Abstract
Gastrointestinal infection due to intestinal parasites is an enormous health problem in developing countries and its reliable diagnosis is demanding. Therefore, this study aimed at evaluating a commercially available immunochromatographic assay (ICA) for the detection of cryptosporidia, Giardia duodenalis, and Entamoeba histolytica/dispar for its usefulness in the Greater Cairo Region, Egypt. Stool samples of 104 patients who presented between October 2012 and March 2013 with gastrointestinal symptoms or for the exclusion of parasites at Kasr-Al-Ainy University Medical School were examined by light microscopy of wet mounts and the triple ICA. Microscopy revealed in 20 % of the patients [95 % confidence interval (CI), 13.5–29.0 %] parasites with Hymenolepis nana, E. histolytica/dispar and Blastocystis hominis being the most frequent ones, but was not able to detect G. duodenalis and cryptosporidia, whereas ICA was positive in 21 % (95 % CI, 14.3–30.0 %) and detected E. histolytica/dispar in 12.5 % (95 % CI, 7.3–20.4 %), cryptosporidia in 6.7 % (95 % CI, 3.1–13.5 %) and G. duodenalis in 15.4 % (95 % CI, 9.6–23.6 %) of the patients. Detection of one or more pathogens was associated with access to water retrieved from a well or pump (p = 0.01). Patients between 20 and 29 years of age (p = 0.08) and patients with symptoms of 5 days or longer (p = 0.07) tended to have a higher risk to be infected than patients of other age groups or with shorter-lasting symptoms. In conclusion, the ICA was easy to perform and timesaving. Importantly, it enabled the detection of cryptosporidia, which cannot be found microscopically in unstained smears, demonstrated a higher sensitivity for the detection of G. duodenalis than microscopy, and was more specific for distinguishing E. histolytica/dispar from apathogenic amoeba.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diarrheal diseases are among the leading infectious causes of morbidity and mortality in developing countries, especially in malnourished children, in patients with chronic diseases and in immunocompromized patients, e.g., suffering from HIV-infection or cancer (Abdel-Hafeez et al. 2012; Antonios et al. 2010; Baiomy et al. 2010; Curtale et al. 1998; El-Helaly et al. 2012; El-Mohammady et al. 2012; El-Naggar et al. 2006; Hassanein et al. 2012). Parasites must be distinguished as causative agents of diarrhea from viruses or bacteria because of possible chronic and extraintestinal manifestations in protozoal infections and different treatment requirements.
Several epidemiological factors, i.e., poor personal hygiene due to low educational level, overcrowding leading to collapsing infrastructure especially regarding water supply, as well as tropical climate promote diarrheal diseases (Alyousefi et al. 2011; Mahmud et al. 1995; Stauffer et al. 2006; Zaglool et al. 2011) and are present in the Greater Cairo Region in Egypt with approximately 17 Million inhabitants. Giardia duodenalis, cryptosporidia (primarily Cryptosporidium parvum and C. hominis), and Entamoeba histolytica are among the most important and prevalent intestinal protozoa in resource-limited countries (Pawlowski et al. 2009).
Light microscopy of stool sediments is the most frequently used diagnostic technique in resource-poor settings for the laboratory diagnosis of protozoal infections, however, it is labor-intensive, time-consuming, and requires experienced laboratory staff. Furthermore, cryptosporidia are missed by light microscopy of wet mounts and their detection generally requires the use of staining techniques, e.g., acid-fast Ziehl–Neelsen staining (Current and Garcia 1991). To overcome these obstacles, new technologies have been developed that rely on the detection of parasitic antigens, e.g., by enzyme-linked immunosorbent assays (ELISAs), or of parasitic DNA by PCR. Both methods have been shown to be more sensitive than light microscopy for the detection of intestinal protozoa (den Hartoq et al. 2013; Selim et al. 2009; Stark et al. 2010). An Egyptian study performed in Cairo and the Nile Delta between 2005 and 2007 applied ELISA technique for the detection of bacterial, viral and parasitic pathogens in 2112 diarrhoeic children below 5 years of age (El-Mohammady et al. 2012). G. duodenalis and Cryptosporidium spp. were the only parasites detected (7.0 and 5.0 %, respectively). Furthermore, Gaafar (2011) compared an ELISA detecting E. histolytica/dispar, G. duodenalis, and Cryptosporidium spp. with microscopy in 100 stool samples from patients in Alexandria, Egypt, between April and October 2011. In that study, the ELISA and microscopy did not differ significantly regarding the detection of the three parasites. Other parasites detected were Blastocystis hominis (1 %) and Cyclospora cayetanensis (1 %).
