Abstract
Purpose
Disturbance in metabolism and inflammation are the main causes of kidney injury in patients with late stage diabetic nephropathy (DN). Here, we explored whether autophagy was activated in mice with late stage DN and whether it was associated with disturbance in metabolism and inflammation.
Methods
In total, mice were divided into the control group (db/m) and DN group (db/db). Mice were raised for 7 months, and their biochemical indices were measured. Subsequently, their kidneys were collected to detect autophagy and the related nutrient-sensing and inflammatory signaling pathways in late stage DN.
Results
The expression levels of autophagy markers LC3-I and LC3-II were significantly increased in mice with late stage DN, whereas that of autophagy flux marker P62 was significantly decreased, indicating activation of autophagy. Concurrently, mechanistic target of rapamycin was highly expressed as a cellular nutrient-sensing and energy regulator in mice with late stage DN. Additionally, the expression levels of markers of nutrient-sensing signaling pathways adenosine monophosphate-activated protein kinase (AMPK) were increased markedly in mice with late stage DN. Additionally, the expression levels of the marker of nutrient-sensing signaling pathways silent information regulator T1 (SIRT1), the marker of inflammatory signaling pathways high mobility group box protein 1 (HMGB1), and interferon regulatory factor 3 (IRF3) were significantly increased in mice with late stage DN.
Conclusions
The findings of our study indicate that autophagy activation in late stage DN may interfere with nutrient-sensing and inflammatory signaling pathways involving AMPK, SIRT1, HMGB1, and IRF3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic nephropathy (DN) is a common complication of diabetes mellitus. DN is also the leading cause of end-stage renal disease [1], with high incidence among diabetes patients and long disease course [2]. DN is characterized by the persistent elevation of albuminuria, thickening of the glomerular basement membrane, and extracellular matrix aggregation. Disturbance in metabolism and inflammation are the main causes of kidney injury in patients with late stage DN [3].
Dysregulation of autophagy can promote podocytes damage and progressive renal dysfunction in patients with DN [3]. The prevalence of DN is increasing with an increase in the aging population [4], however, the pathogenesis of late stage DN remains unclear [2].
The dysregulation of autophagy is associated with DN pathogenesis. However, most of the previous studies on autophagy in DN models focused on the early stages of DN. For instance, mice with early stage DN were studied 8 weeks after establishing the DN model, which is comparable to DN course in affected patients for six and a half years [5]. However, only a few studies have focused on autophagy in the late stage of DN. This study aimed to explore autophagy activation and its effects on nutrient metabolism and inflammatory pathways in mice with late stage DN.
Materials and methods
Experimental animals
All animal studies were approved by the Animal Ethics Committee of the Chinese People's Liberation Army General Hospital and Military Medical School and complied with the ARRIVE guidelines (No.2018-X14-73). Male db/db (db: a mutation of the leptin receptor gene) (DN group) and male db/m (control group) mice (Jiangsu Jicuikang Biotechnology Co., Ltd.) were raised at the Experimental Animal Center of the Chinese People's Liberation Army General Hospital. All mice were fed common chow and provided ad libitum access to food. Mice were tested for blood glucose levels periodically using the Roche blood glucose meter (ACCU-CHEK Performa). The DN group mice were raised for seven months, and their biochemical indices were measured. After the mice were euthanized, their blood, urine, and kidney tissue were collected.
Blood glucose test
The mice were fasted for 12 h. Mice were weighed and blood was collected from their tail veins. Primary blood glucose levels were measured using the Roche blood glucose meter.
Serum creatinine and urea nitrogen measurement
The mice were fasted for 12 h; then the mice were administered intraperitoneal injection anesthesia and blood samples were collected through the abdominal aorta. The blood samples were incubated at room temperature (25 °C) for 2–3 h and centrifuged at 3000 rpm for 10 min. Serum creatinine and urea nitrogen levels were measured at the Department of Biochemistry of the Chinese People's Liberation Army General Hospital.
Urine creatinine and urine protein test
Urine creatinine levels were detected using a creatinine (urinary) Assay Kit (Cayman, 500701, Ann Arbor, USA) as per the manufacturer’s instructions. Urine protein levels were detected using the Mouse Albumin ELISA Kit (Bethyl, E99-134-190329, USA) following the manufacturer’s instructions.
