Abstract
The present study assessed the presence of ESBL-producing Escherichia coli in livestock farm wastewater (LFWW), hospital wastewater (HWW), and natural water sources (NWS) from five districts (Prayagraj, Mirzapur, Varanasi, Sonbhadra, and Jaunpur) of eastern parts of Uttar Pradesh, India (n = 134). Phenotypic ESBL production among cefotaxime-resistant E. coli isolates (91.29%, 283/310) was significantly different (p < 0.05) in the samples from Jaunpur and Sonbhadra, but not from Prayagraj, Mirzapur and Varanasi (p > 0.05). The MIC of cefotaxime and ceftazidime against these isolates were in the ranges of 64–512 µg/mL and 16–512 µg/mL, respectively. Genotypically, 38.51% (109/283) of the isolates harbored at least one or more plasmid-mediated ESBL-genes, of which, blaCTX-M-gr-1 was the predominant (90.82%, 99/109), followed by blaTEM (73.39%, 80/109). A non-significant difference (p > 0.05) was observed in the occurrence of ESBL genes among the phenotypically positive isolates of different sampling places. Multidrug-resistant (MDR) traits were observed in 105 (96.33%) of 109 tested isolates with a MAR index ranging from 0.31 to 1.0. Absolute resistance (100%) was evident against azithromycin for all isolates recovered from Varanasi, Prayagraj, and Sonbhadra irrespective of their sources. The majority of the isolates belonged to commensal phylogroup A (40.37%, 44/109) and B1 (27.44%, 31/109), while only two isolates recovered from HWW sources of Varanasi belonged to the extra-intestinal pathogenic phylogroup B2. These findings suggested that the wastewater and natural water sources of eastern parts of Uttar Pradesh, India, harbored a high magnitude of MDR-ESBL E. coli with the potential to be transmitted to humans and animals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The worldwide emergence and spread of antimicrobial resistance (AMR) as a “silent pandemic” may result in up to 10 million AMR-related mortality by 2050 (Bengtsson-Palme et al., 2018; WHO, 2017, 2019). Often the environment acts as a reservoir and “mixing vessel” of AMR pathogens that harbor AMR genes (ARGs) in their plasmids, integrons, transposons, or insertion sequences which can be transferred to other pathogenic and commensal microbes via horizontal gene transfer (Raimondi et al., 2019; Ramos et al., 2020). Among the environmental components, the wastewater originating from various sources like hospitals, livestock and poultry farms, and slaughterhouses is a major source of antibiotic-resistant bacteria and resistant genes. These can enter natural water sources like rivers, lakes, and groundwater through the discharge of treated or untreated wastewater (Adelowo et al., 2018). This creates high selection pressure zones within the recipient aquatic environment which helps in further dissemination of AMR organisms with novel resistant mechanisms through recreational water activities or consumption of contaminated water or food (Amos et al., 2014; Alouache et al., 2014; Chukwu et al., 2023).
Escherichia coli is a common inhabitant of the gastrointestinal tract of humans and animals, and it has been used as a sentinel organism for antimicrobial surveillance studies (Nyirabahizi et al., 2020). Antibiotic resistance (AR) in E. coli to β-lactams (viz. penicillin, cephalosporins, carbapenems, etc.) is mainly mediated by the production of β-lactamase enzymes (Hussain et al., 2021; Sta Ana et al., 2021). Among the β-lactamases, the extended-spectrum beta-lactamases (ESBLs) are of special importance which confer resistance to all β-lactams except carbapenems and cephamycin and is inhibited by β-lactamase inhibitors like clavulanic acid, sulbactam, or tazobactam (Paterson & Bonomo, 2005). The worldwide dissemination of ESBL-producing E. coli in clinical infections, foods of livestock and plant origin, aquatic and soil ecosystems, and wastewater from industry, slaughterhouses, hospitals, livestock farms, and sewage treatment plants is a matter of serious concern for public health and environment ecosystem (Conte et al., 2017; Girijan & Pillai, 2023; Gregova et al., 2021; Korzeniewska et al., 2013; Marathe et al., 2019). Many clinically significant ESBL-producing E. coli harbor plasmid-mediated blaTEM, blaSHV, blaCTX-M, and blaOXA gene variants (Shaikh et al., 2015; Liakopoulos et al., 2016; Hooban et al., 2020). Infections caused by multi-drug resistant (MDR) ESBL-producing E. coli is challenging to treat and their occurrences in the environment possess a significant public health risk (Kasanga et al., 2023).
In the context of the “One Health” approach, the detection and characterization of the ESBL-producing bacteria at the human-animal-environment interface, taking E. coli as the indicator organism, can add substantial knowledge to safeguard public health. This will also preserve the effectiveness and use of antibiotics. In the existing literature, there is a lack of information related to the detection and characterization of ESBL-producing bacteria at the human-animal-environment interface, particularly from developing countries like India. Hence, the present study was undertaken to detect the occurrence of ESBL-producing E. coli in wastewater from hospitals and livestock farms as well as the natural water sources (viz. rivers, canals, reservoirs, etc.) from five districts of the eastern parts of Uttar Pradesh, India, based on their proximity and constant interaction. The recovered E. coli isolates were further tested by employing molecular tools for the detection of ESBL genes, phenotypic co-occurrence of ESBL-production and multi-drug resistance (MDR) traits, and phylogenetic typing. This study aims to provide an insight into the perpetuation of ESBL-producing E. coli in environmental sources in parts of Eastern Uttar Pradesh, India, which will add information on AMR surveillance on “One Health” perspective.
2 Materials and Methods
2.1 Study Area and Collection of Samples
The study was carried out in the Department of Veterinary Public Health and Epidemiology at the Faculty of Veterinary and Animal Sciences, Rajiv Gandhi South Campus, Banaras Hindu University, Mirzapur, Uttar Pradesh, India, from January 2022 to March 2023. A total of 134 sites comprising 58 livestock farms, 43 hospitals, and 33 natural water sources were included for sample collection by simple random sampling method (95% confidence interval, ± 5% precision applied to determine the number of sampling sites with respect to places and sources) from five districts (Prayagraj (25.43°N latitude and 81.84°E longitude), Mirzapur (25.12°N latitude and 82.56°E longitude), Varanasi (25.31°N latitude and 82.97°E longitude), Sonbhadra (24.53°N latitude and 83.03°E longitude), and Jaunpur (25.75°N latitude and 82.68°E longitude)) of eastern Uttar Pradesh, India, which are located within a 100-km radius around the place of work (Mirzapur) (Fig. 1, Supplementary Table 1). In each sampling event, approximately 500 mL of pooled samples (livestock farm wastewater (LFWW), hospital wastewater (HWW) as well as water samples from natural water sources (NWS)) was collected from three different spots of each site by grab sampling method. The water sample was collected in sterile wide-mouthed glass bottles preferably in the morning hours (Baird et al., 2017), transported to the laboratory in a cold chain (4 ± 1℃), and processed within 6 h.
Map revealing places and sources of sample collection from five districts (1, Prayagraj; 2, Mirzapur; 3, Varanasi; 4, Sonbhadra; 5, Jaunpur) of the eastern part of Uttar Pradesh, India. Livestock farm wastewater (LFWW) sources are represented by brown dots, hospital wastewater (HWW) sources as red dots, and natural water sources (NWS) as blue dots, respectively
2.2 Isolation of Cefotaxime-Resistant E. coli
The water sample was thoroughly mixed by inverting the bottle several times and 1 mL of the sample was enriched in 9 mL of McConkey broth and incubated overnight at 37℃. After incubation, a loopful of the inoculum was streaked on Eosin Methylene Blue agar plates supplemented with 4 µg/mL of cefotaxime and incubated overnight at 37℃. The colonies exhibiting a greenish metallic sheen with dark purple background were presumptively identified as Escherichiae. The phenotypic appearance of colonies may not reflect the genetic variability among different strains in the same sample, for which additional testing like antibiotic resistance profiling, serogrouping, plasmid profiling, or DNA fingerprinting is required. Also, it is difficult to ascertain the number of colonies to be picked from each plate without knowledge of the actual number of strains on the plate (Singer et al., 2000). Earlier study on the isolation of E. coli from cellulitis lesions in broilers processed three colonies from each McConkey plates with an assumption that there would be three or fewer strains per lesions and equal growth of different strains on the plates (Singer et al., 2000). Hence, at least three colonies were randomly selected from different streaking lines of the plates and characterized by biochemical tests and molecular tools for the identification of Escherichia coli. After molecular confirmation, these were further processed to determine the ESBL production by phenotypic and genotypic methods, antimicrobial resistant profile, and phylogenetic grouping.
