Abstract
Introduction and aim
To determine the predictive value of temporal muscle thickness (TMT) measured by ultrasonography in the diagnosing of moderate to severe malnutrition in chronic hemodialysis (CHD) patients.
Materials and methods
Adult patients (> 18 years) who had been on CHD for at least 3 months were included in this cross-sectional study. Patients with infection or inflammatory disease, malignancy, malabsorption syndrome, history of surgery within the last 3 months excluded. Demographic, anthropometric, laboratory parameters, and Malnutrition Inflammation Score (MIS) test results recorded.
Results
A total of 60 chronic hemodialysis (CHD) patients (median age: 66 years, 46.7% female) and 30 healthy individuals (median age: 59.5 years, 55% female) were examined. While there were no significant difference between the dry weight (70 vs 71 kg) and body mass index (BMI) (25.8 vs 26 kg/m2) of the CHD patients and healthy control group, we found that triceps skinfold thickness (TST) (16 vs 19 mm) and left and right TMT (9.6 vs 10.7 and 9.8 vs 10.9 mm) values were significantly lower in the CHD patients (p < 0.001). CHD patients were divided into two groups according to their MIS values as mild (MIS < 6) and moderate/severe malnutrition (MIS ≥ 6). Patients with moderate/severe malnutrition were older, predominantly female and with longer HD vintage. Left (8.8 vs 11 mm) and right TMT (9.1 vs 11.2 mm) values were lower in moderate/severe malnutrition group. In the correlation analysis, a negative correlation was found between TMT and age and MIS, and a positive correlation determined with dry weight, BMI, TST and serum uric acid. In the ROC curve analysis, we found that the optimal cut-off value of left and right TMT for predicting moderate/severe malnutrition were 10.05 and 10.45 mm, respectively. Multivariate regression analysis showed that HD vintage, URR, and TMT values were independently associated with moderate/severe malnutrition.
Conclusion
TMT value measured by ultrasonography in CHD patients can be used as a reliable, easily accessible and non-invasive diagnostic method for predicting moderate/severe malnutrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Protein-energy malnutrition (PEM) is a clinical and measurable nutritional disorder secondary to insufficient and/or irregular protein intake, which contributes to atherosclerosis and inflammation along with the decrease in fat and protein stores in the body, resulting in decreased body performance and impaired functions [1]. Malnutrition is common in chronic hemodialysis (CHD) patients and significantly increases the morbidity and mortality [2,3,4]. PEM is observed in 23–76% of CHD patients [5]. Many parameters are used to evaluate the nutritional status, but there is no sufficient gold standard test alone to determine PEM in this population [6]. There is a view that one of the most valid criteria in the diagnosis of PEM is a decrease in muscle mass [7]. There is evidence in the current literature that a reduction in temporal muscle mass, an anthropometric measure, can be a strong predictor of the presence of malnutrition and mortality in various malignancies [8, 9]. The temporal muscle possesses a high degree of sensitivity to malnutrition in the early stages of depletion, which makes it a valuable tool for assessing nutritional status. Furthermore, its size and strength correlate directly with an individual's overall muscle mass, rendering it a representative marker of muscle health. Additionally, the temporal muscle is conveniently located and can be easily accessed, thereby facilitating repetitive measurements via non-invasive and rapid techniques. As such, the temporal muscle serves as a promising indicator of nutritional status in clinical settings. Therefore, in our study, we aimed to verify the validity and reliability of temporal muscle thickness (TMT) measured by ultrasonography and to show whether it is significantly associated with nutritional status as an indicator of malnutrition in patients receiving CHD treatment.
Materials and methods
Study design and ethics committee approval
This is a single-center, cross-sectional study. Data were collected within 6 months between December 2018 and May 2019. Written informed consent was obtained from the patients, which included a detailed explanation of the objectives of the study and the methods to be used. Ethics committee approval was obtained from our hospital (decision number 159 dated 14.11.2018).
Inclusion and exclusion criteria
A total of 60 patients over the age of 18 who had been regularly receiving CHD treatment for at least 3 months due to end-stage renal disease were included in this study. Those who were temporarily on dialysis due to acute renal failure (ARF), those with a history of hospitalization and surgery within the last 3 months, who have a significant infection or inflammatory disease, nephrotic proteinuria, end-stage liver disease, metastatic malignancy or malabsorption syndrome were excluded. To compare anthropometric measurements and TMT values between chronic hemodialysis patients and healthy individuals, a control group (n = 30) without CKD was included in our study.