The main disadvantages of ELISAs and PCR, however, are their costs and the requirement of additional equipment, e.g., ELISA reader or PCR machine. Immunochromatographic assays (ICAs) may constitute an interesting alternative. They also detect antigens but are easy to perform independently of further equipment (Garcia and Garcia 2006; Costache et al. 2009). ICAs for the detection of G. duodenalis and C. parvum have been evaluated previously in Egypt with inconsistent results (Abdel Hameed et al. 2008; El-Hamshary et al. 2008; Antonios et al. 2010).
Recently, a novel assay has been licensed that simultaneously detects G. duodenalis, E. histolytica/dispar, and cryptosporidia. An evaluation of this assay in Zaragoza, Spain, in comparison with microscopy and PCR revealed acceptable sensitivities and specificities for G. duodenalis and cryptosporidia and slightly inferior results for E. histolytica/dispar (Goñi et al. 2012). The present study was carried out to evaluate for the first time the triple ICA for its benefit in diagnostic parasitology in Egypt.
Materials and methods
Study site and study population
This observational cross-sectional study included all patients who presented between October 2012 and March 2013 with gastrointestinal symptoms, e.g., diarrhea, abdominal pain or discomfort, indigestion, flatulence, or unspecific symptoms, at Kasr-Al-Ainy University Hospital, Greater Cairo Region, Egypt, and who attended the outpatient laboratory for the exclusion of intestinal parasites and agreed to participate. The patients were residents of all parts of Cairo or the surrounding rural areas. A questionnaire regarding demographic and social data, symptoms, and the source of drinking water was filled out for each patient.
Laboratory investigations
Stool investigations including microscopy and ICA were performed at the German Embassy Clinic, Cairo. Each patient delivered one stool sample to the laboratory in a clean plastic container. Consistency, color, presence of blood and/or mucus, undigested food particles or adult parasites were recorded for all specimens.
Direct wet smears were performed: one with saline and, in the case of stool samples with blood and/or mucus, a second one with iodine. Stool samples were concentrated by using the Paraprep S-kit (DiaMondial DML9000, Vienna, Austria) which was performed as follows: 0.5 g feces were mixed with formalin and ethyl acetate and left for 24 h to soften and ensure the bactericidal action of formalin. After 1 min centrifugation at 1500 rpm, each sample was examined microscopically with and without iodine by at least two independent professionals trained in stool diagnostics. In case of mismatching findings, a third examination was added. After microscopy all samples were kept frozen at −20 °C for subsequent antigen detection by ICT.
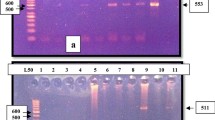
The triple ICA (RIDA ® QUICK Cryptosporidium/Giardia/Entamoeba Combi, R-Biopharm, Darmstadt, Germany) was performed according to the manufacturer’s instructions. Briefly, all reagents were brought to room temperature (20–25 °C). Fifty mg of stool per sample were mixed in a test tube with 1 ml of diluent and then left to settle for 3 min. Four drops of the clear supernatant were added to the round opening of the cassette. The results were read after another 10 min. The results for the three parasites tested appeared as three bands with different colors (green, E. histolytica/dispar; red, G. duodenalis; blue, cryptosporidia). Independently, the appearance of a crimson red control band was an indicator of the validity of the test. The color intensity of each test band may vary depending on the quantity of the antigen. According to the manufacturer, the sensitivity of this assay compared with light microscopy is 83.0 % (cryptosporidia), 91.9 % (G. duodenalis), and 84.8 % (E. histolytica/dispar), its specificity is 93.3 % (cryptosporidia), 99.5 % (G. duodenalis), and 87.4 % (E. histolytica/dispar).
Statistical analysis
The questionnaire data, results of microscopic examination of fecal specimens and the results of the ICA were analyzed in STATA version 10.0 for windows. Bivariable analysis was performed to explore associations between patients’ characteristics and prevalence of infection. Odds ratios and 95 % confidence intervals were computed. Pearson’s Chi-square test was performed for comparing proportions. p values <0.05 were considered significant.
Ethics statement
All patients and in case of minors, the legal guardians, were thoroughly informed about the study and gave their written informed consent. The study was reviewed and approved by the Ethical Committee of Kasr Al-Ainy, Medical School.
