Abstract
Bacteriophages, as the most dominant and diverse entities in the universe, have the potential to be one of the most promising therapeutic agents. The emergence of multidrug-resistant bacteria and the antibiotic crisis in the last few decades have resulted in a renewed interest in phage therapy. Furthermore, bacteriophages, with the capacity to rapidly infect and overcome bacterial resistance, have demonstrated a sustainable approach against bacterial pathogens-particularly in biofilm. Biofilm, as complex microbial communities located at interphases embedded in a matrix of bacterial extracellular polysaccharide substances (EPS), is involved in health issues such as infections associated with the use of biomaterials and chronic infections by multidrug resistant bacteria, as well as industrial issues such as biofilm formation on stainless steel surfaces in food industry and membrane biofouling in water and wastewater treatment processes. In this paper, the most recent studies on the potential of phage therapy using natural and genetically-modified lytic phages and their associated enzymes in fighting biofilm development in various fields including engineering, industry, and medical applications are reviewed. Phage-mediated prevention approaches as an indirect phage therapy strategy are also explored in this review. In addition, the limitations of these approaches and suggestions to overcome these constraints are discussed to enhance the efficiency of phage therapy process. Finally, future perspectives and directions for further research towards a better understanding of phage therapy to control biofilm are recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacteriophages (phages) are viruses that infect only prokaryotes. They are the most ubiquitous and abundant organisms on Earth with an estimated total number of 1032 phages on the planet (Hanlon 2007). Phages play a significant role in maintaining microbial community balance on the planet (Sulakvelidze 2011). Although phages were discovered more than a century ago, lack of knowledge on phage biology and the discovery of antibiotics in the mid-1940s resulted in disregarding of phage applications. However, emergence of multi-drug resistant bacteria as the consequence of overuse of antibiotics in the last few decades has renewed interest in, and the urgent need for, other alternative antibacterial strategies including phage therapy. In addition, biofouling, i.e. the formation of biofilm, on stainless steel surfaces in food processing and membrane reactors performing water and wastewater treatment, is an unwanted situation and a major issue impacting the long term sustainability of these processes.
Biofilm is complex aggregates of structured microbial communities located at interphases and embedded in a matrix of bacterial extracellular polysaccharide substances (EPS) (Costerton et al. 1999). Through diverse metabolic processes and interactions between individual components, biofilm exhibit dynamic structural characteristics. The bacterial cells within a biofilm may not be at the same growth phase and thus form a phenotypically heterogeneous construction (Hall-Stoodley et al. 2004). The combination of an exopolysaccharide matrix, i.e. EPS, and phenotypic heterogeneity of the constituent cells confer on the biofilm a significant resistance to chemical and immunological approaches (Burrowes et al. 2011). Biofilm is a long-term survival strategy employed by bacteria and involved in 60 % of all microbial infections associated with the use of biomaterials, chronic infection with multi-drug resistant bacteria, as well as industrial issues such as biofouling (Percival et al. 2012; Wu et al. 2015). Many studies have been focused on developing efficient physical, chemical, and biological methods for biofilm prevention and disruption (Taylor and Webster 2009; Musk et al. 2006; Xiong and Liu 2010). However, due to significant increases in tolerance to antimicrobial agents, the emergence of antibiotic resistant bacterial strains, the presence of EPS matrices, and the effects of biofilm age, researchers are increasingly studying alternative strategies such as the use of bacteriophages to fight biofilm development.
Bacteriophage life cycles, properties and advantages
The genetic material of bacteriophages is contained in a protein capsid. Majority of phages have helical or icosahedral capsid construction (Lidmar et al. 2003; Lodish et al. 2000). The capsid is connected through a collar to a tail composed of tail fibers with tips (Orlova 2012). The tail fibers recognize receptors on the bacterial cell surface, which determine the range of phage’s host organisms. Depending on the specificity of the receptors, phages can be categorized into monovalent phages with the capacity to infect a specific bacterial species or strain, and polyvalent phages that are able to adsorb to bacterial surfaces enabling them to infect across different bacterial species or even genera.
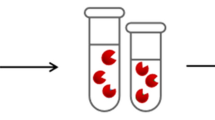
Bacteriophages can be categorized into two major classes according to their life cycle: virulent (lytic) phages and temperate (lysogenic) phages (Guttman et al. 2004; Lodish et al. 2000). As shown in Fig. 1, during a lytic cycle, virulent phage particles attach to the host bacterial surface, inject their genetic material into the host’s DNA, replicate their DNA using host machinery, and then assemble their structural components until lysing the host cell and releasing new phage progenies into the environment. During the lysogenic cycle, temperate phages integrate their genome onto the host chromosome, remain as a prophage within the bacterium and vertically transmit, by cell division, its progeny until the lytic cycle is induced (Casjens 2003; Motlagh et al. 2015). Although only lytic phages generally qualify for therapeutic purposes, lysogenic phages can also be exploited therapeutically to transfer genes for making the bacteria more susceptible to other factors such as antibiotics (Lu and Collins 2009).
Phage therapy mechanisms to control bacterial biofilm through phage mediated disruption. As labeled in the figure, the steps of biocontrol of biofilm using bacteriophages include: 1 application of phages, 2 initiation of biofilm EPS disruption through virion associated enzymes such as dispersin B (DspB) or EPS depolymerases, 3 biofilm disruption through disintegration of EPS networks and exposing the bacteriophage infection, and 4 complete disintegration of biofilm and bacterial cell lysis. ABX stands for antibiotics
The greatest characteristic of phages that makes them riveting for therapeutics is their high specificity of infection (Koskella and Meaden 2013). The specificity of the receptors on the bacterial cell surface determines the range of phage host organisms resulting in phages typically recognizing only a limited range of bacterial strains, and reducing the damage to the overall microbial community structure (Modi et al. 2014). This host-specificity selection confers an array of advantages compared to antibiotics which affect the entire microbial community structure, rather than the intended target pathogen (Chibani-Chennoufi et al. 2004).