Hemodialysis method
HD was applied to the patients by using bio compatible HD membranes with dialysate containing standard bicarbonate and 140 mEq/l sodium. While blood flow rates varied between 300 and 350 ml/min, the dialysate flow rate was kept constant at 500 ml/min. None of the patients used the dialyzer again, and no bacteria or pyrogen growth was observed in the dialysate obtained from water by reverse osmosis. To calculate the given dialysis dose (URR and spKt/V), the post dialysis plasma urea levels of the same dialysis session were measured by the Daugirdas method.
Data collection
The first evaluation including demographic, anthropometric and biochemical data was performed for all patients in December 2018. Demographic data of the patients (age, gender, HD duration, primary etiology of renal disease, vascular access type), laboratory parameters and dialysis adequacy measurements (URR and spKt/V) were obtained retrospectively by examining the patient files. Anthropometric measurements (dry weight, BMI, TST, TMT) were calculated by examining the patients 15–30 min after the end of the mid-week HD session. TST was measured at the back of the arm without AV fistula, from the midpoint between the olecranon and the acromion, with the arms released from the side, by applying standard pressure by clamping the skin with the Saehan Skinfold Caliper. The measurement was repeated three times and average values were obtained. After fasting overnight, predialysis (before the mid-week session) venous blood samples were taken from all subjects in the morning. All biochemical analyzes including serum urea, creatinine, uric acid, sodium, potassium, calcium, phosphorus, intact parathormone (iPTH), hemoglobin, ferritin, albumin, total cholesterol and triglyceride were performed by automated procedures. Malnutrition inflammation score (MIS) is a reliable scoring system that has been used to evaluate the nutritional status in CHD patients and has been proven to detect malnutrition effectively. Scoring is made by looking at nutritional history, physical examination, BMI and laboratory data. It consists of four parts and 10 questions. Each question is given a score between 0 (normal) and 3 (severe malnutrition). Scoring is made between 0 (normal) and 30 (severe malnutrition). Total score 0, 1, 2 normal; 3–5 light; 6–8 moderate and > 9 is considered as severe malnutrition. High scores reflect the severity of malnutrition and inflammation. It has been proven that high MIS scores are predictors of morbidity and mortality in these patients [10, 11]. TMT was measured by a single observer blinded to the MIS or other relevant characteristics of the patient. Toshiba (Toshiba Medical Systems Company, Otawara, Japan) Aplio 500 USA device and 12 MHz linear probe were used for measurement of TMT in a relaxed state. The linear transducer was placed in the temporal fossa perpendicular to the muscle plane with gently pressure, approximately 2 cm behind and upper part of the lateral edge of the eyelid bilaterally. The thickness of the middle part of the temporal muscle was measured. During the collection of ultrasonographic images, three measurements were recorded for each muscle. The average of three measurements for the right and left sides was taken as the final data [12].
Statistical analysis
SPSS 20.0 software (SPSS Inc., Chicago, USA) was used for statistical analysis. Descriptive statistics were presented as median (IQR: interquartile range (25–75%)), frequency distribution and percentage. Pearson Chi-Square Test and Fisher's Exact Test were used to evaluate categorical variables. The suitability of the variables to normal distribution was examined with analytical methods (Kolmogorov–Smirnov/Shapiro–Wilk Test). Mann–Whitney U Test was used for statistical significance between two independent groups for variables that were not found to conform to normal distribution. The relationship between variables was evaluated using the Spearman Correlation Test. The correlation coefficient between 0 and 0.25 was accepted as a “weak level” relationship, 0.26–0.50 as a “moderate” relationship, 0.51–0.75 as a “strong” relationship and 0.76–1.00 as a "very strong" relationship. The diagnostic decision-making feature of left and right TMT in predicting moderate/severe malnutrition was evaluated by ROC Curve Analysis. In multivariate analysis, independent predictors were examined using Logistic Regression analysis to predict moderate/severe malnutrition using possible factors identified in previous analyzes. Hosmer–Lemeshow test was used for model fit. Statistical significance level was accepted as p < 0.05.