2.3 Molecular Confirmation of E. coli by PCR Assay
The cefotaxime-resistant E. coli isolates were confirmed by polymerase chain reaction (PCR) assay by amplifying the housekeeping uidA gene as described previously (Alsanjary & Sheet, 2022; McDaniels et al., 1996). In brief, the genomic DNA was extracted by boiling lysis method (Mahmud et al., 2020). The PCR assay was carried out in a 25-µL reaction mixture comprising of 12.5 µl 2 × master mix (Promega Corporations, USA), 1 µL (10 pmol/µL) each of forward (5′-CCAAAAGCCAGACAGAGT-3′) and reverse (5′-GCACAGCACATCCCCAAAGAG-3′) primers (synthesized at Eurofins Genomics Pvt. Ltd., Bengaluru), 7.5 µL NFW (Promega Corporations, USA), and 3 µl DNA template. The PCR products were electrophoresed on 1.5% agarose gel (Genei, Bangalore) with a 100-bp DNA ladder (BR Biochem, India) and visualized in a gel documentation system (Biorad, USA).
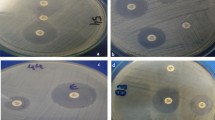
2.4 Phenotypic Identification of ESBL Production by DDST, CDM, and MIC
All the PCR-confirmed cefotaxime-resistant E. coli isolates were screened for phenotypic production of ESBL enzymes by double disk synergy test (DDST) and combination disk method (CDM) using Mueller Hinton Agar (MHA) and the results were interpreted as per Clinical and Laboratory Standards Institute (CLSI) guidelines (CLSI, 2018). For DDST, ceftazidime (CAZ 30 µg) and/or cefotaxime (CTX 30 µg) disks and amoxicillin/clavulanate (20 µg/10 µg) disks (Himedia, India) were placed at a distance of 30 mm on sterile MHA plates swabbed with the standard inoculum (0.5 McFarland) of the test isolates. The plates were incubated overnight at 37℃. Extension of the zone of inhibition (ZOI) towards amoxicillin/clavulanate disk was measured to interpret ESBL producer (Drieux et al., 2008; Sageerabanoo et al., 2015). For CDM, ceftazidime (CAZ 30 µg) and/or cefotaxime (CTX 30 µg) disks along with ceftazidime-clavulanate (30 µg/10 µg) and/or cefotaxime-clavulanate (30 µg/10 µg) disk (Himedia, India) respectively were placed at a distance of 30 mm on sterile MHA plates swabbed with the standard inoculum (0.5 McFarland) of the test isolates. The plates were incubated overnight at 37℃. An increase in the ZOI ≥ 5 mm around the disk with the antibiotic-clavulanic acid combination compared to the antibiotic disk alone was considered positive for ESBL production (CLSI, 2018).
The minimum inhibitory concentration (MIC) of antibiotics (ceftazidime and cefotaxime alone and their combination with clavulanic acid) was determined by microbroth dilution assay in cation-adjusted Mueller Hinton broth (CAMHB) using ceftazidime (0.25–512 µg/mL), ceftazidime plus clavulanic acid (0.25/4–512/4 µg/mL), and cefotaxime (0.25–512 µg/mL), cefotaxime plus clavulanic acid (0.25/4–512/4 µg/mL) in 96-well microtiter plates (Corning, USA) (CLSI, 2018). The plates were incubated for 18–24 h at 37℃. A ≥ 3 twofold concentration decrease in a MIC for either antibiotic tested in combination with clavulanic acid vs the MIC of the antibiotics when tested alone was considered phenotypically positive for ESBL production. As quality control strains, Klebsiella pneumoniae ATCC 700603 and E. coli ATCC 25922 were used.
2.5 Molecular Detection of Plasmid-Mediated ESBL Genes Among the Phenotypically ESBL-Positive Isolates
Plasmid DNA was extracted from all the phenotypically positive ESBL-producing E. coli isolates (overnight grown fresh cultures) employing the alkaline lysis method (Sambrook & Russell, 2001) and subjected to molecular detection of plasmid-mediated ESBL-producing genes by multiplex-PCR (mPCR) assay as described previously (Dallenne et al., 2010) using primers (synthesized at Eurofins Genomics Pvt. Ltd., Bengaluru, India) presented in Supplementary Table 2. The mPCR assay was carried out in two sets—the first one amplified the target regions of blaTEM, blaSHV, and blaOXA-1-like genes, and the second one amplified that of blaCTX-M gr-1, blaCTX-M gr-2, blaCTX-M gr-8, blaCTX-M gr-9, and blaCTX-M gr-25 genes in separate 25-µL reaction mixtures comprising of 12.5 µl 2 × master mix (Promega Corporations, USA), 1 pmol/µL of respective primers, 2 µl template DNA, and NFW to adjust the volume. The PCR product was electrophoresed and visualized as described earlier.
2.6 Antibiotic Sensitivity Test and MAR Index
All the genotypically positive ESBL-producing isolates were tested for their sensitivity to other antibiotics by the Kirby-Bauer disk diffusion method. Briefly, the sterile MHA plates were swabbed with the standard inoculum (0.5 McFarland) of the test isolates. The antibiotics used in this test belonged to nine different classes, namely penicillin: ampicillin (AMP 30 µg), piperacillin (PI 100 µg), and piperacillin-tazobactam (PIT 100 µg/10 µg); cephalosporins: cefepime (CPM 30 µg) and cefoxitin (CX 30 µg); aminoglycosides: gentamicin (GEN 10 µg) and kanamycin (K 30 µg); macrolides: azithromycin (AZM 15 µg); tetracyclines: doxycycline (DO 30 µg); folate pathway antagonists: co-trimoxazole (COT 1.25/23.75 µg); quinolones and fluoroquinolones: ciprofloxacin (CIP 5 µg) and nalidixic acid (NA 30 µg); phenicols: chloramphenicol (C 30 µg); and nitrofurans: nitrofurantoin (NIT 300 µg). The results were interpreted according to CLSI breakpoints (CLSI, 2018). Isolates that displayed resistance to three or more antibiotic classes were considered multi-drug resistant (MDR) (Magiorakos et al., 2012). The multiple antibiotic resistance (MAR) index was determined as the ratio of the number of antibiotics to which the isolate was resistant to the total number of antibiotics used in the test (Krumperman, 1983).
2.7 Phylogenetic Typing of ESBL-Producing E. coli Isolates
All the genotypically positive ESBL-producing E. coli isolates were subjected to phylogenetic typing to determine the distribution of phylogroups (A, B1, B2, C, D, E, and F) using PCR assay as described previously (Clermont et al., 2013).
2.8 Statistical Analysis
The difference in phenotypic ESBL production among cefotaxime-resistant E. coli isolates recovered from various sources and places were compared by the Pearson chi-square test. The presence of ESBL genes among phenotypically ESBL-producing E. coli isolates concerning their source and place of sample collection was compared by Pearson chi-square (when n > 3) and Fisher’s exact test (when n < 3) using IBM SPSS version 23. The level of significance was determined at a 95% confidence interval, where p < 0.05 was considered significantly different and p > 0.05 was non-significantly different.
3 Results
3.1 Phenotypic Identification of ESBL-Producing E. coli
In this study, a total of 310 cefotaxime-resistant E. coli isolates were recovered from various environmental sources. Their distribution across places and sources is presented in Table 1 and Fig. 2. All the isolates were biochemically and molecularly confirmed as E. coli by PCR assay targeting species-specific uidA gene which yielded a 623-bp product upon electrophoresis.
Of the cefotaxime-resistant E. coli isolates, 91.29% (283/310) were observed to be phenotypically positive for ESBL production based on the DDST and CDM results (Table 1, Supplementary Fig. 1 and 2). A highly significant difference (p < 0.01) was observed in the occurrence of phenotypic ESBL production among the cefotaxime-resistant E. coli isolates recovered from different places (districts) and sources (LFWW, HWS, and NWS) of the Eastern Uttar Pradesh (Table 2 and 3). After Bonferroni correction, a significant (p < 0.01) number of cefotaxime-resistant E. coli isolates exhibiting phenotypic ESBL production and those not exhibiting ESBL production were obtained from LFWW and NWS sources than HWW sources (p > 0.05). Further, phenotypic ESBL expression among cefotaxime-resistant E. coli isolates recovered from Jaunpur and Sonbhadra districts differed significantly (p < 0.05), although a similar significant difference was not evident (p > 0.05) among cefotaxime-resistant E. coli isolates recovered from Prayagraj, Mirzapur, and Varanasi.
The MIC of cefotaxime and ceftazidime for the phenotypically ESBL-positive E. coli isolates was found to be in the range of 64–512 µg/mL and 16–512 µg/mL, respectively (Table 1). A ≥ 3 twofold decrease in the MIC of antibiotics was observed when tested in combination with clavulanic acid (at a fixed concentration of 4 µg/mL). MIC values above 256 µg/mL for cefotaxime and ceftazidime were observed in 83.45% and 53.11% of E. coli isolates respectively. The highest MIC value for the antibiotics (512 µg/mL) was observed in isolates primarily recovered from LFWW sources.