Bacteriophages multiply at the site of infection and only when the bacterial hosts are available. Therefore, propagation of phages depends on the presence of their host with self-limiting and self-dosing properties (Kutter 2005). In addition, although phage-based therapeutic approaches have their own limitation and bacterial resistance to bacteriophages may be developed, but phage treatment is usually applied only in one treatment dose and the chance of cumulative mutations with phage resistance is much lower (Alisky et al. 1998). Furthermore, phage therapy can be a successful method to use when addressing the challenge of biofilm as some phages are capable of synthesizing specific enzymes such as polysaccharidases, polysaccharide lyases, or hydrolases which are able to degrade exopolysaccharide structural networks-a major component of biofilm-even before they begin interacting with their specific hosts within the biofilm (Wittebole et al. 2014; Drulis-Kawa et al. 2012). Previous studies showed that these enzymes can be synthesized with phages interacting with strains of Escherichia Coli (Chibeu et al. 2012), Pseudomonas Aeruginosa (Hanlon et al. 2001), Pseudomonas Putida (Cornelissen et al. 2011), Erwinia amylovora (Born et al. 2014), and other ESKAPE pathogens (Bales et al. 2013).
Phage therapy applications for biofilm control
In this review, phage therapy applications for biofilm control are categorized into two major sections: medical and industrial applications. The biofilm that develop on or within indwelling medical devices is one of the major components of bacterial infection in patients using those devices which can be prevented and controlled using bacteriophages. Besides medical applications, using bacteriophages in biofilm control in industrial applications such as stainless steel surfaces in food processing and membrane reactors in water and wastewater treatments facilities is another approach that is reviewed in this article. Figure 1 illustrates the schematic diagram of typical phage therapy mechanisms on bacterial biofilm and the following disintegration of the biofilm.
As biofilm consist of complex microbial communities embedded in an extracellular polysaccharide substance (EPS), their interactions with phages are also relatively complex and diverse. Bacteriophages may infect biofilm-forming bacteria (Merril et al. 2003; Curtin and Donlan 2006; Harper et al. 2014), planktonic bacteria passing through a biofilm, or disrupt the stability of the EPS by producing degrading enzymes (Leiman et al. 2004; Lu and Collins 2007; Yan et al. 2014). In addition, imaging techniques such as atomic force microscopy (AFM) have shown the heterogeneity of biofilm structures with a diverse distribution of cells, extracellular matrix, and water-filled channels and pores (Zaky et al. 2012) that may facilitate phage access inside the biofilm. An increase in the medium composition and the amount of nutrients causes an increase in bacterial cell growth, which results in larger burst sizes, shorter eclipse and latency periods, and eventually expedited phage therapy processes (Krogfelt et al. 1993; Poulsen et al. 1995; Letarov et al. 2010).
Although phages have significant capacity as antimicrobial agents for biofilm control, several factors may reduce the efficiency of lytic phages resulting in an impact on the effectiveness of phage therapy. As bacterial communities in biofilm are surrounded by a polysaccharide matrix, phages may not be able to penetrate into deeper layers of the biofilm to reach the host cells (Briandet et al. 2008). In fact, EPS can act as a shelter or shield to protect the bacteria in the biofilm and decrease their susceptibility to antibiotics or other biocides. Therefore, the fundamental step in a phage infection, i.e. initial adsorption of phage particles on the bacterial cell surface with specific receptors, may not occur (Doolittle et al. 1996). However, some phages have accompanying polymerase enzymes to hydrolyze the EPS and reach the lipopolysaccharide (LPS) and outer membrane proteins (OMP) of the exposed surface of the bacterial cell (Glonti et al. 2010). Additionally, phages can be genetically modified for depolymerase synthesis to produce EPS-degrading enzymes (Azeredo and Sutherland 2008; Donlan 2009). Indeed, extracellular proteins and polysaccharides are two main components of the most EPS matrices, and therefore the proteolytic enzyme (protease) and polysaccharases enzyme are two main EPS-degrading enzymes that can be applied for biofilm detachment (Loiselle and Anderson 2003). However, these enzymes are not stable in the environment, and high pH, temperature, or salt concentrations could denature them leading to a decrease in enzymatic activity. Therefore, using phages that have evolved to naturally synthesize and produce these enzymes in situ can significantly increase the success of the EPS degradation process.
The other decisive factor in phage-based control of biofilm is the appropriate use of the phage-to-host ratio (PHR) for the treatment process. As it was shown in the Hanlon et al. (2001) study, a 100:1 phage:host ratio caused a 1 log reduction in P. aeruginosa biofilm viable count while a 1000:1 phage:host ratio caused 10 times more with 2 log reduction after 24 h of treatment. In another study treating 72 h E. coli K12 biofilm with phages for a short period of 30 min also showed greater biofilm disruption with phage:host ratio of 100:1 compared to 10:1 ratio (Corbin et al. 2001).
