Abstract
Purpose
Fournier’s Gangrene (FG) is a fatal condition, therefore prognosis prediction is a crucial step before treatment planning. We aimed to investigate the predictive value of Hemoglobin, Albumin, Lymphocyte and Platelet (HALP) score which is frequently employed in vascular disorders and malignancies, on disease severity and survival in FG patients and to compare HALP score with well-known scoring systems on this aspect.
Materials and methods
Eighty-seven men who had surgical debridement for FG between December 2006 and January 2022 were included in this study. Their symptoms, physical examination findings, laboratory tests, medical histories, vital signs, extent and timing of the surgical debridement and antimicrobial therapies were noted. The HALP score, Age-adjusted Charlson Comorbidity Index (ACCI) and Fournier’s Gangrene Severity Index (FGSI) were evaluated for their predictive values for survival.
Results
FG patients were grouped as survivors (Group 1, n = 71) and non-survivors (Group 2, n = 16) and the results were compared. The mean ages of survivors (59 ± 12.55 years) and non-survivors (64.5 ± 14.6 years) were similar (p = 0.114). The median size of necrotized body surface area was 3% in Group 1 and 4.8% in Group 2 (p = 0.013). On admission, hemoglobin, albumin and serum urea levels and white blood cell counts were significantly different in two study groups. Two study groups were similar for HALP scores. However, ACCI and FGSI scores were greater significantly in non-survivors.
Conclusions
Our results indicated that HALP score does not predict a survival successfully in FG. However, FGSI and ACCI are successful outcome predictors in FG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fournier’s gangrene (FG) is a rare soft tissue infection of the perineum and genital region leading to necrosis [1]. Genitourinary system infections are often polymicrobial and may extend promptly resulting in multi-organ failure, septic shock and fatality [2]. Although a decline in the previous two decades, the mean inpatient mortality rate is 7.3% (range 4.7–40.4%) for FG which is still high [3]. Recent decline in the mortality rate is due to advances in diagnosis and treatment methods.
Survival prediction is important for treatment planning, therefore various scoring systems were employed gor this purpose. Fournier’s Gangrene Severity Index (FGSI) helps clinicians for outcome prediction in FG patients [4]. This scoring has been established on the metabolic and physiologic condition of the patient. The age-adjusted Charlson Comorbidity Index (ACCI) was developed to estimate the 1-year risk of mortality based on existing comorbid conditions [5]. ACCI has been widely used to predict outcomes of various medical conditions and malignancies, it is also employed to predict survival in FG [6, 7].
HALP score is a biomarker that combines various indicators for immune and nutritional statuses of an individual, and has been employed to predict prognosis particularly in patients with cancer [8]. Apart from cancer patients, it has also been employed as a prognostic tool in various other clinical conditions: to predict mortality in COPD exacerbations, to predict preterm labor, and to determine the severity and postoperative outcome of acute appendicitis since it is able to demonstrate systemic inflammation as well as immune and nutritional statuses [9,10,11]. Immunonutritional status is an important consideration in patients with FG, similar to cancer patients. Therefore, we aimed to determine the value of HALP score to determine disease severity and to predict survival in FG patients, to compare its prognostic value as an outcome predictor with FGSI and ACCI, and to identify other prognostic factors for FG.
Material-methods
Ethics Committee of our Institution approved the study protocol of this retrospective study (No: E2-22-2573). A total of 87 patients who had radical surgical debridement for FG between December 2006 and January 2022 in our institution were included. FG patients were grouped into two groups as those who died (n = 16) and survived (n = 71). History, extent of necrosis and infection, clinical symptoms, vital parameters, and the microbiological, biochemical and hematological results of the patients were noted. Etiological factors and comorbid conditions that could have played role in the pathophysiology FG were also noted.