3.2 Molecular Detection of ESBL-Producing Genes
One or more plasmid-mediated ESBL genes among phenotypically positive ESBL-producing E. coli isolates (n = 283) were detected in 38.51% (109/283) of the isolates by multiplex PCR assay (Table 4). Among the isolates (n = 109), the blaCTX-M-gr-1 gene was detected predominantly (90.82%), followed by blaTEM (73.39%), blaOXA-1 like (11%), and blaSHV (2.75%) genes. Co-occurrence of blaCTX-M-gr-1 and blaTEM genes was observed in 51.37% (56/109) of isolates (Table 4). ESBL genes could not be detected in 61.48% (174/283) of phenotypically positive ESBL-producing E. coli isolates. Also, a significant difference (p < 0.05) was observed in the presence of blaCTX-M-gr-1, blaTEM, and blaOXA-1-like genes among phenotypically positive ESBL-producing E. coli isolates and their sources, except for blaSHV gene (p > 0.05) (Table 5).
Phenotypically positive ESBL-producing E. coli isolates recovered from LFWW sources revealed the distribution of blaCTX-M-gr-1 gene to the tune of 11.11% (2/18), 10.86% (5/46), 21.42% (6/28), 34.48% (10/29), and 57.14% (12/21) from Mirzapur, Varanasi, Prayagraj, Jaunpur, and Sonbhadra, respectively (Table 4). Besides, blaCTX-M-gr-1 gene was predominantly detected in all the ESBL-producing isolates (19/19) recovered from HWW sources from Mirzapur, whereas its detection was between 26 and 36% in ESBL-producing isolates recovered from the same source (HWW) of four other places. While ESBL-producing isolates were recovered from NWS, the blaCTX-M-gr-1 gene could be detected up to 69.23% (9/13) in isolates recovered from Varanasi, followed by that of Prayagraj (50%), Jaunpur (33.33%), Sonbhadra (33.33%), and Mirzapur (23.07%), respectively (Table 4).
The presence of the blaTEM gene was predominantly observed in isolates recovered from LFWW sources of the Sonbhadra district (52.38%, 11/21) and HWW sources of the Varanasi district (48%, 12/25). The distribution of blaOXA-1-like genes was limited to the isolates recovered from HWW sources from Mirzapur (15.78%, 3/19) and Jaunpur (22.22%, 2/9), although HWW (15%, 3/20), NWS (25%, 3/12), and LFWW (3.5%, 1/28) sources also revealed blaOXA-1-like genes from Prayagraj district. Moreover, the blaSHV genes were detected in only three isolates recovered from LFWW sources of Sonbhadra (Table 4). Overall, a significant difference (p > 0.05) was not observed concerning the occurrence of ESBL genes among the phenotypically positive isolates of different sampling places (Table 6).
3.3 Antibiotic Sensitivity Test of ESBL-Producing E. coli Isolates
Antibiotic sensitivity test of ESBL-producing E. coli isolates (n = 109) revealed an MDR trait in 91.41% (104/109) of isolates; i.e., these isolates were resistant to three or more than three classes of antibiotics (Table 7, Supplementary Table 3). Overall antibiotic susceptibility pattern revealed all isolates (100%) to be resistant to ampicillin, piperacillin, cefotaxime, and ceftazidime irrespective of their place and source of collection. Apart from the β-lactam antibiotics, a 100% resistance was observed towards azithromycin by all isolates recovered from Varanasi, Prayagraj, and Sonbhadra irrespective of their sources of collection. Among the isolates recovered from LFWW sources from various places under this study area, a lower resistance was observed towards doxycycline (0–25%, except those from Varanasi—60%), chloramphenicol (0–46.67%), and gentamicin (0–45.45%). Resistance to doxycycline was observed to be the least (0–33.33%) among the isolates recovered from HWW sources across all places that were sampled.
Based on the resistance profile of the isolates, a varied distribution of resistant patterns was observed. Resistance patterns of AMP-PI-PIT-K-CPM-CX-AZM-CIP-NA-CTX-CAZ and AMP-PI-PIT-K-CPM-AZM-CIP-NA-CTX-CAZ were the most frequently observed in 7 (6.54%) and 5 (4.67%) of the isolates respectively. The MAR index of all the isolates (100%) was found to be higher than 0.2 (0.31 to 1). An isolate (JC8a), recovered from an LFWW source of Sonbhadra, revealed a MAR index of 1.0 (resistant to all the antibiotics tested). Similarly, two isolates, viz., JC4a and VH9c which were recovered from an LFWW sample from Jaunpur and an HWW sample from Varanasi, respectively, had a MAR index of 0.94 (resistance to 15 antibiotics) (Supplementary Table 3).
3.4 Phylogenetic Typing of the Isolates
Phylogenetic groups identified among the ESBL-producing E. coli isolates (n = 109) included phylogroup A (40.37%, 44/109), B1 (27.44%, 31/109), B2 (1.83%, 2/109), C (11.93%, 13/109), D (4.59%, 5/109), E (2.75%, 3/109), and F (0.92%, 1/109). However, the remaining 10 isolates could not be typed by the current method (Table 8).
4 Discussion
This is the first report on the detection of MDR ESBL-producing E. coli in wastewater from livestock farms, hospitals, and the natural water sources of the surrounding areas of five selected districts of the Eastern parts of Uttar Pradesh, India. In this study, about 91.29% of the recovered cefotaxime-resistant E. coli isolates were observed to be phenotypically positive for ESBL production. The use of a selective medium and picking more than one colony might be a probable reason for the higher isolation rate in this study, which is supported by similar observations by other researchers (Diwan et al., 2012; Samanta et al., 2018). This high detection rate of cephalosporin-resistant E. coli from wastewater and water sources is a major threat to the environment (Korzeniewska et al., 2013). A similarly high prevalence of cefotaxime resistance (100%) was observed among ESBL-producing E. coli (24/38) recovered from wastewater from a University Health Centre facility in Nigeria (Adekanmbi et al., 2020). In India, wastewater treatment and management are not commonly practiced in many hospital settings (Diwan et al., 2012). The situation is even worse when it comes to animal husbandry practices. Also, β-lactams are the most frequently prescribed antibiotics in India (Van Boeckel et al., 2014). Most of the veterinary antibiotics (up to 90%) could not be assimilated in animals and excreted unchanged via urine or feces (Kemper, 2008), which might contaminate the nearby surface or groundwater. It has been reported that the use of third- and fourth-generation cephalosporins in livestock 12 months before the analysis may ensure at least four times more ESBL-positive E. coli isolates (Snow et al., 2012). Even the use of antibiotics other than β-lactams has been known to select ESBL phenotypes in E. coli isolates recovered from cattle farms (Schmid et al., 2013). All these probable factors in addition to antibiotic over-prescription, irrational use, over-the-counter availability, incomplete dose regimen, lack of sanitation (Kalasseril et al., 2020; Manyi-Loh et al., 2018), and overcrowding with a floating population at the pilgrimage sites (e.g. Prayagraj and Varanasi) of eastern Uttar Pradesh region might have induced a high selection pressure in the environment leading to higher detection of MDR bacteria.
The predominant ESBL genes detected among ESBL-producing E. coli isolates from LFWW sources were blaCTX-M-gr-1 (87.50%, 35/40) and blaTEM (72.50%, 29/40) across all places under the study area. Similar observations have been reported in an earlier study from Thailand, wherein 60.2% of ESBL-producing E. coli isolates that were recovered from dairy farms wastewater revealed the presence of blaCTX-M and blaTEM genes (Saekhow & Sriphannam, 2021). Besides, the blaCTX-M gene was found to be the major genetic determinant in ESBL-producing E. coli isolated from floor swabs and drinking water of a pig pen in West Bengal, India (Samanta et al., 2018). In India, most of the studies on the detection of ESBL-producing E. coli have focused on foods of animal origin, clinical samples, and fecal samples (Ghatak et al., 2013; Pruthvishree et al., 2017; Rawat et al., 2018), Without proper drainage and disposal facilities, the surrounding environment of farms may get repeated contamination with farm wastewater which may increase the concentration and survivability of ESBL-producing E. coli (Hartmann et al., 2012). Further dissemination from those areas is possible via rainwater run-offs to nearby rivers or natural water sources which may increase the chance of human acquisition via drinking, bathing, or other recreational purposes (Runcharoen et al., 2017; Xi et al., 2009).
