Abstract
Purpose
Asymptomatic pyuria and bacteriuria are more prevalent in diabetic patients and may be associated with urinary tract infection (UTI). The aim of this study is to investigate the association between asymptomatic pyuria/bacteriuria at the initiation of SGLT2 inhibitor and UTI risk in female patients with type 2 diabetes.
Methods
The study was designed as a practical, single-center, prospective, cohort study. The female outpatients with type 2 diabetes initiated SGLT2 inhibitor were included. Patients who were symptomatic or treated in the past 3 months for urinary or genital tract infection, had a high risk for UTI were excluded. Hospitalization/antibiotic use for indications other than UTI were exclusion criteria during follow-up. All patients were followed up for 3 months. Pyuria and bacteriuria were exposure and, UTI was the outcome. Cumulative incidence and relative risk of UTI were analyzed for pyuria and bacteriuria.
Results
143 female patients were included among 1132 female type 2 diabetic patients. 13 patients were excluded during follow-up. 41.5% of the patients (n = 54) had pyuria and 28.5% (n = 37) had bacteriuria. The cumulative incidence of UTI was 20% in the whole cohort, 25,9% (n = 14/54) in the pyuria group and 18.9% (n = 7/37) in the bacteriuria group. The relative risk of UTI was 1.64 (95% CI: 0.82–3.26, p = 0.15) for pyuria, 0.92 (95% CI: 0.42–2.01, p = 0.84) for bacteriuria, and 1.2 (95% CI: 0.47–3.08, p = 0.69) for pyuria plus bacteriuria. Adjusted odd ratios revealed similar results.
Conclusions
Asymptomatic pyuria/bacteriuria at the initiation of SGLT2 inhibitors are not risk factors for UTI in women with type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sodium–glucose cotransporter 2 inhibitors (SGLT2i) have dramatically changed the management of type 2 diabetes mellitus, especially in patients with cardiovascular or renal comorbidity due to their cardiorenal protective effect besides the role of glycemic control [1,2,3,4]. SGLT2i are recommended as first-line medication in patients who have established atherosclerotic cardiovascular disease or indicators of high cardiovascular risk, established kidney disease, or heart failure [5]. The efficacy of SGLT2i for glucose lowering is high and intermediate for weight loss, thus, their use is recommended for the achievement and maintenance of glycemic and weight management goals [5].
Asymptomatic pyuria and bacteriuria prevalence are higher in diabetic patients compared to non-diabetics [6,7,8]. Asymptomatic bacteriuria is associated with an increased risk of urinary tract infection among patients with type 2 diabetes [6, 9], however, treatment of asymptomatic bacteriuria does not appear to reduce complications, thus screening and treatment are not recommended [10, 11].
The action mechanism of SGLT2i is to suppress glucose reabsorption in renal proximal tubules, which causes glucosuria, thus, concern for the risk of urinary tract infection (UTI). Although the warning was added for severe UTI with the use of SGLT2i in early years of clinical use, subsequent randomized controlled trials, meta-analyses and retrospective cohort studies comparing SGLT2i versus placebo, dipeptidyl peptidase-4 inhibitors (DPP4i) and glucagon-like peptide-1 receptor agonists (GLP1-RA) have not shown an increased risk of UTI for SGLT2i [1,2,3, 12,13,14,15]. On the other hand, several retrospective and observational studies have revealed an increased risk of UTI with the use of SGLT2i [16,17,18,19].
Despite the data against screening and treatment of asymptomatic bacteriuria in diabetic patients, it is not known whether asymptomatic pyuria or bacteriuria at the initiation of SGLT2i are risk factors for UTI in female patients. UTI may still be a concern for clinicians, however, there is not enough data to recommend or not to recommend performing a urinalysis or urine culture test before initiation of SGLT2i. This study aims to investigate the association between asymptomatic pyuria/bacteriuria at the initiation of SGLT2i and UTI risk in a prospective cohort of women with type 2 diabetes.