Periodic acid–Schiff (PAS) stain
Mice were raised for seven months; subsequently, their blood and kidneys were collected under anesthesia. The kidneys were fixed in 10% formalin (ACMEC, Shanghai, China), embedded in paraffin (Beijing Beihua Kangtai Clinical Reagent Co. Ltd, Beijing, China), and sliced to obtain 4-μm-thick sections. The sections were stained with the PAS stain. Images were visualized under an Olympus BX 53 inverted microscope (Tokyo, Japan) and scored from 10 individual fields from each mouse kidney.
Electron microscopy
Kidneys were harvested as done with the PAS stain analysis. After gradient dehydration, acetone was added to the kidneys at 25 °C for 15–20 min. The kidneys were permeated, embedded, cured, and observed using scanning electron microscopy. Kidneys were stained with 3% uranyl acetate-lead citrate and observed using transmission electron microscopy.
Western blotting analysis
Kidneys were harvested and lysed in radioimmunoprecipitation assay lysis buffer (Beyotime, Shanghai, China) containing phenylmethylsulfonyl fluoride (Solarbio, Beijing, China). Using this method, whole cell proteins including nuclear proteins, cytoplasmic proteins, and nuclear transcription factors were obtained. Protein concentrations were determined using the bicinchoninic acid assay. Protein samples were separated using 30% sodium dodecyl sulfate polyacrylamide gel at 120 V and transferred onto nitrocellulose membranes (Pall Corporation, NY, USA) using a Turbo Transfer System (Bio-Rad, Hercules, CA, USA). Membranes were blocked with casein solution (VECTOR) for 1 h at 25 °C, incubated with the appropriate primary antibodies at 4 °C overnight, and washed three times with Tris-buffered saline-Tween 20 (Sigma Aldrich, Burlington, MA, USA). The membranes were then incubated with horseradish peroxidase–conjugated secondary antibodies for 1 h at 25 °C and subsequently washed with Tris-buffered saline-Tween 20. Protein bands were visualized using chemiluminescence with ECL Plus (P1050, APPLYGEN, Beijing, China), as per the manufacturer’s instructions. The primary antibodies used in our study were LC3 (ab131512, Abcam), P62 (ab10912, Abcam), silent information regulator T1 (SIRT1, ab110304, Abcam), the active form of adenosine monophosphate-activated protein kinase (p-AMPK, ab131512, Abcam), high mobility group box protein 1 (HMGB1, ab79823, Abcam), the active form of mechanistic target of rapamycin (p-mTOR, 5536S, Cell Signaling), and interferon regulatory factor 3 (IRF3, ab684871, Abcam).
Statistical analyses
Data are presented as the mean ± standard deviation (mean ± SD). Statistical analyses (Student’s t-tests) and one-way analysis of variance (ANOVA) were performed using GraphPad Prism 8.1. Statistical significance was set at P < 0.05.
Results
Weight, blood glucose levels, and urine albumin-creatinine ratio (UACR) of late stage DN mice
To assess the renal function and biochemical indices in the DN group, 7-month-old mice were euthanized, and their kidneys were harvested. The DN characteristic trait of increased blood glucose levels was exhibited by the DN group mice (P < 0.0001) (Fig. 1b). We further assessed the serum creatinine and serum urea nitrogen levels, which reflect renal function; the 24-h UACR reflects glomerular dysfunction (Fig. 1c–e). The body weights (P < 0.00001) (Fig. 1a), blood glucose levels, and UACR were significantly higher in the DN group mice than in the control group mice, recapitulating human DN pathology.