The majority of the ESBL-producing E. coli isolates recovered from HWW samples across different places in this study were observed to harbor blaCTX-M-gr-1, blaTEM, and blaOXA-1-like genes. A similar outcome was observed earlier (Girijan & Pillai, 2023), where blaCTX-M was the most prevalent (32.8%) ESBL-encoding gene followed by blaTEM (15.6%) among the E. coli isolates from clinical environments. A diverse distribution of ESBL genes (blaCTX-M-15, blaTEM-1 and blaSHV-12, blaOXA-10) among E. coli isolates from HWW samples have been observed in various studies from India (Diwan et al., 2012; Marathe et al., 2019; Bardhan et al., 2020; Kalasseril et al., 2020). Several studies have shown the emergence of blaCTX-M coded ESBLs (mainly the blaCTX-M-15 which is placed under the blaCTX-M-gr-1) as the most significant ESBL-encoding genes among cephalosporin-resistant E. coli in recent years from clinical isolates and hospital settings worldwide because of the overuse of cephalosporins (Cantón et al., 2012; D’Andrea et al., 2013; Ibrahimagić et al., 2015). The TEM-β-lactamases were also observed to be one of the most clinically relevant to the β-lactamase family (Girijan & Pillai, 2023). It has been reported that the frequency of ESBL producer and number of β-lactamase genes are directly associated with the “hospital size,” wherein bigger hospitals were found to contribute a greater bacterial load to their surrounding environment in comparison to smaller ones (Girijan & Pillai, 2023; Lamba et al., 2017). This was also evident in our study that the presence of high-end tertiary care hospitals in Prayagraj, Varanasi, and Mirzapur contributed a higher frequency of ESBL-producing E. coli and ESBL genes in comparison to that of Sonbhadra and Jaunpur. The continuous exposure of β-lactam antibiotics may be responsible for creating selective pressure for blaTEM and blaCTX-M genes, as a substantial increase in the prescription of certain β-lactam antibiotics like ceftriaxone, meropenem, and ertapenem has been linked to increased ARB in hospital effluent (Diwan et al., 2010; Hsu et al., 2010).
Screening of NWS samples from various places under this study has revealed the presence of blaCTX-M-gr-1 and blaTEM as the major genetic determinants of ESBL genes among the recovered isolates. Similar findings were observed in a study on river water samples collected from five states (Goa, Bihar, Karnataka, Tamil Nadu, and Telangana) of India (Akiba et al., 2016); Yamuna River water collected from Delhi (Bajaj et al., 2015), and Ganga river water collected across the state of Uttar Pradesh, India (Chaturvedi et al., 2020). Our study also supports the observations on the worldwide occurrence of CTX-M and TEM as the dominant ESBL-gene family in E. coli isolates from surface water (Blaak et al., 2015), steam and well water (Caltagirone et al., 2017), river water (Chen et al., 2010; Kamruzzaman et al., 2013; Kim et al., 2008; Wambugu et al., 2018; Zarfel et al., 2017), and recreational water (Jørgensen et al., 2017). Although large water bodies may dilute the concentration of antibiotics and metabolites, repeated exposure even in sub-therapeutic concentration provides an ideal milieu for the transfer of resistance among the bacterial community (Watkinson et al., 2009).
The current study detected mostly the blaTEM and blaCTX-M genes among the isolates in comparison to blaOXA-1-like or blaSHV genes. Similar observations have been noted in earlier studies where TEM, OXA, and CTX-M genes were predominantly detected from isolates recovered from wastewater samples (Kutilova et al., 2021; Liedhegner et al., 2022; Nzima et al., 2020). It may be hypothesized that bla genes have exchanged and recombined in the aqueous environment giving rise to predominantly blaTEM-and blaCTX-M genotypes. The bla gene transfer theory may explain the possible difference between clinical bla gene types and those obtained from the environment (Chen et al., 2010). Wastewater from animal farms may contain ESBL-E. coli with completely different resistant genetic determinants, but reports are scarce in this regard for discussion. The TEM enzyme has been known to be an ESBL-producing enzyme for a long time, but the significance of CTX-M enzymes has been recently known (Paterson & Bonomo, 2005). In our study, negative PCR results of ESBL genes were observed in 61.48% of phenotypically ESBL-positive isolates. This probably indicated the presence of other non-detectable ESBL-producing genes (like GES, PER, VEB, SFO, TLA) in the same molecular class A or novel ESBL genes or substantial genetic variations. A similar outcome was observed in a study on the blaVIM carbapenemase gene among phenotypic carbapenem-resistant E. coli isolates recovered from calves in India (Murugan et al., 2019). Additionally, the β-lactamase gene selected and amplified in this case represents a selected cellular mechanism of drug resistance deployed by prokaryotes. Moreover, the involvement of other mechanisms in drug resistance cannot be ruled out. In the absence of sequence data, it was not possible to interpret whether a lower detection rate of ESBL genes was due to a problem in the confirmation method or the presence of another enzyme not detected by the current PCR-based method (Bell et al., 2007).
In this study, about 96.33% (105/109) of isolates exhibited an MDR pattern with a MAR index above 0.3. Similar findings were also obtained in a study from Ecuador where 98.3% of cefotaxime-resistant isolates from broiler farms were MDR (Vinueza-Burgos et al., 2019). The occurrence of MDR isolates in environmental sources is highly worrisome from a public health point of view. It has been reported that bacteria having a MAR index ≥ 0.2 originate from high-risk areas where several antibiotics are used (Afunwa et al., 2020; Sandhu, 2016). Most of the isolates exhibited high resistance to the quinolone class of antibiotics. Co-existence of cephalosporin and quinolone resistance phenotypes and genotypes among Enterobacteriaceae was previously reported (Galvin et al., 2010; Lavilla et al., 2008) as the plasmids carrying blaCTX-M and qnr genes occur as self-transmissible plasmids carrying transportable ARGs (Diwan et al., 2012). Isolates from HWW samples of Prayagraj, Varanasi, and Mirzapur were observed to be resistant to Kanamycin, which may be due to their higher indiscriminate use in those areas. It is noteworthy and a matter of concern that 42–93% of E. coli isolates recovered from HWW sources of Prayagraj, Varanasi, and Mirzapur was resistant to cefepime, a fourth-generation cephalosporin. One of the interesting findings is 96% (104/109) of the ESBL-producing E. coli isolates were co-resistant to azithromycin irrespective of the place or source of sample collection. It can be hypothesized that increased and indiscriminate use of azithromycin in the treatment of COVID-19 infection and other respiratory illnesses during the ongoing pandemic might have induced an extreme selection pressure on bacteria leading to their higher resistance to azithromycin. This is well supported by various studies wherein an increased use of azithromycin has led to bacterial resistance to this drug (Seabra et al., 2021; Silva Segundo et al., 2022; Sultana et al., 2020; Wu et al., 2020). Azithromycin has been increasingly and widely used in the management of COVID-19 (Ayerbe et al., 2022; Gyselinck et al., 2021). It was also observed that an increase in use of azithromycin (a macrolide) in COVID-19 patients had led to an increased resistance to erythromycin (another macrolide) in Staphylococcus aureus in Mexico (López-Jácome et al., 2022). Moreover, another study from Spain reported that 10 COVID-19 patients out of 48 (21%) admitted to ICU revealed azithromycin resistance strains of P. aeruginosa, E. faecium, H. influenza, and MRSA (Barrasa et al., 2020). Resistant determinants against aminoglycosides, tetracyclines, sulphonamides, and cephalosporins are often present on the same plasmid along with resistance to some heavy metals and toxic elements which might have aided in the co-occurrence of ESBL and MDR traits displayed by the isolates in our study. This will provide a suitable platform for the exchange of genetic material among the microbiota through horizontal gene transfer leading to the spread of MDR strains across the anthropogenic environment (Ibrahim et al., 2016; Chaturvedi et al., 2020). Comparison with other studies may not give the same resistant pattern, but studying resistance to different groups of antibiotics in a sentinel species like E. coli has indicated the presence of an antibiotic “resistome” among the environmental E. coli isolates.
The phylogroups result revealed that the majority of the isolates belonged to the commensal phylogroups A, B1, and C irrespective of sources or places of sampling. Only 2 isolates recovered from HWW sources of Varanasi belonged to the extra-intestinal virulence-associated phylogroup B2. It is documented that, human commensal strains belong mostly to phylogroups A and B1 (Stoppe et al., 2017) and strains isolated from animals fall under group B1 (Higgins et al., 2007). The presence of phylogroup A and B1 may result from anthropogenic activities (Escobar-Páramo et al., 2006; Hanna et al., 2020); this might be the explanation for the result observed in our study. It has been reported that E. coli with extended-spectrum cephalosporin resistance belonged predominantly to non-B2 groups, which was also well observed in our study. Extremely low abundances of phylogroup B2 were reported from Indian aquatic environments (Bajaj et al., 2015) and wastewater contaminated with human and animal waste in Spain (Garcia-Aljaro et al., 2009; Sabaté et al., 2008). Also, it was reported by several researchers that the pandemic ST131 clone of E. coli belonging to phylogroup B2 was often associated with CTX-M mediated ESBL phenotype (Dhanji et al. 2011; Bajaj et al., 2015), but other sequence types belonging to phylogroup B2 have been associated with less CTX-M production (Brisse et al., 2012). In our study, both the phylogroup B2 isolates carried only blaTEM as the major ESBL determinant. Although we could not perform the sequence typing analysis, it may be presumed that a lower prevalence of pathogenic phylogroup B2 in the environmental sources would have a less significant role in the transmission of the pandemic ST131 clones carrying CTX-M genes in those areas. Also, five isolates in this study were found to be grouped under the extra-intestinal pathogenic phylogroup D, with 80% of these harboring the blaCTX-M-gr-1 gene. A similar observation was reported for the E. coli isolates recovered from Yamuna river water in Delhi, India (Bajaj et al., 2015). The presence of the same phylogroups among the E. coli isolates recovered from various environmental sources of a particular area does not necessarily indicate a zoonotic transfer, but rather a common source of acquisition.