Methods
Study design
The study was designed as a practical, single-center, prospective, cohort study. Female outpatients with type 2 diabetes under follow-up in the internal medicine department of a secondary hospital which cares for a district, and initiated SGLT2i (dapagliflozin/empagliflozin) were included between February and September 2022. Patients who were symptomatic for UTI or genital infection at the initiation, were treated for UTI or genital infection in the past 3 months, or had a high risk for UTI (any urological disease/catheter use, cancer, immunodeficiency, bedridden) were excluded. Anamnesis, physical examination, complete blood count, metabolic panel, HbA1c, lipid profile, automated urinalysis, and urine culture were performed on the SGLT2i initiation day. All patients were followed up for 3 months after SGLT2i initiation. Hospitalization and antibiotic use for indications other than UTI were exclusion criteria during follow-up. All patients were observed either by repeated visits to the same hospital or by the national patient database which includes patient data containing visits to the healthcare centers, diagnosis, treatment, laboratory, and imaging results (E-Nabiz). Urinary tract infection diagnosed or treated by any physician in any healthcare center was recorded as the outcome.
Approval of the Ethical Committee was obtained from SBU Kanuni Education and Research Hospital, Ethics Committee of Clinical Studies (Decision number: 2022/42) in compliance with the Helsinki Declaration.
Laboratory tests
Urine samples were collected in sterile, preservative containers and analyzed within 2 h by DIRUI FUS-100/H-800 automated urine analyzer which is based on flow cell digital imaging and identification using software. Pyuria was defined as ≥ 3 white cells per high-power field.
Midstream urine samples were collected for urine culture. 10 μL of the sample was dispensed onto blood agar and eosin methylene blue agar medium and incubated at 37 °C for 24 h. Conventional methods (colony morphology, Gram stain, MVC reactions) and VITEK 2 automated system (bioMerieux, Marcy-l’Étoile, France) were used for bacterial identification. Any bacterial growth irrespective of colony-forming units (CFU)/mL reported by the microbiology laboratory was defined as bacteriuria except contamination.
The complete blood count was performed by Abbott CELL-DYN Ruby Analyzer using techniques of flow cytometry. The metabolic panel, lipid panel, and HbA1c were measured using the Abbott Architect chemistry system. HbA1c was measured by automated direct enzymatic method from whole blood. The estimated glomerular filtration rate (eGFR) was calculated by CKD-EPI.
Output and statistical analysis
The sample size per group was calculated as 39 (78 for the total sample size) in the power analysis. Expected incidence in unexposed (without bacteriuria or pyuria) 0.335 [17], assumed relative risk 1.91 [9], confidence level 0.95 and power 0.8 were used for power analysis.
Age, comorbidities (hypertension, dyslipidemia, cardiovascular disease), medications, fasting blood glucose level, HbA1c, complete blood count, metabolic panel and lipid panel data, SGLT2i type and dosage were presented as characteristics of the study population. The characteristics were compared as univariable between UTI( +) and UTI(–) groups. Pyuria and bacteriuria frequency were determined. Cumulative incidence and relative risk of UTI were analyzed for pyuria and bacteriuria. Risk of urinary tract infection associated with pyuria and bacteriuria was analyzed by univariable logistic regression analysis for unadjusted odd ratios and by multivariable logistic regression analysis to adjust pyuria and bacteriuria for clinically relevant variables (age, HbA1c, CVD as comorbidity, eGFR, and SGLT2i type). Pyuria and bacteriuria were adjusted for age in model 1; for age, HbA1c, CVD and eGFR in model 2; for age, HbA1c, CVD, eGFR and SGLT2i type in model 3. Finally, pyuria and bacteriuria were adjusted for significant variables in univariable analysis in addition to previous variables.
Continuous variables were given as median (mini-mum (min)-maximum (max)). Categorical variables were represented as a percentage. The significance of relative risks was interpreted as 95% confidence intervals and p-values. Univariable analyses of characteristics were performed using chi-square, Fisher exact, Student’s t, and Mann–Whitney U tests, where needed. Unadjusted and adjusted odd ratios were calculated by univariable and multivariable logistic regression analysis. All p-values were based on a 2-tailed test of significance (p = 0.05). Statistical analyses were conducted using software SPSS version 26 (SPSS Inc, USA).