Renal function and biochemical indices of mice in the control and DN groups. a, b The body weight and blood glucose levels of mice in the control and DN groups. c, d The levels of Scr and Bun in mice with DN were measured. The UACR was determined using enzyme-linked immunosorbent assay. Data are presented as the mean ± standard deviation, *P < 0.05, ***P < 0.001, ****P < 0.0001 (n = 6). DN diabetic nephropathy, Scr serum creatinine, BUN blood urea nitrogen, UACR urine protein-creatinine ratio
Pathophysiological kidney changes in late stage DN mice
In the evaluation of kidney physiology, PAS staining revealed that the glomerular structure and basement membrane were intact and that the capillary lumen was uniform in the control group mice (Fig. 2a). Additionally, the renal tubules were neatly arranged, and no inflammatory cell infiltration was observed in the control group mice. Conversely in the DN group mice, kidneys exhibited glomerular hypertrophy and malformation, mesangial cell proliferation, tubular epithelial degeneration, partial tubular lumen dilatation, and inflammatory cell infiltration (Fig. 2a).
Pathological changes in mice in the control and DN groups. a PAS staining of the kidney sections from the control and DN group mice. Scale bar = 50 μm. b The glomerular podocytes of the control and DN mice were observed using electron microscopy (n = 3). Scale bar = 1 μm. DN diabetic nephropathy, PAS periodic acid–Schiff
Electron microscopy showed that the glomerular podocytes in the control group mice were evenly distributed without evident thickening. However, glomerular podocytes in the DN group mice were markedly thickened, their structure was blurred, and their foot processes were fused (Fig. 2b).
Renal autophagy activation in late stage DN
A growing body of evidence indicates a critical role of autophagy in maintaining podocyte integrity and renal function [6]. Examination of autophagosomes in podocytes was conducted to explore renal autophagy in mice with late stage DN. Using the scanning electron microscopy, autophagosomes were observed by in the DN group mice, but not in the control group mice (Fig. 3a). The autophagy marker LC3 is involved in the initiation and elongation of autophagosomes, whereas the P62 marker is a selective substrate for autophagy that indicates the clearance of autophagosomes [7]. To verify the dysregulation of autophagy in the DN group mice, we measured the expression levels of LC3 and P62. Western blotting showed that the expression level of LC3-II/I significantly increased (P < 0.001) (Fig. 3b, d) whereas that of P62 significantly decreased in the DN group (P < 0.05) (Fig. 3c, e). These results indicate the activation of renal autophagy in late stage DN mice.
Activation of renal autophagy in late stage DN. a The autophagosomes in podocytes of the control and DN group were observed using electron microscopy. Scale bar = 1 μm. b, d Expression levels of LC3-I and LC3-II/I in the kidneys of mice in the control and DN groups, as determined via western blotting. c, e Expression of P62 in the kidneys of mice in the control and DN groups, as determined via western blotting. Data are presented as the mean ± standard deviation, *P < 0.05, ***P < 0.001 (n = 6). DN: diabetic nephropathy
Dysregulation of nutrient-sensing pathways in late stage DN mice
Nutrient-sensing signaling pathways regulate autophagy [8]. One such pathway is the mTOR pathways; a classical nutrient-sensing pathway involved in the negative feedback regulation of autophagy [9]. To explore the mechanism of autophagy activation in the DN group mice, we verified the expression levels of three major nutrient-sensing signaling pathway marker proteins using western blotting and Image J; it is a valid measuring tool for the quantification of western blot bands. p-mTOR expression level was higher in the DN group mice than in the control group mice; however, the difference was not statistically significant (Fig. 4a, b) The results showed significantly lower p-AMPK expression level in the DN group mice than in the control group mice (P < 0.05) (Fig. 4c, d). SIRT1, an important protein of the nutrient-sensing pathway, positively regulates autophagy[10]. The results showed significantly higher SIRT1 protein expression level in the DN group mice than in the control group mice (P < 0.05) (Fig. 4e, f). These results indicate that the activation of autophagy in late stage DN may be related to the activation of the SIRT1 signaling pathway.