5 Conclusion
This study reports the presence of multi-drug resistant ESBL-producing E. coli isolates in wastewater from hospitals, livestock farms, and natural water samples collected from the eastern parts of Uttar Pradesh, India. This is the first research data on the molecular detection of ESBL-producing E. coli isolates involving the three types of environmental sources of the concerned study area. In this study, significant differences in the occurrence of phenotypic ESBL production among the cefotaxime-resistant E. coli isolates recovered from different places (districts) and sources (LFWW, HWS, and NWS) were observed. The blaCTX-M-gr-1 and blaTEM genes were found to be the predominant ESBL genotypes among the recovered isolates. Additionally, pathogenic phylogroups B2 and D were observed to a lesser extent, and a majority of the tested isolates belonged to the commensal phylogroups A, B1, and C. Moreover, the observation of a high degree of resistance to critically important antibiotics among the environmental E. coli isolates of the study area is a matter of serious concern to public health. Further, the use of molecular typing tools will aid in determining the origin and distribution of AMR organisms in a particular geographical area. Optimizing the use of antibiotics in clinical and animal husbandry practices, adopting effective wastewater treatment facilities and routine AMR surveillance among environmental isolates will help to protect public health to a great extent.
Data Availability
All data supporting the findings of this study are available within the paper and its supplementary files. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Adekanmbi, A. O., Akinpelu, M. O., Olaposi, A. V., & Oyelade, A. A. (2020). Diversity of Extended Spectrum Beta-lactamase (ESBL) genes in Escherichia coli isolated from wastewater generated by a Sick Bay located in a University Health Care Facility. Gene Reports, 20. https://doi.org/10.1016/j.genrep.2020.100738
Adelowo, O. O., Caucci, S., Banjo, O. A., Nnanna, O. C., Awotipe, E. O., Peters, F. B., et al. (2018). Extended spectrum beta-lactamase (ESBL)-producing bacteria isolated from hospital wastewaters, rivers and aquaculture sources in Nigeria. Environmental Science and Pollution Research, 25(3), 2744–2755. https://doi.org/10.1007/s11356-017-0686-7
Afunwa, R. A., Ezeanyinka, J., Afunwa, E. C., Udeh, A. S., Oli, A. N., & Unachukwu, M. (2020). Multiple antibiotic resistant index of gram-negative bacteria from bird droppings in two commercial poultries in Enugu. Nigeria. Open Journal of Medical Microbiology, 10(04), 171–181. https://doi.org/10.4236/ojmm.2020.104015
Akiba, M., Sekizuka, T., Yamashita, A., Kuroda, M., Fujii, Y., Murata, M., et al. (2016). Distribution and relationships of antimicrobial resistance determinants among extended-spectrum-cephalosporin-resistant or carbapenem-resistant Escherichia coli isolates from rivers and sewage treatment plants in India. Antimicrobial Agents and Chemotherapy, 60(5), 2972–2980. https://doi.org/10.1128/AAC.01950-15
Alouache, S., Estepa, V., Messai, Y., Ruiz, E., Torres, C., & Bakour, R. (2014). Characterization of ESBLs and associated quinolone resistance in escherichia coli and klebsiella pneumoniae isolates from an urban wastewater treatment plant in Algeria. Microbial Drug Resistance, 20(1), 30–38. https://doi.org/10.1089/mdr.2012.0264
Alsanjary, L. H., & Sheet, O. H. (2022). Molecular detection of uidA gene in Escherichia coli isolated from the dairy farms in Nineveh governorate, Iraq. Iraqi Journal of Veterinary Sciences, 36(3), 599–603. https://doi.org/10.33899/ijvs.2021.131046.1913
Amos, G. C. A., Hawkey, P. M., Gaze, W. H., & Wellington, E. M. (2014). Waste water effluent contributes to the dissemination of CTX-M-15 in the natural environment. Journal of Antimicrobial Chemotherapy, 69(7), 1785–1791. https://doi.org/10.1093/jac/dku079
Ayerbe, L., Risco-Risco, C., Forgnone, I., Pérez-Piñar, M., & Ayis, S. (2022). Azithromycin in patients with COVID-19: A systematic review and meta-analysis. Journal of Antimicrobial Chemotherapy, 77(2), 303–309. https://doi.org/10.1093/jac/dkab404
Baird, R. B., Eaton, A. D., & Rice, E. W. E. (2017). Part 9000 Microbiological Examination. Standard Methods for the Examination of Water and Wastewater (23rd ed., pp. 36–39). Washington D.C.: American Public Health Association, American Water Works Association, Water Environment Federation. https://doi.org/10.2105/SMWW.2882.184
Bajaj, P., Singh, N. S., Kanaujia, P. K., & Virdi, J. S. (2015). Distribution and molecular characterization of genes encoding CTX-M and AmpC β-lactamases in Escherichia coli isolated from an Indian urban aquatic environment. Science of the Total Environment, 505, 350–356. https://doi.org/10.1016/j.scitotenv.2014.09.084
Bardhan, T., Chakraborty, M., & Bhattacharjee, B. (2020). Prevalence of colistin-resistant carbapenem-hydrolyzing proteobacteria in hospital water bodies and out-falls of West Bengal, India. International Journal of Environmental Research and Public Health, 17(3), 1007. https://doi.org/10.3390/ijerph17031007
Barrasa, H., Rello, J., Tejada, S., Martín, A., Balziskueta, G., Vinuesa, C., et al. (2020). SARS-CoV-2 in Spanish intensive care units: Early experience with 15-day survival in Vitoria. Anaesthesia Critical Care and Pain Medicine, 39(5), 553–561. https://doi.org/10.1016/j.accpm.2020.04.001
Bell, J. M., Chitsaz, M., Turnidge, J. D., Barton, M., Walters, L. J., & Jones, R. N. (2007). Prevalence and significance of a negative extended-spectrum β-lactamase (ESBL) confirmation test result after a positive ESBL screening test result for isolates of Escherichia coli and Klebsiella pneumoniae: Results from the SENTRY asia-pacific surveillan. Journal of Clinical Microbiology, 45(5), 1478–1482. https://doi.org/10.1128/JCM.02470-06
Bengtsson-Palme, J., Kristiansson, E., & Larsson, D. G. J. (2018). Environmental factors influencing the development and spread of antibiotic resistance. FEMS Microbiology Reviews, 42(1), 68–80. https://doi.org/10.1093/femsre/fux053
Blaak, H., Lynch, G., Italiaander, R., Hamidjaja, R. A., Schets, F. M., & De Husman, A. M. R. (2015). Multidrug-resistant and extended spectrum beta-lactamase-producing escherichia coli in dutch surface water and wastewater. PLoS ONE, 10(6). https://doi.org/10.1371/journal.pone.0127752
Brisse, S., Diancourt, L., Laouénan, C., Vigan, M., Caro, V., Arlet, G., et al. (2012). Phylogenetic distribution of CTX-M- and non-extended-spectrum-β- lactamase-producing Escherichia coli isolates: Group B2 isolates, except clone ST131, rarely produce CTX-M enzymes. Journal of Clinical Microbiology, 50(9), 2974–2981. https://doi.org/10.1128/JCM.00919-12
Caltagirone, M., Nucleo, E., Spalla, M., Zara, F., Novazzi, F., Marchetti, V. M., et al. (2017). Occurrence of extended spectrum β-lactamases, KPC-Type, and MCR-1.2-producing enterobacteriaceae from wells, river water, and wastewater treatment plants in Oltrepò Pavese area, Northern Italy. Frontiers in Microbiology, 8(NOV). https://doi.org/10.3389/fmicb.2017.02232
Cantón, R., González-Alba, J. M., & Galán, J. C. (2012). CTX-M enzymes: Origin and diffusion. Frontiers in Microbiology, 3(APR). https://doi.org/10.3389/fmicb.2012.00110
Chaturvedi, P., Chaurasia, D., Pandey, A., & Gupta, P. (2020). Co-occurrence of multidrug resistance, β-lactamase and plasmid mediated AmpC genes in bacteria isolated from river Ganga, northern India. Environmental Pollution, 267. https://doi.org/10.1016/j.envpol.2020.115502
Chen, H., Shu, W., Chang, X., Chen, J. A., Guo, Y., & Tan, Y. (2010). The profile of antibiotics resistance and integrons of extended-spectrum beta-lactamase producing thermotolerant coliforms isolated from the Yangtze River basin in Chongqing. Environmental Pollution, 158(7), 2459–2464. https://doi.org/10.1016/j.envpol.2010.03.023
Chukwu, K. B., Abafe, O. A., Amoako, D. G., Essack, S. Y., & Abia, A. L. K. (2023). Antibiotic, heavy metal, and biocide concentrations in a wastewater treatment plant and its receiving water body exceed PNEC limits: Potential for antimicrobial resistance selective pressure. Antibiotics, 12(7). https://doi.org/10.3390/antibiotics12071166
Clermont, O., Christenson, J. K., Denamur, E., & Gordon, D. M. (2013). The Clermont Escherichia coli phylo-typing method revisited: Improvement of specificity and detection of new phylo-groups. Environmental Microbiology Reports, 5(1), 58–65. https://doi.org/10.1111/1758-2229.12019
CLSI. (2018). Performance Standards for Antimicrobial Susceptibility Testing. CLSI supplement M100 (28th ed.). Wayne, PA: Clinical and Laboratory Standards Institute, Wayne, PA. Accessed 20 May 2023.