Results
Study population and characteristics
Totally 143 female patients were included among 1132 female type 2 diabetes patients during the study period. 13 patients were excluded during follow-up (7 patients because of antibiotic use for indications other than UTI, hospitalization of 1 patient for coronary artery bypass surgery, 1 for decompensated heart failure, 1 for non-ST-elevation myocardial infarction, 1 for cerebrovascular disease, 1 for acute pancreatitis and 1 for pulmonary thromboembolism) (Fig. 1). The characteristics of the study population (n = 130) were given in Table 1. The median age was 62 (range 34–87). 79.2% of the patients had hypertension, 63.1% had dyslipidemia and 20.8% had cardiovascular disease (CVD) (established atherosclerotic cardiovascular disease and/or heart failure). Dapagliflozin 10 mg was initiated in 70% of the patients (n = 91), empagliflozin 10 mg in 24.6% (n = 32), and empagliflozin 25 mg in %5.4 (n = 7). 89.2% of the patients were using metformin at the SGLT2i initiation. Median fasting blood glucose and HbA1c were 205 mg/dl (range 69–642) and 9.1% (range 5.9–13.9), respectively. Median eGFR was 80 ml/min (range 32–120). 41.5% of the patients (n = 54) had pyuria and 28.5% (n = 37) had bacterial growth in urine culture. The most common microorganisms were E. coli (n = 13, 35.1%) and S. agalactiae (n = 12, 32.4%). (Other microorganisms were Klebsiella pneumoniae, Enterococcus sp., Pseudomonas aeruginosa, Lactobacillus, alfa, and beta hemolytic streptococcus). 59.4% of the patients in bacteriuria group had bacterial growth of ≥ 100.000 CFU/ml. The characteristic were compared between UTI( +) and UTI(–) groups (Table 1). Only three variables were statistically different between groups. The ACEi-ARB use was more common in the UTI(–) group than the UTI( +) group (74% vs 50%, p = 0.01), median HDL level was higher in the UTI(–) group ( 52 mg/dL vs 47 mg/dL, p = 0.05); and median leukocyte count was higher in the UTI( +) group (9.4 × 10*3/mcL vs 8.2 × 10*3/mcL, p = 0.01).
UTI risk
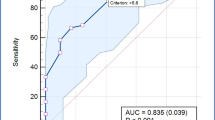
The cumulative incidence of UTI for 3-months follow-up was 20% (n = 26/130) in the whole cohort, 25,9% (n = 14/54) in the pyuria group and 18.9% (n = 7/37) in the bacteriuria group (Fig. 1). The relative risk of UTI was 1.64 (95% CI: 0.82–3.26, p = 0.15) for pyuria, 0.92 (95% CI: 0.42–2.01, p = 0.84) for bacteriuria, and 1.2 (95% CI: 0.47–3.08, p = 0.69) for pyuria plus bacteriuria (Table 2, Fig. 2). 2 patients (1.5% of the whole cohort) had severe UTI (pyelonephritis n = 1 and urosepsis n = 1).
Risk of urinary tract infection associated with pyuria and bacteriuria was analyzed by univariable logistic regression analysis for unadjusted odd ratios and by multivariable logistic regression analysis for adjusted odd ratios. In the final model, pyuria and bacteriuria were adjusted for clinically relevant variables (age, HbA1c, CVD, eGFR and SGLT2i type) and significant variables in univariable analysis (ACEi-ARB, HDL, leukocyte count). Non of the models did not reveal significant odds ratio for pyuria and bacteriuria. The adjusted OR (95% CI) for pyuria and bacteriuria were 1,55 (0,5–4,83) and 0,95 (0,29–3,06) in model 4, respectively (Table 3).
Discussion
Screening and treatment of asymptomatic bacteriuria and pyuria are not recommended in diabetic patients. Although currently available data suggest that UTI is not a concern with the use of SGLT2i, there is some conflicting data and a lack of proof about asymptomatic pyuria and bacteriuria in the SGLT2i era. This prospective cohort study investigated whether asymptomatic pyuria and bacteriuria at the SGLT2i initiation are risk factors for UTI and revealed that there was no increased risk. The relative risk of UTI was 1.64 (95% CI: 0.82–3.26) for pyuria, and 0.92 (95% CI: 0.42–2.01) for bacteriuria.