Results
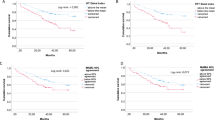
A total of 60 chronic hemodialysis (CHD) patients (median age: 66 (IQR 53–74) years, 46.7% female) and 30 healthy individuals (control group; median age: 59.5 (IQR 54–70.8) years, 55% female) were examined. While there were no significant difference between the dry weight (70 vs 71 kg) and BMI (25.8 vs 26 kg/m2) of the CHD patients and healthy control group, we found that TST (16 vs 19 mm) and left and right TMT (9.6 vs 10.7 and 9.8 vs 10.9 mm) values were significantly lower in the CHD patients (p < 0.001). The median HD vintage of the patients was 42.5 (IQR 14.5–95.8) months and 23.3% had diabetes mellitus (DM). Looking at the type of vascular access; 61.7% of the patients had arteriovenous fistula (AVF), 35% had a permanent tunneled catheter (PTC) and the remaining 3.3% had arterio-venous graft (AVG). Considering the primary etiology of the CKD patients; it was observed that hypertension took the first place with 43.3%, followed by diabetes mellitus with 23.3% and chronic glomerulonephritis with 3.3% (Table 1). The median MIS score of the patients examined was 7 (IQR 5–9), while the minimum score was 3 and the maximum score was 15. It was observed that all of the patients had malnutrition (31.7% mild, 68,3% moderate-severe). The patients were divided into 2 groups according to their MIS as mild (MIS < 6, n = 19) and moderate-severe malnutrition (MIS ≥ 6, n = 41). Compared to those with mild malnutrition group, patients with moderate/severe malnutrition were found to be older, predominantly female and had a longer HD vintage (p = 0.027; p = 0.031; p = 0.004, respectively). No statistically significant difference was found in terms of primary etiology and vascular access type (p > 0.05) (Table 1). Laboratory parameters of all patients and malnutrition groups are presented in Table 2. URR, spKt/V and serum uric acid values were found to be significantly lower in patients with moderate/severe malnutrition (p = 0.015; p = 0.024; p = 0.006, respectively). No statistically significant difference was found in terms of other laboratory values (Table 2). Anthropometric measurements and TMT results of all patients and groups are presented in Table 3. The median dry weight, BMI and TST values of all patients were 70 kg, 25.8 kg/m2 and 16 mm, respectively. Patients with moderate/severe malnutrition had significantly lower TST values (p = 0.029). There were no statistically significant difference in terms of dry weight and BMI. The median (IQR) value of the left and right TMT of all patients were 9.6 (IQR 8.5–11) and 9.8 (IQR 8.7–11.2) mm, respectively. Both left and right TMT values were significantly lower in moderate/severe malnutrition group (respectively; p < 0.001; p < 0.001) (Table 3). Table 4 shows the correlation analysis between left and right TMT with demographics, anthropometric measurements, laboratory data and MIS values of all patients. There was a statistically significant relationship between TMT values with age (r = − 0.50), MIS (r = − 0.43), bicarbonate value (r = − 0.29) in the negative direction (moderate); dry weight (r = 0.38), BMI (r = 0.36), TST (r = 0.33) and serum uric acid value (r = 0.41) in the positive direction (moderate) (p < 0.05). It was determined that both left (AUC 0.81, 95% CI 0.69–0.93) and right (AUC 0.82, 95% CI 0.70–0.94) TMT had a diagnostic value in predicting moderate/severe malnutrition (p < 0.05). In the ROC curve analysis, we found that the optimal cut-off value of left TMT for predicting moderate/severe malnutrition was 10.05 mm with 73.2% sensitivity and 73.7% specificity (positive and negative predictive values were 85.7% and 56%, respectively). Optimal cut-off value of right TMT for predicting moderate/severe malnutrition was 10.45 mm with 78% sensitivity and 73.7% specificity (positive and negative predictive values were 86.5% and 60.9%, respectively) (Fig. 1, Table 5). Table 6 shows the multivariate logistic regression analysis of the independent parameters which predicts moderate/severe malnutrition. HD vintage, URR and TMT were found to be independent predictors of moderate/severe malnutrition, even after adjusting for confounding factors such as age, gender and serum uric acid values (Table 6).