In our clinic, we perform surgical debridement urgently and aggressively after diagnosis of FG: we remove all necrotic tissues until viable soft tissues are recognized. The time and range of the surgical debridement were noted. Modified body surface area nomogram used in burn injuries was employed to measure gangrene size: scrotum, penis and perineum were taken 1% for each, and the spread of gangrene to each ischiorectal fossa was taken as 2.5% [4]. During surgery, colostomy was performed if anal sphincter was involved, and suprapubic cystostomy was done in the ones with involvement of urethra. Samples for bacterial culture were obtained both from the wound and the pus. Appropriate IV fluid replacement and empirical parenteral antibiotics (ceftriaxone 4 g/day and metronidazole 1.5 g/day] were administered until bacteriologic culture and susceptibility results were available. Afterwards culture-directed antibiotics were administered if necessary. Surgical debridement was repeated usually with 24–48 h-intervals until the wound was healed. The number of surgical debridements was noted. A primary suturing was performed after the wound healed and it was ensured that all surrounding tissues were viable. If the wound was large and not suitable for primary closure, plastic and reconstructive surgeons covered it with a partial thickness skin graft.
FGSI is obtained from the sum of 9 parameters including respiratory rate, temperature, heart rate, serum sodium, potassium, creatinine and bicarbonate levels, leukocyte count and hematocrit, scored between 0 and 4 according to their values [4].
ACCI is a combination of Charlson Comorbidity Index and age equivalence index. The Charlson comorbidity index is derived from the sum of 19 different conditions scored between 1 and 6. The age equivalence index is calculated by increasing the age, which is 1 point in the 6th decade, by one point cumulatively with each increasing decade (e.g., 2 points in the 7th decade, 3 points in the 8th decade). ACCI is obtained by the sum of these two scores [5].
The HALP score is usually employed as an indicator of systemic inflammation, and calculated based on haemoglobin and albumin levels, and leukocyte and platelet counts. The calculation formula is as follows: hemoglobin (g/L) × albumin (g/L) × lymphocytes (/L)/platelets (/L) [12].
FGSI, ACCI and HALP scores of each patient included in the study were calculated.
Statistical analysis
SPSS (Statistical Package for Social Sciences, Chicago, IL) v.20 for Windows was used for statistical analyses. Kolmogorov Smirnov test was used to test normal distribution of quantitative parameters. For comparing survival and non-survival groups, Independent Samples t-test was employed for the data conforming to normality and Mann Whitney-U test was used for the data not conforming to normality. FGSI, ACCI and HALP scores were compared with Mann Whitney-U test between the groups as they did not conform to normality. Receiver operating characteristic curves (ROCs) were created to address the predictive role of ACCI, FGSI and HALP scores for mortality. Logistic regression analyses were performed for parameters that could significantly predict survival. p < 0.05 was accepted as statistically significant in the statistical analyses.
Results
Of 87 patients, 16 (18.4%) died and 71 (81.6%) survived. In non-survivors, the median survival time was 14 ± 15.55 (2–60) days. The overall median age was 60 (25–89) years. The median ages of survivors and non-survivors were similar (p = 0.1). The median body surface area of necrosis was 3% in survivors and 4.8% in non-survivors (p = 0.013). Symptom durations were similar in survivors and non-survivors (p = 0.6). When all participants were taken into consideration, the most common comorbid condition was diabetes mellitus (DM) which was evident in 55.2% of the patients. DM was followed by hypertension (HT) (26.4%), atherosclerotic coronary heart disease (ASCD) (18.4%), perianal abscess (12.6%), chronic renal failure (10.3%), malignancies (8%), and peripheral vascular disease (PVD) (2.8%). The prevalence of all comorbid conditions were similar in two the groups except for the presence of a malignancy (Table 1).
All FG patients had a radical surgical debridement and all necrotic tissues were resected. Orchiectomy was performed in 35 (49.3%) survived patients (26 unilateral, 9 bilateral) and in 11 (68.8%) patients who did not survive (6 unilateral, 5 bilateral). Hemiscrotectomy was performed in 49 (69%) survivors (45 unilateral, 14 bilateral) and 13 (81.2%) patients who did not survive (4 unilateral, 9 bilateral). Four survivors and 2 non-survivors had diverting colostomies. Cystostomy was performed in 3 survivors and 4 non-survivors. The wound was sutured primarily in 57 (80.3%) survivors and 3 (18.8%) non-survivors. Split-thickness skin grafts were needed in 14 (19.7%) survivors and 1 (6.2%) non-survivor.