In the meta-analysis study of Renko et al., asymptomatic bacteriuria, which was defined as at least 100.000 CFU/ml, was present 12.2% of the diabetic patients, OR was 3.2 (95% CI: 2–5.2) for patients with type 2 diabetes compared to non-diabetics. In women, the prevalence of asymptomatic bacteriuria was 14.2% [6]. In our study, which had a female population, 28.5% of the patients had bacteriuria, however, we included the patients with bacterial growth less than 100.000 CFU/ml in culture. Asymptomatic bacteriuria was associated with UTI in this meta-analysis, not like in our study. Another study comparing postmenopausal diabetic and non-diabetic women showed that diabetic women had approximately doubled risk for both of the asymptomatic bacteriuria and UTI [8]. In our study, the median age was 62 (range 34–97), most of the patients were postmenopausal. A cohort study searched the consequences of asymptomatic bacteriuria in women with diabetes. 29% of the patients had asymptomatic bacteriuria at baseline and 34% of the patients with asymptomatic bacteriuria had UTI during the 18-months follow-up [9]. Although asymptomatic bacteriuria is more prevalent and associated with an increased risk of UTI in these studies, a randomized controlled trial revealed that treatment of asymptomatic bacteriuria did not reduce the episodes of UTI [10]. In this randomized controlled trial, 40% of the patients in the placebo group had at least one UTI episode during a 27-month follow-up. On the other hand, asymptomatic pyuria is less investigated in the literature. Nakano et al. showed that diabetic women more often had asymptomatic pyuria than non-diabetic women (27.9 vs. 15.8%) [7]. However, pyuria was defined as ≥ 10 white cells per high-power field in this study, whereas it was 3 in our study. Taken together, the prevalence of pyuria and bacteriuria at baseline in our study was consistent with the literature. The cumulative incidence of UTI in our study was 20% in the whole cohort, 25,9% in the pyuria group, and 18.9% in the bacteriuria group. The lower incidence of UTI comparing the previous studies [9, 10] may be attributed to the shorter follow-up period of our study.
The main randomized controlled studies showing cardiovascular and renal protective effects of dapagliflozin and empagliflozin did not show an increased risk of UTI with SGLT2i [1,2,3]. In the randomized controlled study of empagliflozin for the progression of kidney disease, 22.9% of the patients in eGFR < 60 groups had UTI and 16.2% in eGFR > 60 groups, which were not different from placebo [2]. In a population-based cohort study (123 752 patients in cohort 1 and 111 978 in cohort 2) comparing SGLT2i versus DPP4i and GLP1-RA, SGLT-2 inhibitors were not associated with increased risk for outpatient UTIs (cohort 1: HR, 0.96 [CI, 0.89 to 1.04]; cohort 2: HR, 0.91 [CI, 0.84 to 0.99]) [12]. Similarly, severe UTI and urosepsis did not increase with the use of SGLT2i in cohort studies [12, 13]. In two different meta-analyses, only dapagliflozin was associated with an increased risk of UTI, but not canagliflozin and empagliflozin. However, all agents were associated with genital tract infections [14, 15]. The majority of the patients (70%) in our study had dapagliflozin. On the other hand, a retrospective cohort study of Yang et al. revealed that SGLT2i were associated with a higher risk of UTI and genital infections when used add-on therapy to metformin [16]. Uitrakul et al. compared SGLT2i and non-SGLT2i in their real-world observational study in terms of UTI. The overall incidence rate of UTI was 33.49% in the SGLT2i group, which was not different between dapagliflozin and empagliflozin treatment. Moreover, patients of female gender and older age had a significantly higher risk of UTI when treated with SGLT2i [17]. Consistently, our study population was female patients with a median age of 62. The SGLT2i study of Kang et al. showed that only women ≥ 50 years showed a significant increase in the risk of urinary tract infections (UTIs) (IRR 1.25, 95% CI 1.14–1.37) and the highest risk of UTI risk was observed 8–14 days after initiating SGLT2 inhibitor therapy [18]. The gender and age of our study population and 3-months follow-up are consistent with these results. However; adjusting pyuria and bacteriuria for age, HbA1c, CVD, eGFR and SGLT2i type did not reveal significant odd ratios in the multivariable logistic regression analysis. In another retrospective longitudinal study of 95 patients, 20 participants discontinued SGLT2i due to genital or urinary tract infections [19].