Discussion
Mortality rates are unacceptably high in patients with CHD. The presence of PEM is a modifiable risk factor that has been shown to be associated with mortality [10]. There is evidence in the current literature that a decrease in temporal muscle mass may be a strong predictor of malnutrition and mortality in various malignancies [8, 9]. Thus, we aimed to determine the predictive value of temporal muscle thickness (TMT) measured by ultrasonography in the diagnosing of moderate to severe malnutrition in chronic hemodialysis (CHD) patients. As a result of our study, we found that TMT measured by ultrasonography, as a non-invasive, simple and easily accessible evaluation method in CHD patients, is an independent diagnostic tool in predicting moderate/severe malnutrition.
In the literature, PEM was observed at a rate of 23–76% in CHD and 18–50% in peritoneal dialysis patients [5]. In our study, we observed that all of the patients had malnutrition (31.7% mild, 68,3% moderate-severe). We think that the reason for this high prevalence of malnutrition is that as a tertiary center, we followed up relatively old patients with multiple comorbidities and longer HD vintage.
We found that patients with moderate/severe malnutrition were older, predominantly female and had a longer HD vintage. These findings are consistent with the literature. The reason is thought to be due to the presence of comorbid diseases contributing to hypercatabolism in elderly patients, inadequate dialysis, socioeconomic status and decreased food intake due to psychological factors. Physiological deficiencies that develop with aging also increase the rate of malnutrition [13]. In a study conducted by Cianciaruso B. et al. with 487 chronic HD patients undergoing regular dialysis, malnutrition rates were found to be 27% in the 18–40 age group, 31% in the 41–64 age group and 51% in the age group 65 and over. It has been observed that the rate of malnutrition increases with advancing age [14]. As in our study, the reason for the higher malnutrition rate in patients who have received HD treatment for a long time is that although malnutrition is common in dialysis patients, the dialysis technique itself can contribute to nutritional deficiencies. For example, HD patients have higher CRP, inflammation, oxidative stress and increased protein muscle breakdown compared to other CKD patients. This has been attributed to the stimulation of an inflammatory pathway when blood comes into contact with the dialyzer membrane [15, 16]. It has been shown in the literature that, because of the loss of amino acids with dialysis, the protein intake of patients who undergo intensive home dialysis should be increased [17]. In our study, we found a higher rate of malnutrition in female gender, in accordance with the literature. As a result of the study conducted by Fatemeh Espahbodi et al. with 105 dialysis patients, malnutrition was not observed in males whereas malnutrition was found in different degrees in females [18]. Likewise, in a study conducted by Farrokhi R. et al. in Iran, malnutrition was shown to be significantly higher in female HD patients [19].
We found a significant relationship between the presence of malnutrition and TST, but we did not find a significant relationship between malnutrition and BMI or dry weight. The reliability of classical anthropometric measurements decreases due to reasons such as loss of lean muscle mass and changes in total body water in this population. Despite malnutrition and muscle loss, weight and BMI may remain the same or even increase due to the presence of hypervolemia. Our results suggest that anthropometric measurements alone are not sufficient in evaluating malnutrition in ESRD patients and these patients should be evaluated with a holistic approach with anamnesis, physical examination, dietary habits, biochemical parameters and scoring systems. If deemed necessary, advanced tests such as bioimpedance analysis (BIA) and dual energy X-ray absorptiometry (DEXA) can be used to more clearly determine the lean muscle mass, water and fat ratios of these patients [20].
It has been shown that increased dialysis adequacy in CHD patients, that is higher URR and spKt/V values, improves morbidity and mortality in chronic HD patients [21]. To say that patients have sufficient dialysis, URR should be > 65% and spKt/V > 1.2 (optimally 1.4). Even if all patients included in our study were at target values in terms of dialysis adequacy, we found that patients with moderate/severe malnutrition had significantly lower URR and spKt/V values than those with mildly malnutrition group. This situation is also compatible with the literature. Fransaidan Charra et al. Divided their patients into two groups as high and low Kt/V and reported that those with a Kt/V of 1.97 ± 0.35 live longer than those with a Kt/V of 1.35 ± 0.16 [22]. Parker et al. reported that the mortality rate decreased within creasing Kt/V from 1.18 ± 0.28 to 1.46 ± 0.30 in the 3-year follow-up with 800 patients [23]. In addition, as a dialysis adequacy indicator, the URR above 65% at each dialysis session decreases the mortality rate [24, 25]. Since it is observed that nutritional status improves as dialysis sufficiency increases in HD patients, HD patients must be followed up regularly in terms of nutritional status and dialysis adequacy, and necessary arrangements should be made [25]. The sufficient number and duration of dialysis sessions in HD patients seriously affects the morbidity and mortality of the patient. It has been proven in the studies that frequent (5–7 days a week) and/or prolonged (6–8 h/session) HD treatment increases the dialysis efficiency, decreases the mortality rate compared to conventional dialysis (3 days/week, 4 h/session), decreases the risk of left ventricular hypertrophy, hypertension, cardiovascular events, increases physical wellbeing, prevents complications such as anemia and bone disease, virtually eliminates the need for erythropoietin and phosphorus binding medication and improves nutritional status [26].