Conte, D., Palmeiro, J. K., da Silva Nogueira, K., de Lima, T. M. R., Cardoso, M. A., Pontarolo, R., et al. (2017). Characterization of CTX-M enzymes, quinolone resistance determinants, and antimicrobial residues from hospital sewage, wastewater treatment plant, and river water. Ecotoxicology and Environmental Safety, 136, 62–69. https://doi.org/10.1016/j.ecoenv.2016.10.031
D’Andrea, M. M., Arena, F., Pallecchi, L., & Rossolini, G. M. (2013). CTX-M-type β-lactamases: A successful story of antibiotic resistance. International Journal of Medical Microbiology, 303(6–7), 305–317. https://doi.org/10.1016/j.ijmm.2013.02.008
Dallenne, C., da Costa, A., Decré, D., Favier, C., & Arlet, G. (2010). Development of a set of multiplex PCR assays for the detection of genes encoding important β-lactamases in Enterobacteriaceae. Journal of Antimicrobial Chemotherapy, 65(3), 490–495. https://doi.org/10.1093/jac/dkp498
Dhanji, H., Doumith, M., Rooney, P. J., O’Leary, M. C., Loughrey, A. C., Hope, R., Woodford, N., & Livermore, D. M. (2011). Molecular epidemiology of fluoroquinolone-resistant ST131 Escherichia coli producing CTX-M extended-spectrum β-lactamases in nursing homes in Belfast, UK. Journal of Antimicrobial Chemotherapy, 66(2), 297–303. https://doi.org/10.1093/jac/dkq463
Diwan, V., Chandran, S. P., Tamhankar, A. J., Stålsby Lundborg, C., & Macaden, R. (2012). Identification of extended-spectrum β-lactamase and quinolone resistance genes in Escherichia coli isolated from hospital wastewater from central India. Journal of Antimicrobial Chemotherapy, 67(4), 857–859. https://doi.org/10.1093/jac/dkr564
Diwan, V., Tamhankar, A. J., Khandal, R. K., Sen, S., Aggarwal, M., Marothi, Y., et al. (2010). Antibiotics and antibiotic-resistant bacteria in waters associated with a hospital in Ujjain, India. BMC Public Health, 10. https://doi.org/10.1186/1471-2458-10-414
Drieux, L., Brossier, F., Sougakoff, W., & Jarlier, V. (2008). Phenotypic detection of extended-spectrum β-lactamase production in Enterobacteriaceae: Review and bench guide. Clinical Microbiology and Infection, 14(SUPPL. 1), 90–103. https://doi.org/10.1111/j.1469-0691.2007.01846.x
Escobar-Páramo, P., Le Menac’h, A., Le Gall, T., Amorin, C., Gouriou, S., Picard, B., et al. (2006). Identification of forces shaping the commensal Escherichia coli genetic structure by comparing animal and human isolates. Environmental Microbiology, 8(11), 1975–1984. https://doi.org/10.1111/j.1462-2920.2006.01077.x
Galvin, S., Boyle, F., Hickey, P., Vellinga, A., Morris, D., & Cormican, M. (2010). Enumeration and characterization of antimicrobial-resistant escherichia coli bacteria in effluent from municipal, hospital, and secondary treatment facility sources. Applied and Environmental Microbiology, 76(14), 4772–4779. http://aem.asm.org/cgi/reprint/76/14/4772%5Cnhttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed9&NEWS=N&AN=20525867.
Garcia-Aljaro, C., Moreno, E., Andreu, A., Prats, G., & Blanch, A. R. (2009). Phylogroups, virulence determinants and antimicrobial resistance in stx2 gene-carrying Escherichia coli isolated from aquatic environments. Research in Microbiology, 160(8), 585–591. https://doi.org/10.1016/j.resmic.2009.08.004
Ghatak, S., Singha, A., Sen, A., Guha, C., Ahuja, A., Bhattacharjee, U., et al. (2013). Detection of new delhi metallo-beta-lactamase and extended-spectrum beta-lactamase genes in escherichia coli isolated from mastitic milk samples. Transboundary and Emerging Diseases, 60(5), 385–389. https://doi.org/10.1111/tbed.12119
Girijan, S. K., & Pillai, D. (2023). Genetic diversity and prevalence of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in aquatic environments receiving untreated hospital effluents. Journal of Water and Health, 21(1), 66–80. https://doi.org/10.2166/wh.2022.194
Gregova, G., Kmet, V., & Szaboova, T. (2021). New insight on antibiotic resistance and virulence of escherichia coli from municipal and animal wastewater. Antibiotics, 10(9). https://doi.org/10.3390/antibiotics10091111
Gyselinck, I., Janssens, W., Verhamme, P., & Vos, R. (2021). Rationale for azithromycin in COVID-19: An overview of existing evidence. BMJ Open Respiratory Research, 8(1). https://doi.org/10.1136/bmjresp-2020-000806
Hanna, N., Purohit, M., Diwan, V., Chandran, S. P., Riggi, E., Parashar, V., et al. (2020). Monitoring of water quality, antibiotic residues, and antibiotic-resistant Escherichia coli in the Kshipra River in India over a 3-year period. International Journal of Environmental Research and Public Health, 17(21), 1–22. https://doi.org/10.3390/ijerph17217706
Hartmann, A., Locatelli, A., Amoureux, L., Depret, G., Jolivet, C., Gueneau, E., & Neuwirth, C. (2012). Occurrence of CTX-M producing Escherichia coli in soils, cattle, and farm environment in France (Burgundy region). Frontiers in Microbiology, 3(MAR). https://doi.org/10.3389/fmicb.2012.00083
Higgins, J., Hohn, C., Hornor, S., Frana, M., Denver, M., & Joerger, R. (2007). Genotyping of Escherichia coli from environmental and animal samples. Journal of Microbiological Methods, 70(2), 227–235. https://doi.org/10.1016/j.mimet.2007.04.009
Hooban, B., Joyce, A., Fitzhenry, K., Chique, C., & Morris, D. (2020). The role of the natural aquatic environment in the dissemination of extended spectrum beta-lactamase and carbapenemase encoding genes: A scoping review. Water Research, 180. https://doi.org/10.1016/j.watres.2020.115880
Hsu, L. Y., Tan, T. Y., Tam, V. H., Kwa, A., Fisher, D. A., Koh, T. H., et al. (2010). Surveillance and correlation of antibiotic prescription and resistance of gram-negative bacteria in Singaporean hospitals. Antimicrobial Agents and Chemotherapy, 54(3), 1173–1178. https://doi.org/10.1128/AAC.01076-09
Hussain, H. I., Aqib, A. I., Seleem, M. N., Shabbir, M. A., Hao, H., Iqbal, Z., et al. (2021). Genetic basis of molecular mechanisms in β-lactam resistant gram-negative bacteria. Microbial Pathogenesis, 158. https://doi.org/10.1016/j.micpath.2021.105040
Ibrahim, D. R., Dodd, C. E. R., Stekel, D. J., Ramsden, S. J., & Hobman, J. L. (2016). Multidrug resistant extended spectrum β-lactamase (ESBL)-producing Escherichia coli isolated from a dairy farm. FEMS Microbiology Ecology, 92(4), fiw013. https://doi.org/10.1093/femsec/fiw013
Ibrahimagić, A., Bedenić, B., Kamberović, F., & Uzunović, S. (2015). High prevalence of CTX-M-15 and first report of CTX-M-3, CTX-M-22, CTX-M-28 and plasmid-mediated AmpC beta-lactamase producing Enterobacteriaceae causing urinary tract infections in Bosnia and Herzegovina in hospital and community settings. Journal of Infection and Chemotherapy, 21(5), 363–369. https://doi.org/10.1016/j.jiac.2015.01.003
Jørgensen, S. B., Søraas, A. V., Arnesen, L. S., Leegaard, T. M., Sundsfjord, A., & Jenum, P. A. (2017). A comparison of extended spectrum β-lactamase producing Escherichia coli from clinical, recreational water and wastewater samples associated in time and location. PLoS ONE, 12(10). https://doi.org/10.1371/journal.pone.0186576
Kalasseril, S. G., Krishnan, R., Vattiringal, R. K., Paul, R., Mathew, P., & Pillai, D. (2020). Detection of New Delhi Metallo-β-lactamase 1 and cephalosporin resistance genes among carbapenem-resistant Enterobacteriaceae in water bodies adjacent to hospitals in India. Current Microbiology, 77(10), 2886–2895. https://doi.org/10.1007/s00284-020-02107-y
Kamruzzaman, M., Shoma, S., Naymul Bari, S. M. N., Ginn, A. N., Wiklendt, A. M., Partridge, S. R., et al. (2013). Genetic diversity and antibiotic resistance in Escherichia coli from environmental surface water in Dhaka City, Bangladesh. Diagnostic Microbiology and Infectious Disease, 76(2), 222–226. https://doi.org/10.1016/j.diagmicrobio.2013.02.016
Kasanga, M., Kwenda, G., Wu, J., Kasanga, M., Mwikisa, M. J., Chanda, R., et al. (2023). Antimicrobial resistance patterns and risk factors associated with ESBL-producing and MDR Escherichia coli in hospital and environmental settings in Lusaka, Zambia: Implications for One Health, Antimicrobial Stewardship and Surveillance Systems. Microorganisms, 11(8). https://doi.org/10.3390/microorganisms11081951
Kemper, N. (2008). Veterinary antibiotics in the aquatic and terrestrial environment. Ecological Indicators, 8(1), 1–13. https://doi.org/10.1016/j.ecolind.2007.06.002
Kim, J., Kang, H. Y., & Lee, Y. (2008). The identification of CTX-M-14, TEM-52, and CMY-1 enzymes in Escherichia coli isolated from the Han River in Korea. Journal of Microbiology, 46(5), 478–481. https://doi.org/10.1007/s12275-008-0150-y
Korzeniewska, E., Korzeniewska, A., & Harnisz, M. (2013). Antibiotic resistant Escherichia coli in hospital and municipal sewage and their emission to the environment. Ecotoxicology and Environmental Safety, 91, 96–102. https://doi.org/10.1016/j.ecoenv.2013.01.014
Krumperman, P. H. (1983). Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods | Applied and Environmental Microbiology. Applied and Environmental Microbiology, 46, 165–170. https://journals.asm.org/doi/abs/10.1128/aem.46.1.165-170.1983.