The conflicting data about UTI risk with the use of SGLT2i, and the importance of asymptomatic bacteriuria for UTI risk in diabetic patients rationalize the design of our study. However, there are some limitations. Our study is a prospective cohort study and does not have a placebo or active control group. Although sample size calculation revealed a total number of 78 patients, sample size is relatively limited, therefore conclusions should be drawn with caution. The follow-up period is relatively short, however, the use of antibiotics and hospitalization for other than UTI indication increase over time in the longer follow-up period, making the interpretation of the effect of asymptomatic pyuria and bacteriuria at baseline difficult. Definitions of asymptomatic pyuria and bacteriuria are more liberal in this study, comparing the literature, but the aim was to conduct a practical pragmatic study reflecting daily practice concerns. Because we did not record the data of exact UTI diagnosis time after SGLT2i initiation, we could not perform Kaplan–Meier analysis. Lastly, although genital tract infections are prominently associated with SGLT2i, our study does not give genital tract infection data because of the lack of reliable data.
In conclusion, this pragmatic practical cohort study reveals that pyuria or bacteriuria at the initiation of SGLT2İ are not risk factors for UTI for female patients with type 2 diabetes in the 3-month follow-up. As an interpretation of this result for daily practice, it is not necessary to perform urine culture and urinalysis for pyuria before initiating SGLT2i and asymptomatic pyuria and bacteriuria should not be an obstacle to initiating SGLT2i when there is an indication of SGLT2i.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JFE, McMurray JJV, Lindberg M, Rossing P, Sjöström CD, Toto RD, Langkilde AM, Wheeler DC (2020) Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383(15):1436–1446. https://doi.org/10.1056/NEJMoa2024816
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375(4):323–334. https://doi.org/10.1056/NEJMoa1515920
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357. https://doi.org/10.1056/NEJMoa1812389
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128. https://doi.org/10.1056/NEJMoa1504720
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Leon J, Lyons SK, Perry ML, Prahalad P, Pratley RE, Seley JJ, Stanton RC, Gabbay RA (2023) 9 Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care 46(Suppl 1):S140-s157. https://doi.org/10.2337/dc23-S009
Renko M, Tapanainen P, Tossavainen P, Pokka T, Uhari M (2011) Meta-analysis of the significance of asymptomatic bacteriuria in diabetes. Diabetes Care 34(1):230–235. https://doi.org/10.2337/dc10-0421
Nakano H, Oba K, Saito Y, Ouchi M, Yamashita N, Okamura K, Takai E, Mizuno S, Matsumura N, Inuzuka Y, Suzuki T (2001) Asymptomatic pyuria in diabetic women. J Nippon Med Sch 68(5):405–410. https://doi.org/10.1272/jnms.68.405
Boyko EJ, Fihn SD, Scholes D, Abraham L, Monsey B (2005) Risk of urinary tract infection and asymptomatic bacteriuria among diabetic and nondiabetic postmenopausal women. Am J Epidemiol 161(6):557–564. https://doi.org/10.1093/aje/kwi078
Geerlings SE, Stolk RP, Camps MJ, Netten PM, Collet JT, Schneeberger PM, Hoepelman AI (2001) Consequences of asymptomatic bacteriuria in women with diabetes mellitus. Arch Intern Med 161(11):1421–1427. https://doi.org/10.1001/archinte.161.11.1421
Harding GK, Zhanel GG, Nicolle LE, Cheang M (2002) Antimicrobial treatment in diabetic women with asymptomatic bacteriuria. N Engl J Med 347(20):1576–1583. https://doi.org/10.1056/NEJMoa021042