Phage therapy for biofilm control in medical applications
The formation of biofilm involves an initial attachment of bacterial cells to the surface followed by formation of micro-colonies and maturation of the biofilm (Motlagh et al. 2013). Therefore, the first strategy for use of bacteriophages in fighting biofilm is prevention and blockage of adhesion and proliferation of bacteria and biofilm development. Preventing the development of Listeria monocytogenes biofilm on stainless steel surfaces (Hibma et al. 1997) was one of the first studies that contributed to further phage therapy research for medical applications such as the study conducted by Curtin and Donlan (2006) to inhibit Staphylococcus epidermidis biofilm on the surfaces of medical devices. Eradication of Pseudomonas fluorescens biofilm at an early stage of biofilm development (Sillankorva et al. 2004) and pre-treatment of an in vitro model to prevent P. aeruginosa biofilm on medical catheters (Fu et al. 2010) were some of the studies on antibiotic-resistant pathogens that proved the effectiveness of phage therapy.
The conventional phage therapy approach is the administration of naturally-isolated virulent phages directly to the targeted bacterial strains with the goal of lysing the bacterial host responsible for an acute or chronic infection. The combination of therapeutic phage application with antibiotic treatment was a step beyond the traditional phage therapy approach for biofilm control. Studies of antimicrobial synergy between phages and antibiotics have shown that sub-lethal concentrations of certain antibiotics, typically involved in cell division inhibition, increases the biosynthetic capacity of the bacterial host, which consequently increases the phage production and ultimately accelerates cell lysis (Comeau et al. 2007; Bedi et al. 2009; Ryan et al. 2012). In fact, the mechanisms of DNA repair system in the bacterial host was studied to be disabled using modified and engineered M13 phage by overexpressing lexA3 gene to suppress the SOS system resulting in inhibition of emergence of antibiotic resistance and enhance of bacterial killing (Lu and Collins 2009).
Another promising alternative in phage therapy is using phage gene products such as endolysins rather than implementing entire virions (Fischetti 2005; Nelson et al. 2012; Schmelcher et al. 2012). This approach eliminates the possibility of transmitting toxic properties through transduction to bacteria by phages (Hermoso et al. 2007) and reduces the risk of emergence of bacterial-resistance to phages (Borysowski et al. 2006). One drawback of this approach is the non-specificity of endolysin for Gram-negative bacteria due to their impermeable outer membrane (Nobrega et al. 2015), which makes this alternative ineffective for Gram-negative biofilm.
Synthetic biology of phages through the use of modular designs to develop more effective phages for the eradication of bacterial biofilm is also a novel approach that has been studied in recent years. Genetically modified phage T7 was able to disrupt bacterial biofilm by expressing dispersin B as an EPS depolymerase and degrading enzyme (Lu and Collins 2007). As a result, the engineered T7 phage showed promising results in significantly increasing the in vivo destruction of E. coli biofilm compared to use of the parent T7 strain or dispersin B enzyme alone.
In another study, genetically-engineered temperate phages were exploited to deliver a functional DNA nuclease, clustered regularly interspaced short palindromic repeats (CRISPR) CRISPR-associated (Cas) system into the genome of antibiotic-resistant bacteria, which repealed antibiotic resistance, eliminated the transfer of resistance between strains, and destroyed both antibiotic resistance-conferring plasmids and genetically modified lytic phages (Kiro et al. 2014; Yosef et al. 2015). Another study by Bender et al. (2015) highlighted the importance of using engineered phages for developing non-antibiotic drugs as therapeutics for the treatment of Clostridium difficile infections. These strategies can be used to facilitate the replacement of antibiotic-resistant pathogens embedded in bacterial biofilm with susceptible bacterial strains that can be eliminated with a combination of antibiotic treatments.
In order to improve the antimicrobial effects of phages to control biofilm, a range of genetic tools have been studied in the last few years to shape phages’ biological properties. Table 1 shows a summary of possibilities for genetically modified improvements to phage therapy for biofilm control.
Phage therapy for biofilm control in industrial applications
Preventing the biofilm development on stainless steel surfaces using phages is also significantly contributed to food processing industry. The presence of extra nutrients in the food production processes intensifies the opportunity for the development of biofilm, which leads to serious hygienic issues and economic losses due to food spoilage (Srey et al. 2013). Previous researches showed the potential of bacteriophages in removing biofilm of Listeria monocytogenes, as one of the most prevalent foodborne pathogens (Soni and Nannapaneni 2010; Chaitiemwong et al. 2014). In addition, study of bacteriophages application in post-production processes to prevent growth of food spoiling bacteria such as Staphylococcus aureus (Garcia et al. 2007), E. coli O157:H7 (Abuladze et al. 2008), and Salmonella enterica (Kocharunchitt et al. 2009) also showed their significance in post-harvest biofilm biocontrol.
Membrane biofouling, i.e. biofilm formation by microorganisms leading to the fouling of membranes, is a major issue encountered in the membrane filtration process, which plays a significant role in determining their practical applications in water and wastewater treatment. As a response to membrane biofouling, the net flowrate passing through the membrane reduces over time, eventually resulting in a need to replace the membrane module. Although both physical and chemical methods are currently employed to cascade the biofilm, the cost and energy, as well as operational issues, are concerns about these processes for biofouling control (Le-Clech et al. 2006). In addition, the EPS matrix that surrounds biofilm is believed to be an irreversible foulant of membranes that cannot be efficiently removed by conventional physical or chemical cleaning methods (Herzberg et al. 2009).