Results
Epidemiological and clinical characteristics of the study population
One hundred and four patients presenting at Kasr-Al-Ainy University Medical School with gastrointestinal symptoms suggestive of gastrointestinal parasites could be included in the study. Demographic data, clinical characteristics and symptoms are presented in Tables 1 and 2.
Results of stool investigations
By light microscopy, 24 parasitic pathogens were detected in 21 (20 %; 95 % CI, 13.5–29.0 %) of the stool specimens including one multiple infection, while 83 specimens (80 %; 95 % CI, 71.0–86.5 %) were negative (Table 3). Notably, G. duodenalis was not detected by this method in any of the samples. Thirteen samples (12.5 %; 95 % CI, 7.3–20.4 %) were positive for non-pathogenic Entamoeba coli. Multiple infections were rare with the exception of one stool specimen, which contained oocysts of Isospora belli and C. cayetanensis as well as cysts of E. histolytica/dispar, and B. hominis.
By ICA, 22 (21 %; 95 % CI, 14.3–30.0 %) of stool specimens were positive for G. duodenalis, E. histolytica/dispar, or cryptosporidia whereas 82 (79 %; 95 % CI, 70.0–85.7 %) samples yielded negative results (Table 4). Thirteen specimens (12.5 %; 95 % CI, 7.3–20.4 %) were positive for E. histolytica/dispar while eight were positive with microscopy (8 %; 95 % CI, 3.7–14.7 %; p = 0.001); notably, four of these eight samples were negative by ICA, while four were positive in both methods. In addition, cryptosporidia were found in samples of seven individuals (6.7 %; 95 % CI, 3.1–13.5 %; Table 4). Of note, the ICA revealed 16 (15.4 %; 95 % CI, 9.6–23.6 %) microscopically negative G. duodenalis infections.
ICA and microscopy together allowed identifying 34 patients with parasitic infections (33 %; 95 % CI, 24.4–42.2 %; Table 5) excluding individuals with only non-pathogenic E. coli. Most patients presented with mild symptoms. Severe clinical symptoms were present in only one HIV-positive patient infected with I. belli, C. cayetanensis, G. duodenalis, and cryptosporidia, and in another patient infected with C. philippinensis, a possible life-threatening infection typically associated with enteropathy and weight loss. Interestingly, 10 out of 16 patients with G. duodenalis did not report considerable gastrointestinal symptoms (Table 4); stool samples had mainly been admitted to exclude intestinal parasites.
Factors associated with the presence of gastrointestinal pathogens
We tested the patients’ data for association with the presence of at least one gastrointestinal pathogen (either detected by microscopy or ICA or both). Detection of one or more pathogens in patients was significantly associated with their access to water retrieved from a well or pump (OR 4.17; CI 1.34–13.02) compared to patients with access to tap water. Individuals between 20 and 29 years old tended to have a higher risk (p = 0.08) of being infected than those of the other age groups (Table 5). Although not being significant, there also was a tendency of being infected when the symptoms lasted for 5 days or longer (p = 0.07). No association was seen for abdominal pain, sex, profession, or area of residence.
Discussion
By light microscopy, we detected parasites in 20 % of 104 patients including one multiple infection with four different species. The most frequent parasites detected were H. nana followed by E. histolytica/dispar and B. hominis. Badawy et al. (2012) also detected parasites in 20.6 % of 150 stool specimens from diarrheic Egyptian military personnel but found mostly C. parvum (14 %), which could not be detected by us using light microscopy, followed by E. histolytica (5.3 %), Strongyloides stercoralis (1.3 %), and G. duodenalis in 0.7 %. El-Kadi et al. (2006), however, found intestinal parasites in 67.1 % of 210 symptomatic patients from Cairo. The difference to our data could be due to their study period of 1 year whereas our study was carried out in the cold season when infections are less frequent. The most prevalent protozoal pathogens were E. histolytica/dispar in 16.2 % (9.1 % confirmed by ELISA) followed by G. duodenalis (14.8 %) and B. hominis (9.5 %). The differences between our findings and the two other studies regarding the most frequent parasites may be due to demographic differences in the study populations.
By ICA, cryptosporidia were found in seven patients (6.7 %; 95 % CI, 3.1–13.5 %). These cases would have remained undetected without the application of ICA. The previous data regarding the value of ICAs for the detection of cryptosporidia has been inconsistent. Abdel Hameed et al. (2008) described a sensitivity of 91.6 % for the RIDA quick Cryptosporidium/Giardia ICA regarding the detection of cryptosporidia compared to 83.3 % for microscopy. A poorer sensitivity (13.6 %), however, of the same product has been shown in comparison with PCR (Helmy et al. 2014). Similarly, Antonios et al. (2010) reported a sensitivity of 13.3 % for the Remel Xpect Giardia/Cryptosporidium ICA.