Kutilova, I., Medvecky, M., Leekitcharoenphon, P., Munk, P., Masarikova, M., Davidova-Gerzova, L., et al. (2021). Extended-spectrum beta-lactamase-producing Escherichia coli and antimicrobial resistance in municipal and hospital wastewaters in Czech Republic: Culture-based and metagenomic approaches. Environmental Research, 193. https://doi.org/10.1016/j.envres.2020.110487
Lamba, M., Graham, D. W., & Ahammad, S. Z. (2017). Hospital wastewater releases of carbapenem-resistance pathogens and genes in urban India. Environmental Science and Technology, 51(23), 13906–13912. https://doi.org/10.1021/acs.est.7b03380
Lavilla, S., González-López, J. J., Sabaté, M., García-Fernández, A., Larrosa, M. N., Bartolomé, R. M., et al. (2008). Prevalence of qnr genes among extended-spectrum β-lactamase-producing enterobacterial isolates in Barcelona, Spain. Journal of Antimicrobial Chemotherapy, 61(2), 291–295. https://doi.org/10.1093/jac/dkm448
Liakopoulos, A., Mevius, D., & Ceccarelli, D. (2016). A review of SHV extended-spectrum β-lactamases: Neglected yet ubiquitous. Frontiers in Microbiology, 7(SEP). https://doi.org/10.3389/fmicb.2016.01374
Liedhegner, E., Bojar, B., Beattie, R. E., Cahak, C., Hristova, K. R., & Skwor, T. (2022). Similarities in virulence and extended spectrum beta-lactamase gene profiles among cefotaxime-resistant Escherichia coli wastewater and clinical isolates. Antibiotics, 11(2). https://doi.org/10.3390/antibiotics11020260
López-Jácome, L. E., Fernández-Rodríguez, D., Franco-Cendejas, R., Camacho-Ortiz, A., Morfin-Otero, M. D. R., Rodríguez-Noriega, E., et al. (2022). Increment antimicrobial resistance during the COVID-19 pandemic: Results from the Invifar Network. Microbial Drug Resistance, 28(3), 338–345. https://doi.org/10.1089/mdr.2021.0231
Magiorakos, A. P., Srinivasan, A., Carey, R. B., Carmeli, Y., Falagas, M. E., Giske, C. G., et al. (2012). Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clinical Microbiology and Infection, 18(3), 268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Mahmud, Z. H., Kabir, M. H., Ali, S., Moniruzzaman, M., Imran, K. M., Nafiz, T. N., et al. (2020). Extended-spectrum beta-lactamase-producing Escherichia coli in drinking water samples from a forcibly displaced, densely populated community setting in Bangladesh. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.00228
Manyi-Loh, C., Mamphweli, S., Meyer, E., & Okoh, A. (2018). Antibiotic use in agriculture and its consequential resistance in environmental sources: Potential public health implications. Molecules, 23(4). https://doi.org/10.3390/molecules23040795
Marathe, N. P., Berglund, F., Razavi, M., Pal, C., Dröge, J., Samant, S., et al. (2019). Sewage effluent from an Indian hospital harbors novel carbapenemases and integron-borne antibiotic resistance genes. Microbiome, 7(1). https://doi.org/10.1186/s40168-019-0710-x
McDaniels, A. E., Rice, E. W., Reyes, A. L., Johnson, C. H., Haugland, R. A., & Stelma, G. N. (1996). Confirmational identification of Escherichia coli, a comparison of genotypic and phenotypic assays for glutamate decarboxylase and β-D- glucuronidase. Applied and Environmental Microbiology, 62(9), 3350–3354. https://doi.org/10.1128/aem.62.9.3350-3354.1996
Murugan, M. S., Sinha, D. K., Vinodh Kumar, O. R., Yadav, A. K., Pruthvishree, B. S., Vadhana, P., et al. (2019). Epidemiology of carbapenem-resistant Escherichia coli and first report of blaVIM carbapenemases gene in calves from India. Epidemiology and Infection, 147. https://doi.org/10.1017/S0950268819000463
Nyirabahizi, E., Tyson, G. H., Dessai, U., Zhao, S., Kabera, C., Crarey, E., et al. (2020). Evaluation of Escherichia coli as an indicator for antimicrobial resistance in Salmonella recovered from the same food or animal ceca samples. Food Control, 115. https://doi.org/10.1016/j.foodcont.2020.107280
Nzima, B., Adegoke, A. A., Ofon, U. A., Al-Dahmoshi, H. O. M., Saki, M., Ndubuisi-Nnaji, U. U., & Inyang, C. U. (2020). Resistotyping and extended-spectrum beta-lactamase genes among Escherichia coli from wastewater treatment plants and recipient surface water for reuse in South Africa. New Microbes and New Infections, 38. https://doi.org/10.1016/j.nmni.2020.100803
Paterson, D. L., & Bonomo, R. A. (2005). Extended-spectrum beta-lactamases: A clinical update. Clinical Microbiology Reviews, 18, 657–686.
Pruthvishree, B. S., Vinodh Kumar, O. R., Sinha, D. K., Malik, Y. P. S., Dubal, Z. B., Desingu, P. A., et al. (2017). Spatial molecular epidemiology of carbapenem-resistant and New Delhi metallo beta-lactamase (blaNDM)-producing Escherichia coli in the piglets of organized farms in India. Journal of Applied Microbiology, 122(6), 1537–1546. https://doi.org/10.1111/jam.13455
Raimondi, S., Righini, L., Candeliere, F., Musmeci, E., Bonvicini, F., Gentilomi, G., et al. (2019). Antibiotic resistance, virulence factors, phenotyping, and genotyping of E. Coli isolated from the feces of healthy subjects. Microorganisms, 7(8). https://doi.org/10.3390/microorganisms7080251
Ramos, S., Silva, V., de Lurdes Enes Dapkevicius, M., Caniça, M., Tejedor-Junco, M. T., Igrejas, G., & Poeta, P. (2020). Escherichia coli as commensal and pathogenic bacteria among food-producing animals: Health implications of extended spectrum β-lactamase (ESBL) production. Animals, 10(12), 1–15. https://doi.org/10.3390/ani10122239
Rawat, N., Singh, F., Hirpurkar, S. D., Sannat, C., & Gade, N. E. (2018). Detection and characterization of extended-spectrum beta-lactamase genes (bla TEM and bla SHV ) among beta-lactam-resistant fecal coliforms of dairy cattle from Chhattisgarh, India. Turkish Journal of Veterinary and Animal Sciences, 42(6), 503–511. https://doi.org/10.3906/vet-1706-77
Runcharoen, C., Raven, K. E., Reuter, S., Kallonen, T., Paksanont, S., Thammachote, J., et al. (2017). Whole genome sequencing of ESBL-producing Escherichia coli isolated from patients, farm waste and canals in Thailand. Genome Medicine, 9(1). https://doi.org/10.1186/s13073-017-0471-8
Sabaté, M., Prats, G., Moreno, E., Ballesté, E., Blanch, A. R., & Andreu, A. (2008). Virulence and antimicrobial resistance profiles among Escherichia coli strains isolated from human and animal wastewater. Research in Microbiology, 159(4), 288–293. https://doi.org/10.1016/j.resmic.2008.02.001
Saekhow, P., & Sriphannam, C. (2021). Prevalence of extended-spectrum beta-lactamase-producing escherichia coli strains in dairy farm wastewater in chiang mai. Veterinary Integrative Sciences, 19(3), 349–362. https://doi.org/10.12982/vis.2021.030
Sageerabanoo, S., Malini, A., Mangaiyarkarasi, T., & Hemalatha, G. (2015). Phenotypic detection of extended spectrum β-lactamase and Amp-C β-lactamase producing clinical isolates in a Tertiary Care Hospital: A preliminary study. Journal of Natural Science, Biology and Medicine, 6(2), 383–387. https://doi.org/10.4103/0976-9668.160014
Samanta, A., Mahanti, A., Chatterjee, S., Joardar, S. N., Bandyopadhyay, S., Sar, T. K., et al. (2018). Pig farm environment as a source of beta-lactamase or AmpC-producing Klebsiella pneumoniae and Escherichia coli. Annals of Microbiology, 68(11), 781–791. https://doi.org/10.1007/s13213-018-1387-2
Sambrook, J., & Russell, D. (Eds.). (2001). Molecular Cloning: A Laboratory Manual (3rd ed.). Cold Spring Harbor Laboratory Press.