There are some recent studies that have demonstrated that addition of specific bacteriophages to membrane bioreactors could reduce microbial attachment to membrane surface and increase membrane permeability (Goldman et al. 2009; Bhattacharjee et al. 2015). It was reported that the addition of bacteriophages reduced the microbial attachment by 40–60 % with continuous inactivation of planktonic and freshly formed biofilm when treating effluents containing three different bacterial species (Goldman et al. 2009). As one of the first studies, Bhattacharjee et al. (2015) showed biocontrol of biofouling on a lab-scale membrane bioreactor by a multidrug-resistant strain, Delftia tsuruhatensis ARB-1, through use of a lytic bacteriophage. When the biofilm consists of multiple species of bacteria, which generally occurs in industrial applications, a phage cocktail including a combination of several phage types may be needed to prevent adhesion and biofilm formation on the membrane surface.
The pore size of most membrane filters that are being used in water and wastewater treatment (e.g., ultrafiltration (UF), nanofiltration (NF), and reverse osmosis (RO)) is between 1 and 100 nm, which is generally smaller than the phage particles (30–200 nm). Therefore, following phage application to the membrane, some of the seed phages can attach and remain immobilized on the membrane surface, possibly contributing to continuous infection of oncoming bacteria (Brockhurst et al. 2006). However, small amounts of phage particles can pass through the membrane, which may pose an issue in real applications of water and wastewater treatment (Goldman et al. 2009).
The most widely used method for wastewater treatment is the activated sludge process (ASP), a process involving a consortium of microorganisms and biological flocs in bioreactors to remove organic carbon and nutrients (Motlagh and Goel 2014). Besides other processes involved in this type of wastewater treatment, sludge dewatering is an important finalizing process to affect a reduction of the sludge volume, resulting in saving equipment capacity as well as downstream treatment costs (Withey et al. 2005). Extracellular polysaccharide substances (EPS) found in bacterial flocs binds microbial cells and particulate matter together, influencing the formation, settling, and water-binding ability of the activated sludge flocs (Bura et al. 1998). High levels of microbial EPS can adversely affect the dewatering ability of the activated sludge and increase the sludge volume (Sanin and Vesilind 1994). Excessive productions of EPS and dewatering problems for activated sludge have been implicated by species such as Zoogloea and Thauera (Lajoie et al. 2000). To address this challenge, since bacteriophages can carry polysaccharide depolymerase enzymes (PDE), they can be exploited to selectively target specific strains producing excessive EPS, reduce the EPS level, and improve the ability of the sludge to be dewatered.
Phage therapy limitations and strategies to overcome these constraints
Despite the significant advances in phage therapy, there are still some major concerns and limitations regarding the use of phages that need to be addressed. However, these constraints are not significant issues and this section discusses some strategies to overcome or diminish these limitations.
Limited spectrum of host infection
Although specificity of phages for the hosts that they infect significantly reduces the damage to normal microbial communities, this specificity means that phage therapy using natural lytic phages requires identification and isolation of the effective phage, which may delay the treatment process. Using a mixture (cocktail) of different phage types with complementary features can circumvent the limited host range of a single phage (Chan et al. 2013; Goodridge 2010). In addition, using different types of phages infecting the same species and strains reduces the probability of phage-resistant bacteria development (Chan and Abedon 2012; Gu et al. 2012). Besides using a phage cocktail, polyvalent phages that have a broad host range can be used for infection. A study of dual-species biofilm formed by P. fluorescens (Gram-negative) and Staphylococcus lentus (Gram-positive) demonstrated successful disinfection by the action of polyvalent lytic phages (Sillankorva et al. 2010). Furthermore, the host range can be expanded by a homologous recombination of phages with a plasmid altering the tail fiber protein (Mahichi et al. 2009; Lin et al. 2012).
Risk of gene transduction
Another concern about phage therapy, particularly when lysogenic phages are being implemented, is the possibility of transduction wherein specific bacterial genes or other bacterial virulence factors may be transferred to other bacteria by the phages, resulting in the transfer of pathogenicity determinants and virulence factors leading to the development of a new pathogen or even more resistant bacteria (Brabban et al. 2005; O’Shea and Boyd 2002; Maiques et al. 2007). However, as most of the therapeutic applications of phages are with lytic phages, the probability of gene transduction is very low.
Release of toxins following the bacterial lysis
A further concern about using lytic phages that needs to be considered is the release of significant amounts of endotoxin, exotoxins, and superantigens following the rapid lysis of bacteria, which may potentially cause serious side effects such as the induction of an inflammatory response leading to multiple organ failures (Drulis-Kawa et al. 2012). However, this potential concern also applies to rapidly bactericidal antibiotics as well (Goodridge 2010).
Production of neutralizing antibodies
The body’s production of neutralizing antibodies against phages and phage immunogenicity is a valid concern in the therapeutic use of phages in vivo which may inhibit the treatment. Following the administration of phages, they can be rapidly recognized by adaptive immune defense mechanisms within the body as invaders and removed from systematic circulation (Dabrowska et al. 2005). However, production of antibodies was only observed when applied intravenously and not much effect was observed after oral and local administration (Abedon et al. 2011). In addition, this limitation is not a considerable issue in case of acute infections since the rate of antibody production is much less than the rate of bacterial infection and lysis.
Development of resistance
The development of bacterial host resistance against phages as a result of mutation and selection or temperate phage acquisition could yield a decreased efficiency in the phage therapy processes. Two major mechanisms can be involved in bacterial resistance to a specific phage including (i) pre-entry resistance mechanisms such as loss or lack of receptor (Liu et al. 2002) and structural modification and/or masking of the receptor (Labrie et al. 2010), and (ii) post-entry resistance mechanisms such as the degradation of phage DNA by restriction-modification defense systems and abortive infections (Drulis-Kawa et al. 2012). However, few studies showed resistance during in vivo phage therapy (Drulis-Kawa et al. 2012; Kutter et al. 2010). In addition, isolation of novel active phages from the environment could provide new possibilities for treatment and minimize the resistance issue.