Dysregulation of nutrient-sensing signaling pathways. a, b Expression level of p-mTOR in the kidneys of mice in the control and DN groups, as analyzed via western blotting. c, d Expression level of p-AMPK in the kidneys of mice in the control and DN groups, as analyzed via western blotting. e, f Expression level of SIRT1 in the kidneys of mice in the control and DN group, as analyzed via western blotting. Data are presented as the mean ± standard deviation, *P < 0.05. DN, diabetic nephropathy; p-mTOR: active form of mechanistic target of rapamycin; AMPK: adenosine monophosphate-activated protein kinase; SIRT1: silent information regulator T1 (n = 3)
Dysregulation of inflammatory signaling pathways in late stage DN mice
Inflammation plays an important role in DN occurrence and progression [11]. Damage-associated molecular patterns (DAMPs) are key substances that promote inflammatory responses. Endogenous DAMPs are targets of autophagic clearance. HMGB1 and IRF3 are the main cytokines downstream of the DAMP inflammatory pathway. HMGB1 is a very important mediator of the inflammatory response [12] and a key pro-autophagy protein. Western blotting indicated that HMGB1 expression level was significantly high in the DN group mice (P < 0.05) (Fig. 5a, b). DAMPS bind to Toll-like receptors (TLRs). In turn, activation of TLRs can produce a series of inflammatory factors [13]. IRF3 is an important marker for the activation of MyD88-independent signaling pathways and is a target of autophagy degradation [14]. IRF3 expression level was significantly higher in the DN group mice than in the control group mice (p < 0.05) (Fig. 5c, d). These results indicate that some inflammatory pathways are activated in late stage DN.
Dysregulation of inflammatory signaling pathways. a, b Expression level of HMGB1 in the kidneys of mice in the control and DN groups, as analyzed via western blotting. c, d Expression level of IRF3 in the kidneys of mice in the control and DN groups, as analyzed via western blotting. Data are presented as the mean ± standard deviation, *P < 0.05. DN diabetic nephropathy, HMGB1 high mobility group box protein 1, IRF3 interferon regulatory factor 3 (n = 3)
Discussion
In this study, mice with late stage DN were studied to explore the activation of renal autophagy and to verify the possible nutrient-sensing and inflammatory signaling pathways involved.
The results showed significant deterioration of renal function in the DN group mice, which was manifested by a significant increase in the serum creatinine level, blood urea nitrogen level, and UACR. Examination under electron microscopy of the pathological change of the kidney samples obtained from the DN group mice showed thickening of the glomerular basement membrane and mesangial dilation, consistent with previous clinical reports of patients with DN [15].
Previous studies have established that impaired autophagy is related to DN pathogenesis. Abnormal autophagy directly causes renal parenchymal cell damage and plays an important role in DN pathogenesis [10]. Previous studies found that electroacupuncture intervention for DN increased the expression levels of autophagy proteins Beclin-1 and LC3-II in the kidney, decreased the expression level of P62, and increased the number of autophagosomes and autophagic vesicles in podocytes, indicating that electroacupuncture activate renal autophagy expression and effectively reduce kidney damage in DN rats [16] The liver kinase B1 (LKB1)/AMPK/SIRT1 signaling pathway positively regulates SIRT1 expression. A decrease in the activity of LKB1/AMPK/SIRT1 leads to the inhibition of podocyte autophagy, which plays a major role in promoting the etiopathogenesis of DN. Activation of the LKB1/AMPK/SIRT1 signaling pathway regulates podocyte autophagic activity in DN [17]
Although the underlying mechanism of the dysregulation of autophagy in patients with DN remains unclear, many studies have suggested that autophagy regulates renal physiology and pathology. Some pre-clinical studies have shown that autophagy is impaired in the early stages of DN, as manifested by decreased LC3-II/I protein levels and accumulation of P62 in the kidney [10]. In our study, electron microscopy results of kidneys of the DN group mice showed an increase in autophagosomes. Western blotting analysis also indicated that the ratio of LC3-II/I significantly increased and the expression level of P62 significantly decreased. These results suggest that autophagy was consistently activated during late stage DN.