In our study, the ICA but not microscopy detected 16 cases of giardiasis, which confirmed a poor sensitivity of microscopy for the detection of G. duodenalis in endemic areas where chronic and repeated infections occur frequently (Ignatius et al. 2014). In contrast, Abdel Hameed et al. (2008) demonstrated a sensitivity of 91.6 % for the RIDA quick ICA for the detection of G. duodenalis compared with microscopy. Elsafi et al. (2013) found 20 cases (13.5 %) of G. duodenalis infections out of 148 samples.
Interestingly, 9 of 16 patients with G. duodenalis did not report abdominal pain or diarrhea. Such mild or rather asymptomatic infections are often seen in giardiasis patients from endemic areas and may be the result of host adaptation, which depends on the nutritional and immunological status of the infected individual (Sahagún et al. 2008).
We detected E. histolytica/dispar by microscopy in 7.7 % and by ICA in 12.5 % of the specimens. Notably, four of the eight cases detected by microscopy were negative by ICA. Since three of these four specimens contained E. coli cysts, these may have been misinterpreted as E. histolytica/dispar; thus, the ICA may be more specific than light microscopy in the diagnosis of amoebiasis. Moreover, nine of the 13 positive cases by ICA were negative by microscopy, which may be due to a higher sensitivity of the ICA as shown previously (Bhaskar et al. 1996). Unfortunately, the ICAs are still not suited to distinguish between the pathogenic E. histolytica and the non-pathogenic species E. dispar or E. moshkovskii.
Notably, the ICA was easy to perform and timesaving, which confirms previous findings (Helmy et al. 2014). As neither advanced technology nor highly trained personnel are necessary, ICAs may be a useful method for field studies (El-Moamly and El-Sweify 2012).
Together, ICA and microscopy identified 34 patients with intestinal parasites; however, the majority of them presented only with mild abdominal symptoms. This is plausible in the case of E. histolytica/dispar since neither ICA nor microscopy can differentiate between E. histolytica and the non-pathogenic species E. dispar or E. moshkovski. One of the patients (No. 85) may have been infected with E. histolytica because he reported bloody stools (Table 5). Two patients presented with severe clinical symptoms. One of these was HIV-positive and infected by four detected parasites, which all could have contributed to the clinical findings, i.e., I. belli, C. cayetanensis, G. duodenalis, and cryptosporidia. The second patient was a 16-year old woman infected with Capillaria philippinensis who lived originally in Sharona village, a rural area in Upper Egypt, and probably got infected by processing or consumption of raw or undercooked fresh water fish. In contrast, a retired 58-year-old male resident of a rural district in Cairo who also presented with C. philppinensis infection did not report severe abdominal symptoms. Intestinal capillariasis has been described in Egypt before (Youssef et al. 1989).
The use of water obtained from a well or pump was significantly associated with parasitic infection. These water sources may by origin be contaminated with fecal material due to lack of proper sanitation and infrastructure, or they may become contaminated by storage in dirty containers (El-Sherbini and Abosdera 2013). Furthermore, patients with symptoms lasting 5 days or longer tend to have a higher risk of being infected with parasites than patients reporting a shorter course of disease. This is plausible since many parasites including the ones primarily detected by our study, i.e., G. duodenalis and Entamoeba spp., may cause chronic intestinal infections. There also was a strong trend towards patients at the age of 20–29 years harboring more likely intestinal parasites than patients belonging to other age groups although it must be assumed that the prevalence of parasites in the study area is generally higher in children (who were not included in the present study) than in adults (Fawzi et al. 2004). In agreement with this finding, adults of 20–29 years have recently been identified also among 2732 expatriate workers in Saudi Arabia as the age group with the highest prevalence of intestinal parasites (Taha et al. 2013). The underlying reasons remain elusive and should be investigated in future studies.
Conclusion
In conclusion, ICAs as the one evaluated in the present study are easy to perform, timesaving, and may complement standard diagnostic methods in parasitology also in the context of field studies. The costs (approximately 10$ per sample) of this triple ICA may be compensated by its higher sensitivity for the detection of G. duodenalis as well as its high sensitivity and specificity for E. histolytica/dispar. Furthermore, the examination of additional Ziehl–Neelsen stained slides for the detection of cryptosporidia can be obviated if an ICA is used.