Sandhu, R. (2016). Evaluation of multiple antibiotic resistance (MAR) index and Doxycycline susceptibility of Acinetobacter species among inpatients. International Journal of Infectious Diseases, 45, 327. https://doi.org/10.1016/j.ijid.2016.02.710
Schmid, A., Hörmansdorfer, S., Messelhäusser, U., Käsbohrer, A., Sauter-Louis, C., & Mansfeld, R. (2013). Prevalence of extended-spectrum β-lactamase-producing Escherichia coli on Bavarian dairy and beef cattle farms. Applied and Environmental Microbiology, 79(9), 3027–3032. https://doi.org/10.1128/AEM.00204-13
Seabra, G., Ventura Mendes, R. F., dos Santos Amorim, L. F. V., Peregrino, I. V., Branquinha, M. H., dos Santos, A. L. S., & Nunes, A. P. F. (2021). Azithromycin use in COVID-19 patients: Implications on the antimicrobial resistance. Current Topics in Medicinal Chemistry, 21(8), 677–683. https://doi.org/10.2174/156802662108210319145317
Shaikh, S., Fatima, J., Shakil, S., Rizvi, S. M. D., & Kamal, M. A. (2015). Antibiotic resistance and extended spectrum beta-lactamases: Types epidemiology and treatment. Saudi Journal of Biological Sciences, 22(1), 90–101. https://doi.org/10.1016/j.sjbs.2014.08.002
Silva Segundo, R. J. E., Rufino, J. P., Sousa, L. G. V., Rodrigues, A. E. L., Falcão, A. L. S., de Melo Lima, I. C., et al. (2022). Bacterial resistance to azithromycin: Causes, effects, and the fight against COVID-19. Research, Society and Development, 11(6), e27711629198. https://doi.org/10.33448/rsd-v11i6.29198
Singer, R. S., Johnson, W. O., Jeffrey, J. S., Chin, R. P., Carpenter, T. E., Atwill, E. R., & Hirsh, D. C. (2000). A statistical model for assessing sample size for bacterial colony selection: A case study of Escherichia coli and avian cellulitis. Journal of Veterinary Diagnostic Investigation, 12(2), 118–125. https://doi.org/10.1177/104063870001200203
Snow, L. C., Warner, R. G., Cheney, T., Wearing, H., Stokes, M., Harris, K., et al. (2012). Risk factors associated with extended spectrum beta-lactamase Escherichia coli (CTX-M) on dairy farms in North West England and North Wales. Preventive Veterinary Medicine, 106(3–4), 225–234. https://doi.org/10.1016/j.prevetmed.2012.03.009
Sta Ana, K. M., Madriaga, J., & Espino, M. P. (2021). β-Lactam antibiotics and antibiotic resistance in Asian lakes and rivers: An overview of contamination, sources and detection methods. Environmental Pollution, 275. https://doi.org/10.1016/j.envpol.2021.116624
Stoppe, N. de C., Silva, J. S., Carlos, C., Sato, M. I. Z., Saraiva, A. M., Ottoboni, L. M. M., & Torres, T. T. (2017). Worldwide phylogenetic group patterns of Escherichia coli from commensal human and wastewater treatment plant isolates. Frontiers in Microbiology, 8(DEC). https://doi.org/10.3389/fmicb.2017.02512
Sultana, J., Cutroneo, P. M., Crisafulli, S., Puglisi, G., Caramori, G., & Trifirò, G. (2020). Azithromycin in COVID-19 patients: Pharmacological mechanism, clinical evidence and prescribing guidelines. Drug Safety, 43(8), 691–698. https://doi.org/10.1007/s40264-020-00976-7
Van Boeckel, T. P., Gandra, S., Ashok, A., Caudron, Q., Grenfell, B. T., Levin, S. A., & Laxminarayan, R. (2014). Global antibiotic consumption 2000 to 2010: An analysis of national pharmaceutical sales data. The Lancet Infectious Diseases, 14(8), 742–750. https://doi.org/10.1016/S1473-3099(14)70780-7
Vinueza-Burgos, C., Ortega-Paredes, D., Narvaéz, C., De Zutter, L., & Zurita, J. (2019). Characterization of cefotaxime resistant Escherichia coli isolated from broiler farms in Ecuador. PLoS ONE, 14(4). https://doi.org/10.1371/journal.pone.0207567
Wambugu, P., Kiiru, J., & Matiru, V. (2018). Escherichia coli harbouring resistance genes, virulence genes and integron 1 isolated from Athi River in Kenya. Advances in Microbiology, 08(11), 846–858. https://doi.org/10.4236/aim.2018.811056
Watkinson, A. J., Murby, E. J., Kolpin, D. W., & Costanzo, S. D. (2009). The occurrence of antibiotics in an urban watershed: From wastewater to drinking water. Science of the Total Environment, 407(8), 2711–2723. https://doi.org/10.1016/j.scitotenv.2008.11.059
WHO. (2017). Global Antimicrobial Resistance Surveillance System (GLASS) Report Early Implementation 2017–2018. Available online: https://www.who.int/glass/resources/publications/earlyimplementation-report-2017-2018/en/. Accessed 08.05.2023.
WHO. (2019). Ten threats to global health in 2019. Available Online. https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019. Accessed 08.05.2023.
Wu, Z., McGoogan, J. M., Wang, D., Hu, B., Hu, C., Zhu, F., et al. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA - Journal of the American Medical Association, 323(13), 1239–1242.
Xi, C., Zhang, Y., Marrs, C. F., Ye, W., Simon, C., Foxman, B., & Nriagu, J. (2009). Prevalence of antibiotic resistance in drinking water treatment and distribution systems. Applied and Environmental Microbiology, 75(17), 5714–5718. https://doi.org/10.1128/AEM.00382-09
Zarfel, G., Lipp, M., Gürtl, E., Folli, B., Baumert, R., & Kittinger, C. (2017). Troubled water under the bridge: Screening of River Mur water reveals dominance of CTX-M harboring Escherichia coli and for the first time an environmental VIM-1 producer in Austria. Science of the Total Environment, 593–594, 399–405. https://doi.org/10.1016/j.scitotenv.2017.03.138
Acknowledgements
The authors would like to acknowledge Prof. Dr. Balaji Veeraraghavan, Professor and Head, Department of Clinical Microbiology, Christian Medical College, Vellore, Tamil Nadu, India, for providing the positive control strains encoding blaCTX-M gr-1, blaCTX-M gr-2, blaCTX-M gr-8, blaCTX-M gr-9, blaCTX-M gr-25, blaTEM, blaOXA-1 like, and blaSHV genes. The authors would like to thank the Director, ICAR-Indian Veterinary Research Institute, Izatnagar, and the Vice-Chancellor, Banaras Hindu University, Varanasi, for providing support to conduct the research work.
Author information
Authors and Affiliations
Contributions
Conceptualization and design: DBR, SVSM, and SBB; sample collection: KS and AD; experimental work: KS; original draft preparation: KS and DBR; review and editing: DBR, SVSM, and SBB; supervision: DBR and PPK; statistical analysis: VMR and AD. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Satyaprakash, K., Pesingi, P.K., Das, A. et al. Occurrence of Multidrug-Resistant (MDR) Extended-Spectrum Beta-lactamase (ESBL)-Producing Escherichia coli in Wastewater and Natural Water Sources from the Eastern Part of Uttar Pradesh, India. Water Air Soil Pollut 235, 125 (2024). https://doi.org/10.1007/s11270-024-06914-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11270-024-06914-y