The mTOR signaling pathway classically inhibits autophagy. In the present study, mTOR activation was detected after autophagy activation in the DN group mice. Expression of p-mTOR increased in the DN group mice, but the difference was not statistically significant, which was inconsistent with the trend of autophagy activation. According to our analyses, this may be because autophagy is regulated by multiple signaling pathways, and there is crosstalk between them. Moreover, the AMPK signaling pathway can both activate and inhibit autophagy through interaction with mTOR. In addition, with the prolongation of the DN course, the microenvironment becomes more complex in vivo, and the crosstalk between signaling pathways becomes more intricate. However, the regulation of autophagy by the mTOR signaling pathway in late stage DN remains to be explored. SIRT1, a histone deacetylase, induces hypertrophy and mitochondrial and autophagy dysfunction and decreases overall survival by downregulating AMPK/SIRT1 signals, thereby promoting DN development [18]. AMPK is a nutrient-sensing kinase activated by phosphorylation following ATP depletion. AMPK is a potent positive regulator of autophagy [10]. In our study, the activation of AMPK and SIRT1 was consistent with the results of autophagy activation. These results suggest that these two signaling pathways are activated during late stage DN. The AMPK and SIRT1 signaling pathways are worthy of further study.
Inflammation plays a key role in the development of kidney diseases. The regulation of inflammation by autophagy may be a potential treatment strategy for kidney damage [10]. DAMPs can cause DN inflammation, and autophagy can clear DAMP-damaging factors. HMGB1 is not only a pro-inflammatory factor but is also directly involved in the activation of autophagy in the cytoplasm [19]. IRF3 is a hallmark inflammatory factor that activates inflammatory signaling pathways independent of the MyD88 signaling pathway and is also one of the factors depleted by autophagy. In our study, we found that the protein expression levels of HMGB1 and IRF3 significantly increased in the DN group mice, suggesting that more cytoplasmic HMGB1 may be produced in late stage DN, which directly promotes the accumulation of autophagosomes. HMGB1 should be considered for further exploration of the specific mechanism of the inflammatory pathway that activates autophagy in late stage DN. Immunofluorescence and other methods can be used to verify more specific roles of HMGB1. IRF3 expression level was significantly elevated in our study, suggesting that it may directly induce and participate in the depletion of autophagosomes by aggravating the inflammatory environment in the kidney, which is consistent with the increased autophagic flux represented by P62. IRF3 also inhibits autophagy by activating the mTOR pathway [20]. The roles of IRF3 and the mTOR signaling pathway in late stage DN must be explored further.
In this study, the autophagy markers and involved nutrient-sensing and inflammatory signaling pathways in the DN group mice were investigated, indicating the correlation among late stage DN and autophagy, inflammation, and nutrient-sensing signals. However, whether autophagy interacts with inflammation and nutrient-sensing signals and their potential mechanisms in late stage DN provide premise for future studies.
Conclusion
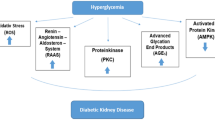
This study explored the activation of renal autophagy in mice with late stage DN. Autophagy activation is related to nutrient-sensing and inflammatory signaling pathways via mTOR, AMPK, SIRT1, HMGB1, and IRF3 (Fig. 6). Our study provides a novel perspective for future studies on late stage DN. Autophagy and inflammatory and nutrient-sensing signaling pathways show promise as clinical targets for late stage DN.
Activation of renal autophagy in late stage DN is related to AMPK and SIRT1 nutrient-sensing and HMGB1 and IRF3 inflammatory signaling pathways. DN diabetic nephropathy, HMGB1 high mobility group box protein 1, AMPK adenosine monophosphate-activated protein kinase, SIRT1 silent information regulator T1, IRF3 interferon regulatory factor 3
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