Laboratory parameters are presented in Table 1. The study groups showed significant differences for hemoglobin, hematocrit, neutrophil, serum total protein, albumin and urea levels. Other laboratory parameters were similar in two study groups.
When the bacteriological culture results are concerned, the most commonly isolated microorganisms from the necrotic area or pus during surgery or in the ward were E. coli in 19 (21.8%), Enterococci in 10 (11.5%), Streptococci in 8 (9.2%), Candida spp. in 7 (8%), Acinetobacter in 6 (6.9%) and coagulase negative Staphylococcus in 5 (5.7%) patients. Polymicrobial infection was detected in 17 patients (19.5%). Anaerobic bacterial growth was not determined in any of the patients. Microbial growth was evident on culture in 42 (59.2%) survivors and 6 (37.5%) non-survivors.
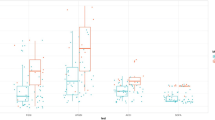
Median scores on admission were as follows: FGSI score was 2 ± 2.7(0–12) in the survivors and 5.5 ± 4.88(0–15) in non-survivors (p = 0.002); ACCI score was 3 ± 1.83 (0–8) in the survivors and 4.5 ± 3.32 (0–15) in non-survivors (p = 0.005), and HALP score was 30.9 ± 80.5 (0–485.5) in the survivors and 33.5 ± 345.8 (1.2–1400) and non-survivors (p = 0.6). FGSI and ACCI scores were significantly greater in non-survivors, however HALP scores were similar in two groups (Table 1).
Comparison of FGSI, ACCI and HALP scores with ROC analysis results are shown in Table 2. Our results indicated that FGSI and ACCI were significant predictors of mortality, however HALP scores did not predict survival.
FGSI score significantly predicted the mortality rate with an accuracy rate of 85.1% (OR 1.33, 95% CI 1.13–1.57, p = 0.001). This rate was 83.9% for ACCI score (OR 1.52, 95% CI 1.13–2.06, p = 0.006). The HALP score was found as an insignificant predictor of mortality in univariate analysis. According to the results of univariate logistic regression analysis; hemoglobin, hematocrit, total protein, albumin and neutrophil values were also predicted mortality rate significantly (Table 3).
Discussion
FG is necrotizing fasciitis of external genitalia and perianal region, causing gangrene of skin and subcutaneous tissues due to arterial thrombosis [13]. There is high mortality despite improvements in the diagnosis and management. In a recent review, FG’s mortality rate was reported as 7.3%. A meta-analysis that included 173 studies reported this rate as 19.8% [3, 14]. In our current study, the mortality rate has been determined as 18.4%. This mortality rate is compatible with the mortality rates reported in our three previous studies on the same subject (22.2%, 14% and 17.2%) [15,16,17].
The relationship of mortality with the comorbid conditions of the FG patients has been investigated in detail. In a systematic review and meta-analysis of 38 studies it was reported that diabetes, heart conditions and kidney failure increased mortality of FG significantly, however hypertension, pulmonary and liver disorders and malignancies had no effect on mortality [18]. In our study, the most common comorbid condition was DM, which was evident in 55.2% of our patients, however we did not find any difference between the survivors (56.3%) and non-survivors (50%) for presence of DM. We did not find any difference between two groups for HT, CASHD or PVD. Similar to the results of this study, comorbid disorder rates were similar in two study groups, and diabetes did not affect mortality rate in our previous studies [16, 17]. The non-survivor group had a significantly higher malignancy rate.