Concluding remarks and directions for future research
Bacteriophage therapy acceptance in medical, industrial, and biotechnological applications has increased in the last few years. Since biofilm, and particularly antibiotic resistant forms of biofilm, pose a significant hurdle to biomaterials as well as industrial applications, new antibacterial strategies such as phage-based therapeutic approaches need to be explored. As phage therapy becomes more acceptable and better understood, genetically-modified phages can supply a crucial alternative to overcome the challenge of biofilm control in environmental, industrial, and clinical settings. Novel synthetic biological techniques will enable rational engineering to equip native bacteriophages with new functionalities such as biofilm-degrading enzymes to produce libraries of enzymatically active phages that can contribute to biofilm-remediation phage therapy processes. Furthermore, phages can alter antibiotic-resistant bacteria to susceptible strains by delivering functional DNA nucleases such as CRISPR fragments.
A better understanding of phage-host interactions in biofilm, phage diversity, and dynamics are essential to recognize the limitations of phage therapy for biofilm control and to design new strategies for anti-biofilm properties. In addition, the majority of phage genome and their gene functions are still unknown and need to be better understood for more effective phage therapy on biofilm.
This review showed the feasibility of phage therapy for biofilm control and the benefits of using phages in medical and industrial settings. Additionally, it demonstrated that genetically-modified phages have the capability of reducing bacterial biofilm more efficiently than conventional approaches. However, phage therapy needs more research and development to achieve the commercial applications in medical and industrial problems.
References
Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM (2011) Phage treatment of human infections. Bacteriophage 1(2):66–85
Abuladze T, Li M, Menetrez MY, Dean T, Senecal A, Sulakvelidze A (2008) Bacteriophages reduce experimental contamination of hard surfaces, tomato, spinach, broccoli, and ground beef by Escherichia coli O157: H7. Appl Environ Microbiol 74(20):6230–6238
Alisky J, Iczkowski K, Rapoport A, Troitsky N (1998) Bacteriophages show promise as antimicrobial agents. J Infect 36(1):5–15
Azeredo J, Sutherland IW (2008) The use of phages for the removal of infectious biofilms. Curr Pharm Biotechnol 9(4):261–266
Bales PM, Renke EM, May SL, Shen Y, Nelson DC (2013) Purification and characterization of biofilm-associated EPS exopolysaccharides from ESKAPE organisms and other pathogens. PLoS ONE 8(6):e67950
Bedi MS, Verma V, Chhibber S (2009) Amoxicillin and specific bacteriophage can be used together for eradication of biofilm of Klebsiella pneumoniae B5055. World J Microbiol Biotechnol 25(7):1145–1151
Bender KO, Garland M, Ferreyra JA, Hryckowian AJ, Child MA, Puri AW, Solow-Cordero DE, Higginbottom SK, Segal E, Banaei N, Shen A, Sonnenburg JL (2015) A small-molecule antivirulence agent for treating Clostridium difficile infection. Sci Transl Med 7(306):306ra148–306ra148
Bhattacharjee AS, Choi JD, Motlagh AM, Mukherji ST, Goel R (2015) Bacteriophage therapy for membrane biofouling in membrane bioreactors and antibiotic-resistant bacterial biofilms. Biotechnol Bioeng 112(8):1644–1654
Born Y, Fieseler L, Klumpp J, Eugster MR, Zurfluh K, Duffy B, Loessner MJ (2014) The tail-associated depolymerase of Erwinia amylovora phage L1 mediates host cell adsorption and enzymatic capsule removal, which can enhance infection by other phage. Environ Microbiol 16(7):2168–2180
Borysowski J, Weber-Dąbrowska B, Górski A (2006) Bacteriophage endolysins as a novel class of antibacterial agents. Exp Biol Med 231(4):366–377
Brabban AD, Hite E, Callaway TR (2005) Evolution of foodborne pathogens via temperate bacteriophage-mediated gene transfer. Foodbourne Pathog Dis 2(4):287–303
Briandet R, Lacroix-Gueu P, Renault M, Lecart S, Meylheuc T, Bidnenko E, Fontaine-Aupart MP (2008) Fluorescence correlation spectroscopy to study diffusion and reaction of bacteriophages inside biofilms. Appl Environ Microbiol 74(7):2135–2143
Brockhurst MA, Buckling A, Rainey PB (2006) Spatial heterogeneity and the stability of host-parasite coexistence. J Evolut Biol 19(2):374–379
Bura R, Cheung M, Liao B, Finlayson J, Lee BC, Droppo IG, Liss SN (1998) Composition of extracellular polymeric substances in the activated sludge floc matrix. Water Sci Technol 37(4):325–333
Burrowes B, Harper DR, Anderson J, McConville M, Enright MC (2011) Bacteriophage therapy: potential uses in the control of antibiotic-resistant pathogens. Expert Rev Anti-infective Ther 9(9):775–785
Casjens S (2003) Prophages and bacterial genomics: what have we learned so far? Mol Microbiol 49(2):277–300
