer G (1995) Quantitative measurement of neuronal degeneration in organotypic hippocampal cultures after combined oxygen/glucose deprivation. J Neurosci Methods 57(2):177–86
Trotti D, Danbolt NC, Volterra A (1998) Glutamate transporters are oxidant-vulnerable: a molecular link between oxidative and excitotoxic neurodegeneration? Trends Pharmacol Sci 19(8):328–34
Liu Y et al (1997) Mechanism of cellular 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) reduction. J Neurochem 69(2):581–93
Noraberg J, Kristensen BW, Zimmer J (1999) Markers for neuronal degeneration in organotypic slice cultures. Brain Res Brain Res Protoc 3(3):278–90
Pringle AK et al (1996) Selective N-type calcium channel antagonist omega conotoxin MVIIA is neuroprotective against hypoxic neurodegeneration in organotypic hippocampal-slice cultures. Stroke 27(11):2124–30
Ferreira AG et al (2012) Experimental hyperprolinemia induces mild oxidative stress, metabolic changes, and tissue adaptation in rat liver. J Cell Biochem 113(1):174–83
Hernanz R et al (2008) Ouabain treatment increases nitric oxide bioavailability and decreases superoxide anion production in cerebral vessels. J Hypertens 26(10):1944–54
Yang Y et al (2004) Nitric oxide spatial distribution in single cultured hippocampus neurons: investigation by projection of reconstructed 3-D image and visualization technique. Cell Biol Int 28(8–9):577–83
Kooy NW et al (1994) Peroxynitrite-mediated oxidation of dihydrorhodamine 123. Free Radic Biol Med 16(2):149–56
Brandwilliams W, Cuvelier ME, Berset C (1995) Use of a free-radical method to evaluate antioxidant activity. Food Sci Technol Lebensmwiss Technol 28(1):25–30
Colle D et al (2012) Antioxidant properties of Taraxacum officinale leaf extract are involved in the protective effect against hepatoxicity induced by acetaminophen in mice. J Med Food 15(6):549–56
Green LC et al (1982) Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem 126(1):131–8
Ehrenberg B et al (1988) Membrane potential can be determined in individual cells from the nernstian distribution of cationic dyes. Biophys J 53(5):785–94
Lorrio S et al (2013) Novel multitarget ligand ITH33/IQM9.21 provides neuroprotection in in vitro and in vivo models related to brain ischemia. Neuropharmacology 67:403–11
Perry SW et al (2011) Mitochondrial membrane potential probes and the proton gradient: a practical usage guide. Biotechniques 50(2):98–115
Dal-Cim T et al (2013) Guanosine controls inflammatory pathways to afford neuroprotection of hippocampal slices under oxygen and glucose deprivation conditions. J Neurochem 126(4):437–50
Molz S et al (2011) Neuroprotective effect of guanosine against glutamate-induced cell death in rat hippocampal slices is mediated by the phosphatidylinositol-3 kinase/Akt/glycogen synthase kinase 3beta pathway activation and inducible nitric oxide synthase inhibition. J Neurosci Res 89(9):1400–8
Cardenas A et al (1998) Protective effect of N-(3-(aminomethyl)benzyl) acetamidine, an inducible nitric oxide synthase inhibitor, in brain slices exposed to oxygen-glucose deprivation. Eur J Pharmacol 354(2–3):161–5
Thauerer B, Zur Nedden S, Baier-Bitterlich G (2012) Purine nucleosides: endogenous neuroprotectants in hypoxic brain. J Neurochem 121(3):329–42
Lara DR et al (2001) Effect of orally administered guanosine on seizures and death induced by glutamatergic agents. Brain Res 912(2):176–80
Schmidt AP, Lara DR, Souza DO (2007) Proposal of a guanine-based purinergic system in the mammalian central nervous system. Pharmacol Ther 116(3):401–16
Ribeiro FF et al (2016) Purine nucleosides in neuroregeneration and neuroprotection. Neuropharmacology 104:226–42
Dal-Cim T et al (2012) Guanosine protects human neuroblastoma SH-SY5Y cells against mitochondrial oxidative stress by inducing heme oxigenase-1 via PI3K/Akt/GSK-3beta pathway. Neurochem Int 61(3):397–404
Traversa U et al (2002) Specific [(3)H]-guanosine binding sites in rat brain membranes. Br J Pharmacol 135(4):969–76
Volpini R et al (2011) Evidence for the existence of a specific g protein-coupled receptor activated by guanosine. ChemMedChem 6(6):1074–80
Schmidt AP et al (2008) Guanosine and its modulatory effects on the glutamatergic system. Eur Neuropsychopharmacol 18(8):620–2
Jackson EK et al (2013) Extracellular guanosine regulates extracellular adenosine levels. Am J Physiol Cell Physiol 304(5):C406–21
Hansel G et al (2014) The potential therapeutic effect of guanosine after cortical focal ischemia in rats. PLoS ONE 9(2):e90693
Quincozes-Santos A et al (2014) Guanosine protects C6 astroglial cells against azide-induced oxidative damage: a putative role of heme oxygenase 1. J Neurochem 130(1):61–74
Cossenza M et al (2014) Nitric oxide in the nervous system: biochemical, developmental, and neurobiological aspects. Vitam Horm 96:79–125
Iadecola C (1997) Bright and dark sides of nitric oxide in ischemic brain injury. Trends Neurosci 20(3):132–9
Nagafuji T et al (1995) Nitric oxide synthase in cerebral ischemia. Possible contribution of nitric oxide synthase activation in brain microvessels to cerebral ischemic injury. Mol Chem Neuropathol 26(2):107–57
Endres M et al (2004) Targeting eNOS for stroke protection. Trends Neurosci 27(5):283–9
Terpolilli NA, Moskowitz MA, Plesnila N (2012) Nitric oxide: considerations for the treatment of ischemic stroke. J Cereb Blood Flow Metab 32(7):1332–46
Huang Z et al (1994) Effects of cerebral ischemia in mice deficient in neuronal nitric oxide synthase. Science 265(5180):1883–5
Vannucchi MG et al (2007) Relationships between neurons expressing neuronal nitric oxide synthase, degree of microglia activation and animal survival. A study in the rat cortex after transient ischemia. Brain Res 1132(1):218–27
Iijima T et al (2003) Mitochondrial membrane potential and intracellular ATP content after transient experimental ischemia in the cultured hippocampal neuron. Neurochem Int 43(3):263–9
Acknowledgments
Research supported by grants from the Brazilian funding agencies to C.I.T.: CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico)–Projects IBN-Net # 01.06.0842-00 and INCT for Excitotoxicity and Neuroprotection; CAPES (Coordenação do Pessoal de Ensino Superior)–Project CAPES-PVE 052/2012; FAPESC (Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina)–Project NENASC. C.I.T. is a recipient of CNPq productivity fellowship and M.P.C. is a recipient of CAPES/PNPD post-doctoral scholarship. The authors state no conflicts of interest. All authors have materially participated in the research and/or article preparation.
Compliance with ethical standards
The procedures used in the present study complied with the guidelines on animal care of the UFSC Ethics Committee on the Use of Animals (CEUA), which follows the “Principles of laboratory animal care” from NIH (2011).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomaz, D.T., Dal-Cim, T.A., Martins, W.C. et al. Guanosine prevents nitroxidative stress and recovers mitochondrial membrane potential disruption in hippocampal slices subjected to oxygen/glucose deprivation. Purinergic Signalling 12, 707–718 (2016). https://doi.org/10.1007/s11302-016-9534-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-016-9534-3