In FG patients, Escherichia coli, Bacteroides, Staphylococcus, Proteus, Streptococcus, Pseudomonas, and Enterococcus were isolated the most frequently [17, 19]. Empirical broad-spectrum antibiotics (encompassing gram-positive, gram-negative, aerobic and anaerobic organisms, with alterations in case of antibiotic hypersensitivity) should be administered just after the diagnosis, and the antibiotics should be revised after the wound culture and susceptibility test results are obtained. Duration of antibiotic therapy has been debated [20]. Therefore, this duration depends on the decision of the clinician. In our center, antibiotics are generally administered until FG is under control and the patient recovers clinically.
It has been reported that various laboratory parameters may be used as prognostic indicators. Low levels of hematocrit [4, 15,16,17], serum albumin [4, 15, 16], magnesium [16, 17], calcium [16], high levels of blood urea nitrogen [4, 15, 16] and ALP [4, 16, 17] have been associated with mortality. Lower hemoglobin, hematocrit, total protein, albumin levels and higher neutrophil and blood urea nitrogen levels were found in the non-survivor group in this study. Logistic regression analysis showed that high neutrophil counts, and low hemoglobin, hematocrit, total protein and albumin values were correlated with a worse prognosis.
It has been reported that an extensive necrotized body surface area affects the prognosis adversely [15,16,17, 21]. Hahn et al. studied 41 patients with FG, and based on the multivariate regression analysis results concluded that necrosis elsewhere from perineum/groin area was an independent predictor for mortality [22]. In the current study, median size of necrotized body surface area was statistically bigger in non-survivors (3% in survivors and 4.8% in non-survivors, p = 0.013), however mortality was not significantly correlated with the surface area involved.
In 1995, Laor et al. defined FGSI to predict prognosis in patients presenting with FG [4]. Since then, several studies have investigated the value of FGSI in predicting the FG prognosis. Although the majority of publications reported FGSI as successful for predicting prognosis and mortality risk in patients with FG [23,24,25], some others concluded that FGSI was not useful for this purpose [7, 15, 26]. The results of current study have proven that FGSI score could predict FG severity and survival.
Charlson et al. published Charlson Comorbidity Index (CCI) in 1987 to estimate 1-year risk of mortality based on existing comorbid conditions [5]. The age-adjusted CCI (ACCI) uses the patient’s age as a correction variable of the score [27]. ACCI has been widely used to predict outcomes of various medical conditions, malignancies and also to predict survival in FG [6, 7, 28, 29]. Roghmann et al. compared mortality prediction of scoring systems in 44 FG patients, and reported that ACCI predicted outcome as successful as FGSI [6]. Zhu et al. also compared scoring systems for FG prognosis, found that the ACCI score was useful for determining the prognosis, and it was better since it was more sensitive and specific and was easier to collect [7]. In our previous article, we evaluated 50 FG patients and compared mortality predictive values of the scoring tools. ACCI scores of survivors and non-survivors were similar, and ACCI did not predict either severity of the disease or survival [15]. In this study, non-survivors had a significantly greater median ACCI score, and a high ACCI score was correlated with a high mortality rate. In our previous two studies we found that neither FGSI nor ACCI had predictive value in disease severity or patients’ survival [15, 26], however in the current study, we have found that high FGSI and ACCI scores are correlated with mortality. In our current study, the number of patients in the non-survivor group was more than doubled. We think that higher number of patients, particularly in the non-survivor group, had an effect on the statistical analyses, and ACCI and FGSI were found to be significant.
The HALP score is a new indicator developed to measure systemic inflammation and nutritional status. It was recently used as a prognostic tool in patients with several malignancies [30, 31]. In a study on 1360 patients who had nephrectomy due to renal cell carcinoma, the HALP score was found as an independent prognostic factor for predicting cancer-specific survival [32]. Another study included 582 patients with adenocarcinoma of pancreas who had radical surgery, and investigated the prognostic importance of admission HALP score. There was a significant correlation between low HALP scores and more extensive lymphatic metastasis, poor tumor differentiation, high TNM stage, early recurrence and short survival [33]. The HALP score has also been studied in vascular conditions. Xu et al. studied the correlation of HALP score with post-stroke cognitive impairment (PSCI) in acute ischemic stroke, and reported that a low admission HALP score was associated with early-onset PSCI. They concluded that the HALP score was useful to identify patients with a high risk for PSCI [34].