Chaitiemwong N, Hazeleger WC, Beumer RR (2014) Inactivation of Listeria monocytogenes by disinfectants and bacteriophages in suspension and stainless steel carrier tests. J Food Prot 77(12):2012–2020
Chan BK, Abedon ST (2012) 1 phage therapy pharmacology: phage cocktails. Adv Appl Microbiol 78:1
Chan BK, Abedon ST, Loc-Carrillo C (2013) Phage cocktails and the future of phage therapy. Future Microbiol 8(6):769–783
Chibani-Chennoufi S, Sidoti J, Bruttin A, Kutter E, Sarker S, Brüssow H (2004) In vitro and in vivo bacteriolytic activities of Escherichia coli phages: implications for phage therapy. Antimicrob Agents Chemother 48(7):2558–2569
Chibeu A, Lingohr EJ, Masson L, Manges A, Harel J, Ackermann HW, Boerlin P (2012) Bacteriophages with the ability to degrade uropathogenic Escherichia coli biofilms. Viruses 4(4):471–487
Comeau AM, Tétart F, Trojet SN, Prere MF, Krisch HM (2007) Phage-antibiotic synergy (PAS): beta-lactam and quinolone antibiotics stimulate virulent phage growth. PLoS ONE 2(8):e799
Corbin BD, McLean RJ, Aron GM (2001) Bacteriophage T4 multiplication in a glucose-limited Escherichia coli biofilm. Can J Microbiol 47(7):680–684
Cornelissen A, Ceyssens PJ, T’Syen J, Van Praet H, Noben JP, Shaburova OV, Lavigne R (2011) The T7-related Pseudomonas putida phage phi15 displays virion-associated biofilm degradation properties. PLoS ONE 6(4):e18597
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284(5418):1318–1322
Curtin JJ, Donlan RM (2006) Using bacteriophages to reduce formation of catheter-associated biofilms by Staphylococcus epidermidis. Antimicrob Agents Chemother 50(4):1268–1275
Dabrowska K, Switała-Jelen K, Opolski A, Weber-Dabrowska B, Gorski A (2005) Bacteriophage penetration in vertebrates. J Appl Microbiol 98(1):7–13
Donlan RM (2009) Preventing biofilms of clinically relevant organisms using bacteriophage. Trends Microbiol 17(2):66–72
Doolittle MM, Cooney JJ, Caldwell DE (1996) Tracing the interaction of bacteriophage with bacterial biofilms using fluorescent and chromogenic probes. J Ind Microbiol 16(6):331–341
Drulis-Kawa Z, Majkowska-Skrobek G, Maciejewska B, Delattre AS, Lavigne R (2012) Learning from bacteriophages-advantages and limitations of phage and phage-encoded protein applications. Curr Protein Pept Sci 13(8):699
Edgar R, Friedman N, Molshanski-Mor S, Qimron U (2012) Reversing bacterial resistance to antibiotics by phage-mediated delivery of dominant sensitive genes. Appl Environ Microbiol 78(3):744–751
Fischetti VA (2005) Bacteriophage lytic enzymes: novel anti-infectives. Trends Microbiol 13(10):491–496
Fu W, Forster T, Mayer O, Curtin JJ, Lehman SM, Donlan RM (2010) Bacteriophage cocktail for the prevention of biofilm formation by Pseudomonas aeruginosa on catheters in an in vitro model system. Antimicrob Agents Chemother 54(1):397–404
Garcia P, Madera C, Martínez B, Rodríguez A (2007) Biocontrol of staphylococcus aureus in curd manufacturing processes using bacteriophages. Int Dairy J 17(10):1232–1239
Glonti T, Chanishvili N, Taylor PW (2010) Bacteriophage-derived enzyme that depolymerizes the alginic acid capsule associated with cystic fibrosis isolates of Pseudomonas aeruginosa. J Appl Microbiol 108(2):695–702
Goldman G, Starosvetsky J, Armon R (2009) Inhibition of biofilm formation on UF membrane by use of specific bacteriophages. J Membr Sci 342(1):145–152
Goodridge LD (2010) Designing phage therapeutics. Curr Pharm Biotechnol 11(1):15–27
Gu J, Liu X, Li Y, Han W, Lei L, Yang Y, Feng X (2012) A method for generation phage cocktail with great therapeutic potential. PLoS ONE 7(3):e31698
Guttman B, Raya R, Kutter E (2004) Basic phage biology. In: Bacteriophages: biology and applications. CRC Press, pp 30–32
Hagens S, Habel A, Von Ahsen U, Von Gabain A, Bläsi U (2004) Therapy of experimental pseudomonas infections with a nonreplicating genetically modified phage. Antimicrob Agents Chemother 48(10):3817–3822
Hall-Stoodley L, Costerton JW, Stoodley P (2004) Bacterial biofilms: from the natural environment to infectious diseases. Nat Rev Microbiol 2(2):95–108
Hanlon GW (2007) Bacteriophages: an appraisal of their role in the treatment of bacterial infections. Int J Antimicrob Agents 30(2):118–128
Hanlon GW, Denyer SP, Olliff CJ, Ibrahim LJ (2001) Reduction in exopolysaccharide viscosity as an aid to bacteriophage penetration through Pseudomonas aeruginosa biofilms. Appl Environ Microbiol 67(6):2746–2753
Harper DR, Parracho HM, Walker J, Sharp R, Hughes G, Werthén M, Lehman S, Morales S (2014) Bacteriophages biofilms. Antibiotics 3(3):270–284
Hermoso JA, García JL, García P (2007) Taking aim on bacterial pathogens: from phage therapy to enzybiotics. Curr Opin Microbiol 10(5):461–472
Herzberg M, Kang S, Elimelech M (2009) Role of extracellular polymeric substances (EPS) in biofouling of reverse osmosis membranes. Environ Sci Technol 43(12):4393–4398