Köves B, Cai T, Veeratterapillay R, Pickard R, Seisen T, Lam TB, Yuan CY, Bruyere F, Wagenlehner F, Bartoletti R, Geerlings SE, Pilatz A, Pradere B, Hofmann F, Bonkat G, Wullt B (2017) Benefits and harms of treatment of asymptomatic bacteriuria: a systematic review and meta-analysis by the european association of urology urological infection guidelines panel. Eur Urol 72(6):865–868. https://doi.org/10.1016/j.eururo.2017.07.014
Dave CV, Schneeweiss S, Kim D, Fralick M, Tong A, Patorno E (2019) Sodium-glucose cotransporter-2 inhibitors and the risk for severe urinary tract infections: a population-based cohort study. Ann Intern Med 171(4):248–256. https://doi.org/10.7326/m18-3136
Fisher A, Fralick M, Filion KB, Dell’Aniello S, Douros A, Tremblay É, Shah BR, Ronksley PE, Alessi-Severini S, Hu N, Bugden SC, Ernst P, Lix LM (2020) Sodium-glucose co-transporter-2 inhibitors and the risk of urosepsis: A multi-site, prevalent new-user cohort study. Diabetes Obes Metab 22(9):1648–1658. https://doi.org/10.1111/dom.14082
Pelletier R, Ng K, Alkabbani W, Labib Y, Mourad N, Gamble JM (2021) Adverse events associated with sodium glucose co-transporter 2 inhibitors: an overview of quantitative systematic reviews. Ther Adv Drug Saf 12:2042098621989134. https://doi.org/10.1177/2042098621989134
Puckrin R, Saltiel MP, Reynier P, Azoulay L, Yu OHY, Filion KB (2018) SGLT-2 inhibitors and the risk of infections: a systematic review and meta-analysis of randomized controlled trials. Acta Diabetol 55(5):503–514. https://doi.org/10.1007/s00592-018-1116-0
Yang H, Choi E, Park E, Na E, Chung SY, Kim B, Han SY (2022) Risk of genital and urinary tract infections associated with SGLT-2 inhibitors as an add-on therapy to metformin in patients with type 2 diabetes mellitus: a retrospective cohort study in Korea. Pharmacol Res Perspect 10(1):e00910. https://doi.org/10.1002/prp2.910
Uitrakul S, Aksonnam K, Srivichai P, Wicheannarat S, Incomenoy S (2022) The incidence and risk factors of urinary tract infection in patients with type 2 diabetes mellitus using sglt2 inhibitors: a real-world observational study. Medicines (Basel) 9(12):59. https://doi.org/10.3390/medicines9120059
Kang M, Heo KN, Ah YM, Yang BR, Lee JY (2021) Age- and sex-specific risk of urogenital infections in patients with type 2 diabetes treated with sodium-glucose co-transporter 2 inhibitors: a population-based self-controlled case-series study. Maturitas 150:30–36. https://doi.org/10.1016/j.maturitas.2021.06.003
Hopf M, Kloos C, Wolf G, Müller UA, Müller N (2021) Effectiveness and safety of SGLT2 inhibitors in clinical routine treatment of patients with diabetes mellitus type 2. J Clin Med 10(4):571. https://doi.org/10.3390/jcm10040571
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EA, AGC, ÖD, DÇ and MŞ designed the study. EA, and AGC collected the data. EA and MŞ performed the analyses. EA, AGC, ÖD, DÇ and MŞ interpreted the data. EA wrote the manuscript, EA, AGC, ÖD, DÇ and MŞ reviewed and made final approval of the manuscript. The corresponding author EA had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no conflicts of interest and competing financial interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of the SBU Kanuni Education and Research Hospital, (Decision number: 2022/42).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akkuş, E., Gökçay Canpolat, A., Demir, Ö. et al. Asymptomatic pyuria and bacteriuria are not risk factors for urinary tract infection in women with type 2 diabetes mellitus initiated SGLT2 inhibitors. Int Urol Nephrol 56, 1165–1172 (2024). https://doi.org/10.1007/s11255-023-03798-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03798-5