Although the HALP score has been employed as a predictor of prognosis in a number of cancer types and vascular conditions, it has not been tested as a prognostic indicator in any infectious disorders until now. FG is an infectious disease with a high mortality rate, and the immune and nutritional statuses of the patients are extremely important in the course of this disease. Therefore, we studied the value of the HALP score, which evaluates the immunonutritional status, in this group of patients. Contrary to our expectation, the results of our study indicated similar median HALP scores in survivors and non-survivors. In addition, HALP score was not correlated with mortality. Despite these results, we suppose that the prognostic value of HALP score in FG patients should be the subject of further studies. We believe that our study is important since it is the first one in the literature that investigated the HALP score in predicting prognosis of FG.
Conclusions
FG remains a life-threatening urological emergency despite advances increasing knowledge about its pathophysiology, diagnosis and treatment. High FGSI and ACCI scores, high neutrophil counts, and low hemoglobin, hematocrit, total protein and albumin levels were correlated with mortality. Necrotized surface area was significantly bigger in non-survivors, however involved surface area was not significantly correlated with mortality.
Survivors and non-survivors did not have any significant difference in terms of HALP score, and no correlation was found between the HALP score and mortality. However, since this is the first study in the literature that investigated the significance of the HALP score in FG, we believe that more comprehensive studies should be performed on this subject.
References
Hakkarainen TW, Kopari NM, Pham TN, Evans HL (2014) Necrotizing soft tissue infections: review and current concepts in treatment, systems of care, and outcomes. Curr Probl Surg 51(8):344–362. https://doi.org/10.1067/j.cpsurg.2014.06.001
Tang LM, Su YJ, Lai YC (2015) The evaluation of microbiology and prognosis of Fournier’s gangrene in past five years. Springerplus 4(1):14. https://doi.org/10.1186/s40064-014-0783-8
Bowen D, Juliebø-Jones P, Somani BK (2022) Global outcomes and lessons learned in the management of Fournier’s gangrene from high-volume centres: findings from a literature review over the last two decades. World J Urol 40(10):2399–2410. https://doi.org/10.1007/s00345-022-04139-4
Laor E, Palmer LS, Tolia BM, Reid RE, Winter HI (1995) Outcome prediction in patients with Fournier’s gangrene. J Urol 154(1):89–92
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Roghmann F, von Bodman C, Löppenberg B, Hinkel A, Palisaar J, Noldus J (2012) Is there a need for the Fournier’s gangrene severity index? Comparison of scoring systems for outcome prediction in patients with Fournier’s gangrene. BJU Int 110(9):1359–1365. https://doi.org/10.1111/j.1464-410X.2012.11082.x
Zhu XD, Ding F, Wang GD, Shao Q (2015) Different scoring systems to evaluate the prognosis of Fournier’s gangrene: a comparative study. Nat J Androl 21(8):720–723
Farag CM, Antar R, Akosman S, Ng M, Whalen MJ (2023) What is hemoglobin, albumin, lymphocyte, platelet (HALP) score? A comprehensive literature review of HALP’s prognostic ability in different cancer types. Oncotarget 14:153–172. https://doi.org/10.18632/oncotarget.28367