Hibma AM, Jassim SA, Griffiths MW (1997) Infection and removal of L-forms of Listeria monocytogenes with bred bacteriophage. Int J Food Microbiol 34(3):197–207
Kiro R, Shitrit D, Qimron U (2014) Efficient engineering of a bacteriophage genome using the type IE CRISPR-Cas system. RNA Biol 11(1):42–44
Kocharunchitt C, Ross T, McNeil DL (2009) Use of bacteriophages as biocontrol agents to control Salmonella associated with seed sprouts. Int J Food Microbiol 128(3):453–459
Koskella B, Meaden S (2013) Understanding bacteriophage specificity in natural microbial communities. Viruses 5(3):806–823
Krogfelt KA, Poulsen LK, Molin S (1993) Identification of coccoid Escherichia coli BJ4 cells in the large intestine of streptomycin-treated mice. Infect Immun 61(12):5029–5034
Kutter E (2005) Phage therapy: bacteriophages as natural, self-limiting antibiotics. Textb Nat Med 1:1147–1161
Kutter E, De Vos D, Gvasalia G, Alavidze Z, Gogokhia L, Kuhl S, Abedon ST (2010) Phage therapy in clinical practice: treatment of human infections. Curr Pharm Biotechnol 11(1):69–86
Labrie SJ, Samson JE, Moineau S (2010) Bacteriophage resistance mechanisms. Nat Rev Microbiol 8(5):317–327
Lajoie CA, Layton AC, Gregory IR, Sayler GS, Taylor DE, Meyers AJ (2000) Zoogleal clusters and sludge dewatering potential in an industrial activated-sludge wastewater treatment plant. Water Environ Res 72(1):56–64
Le-Clech P, Chen V, Fane TA (2006) Fouling in membrane bioreactors used in wastewater treatment. J Membr Sci 284(1):17–53
Leiman PG, Chipman PR, Kostyuchenko VA, Mesyanzhinov VV, Rossmann MG (2004) Three-dimensional rearrangement of proteins in the tail of bacteriophage T4 on infection of its host. Cell 118(4):419–429
Letarov AV, Golomidova AK, Tarasyan KK (2010) Ecological basis for rational phage therapy. Acta Nat 2(1):60
Lidmar J, Mirny L, Nelson DR (2003) Virus shapes and buckling transitions in spherical shells. Phys Rev E 68(5):051910
Lin TY, Lo YH, Tseng PW, Chang SF, Lin YT, Chen TS (2012) A T3 and T7 recombinant phage acquires efficient adsorption and a broader host range. PLoS ONE 7(2):e30954
Liu M, Deora R, Doulatov SR, Gingery M, Eiserling FA, Preston A, Maskell DJ, Simons RW, Cotter PA, Parkhill J, Miller JF (2002) Reverse transcriptase-mediated tropism switching in Bordetella bacteriophage. Science 295(5562):2091–2094
Lodish H, Berk A, Zipursky SL, Matsudaira P, Baltimore D, Darnell J (2000) Section 6.3, viruses: structure, function, and uses. In: Molecular cell biology, 4th edn. New York
Loiselle M, Anderson KW (2003) The use of cellulase in inhibiting biofilm formation from organisms commonly found on medical implants. Biofouling 19(2):77–85
Lu TK, Collins JJ (2007) Dispersing biofilms with engineered enzymatic bacteriophage. Proc Natl Acad Sci 104(27):11197–11202
Lu TK, Collins JJ (2009) Engineered bacteriophage targeting gene networks as adjuvants for antibiotic therapy. Proc Natl Acad Sci 106(12):4629–4634
Mahichi F, Synnott AJ, Yamamichi K, Osada T, Tanji Y (2009) Site-specific recombination of T2 phage using IP008 long tail fiber genes provides a targeted method for expanding host range while retaining lytic activity. FEMS Microbiol Lett 295(2):211–217
Maiques E, Úbeda C, Tormo MÁ, Ferrer MD, Lasa Í, Novick RP, Penadés JR (2007) Role of staphylococcal phage and SaPI integrase in intra-and interspecies SaPI transfer. J Bacteriol 189(15):5608–5616
Matsuda T, Freeman TA, Hilbert DW, Duff M, Fuortes M, Stapleton PP, Daly JM (2005) Lysis-deficient bacteriophage therapy decreases endotoxin and inflammatory mediator release and improves survival in a murine peritonitis model. Surgery 137(6):639–646
Merril CR, Biswas B, Carlton R, Jensen NC, Creed GJ, Zullo S, Adhya S (1996) Long-circulating bacteriophage as antibacterial agents. Proc Natl Acad Sci 93(8):3188–3192
Merril CR, Scholl D, Adhya SL (2003) The prospect for bacteriophage therapy in Western medicine. Nat Rev Drug Discov 2(6):489–497
Modi SR, Collins JJ, Relman DA (2014) Antibiotics and the gut microbiota. J Clin Invest 124(10):4212–4218
Motlagh AM, Goel R (2014) Sustainability of activated sludge processes. Water reclamation and sustainability. Elsevier Science Ltd, Waltham, pp 391–414
Motlagh AM, Pant S, Gruden C (2013) The impact of cell metabolic activity on biofilm formation and flux decline during cross-flow filtration of ultrafiltration membranes. Desalination 316:85–90
Motlagh AM, Bhattacharjee AS, Goel R (2015) Microbiological study of bacteriophage induction in the presence of chemical stress factors in enhanced biological phosphorus removal (EBPR). Water Res 81:1–14
Musk J, Dinty J, Hergenrother PJ (2006) Chemical countermeasures for the control of bacterial biofilms: effective compounds and promising targets. Curr Med Chem 13(18):2163–2177
Nelson DC, Schmelcher M, Rodriguez-Rubio L, Klumpp J, Pritchard DG, Dong S, Donovan DM (2012) Endolysins as antimicrobials. Adv Virus Res 83:299–365