References
Abdel Hameed DM, Elwakil HS, Ahmed MA (2008) A single-step immunochromatographic lateral-flow assay for detection of Giardia lamblia and Cryptosporidium parvum antigens in human fecal samples. J Egypt Soc Parasitol 38:797–804
Abdel-Hafeez EH, Ahmad AK, Ali BA, Moslam FA (2012) Opportunistic parasites among immunosuppressed children in Minia district, Egypt. Korean J Parasitol 50:57–62
Alyousefi NA, Mahdy MAK, Mahmud R, Lim YAL (2011) Factors associated with high prevalence of intestinal protozoan infections among patients in Sana’a city Yemen. PLoS One 6:1–7
Antonios SN, Tolba OA, Orthman AA, Saad MA (2010) A preliminary study on the prevalence of parasitic infections in immunocompromised children. J Egypt Soc Parasitol 40:617–630
Badawy AA, Gneidy MR, Ghoniemy AE (2012) Acute diarrhea among military recruits. J Egypt Soc Parasitol 42:309–320
Baiomy AM, Mohamed KA, Ghannam MA, Shahat SA, Al-Saadawy AS (2010) Opportunistic parasitic infections among immunocompromised Egyptian patients. J Egypt Soc Parasitol 40:97–808
Bhaskar S, Singh S, Sharma M (1996) A single-step immunochromatographic test for the detection of Entamoeba histolytica antigen in stool samples. J Immunol Methods 196:193–198
Costache CA, Calosi IA, Colosi HA (2009) Immunochromatography versus microscopy for the identification of Giardia lamblia and Cryptosporidium parvum in human feces. Scient Parasit 1–2:26–31
Current WL, Garcia LS (1991) Cryptosporidiosis. Clin Microbiol Rev 4:325–358
Curtale F, Nabil M, El Wakeel A, Shamy MY (1998) Anaemia and intestinal parasitic infections among school age children in Behera Governorate, Egypt. Behera Survey Team. J Trop Pediatr 44:323–328
Den Hartoq J, Rosenbaum L, Wood Z, Burt D Jr, Petri WA (2013) Diagnosis of multiple enteric protozoan infections by enzyme-linked immunosorbent assay in the Guatemalan highlands. Am J Trop Med Hyg 88:167–171
El-Hamshary EM, El-Sayed HF, Hussein EM, Rayan HZ, Soliman RH (2008) Comparison of polymerase chain reaction, immunochromatographic assay and staining techniques in diagnosis of Cryptosporidiosis. PUJ 1:77–86
El-Helaly NA, Mona MA, Samar SA (2012) Detection of Cryptosporidium infection among children with diarrhoea. N Y Sci J 5:68–76
El-Kadi MA, Ahmad OD, Shoukry NM (2006) Patients with gastrointestinal complaints due to enteric parasites, with reference to Entamoeba histolytica/dispar as detected by ELISA E. histolytica adhesion in stool. J Egypt Soc Parasitol 36:53–64
El-Moamly AAR, El-Sweify MA (2012) ImmunoCard STAT! cartridge antigen detection assay compared to microplate enzyme immunoassay and modified Kinyoun’s acid-fast staining technique for detection of Cryptosporidium in fecal specimens. Parasitol Res 110:1037–1041
El-Mohammady H, Mansour A, Shaheen HI, Henien NH, Motawea MS, Rafaat I, Moustafa M, Adip-Messih I, Seben PJ, Young SYN et al (2012) Increase in the detection rate of viral and parasitic enteric pathogens among Egyptian children with acute diarrhoea. J Infect Dev Ctries 6:774–781
El-Naggar SM, El-Bahy MM, Abd Elaziz J, El-Dardiry MA (2006) Detection of protozoal parasites in the stools of diarrhoeic patients using different techniques. J Egypt Soc Parasitol 36:7–22
Elsafi SH, Al-Maqati TN, Hussein MI, Adam AA, Abu Hassan MM, Al Zahrani EM (2013) Comparison of microscopy, rapid immunoassay, and molecular techniques for the detection of Giardia lamblia and Cryptosporidium parvum. Parasitol Res 112:1641–1646
El-Sherbini GT, Abosdera MM (2013) Risk factors associated with intestinal parasitic infections among children. J Egypt Soc Parasitol 43:287–294
Fawzi M, El-Sahn AA, Ibrahim HF, Shehata AI (2004) Vegetable-transmitted parasites among inhabitants of El-Prince, Alexandria and its relation to housewives’ knowledge and practices. J Egypt Public Health Assoc 79:13–29