In the literature, it has been shown that the incidence of malnutrition is increased in diabetic patients and/or hemodialysis using indwelling catheters [27, 28]. In our study, we found no significant difference between the groups in terms of the type of vascular access used for HD, the primary etiology of ESRD and the presence of DM, although the rate of DM and the use of catheters was slightly higher in patients with moderate/severe malnutrition. We think that this result is due to the limited number of our patients.
Serum albumin value is still one of the most important parameters in the determination and follow-up of malnutrition in CHD patients. However, in our study, we found that although most of our patients had moderate/severe malnutrition according to the MIS scores, serum albumin levels were within the target range (median for all patients: 3.8 (3.5–3.9) g/dl). In addition, we did not see a significant difference in serum albumin levels between those with mild malnutrition and those with moderate/severe malnutrition (3.9 g/dl versus 3.8 g/dl, respectively). Again, in the correlation analysis, we did not find a relationship between TMT and serum albumin values. In the study conducted by Tapiawala et al. with 81 patients in India, no significant relationship was found between serum albumin level and malnutrition in accordance with our findings [29]. However, a significant association was found with 52 patients in an American study by Eustace et al. [30]. Albumin is a negative acute phase reactant. Acidemia and volume status are other factors affecting serum albumin level. When we consider serum albumin level as a nutritional indicator, it is necessary to evaluate the clinical condition of the patient such as comorbidities, dialysis adequacy, acid–base and volume status [31]. We would like to emphasize that it is not sufficient to use serum albumin value alone when evaluating nutritional status in patients receiving CHD treatment according to results we obtained in our study. Serious malnutrition may still exist in these patients, even if serum albumin levels are within target ranges.
There is no gold standard test for detecting malnutrition. There is a need for an inexpensive, easy-to-apply, reliable and sensitive method. It should not be affected by non-nutritional factors and should be able to normalize when nutritional status improves [6]. For this purpose, an objective parameter recently determined to define the fragility of patients is the determination of skeletal muscle mass. Studies have shown that there is a relationship between skeletal muscle mass and TMT. Temporal muscle loss is one of the physical signs of the loss of skeletal muscle mass in malnutrition and can manifest itself with the depression developing in the temporal fossa [32, 33]. It is believed that a decrease in muscle mass is one of the most valid criteria for diagnosing PEM in patients with CHD [7]. There is evidence in the current literature that a reduction in temporal muscle mass, an anthropometric measure, may be a strong predictor of malnutrition and mortality [8, 34]. However, these studies have been conducted on patients with malignancy. Temporal muscle wasting is one of the physical manifestations of the loss of skeletal muscle mass that occurs in malnutrition [12]. Imaging methods such as tomography and MRI can be used to evaluate skeletal muscle mass. In the study of Furtner et al., a correlation was shown with the presence of malnutrition in cancer patients by measuring TMT with MRI. In this study conducted with 146 metastatic melanoma patients, survival rate was found to be decreased in patients with TMT median value measured by MRI of < 5.8 mm. It has been observed that every 1 mm decrease in TMT value is associated with a 27.9% increase in mortality. In our study, the median of left TMT measured by ultrasonography was 9.6 (IQR 8.5–11.0) mm, while the median of right TMT was 9.8 (IQR 8.7–11.2) mm. We found that the left (8.8 versus 11 mm) and right TAC (9.1 versus 11.2 mm) values were statistically significantly lower in patients with moderate/severe malnutrition compared to those with mild malnutrition (p < 0.001). In the study of Furtner et al., it was observed that as the age of the patient increased, the mean TMT value decreased [8]. In our study, we found that there was a significant negative correlation between the left and right TMT values of all patients and age in the correlation analysis. This may be due to the development of physical disability in the elderly, the presence of hypercatabolism, a decrease in food intake due to different socioeconomic and psychological factors and a decrease in muscle mass with age [13]. We found a statistically significant negative correlation between