Nobrega FL, Costa AR, Kluskens LD, Azeredo J (2015) Revisiting phage therapy: new applications for old resources. Trends Microbiol 23(4):185–191
Orlova EV (2012) Bacteriophages and their structural organisation. In: Kurtboke I (ed) Bacteriophages. InTech, Rijeka, pp 3–30
O’Shea YA, Boyd EF (2002) Mobilization of the Vibrio pathogenicity island between Vibrio cholerae isolates mediated by CP-T1 generalized transduction. FEMS Microbiol Lett 214(2):153–157
Percival SL, Hill KE, Williams DW, Hooper SJ, Thomas DW, Costerton JW (2012) A review of the scientific evidence for biofilms in wounds. Wound Repair Regen 20(5):647–657
Poulsen LK, Licht TR, Rang C, Krogfelt KA, Molin S (1995) Physiological state of Escherichia coli BJ4 growing in the large intestines of streptomycin-treated mice. J Bacteriol 177(20):5840–5845
Rapson ME, Burden FA, Glancy LP, Hodgson DA, Mann NH (2003) Bacteriophages useful for therapy and prophylaxis of bacterial infections. Patent WO03080823
Ryan EM, Alkawareek MY, Donnelly RF, Gilmore BF (2012) Synergistic phage-antibiotic combinations for the control of Escherichia coli biofilms in vitro. FEMS Immunol Med Microbiol 65(2):395–398
Sanin F, Vesilind P (1994) Effect of centrifugation on the removal of extracellular polymers and physical properties of activated sludge. Water Sci Technol 30(8):117–127
Schmelcher M, Donovan DM, Loessner MJ (2012) Bacteriophage endolysins as novel antimicrobials. Future Microbiol 7(10):1147–1171
Scholl D, Adhya S, Merril C (2005) Escherichia coli K1’s capsule is a barrier to bacteriophage T7. Appl Environ Microbiol 71(8):4872–4874
Sidhu SS (2001) Engineering M13 for phage display. Biomol Eng 18(2):57–63
Sillankorva S, Oliveira R, Vieira MJ, Sutherland I, Azeredo J (2004) Bacteriophage Φ S1 infection of Pseudomonas fluorescens planktonic cells versus biofilms. Biofouling 20(3):133–138
Sillankorva S, Neubauer P, Azeredo J (2010) Phage control of dual species biofilms of Pseudomonas fluorescens and Staphylococcus lentus. Biofouling 26(5):567–575
Soni KA, Nannapaneni R (2010) Removal of Listeria monocytogenes biofilms with bacteriophage P100®. J Food Prot 73(8):1519–1524
Srey S, Jahid IK, Ha SD (2013) Biofilm formation in food industries: a food safety concern. Food Control 31(2):572–585
Sulakvelidze A (2011) Bacteriophage: a new journal for the most ubiquitous organisms on Earth. Bacteriophage 1(1):1–2
Taylor EN, Webster TJ (2009) The use of superparamagnetic nanoparticles for prosthetic biofilm prevention. Int J Nanomed 4:145
Vitiello CL, Merril CR, Adhya S (2005) An amino acid substitution in a capsid protein enhances phage survival in mouse circulatory system more than a 1000-fold. Virus Res 114(1):101–103
Westwater C, Kasman LM, Schofield DA, Werner PA, Dolan JW, Schmidt MG, Norris JS (2003) Use of genetically engineered phage to deliver antimicrobial agents to bacteria: an alternative therapy for treatment of bacterial infections. Antimicrob Agents Chemother 47(4):1301–1307
Withey S, Cartmell E, Avery LM, Stephenson T (2005) Bacteriophages—potential for application in wastewater treatment processes. Sci Total Environ 339(1):1–18
Wittebole X, De Roock S, Opal SM (2014) A historical overview of bacteriophage therapy as an alternative to antibiotics for the treatment of bacterial pathogens. Virulence 5(1):226–235
Wu H, Moser C, Wang HZ, Høiby N, Song ZJ (2015) Strategies for combating bacterial biofilm infections. Int J Oral Sci 7(1):1–7
Xiong Y, Liu Y (2010) Biological control of microbial attachment: a promising alternative for mitigating membrane biofouling. Appl Microbiol Biotechnol 86(3):825–837
Yan J, Mao J, Xie J (2014) Bacteriophage polysaccharide depolymerases and biomedical applications. BioDrugs 28(3):265–274
Yoichi M, Abe M, Miyanaga K, Unno H, Tanji Y (2005) Alteration of tail fiber protein gp38 enables T2 phage to infect Escherichia coli O157: H7. J Biotechnol 115(1):101–107
Yosef I, Manor M, Kiro R, Qimron U (2015) Temperate and lytic bacteriophages programmed to sensitize and kill antibiotic-resistant bacteria. In: Proceedings of the national academy of sciences, 201500107
Zaky A, Escobar I, Motlagh AM, Gruden C (2012) Determining the influence of active cells and conditioning layer on early stage biofilm formation using cellulose acetate ultrafiltration membranes. Desalination 286:296–303
Acknowledgments
We greatly appreciate the time reviewers have spent on this manuscript to provide their useful comments. This research was partially supported by National Science Foundation Grant #1055786. The views and rationale expressed in this manuscript are those of the authors and do not necessarily represent the funding agency.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Motlagh, A.M., Bhattacharjee, A.S. & Goel, R. Biofilm control with natural and genetically-modified phages. World J Microbiol Biotechnol 32, 67 (2016). https://doi.org/10.1007/s11274-016-2009-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11274-016-2009-4