Gaafar RM (2011) Evaluation of enzyme immunoassay techniques for diagnosis of the most common intestinal protozoa in fecal samples. Int J Infect Dis 15:541–544
Garcia LS, Garcia JP (2006) Detection of Giardia lamblia antigens in human fecal specimens by a solid-phase qualitative immunochromatographic assay. J Clin Microbiol 44:4587–4588
Goñi P, Martin B, Villacampa M, Garcia A, Seral C, Castillo FJ, Clavel A (2012) Evaluation of an immunochromatographic dip strip test for simultaneous detection of Cryptosporidium spp., Giardia duodenalis, and Entamoeba histolytica antigens in human faecal samples. Eur J Clin Microbiol Infect Dis 31:2077–2082
Hassanein SM, Abd-El-Latif MM, Hassanin OM, Abd-El-Latif LM, Ramadan NI (2012) Cryptosporidium gastroenteritis in Egyptian children with acute lymphoblastic leukemia: magnitude of the problem. Infection 40:279–284
Helmy YA, Krücken J, Nöckler K, von Samson-Himmelstjerna G, Zessin K-H (2014) Comparison between two commercially available serological tests and polymerase chain reaction in the diagnosis of Cryptosporidium in animals and diarrhoeic children. Parasitol Res 113:211–216
Ignatius R, Gahutu JB, Klotz C, Musemakweri A, Aebischer T, Mockenhaupt FP (2014) Detection of Giardia duodenalis assemblage A and B by immunochromatography in stoolsamples from Rwandan children. CMI 20:O783–O785
Mahmud AM, Chappell C, Hossain MM, Habib M, Dupont HL (1995) Risk factors for development of first symptomatic Giardia infection among infants of birth cohort in rural Egypt. Am J Trop Med Hyg 53:84–88
Pawlowski SW, Warren CA, Guerrant R (2009) Diagnosis and treatment of acute or persistent diarrhea. Gastroenterol 136:1874–1886
Sahagún J, Clavel A, Goñi P, Llorente MT, Castillo FJ, Capilla S, Arias A, Gómez-Lus R (2008) Correlation between the presence of symptoms and the Giardia duodenalis genotype. Eur J Clin Microbiol Infect Dis 27:81–83
Selim S, Nassef N, Sharaf S, Badra G, Abdel Atty D (2009) Copro-antigen detection versus direct methods for the diagnosis of Giardia lamblia in patients from the National Liver Institute. J Egypt Soc Parasitol 39:575–583
Stark D, Al-Qassab E, Barratt JLN, Stanley K, Roberts T, Marriott D, Harkness J, Ellis JT (2010) Evaluation of multiplex tandem real-time PCR for detection of Cryptosporidium spp., Dientamoeba fragilis, Entamoeba histolytica, and Giardia intestinalis in clinical stool samples. J Clin Microbiol 49:257–262
Stauffer W, Abd-Alla M, Ravdin JI (2006) Prevalence and incidence of Entamoeba histolytica infection in South-Africa and Egypt. Arch Med Res 37:266–269
Taha HA, Soliman MI, Banjar SAN (2013) Intestinal parasitic infections among expatriate workers in Al-Madina Al-Munawarah, Kingdom of Saudi Arabia. Trop Biomed 30:78–88
Youssef FG, Mikhail EM, Mansour NS (1989) Intestinal capillariasis in Egypt, a case report. Am J Trop Med Hyg 40:195–196
Zaglool DA, Khodiari YA, Orthman RAM, Farooq MU (2011) Prevalence of intestinal parasites and bacteria among food handlers in a tertiary care hospital. Niger Med J 52:266–270
Acknowledgments
We are grateful to Renate Culley, Danijela Meister-Babić, Claudia Schubert and Antje Vincentz for their experienced help in microscopic diagnosis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Banisch, D.M., El-Badry, A., Klinnert, J.V. et al. Simultaneous detection of Entamoeba histolytica/dispar, Giardia duodenalis and cryptosporidia by immunochromatographic assay in stool samples from patients living in the Greater Cairo Region, Egypt. World J Microbiol Biotechnol 31, 1251–1258 (2015). https://doi.org/10.1007/s11274-015-1875-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11274-015-1875-5