Han H, Hu S, Du J (2023) Predictive value of the hemoglobin-albumin-lymphocyte-platelet (HALP) index for ICU mortality in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD). Intern Emerg Med 18(1):85–96. https://doi.org/10.1007/s11739-022-03132-4
Hrubaru I, Motoc A, Dumitru C, Bratosin F, Fericean RM, Alambaram S, Citu IM, Chicin GN, Erdelean I, Gorun F, Citu C, Popa ZL (2023) Assessing the utility of hemoglobin, HALP Score, FAR Ratio, and coagulation parameters as predictors for preterm birth. Children (Basel, Switzerland) 10(3):527. https://doi.org/10.3390/children10030527
Benli S, Tazeoğlu D (2023) The efficacy of hemoglobin, albumin, lymphocytes, and platelets (HALP) score in signifying acute appendicitis severity and postoperative outcomes. Updat Surg. https://doi.org/10.1007/s13304-023-01513-8
Chen XL, Xue L, Wang W, Chen HN, Zhang WH, Liu K, Chen XZ, Yang K, Zhang B, Chen ZX, Chen JP, Zhou ZG, Hu JK (2015) Prognostic significance of the combination of preoperative hemoglobin, albumin, lymphocyte and platelet in patients with gastric carcinoma: a retrospective cohort study. Oncotarget 6(38):41370–41382. https://doi.org/10.18632/oncotarget.5629
Aliev SA, Rafiev SF, Rafiev FS, Aliev ES (2008) Fournier disease in surgeon’s practice. Khirurgiia (Mosk) 11:58–63
Radcliffe RS, Khan MA (2020) Mortality associated with Fournier’s gangrene remains unchanged over 25 years. BJU Int 125(4):610–616. https://doi.org/10.1111/bju.14998
Tuncel A, Keten T, Aslan Y, Kayali M, Erkan A, Koseoglu E, Atan A (2014) Comparison of different scoring systems for outcome prediction in patients with Fournier’s gangrene: experience with 50 patients. Scandinavian J Urol 48(4):393–399. https://doi.org/10.3109/21681805.2014.886289
Erol B, Tuncel A, Tok A, Hanci V, Sari U, Sendogan F, Budak S, Aydemir H, Amasyali AS, Yildirim A, Caskurlu T (2015) Low magnesium levels an important new prognostic parameter can be overlooked in patients with Fournier’s gangrene: a multicentric study. Int Urol Nephrol 47(12):1939–1945. https://doi.org/10.1007/s11255-015-1131-9
Erol B, Tuncel A, Hanci V, Tokgoz H, Yildiz A, Akduman B, Kargi E, Mungan A (2010) Fournier’s gangrene: overview of prognostic factors and definition of new prognostic parameter. Urology 75(5):1193–1198. https://doi.org/10.1016/j.urology.2009.08.090
El-Qushayri AE, Khalaf KM, Dahy A, Mahmoud AR, Benmelouka AY, Ghozy S, Mahmoud MU, Bin-Jumah M, Alkahtani S, Abdel-Daim MM (2020) Fournier’s gangrene mortality: a 17-year systematic review and meta-analysis. Int J Infect Dis 92:218–225. https://doi.org/10.1016/j.ijid.2019.12.030
Yanar H, Taviloglu K, Ertekin C, Guloglu R, Zorba U, Cabioglu N, Baspinar I (2006) Fournier’s gangrene: risk factors and strategies for management. World J Surg 30(9):1750–1754. https://doi.org/10.1007/s00268-005-0777-3
Singh A, Ahmed K, Aydin A, Khan MS, Dasgupta P (2016) Fournier’s gangrene. A clinical review. Archivio italiano di urologia andrologia 88(3):157–164. https://doi.org/10.4081/aiua.2016.3.157
Palmer LS, Winter HI, Tolia BM, Reid RE, Laor E (1995) The limited impact of involved surface area and surgical débridement on survival in Fournier’s gangrene. Br J Urol 76(2):208–212. https://doi.org/10.1111/j.1464-410x.1995.tb07676.x
Hahn HM, Jeong KS, Park DH, Park MC, Lee IJ (2018) Analysis of prognostic factors affecting poor outcomes in 41 cases of Fournier gangrene. Ann Surg Treat Res 95(6):324–332. https://doi.org/10.4174/astr.2018.95.6.324