References
Calle P, Hotter G (2020) Macrophage Phenotype and fibrosis in diabetic nephropathy. Int J Mol Sci 21(8):2806
Tonnies T, Stahl-Pehe A, Baechle C, Castillo K, Yossa R, Holl RW et al (2019) Diabetic nephropathy and quality of life among youths with long-duration type 1 diabetes: a population-based cross-sectional study. Pediatr Diabetes 20:613–621
Jin J, Shi Y, Gong J, Zhao L, Li Y, He Q et al (2019) Exosome secreted from adipose-derived stem cells attenuates diabetic nephropathy by promoting autophagy flux and inhibiting apoptosis in podocyte. Stem Cell Res Ther 10:95
Jankauskas SS, Silachev DN, Andrianova NV, Pevzner IB, Zorova LD, Popkov VA et al (2018) Aged kidney: can we protect it? Autophagy, mitochondria and mechanisms of ischemic preconditioning. Cell Cycle 17:1291–1309
Wilkinson JE, Burmeister L, Brooks SV, Chan CC, Friedline S, Harrison DE et al (2012) Rapamycin slows aging in mice. Aging Cell 11:675–682
Korbut AI, Taskaeva IS, Bgatova NP, Muraleva NA, Orlov NB, Dashkin MV et al (2020) SGLT2 inhibitor empagliflozin and DPP4 inhibitor linagliptin reactivate glomerular autophagy in db/db mice, a model of type 2 diabetes. Int J Mol Sci 21.21(8):2987
Liu H, Wang Q, Shi G, Yang W, Zhang Y, Chen W et al (2021) Emodin ameliorates renal damage and podocyte injury in a rat model of diabetic nephropathy via regulating AMPK/mTOR-mediated autophagy signaling pathway. Diabetes Metab Syndr Obes 14:1253–1266
Towers CG, Wodetzki D, Thorburn A (2020) Autophagy and cancer: Modulation of cell death pathways and cancer cell adaptations. J Cell Biol 219(1):e201909033
Murrell TW Jr (1918) The opportunity offered by regional medical programs. Va Med Mon 1969(96):609
Ding Y, Choi ME (2015) Autophagy in diabetic nephropathy. J Endocrinol 224:R15-30
Samsu N (2021) Diabetic nephropathy: challenges in pathogenesis, diagnosis, and treatment. Biomed Res Int 2021:1497449
Chen X, Ma J, Kwan T, Stribos EGD, Messchendorp AL, Loh YW et al (2018) Blockade of HMGB1 attenuates diabetic nephropathy in mice. Sci Rep 8:8319
Florim GMS, Caldas HC, Goncalves NN, Bueno G, Baptista M, Fernandes-Charpiot IMM et al (2020) Activation of HMGB1-TLR4 pathway and inflammasome contribute to enhanced inflammatory response in extended criteria and kidneys with KDPI >/=85. Transplantation 104:724–730
Wu Y, Jin S, Liu Q, Zhang Y, Ma L, Zhao Z et al (2021) Selective autophagy controls the stability of transcription factor IRF3 to balance type I interferon production and immune suppression. Autophagy 17:1379–1392
Ebrahim N, Ahmed IA, Hussien NI, Dessouky AA, Farid AS, Elshazly AM et al (2018) Mesenchymal stem cell-derived exosomes ameliorated diabetic nephropathy by autophagy induction through the mTOR signaling pathway. Cell 7(12):226
Huang HCL, Wu H, Jin J (2022) Effect of electroacupuncture on renal function and autophagy expression in diabetic nephropathy rat. J Acupunct Res 47(02):108–114. https://doi.org/10.13702/j.1000-0607.20210329
Wang HDD, Zhao S, Si H (2023) Shuiludhuang capsule regulates podocyte autophagy through LKB1/AMPK/Sirt1 signaling pathway in diabetic nephropathy rats. Glob Trad Chin Med 14(12):2142–2148
Wang W, Sun W, Cheng Y, Xu Z, Cai L (2019) Role of sirtuin-1 in diabetic nephropathy. J Mol Med (Berl) 97:291–309
Wang S, Zhang Y (2020) HMGB1 in inflammation and cancer. J Hematol Oncol 13:116
Li Y, Wang C, Wu X, Tian H, Jiang S, Xu T et al (2020) IRF3 and IRF7 contribute to diesel exhaust particles-induced pulmonary inflammation by mediating mTORC1 activation and restraining autophagy in mice. Eur J Immunol 50:1142–1153
Author information
Authors and Affiliations
Contributions
DL and YD designed the study. DL and SY wrote the manuscript. DL performed the experiments. DL, SY and YD supervised the study and edited the manuscript. All authors contributed to the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest associated with the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, D., Yuan, S. & Deng, Y. Interference in the nutrient-sensing and inflammatory signaling pathways by renal autophagy activation in mice with late stage diabetic nephropathy. Int Urol Nephrol 56, 303–311 (2024). https://doi.org/10.1007/s11255-023-03687-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03687-x