Lin E, Yang S, Chiu AW, Chow YC, Chen M, Lin WC, Chang HK, Hsu JM, Lo KY, Hsu HH (2005) Is Fournier’s gangrene severity index useful for predicting outcome of Fournier’s gangrene? Urol Int 75(2):119–122. https://doi.org/10.1159/000087164
Arora A, Rege S, Surpam S, Gothwal K, Narwade A (2019) Predicting mortality in Fournier gangrene and validating the Fournier gangrene severity index: our experience with 50 patients in a tertiary care center in India. Urol Int 102(3):311–318. https://doi.org/10.1159/000495144
Noegroho BS, Siregar S, Mustafa A, Rivaldi MA (2021) Validation of FGSI scores in predicting Fournier gangrene in tertiary hospital. Res Rep Urol 13:341–346. https://doi.org/10.2147/RRU.S309145
Tuncel A, Aydin O, Tekdogan U, Nalcacioglu V, Capar Y, Atan A (2006) Fournier’s gangrene: three years of experience with 20 patients and validity of the Fournier’s Gangrene severity index score. Eur Urol 50(4):838–843. https://doi.org/10.1016/j.eururo.2006.01.030
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251. https://doi.org/10.1016/0895-4356(94)90129-5
Goyal J, Pond GR, Galsky MD, Hendricks R, Small A, Tsao CK, Sonpavde G (2014) Association of the Charlson comorbidity index and hypertension with survival in men with metastatic castration-resistant prostate cancer. Urol Oncol 32(1):36.e27-36.e3.6E34. https://doi.org/10.1016/j.urolonc.2013.02.015
Radovanovic D, Seifert B, Urban P, Eberli FR, Rickli H, Bertel O, Puhan MA, Erne P (2014) Validity of Charlson comorbidity Index in patients hospitalised with acute coronary syndrome. Insights from the nationwide AMIS plus registry 2002-2012. Heart (British Cardiac Society) 100(4):288–294. https://doi.org/10.1136/heartjnl-2013-304588
Njoku K, Barr CE, Ramchander NC, Crosbie EJ (2022) Impact of pre-treatment prognostic nutritional index and the haemoglobin, albumin, lymphocyte and platelet (HALP) score on endometrial cancer survival: a prospective database analysis. PloS one 17(8):e0272232. https://doi.org/10.1371/journal.pone.0272232
Gao X, Lin B, Lin Q, Ye T, Zhou T, Hu M, Zhu H, Lu F, Chen W, Xia P, Zhang F, Yu Z (2022) A HALP score-based prediction model for survival of patients with the upper tract urothelial carcinoma undergoing radical nephroureterectomy. Bosnian J Basic Med Sci 22(2):280–290. https://doi.org/10.17305/bjbms.2021.6543
Peng D, Zhang CJ, Tang Q, Zhang L, Yang KW, Yu XT, Gong Y, Li XS, He ZS, Zhou LQ (2018) Prognostic significance of the combination of preoperative hemoglobin and albumin levels and lymphocyte and platelet counts (HALP) in patients with renal cell carcinoma after nephrectomy. BMC Urol 18(1):20. https://doi.org/10.1186/s12894-018-0333-8
Xu SS, Li S, Xu HX, Li H, Wu CT, Wang WQ, Gao HL, Jiang W, Zhang WH, Li TJ, Ni QX, Liu L, Yu XJ (2020) Haemoglobin, albumin, lymphocyte and platelet predicts postoperative survival in pancreatic cancer. World J Gastroenterol 26(8):828–838. https://doi.org/10.3748/wjg.v26.i8.828
Xu M, Chen L, Hu Y, Wu J, Wu Z, Yang S, Kang W, He J, Ren W (2023) The HALP (hemoglobin, albumin, lymphocyte, and platelet) score is associated with early-onset post-stroke cognitive impairment. Neurol Sci 44(1):237–245. https://doi.org/10.1007/s10072-022-06414-z
Funding
Authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keten, T., Ozercan, A.Y., Eroglu, U. et al. Can HALP score, a new prognostic tool, take the place of traditional scoring systems in Fournier’s gangrene?. Int Urol Nephrol 55, 2389–2395 (2023). https://doi.org/10.1007/s11255-023-03695-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03695-x