the left and right TMT values and MIS scores of the patients. Again, in the study conducted by Furtner et al. 146 patients diagnosed with metastatic melanoma, a negative correlation was found between the diagnosis specific graded prognostic assessment (DS-GPA) scoring used in the detection of malnutrition and TMT. We found that while there was no difference in dry weight and BMI between malnutrition groups, TST value was lower in the moderate/severe malnutrition group. In the correlation analysis, there was a statistically significant positive correlation between left and right TMT values and dry weight, BMI and TST values of all patients. In the study of Furtner et al., no relationship was found between TMT and BMI. Because TMT can reflect skeletal muscle mass, but BMI focuses only on the weight of the patient, regardless of body composition. Therefore, BMI cannot define sarcopenia in an obese patient population [35]. As a result of our study, we think that using anthropometric measurements such as BMI, dry weight and TST alone in determining malnutrition may be misleading. In the determination of nutritional status in CHD patients, the measurement of TMT performed by ultrasonography can be used as a reliable parameter since it is not affected by the volume state and represents the skeletal muscle mass better. As a result of our research, we determined that right and left TMT values are reliable for predicting moderate/severe malnutrition according to the ROC curve analysis. While sensitivity was calculated as 73.2%, specificity 73.7%, positive predictive value 85.7% and negative predictive value 56% according to the 10.05 mm cut-off value determined for the left TMT in predicting moderate/severe malnutrition; sensitivity was calculated as 78%, specificity 73.7%, positive predictive value 86.5% and negative predictive value 60.9% according to the cut-off value of 10.45 mm determined for the right TMT. In multivariate logistic regression analyses, it was observed that hemodialysis vintage, URR, left and right TMT had independent effects in predicting moderate/severe malnutrition. In an oral presentation held at the 2019 National Neurology Congress, Yılmaz et al.'s research with 93 patients with acute ischemic stroke revealed diagnosis of sarcopenia with a TMT value below 11.5 mm measured by ultrasonography with 42% sensitivity and 92% specificity and it has been concluded that measurement of TMT by ultrasonography is a useful index and a useful method in the diagnosis of sarcopenia [36].
There is no study in the literature regarding the role of TMT measurement in determining malnutrition in CHD patients. In our knowledge, this study is the first study conducted with Turkish CHD patients on this subject and is the first cut-off value determined for the TMT measurement value. The limitations of our study; relatively small number of patients, evaluation with a single measurement as it is a cross-sectional study, not following the nutritional status and changes in TMT values with repeated measurements, not evaluating the dietary habits of the patients and since we are a tertiary center, we have examined a specific patient group (elderly and multiple comorbidities), so it may not reflect the general HD population.
Conclusion
TMT measured by ultrasonography is an reliable, easily applicable, non-invasive and new method which can independently predict moderate/severe malnutrition in CHD patients. Patients with TMT < 10.05 mm need to be examined and followed up in terms of malnutrition. Further prospective studies with a larger number of patients are needed, regarding the role of TMT value in diagnosis, follow-up and treatment approach of malnutrition, which is an important problem affecting mortality in chronic HD patients.
References
Kalantar-Zadeh K et al (2003) Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis 42(5):864–881
Kalantar-Zadeh K, Kopple JD (2001) Relative contributions of nutrition and inflammation to clinical outcome in dialysis patients. Am J Kidney Dis 38(6):1343–1350
Qureshi AR et al (2002) Inflammation, malnutrition, and cardiac disease as predictors of mortality in hemodialysis patients. J Am Soc Nephrol 13(suppl 1):S28–S36
Öznur K (2018) The relationship between malnutrition, inflammation and cannulation pain in hemodialysis patients. Medeniyet Med J 33(1):33–40
Stenvinkel P et al (2000) Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant 15(7):953–960
Amparo FC et al (2014) Diagnostic validation and prognostic significance of the Malnutrition-Inflammation Score in nondialyzed chronic kidney disease patients. Nephrol Dial Transplant 30(5):821–828
Axelsson J et al (2006) Are insulin-like growth factor and its binding proteins 1 and 3 clinically useful as markers of malnutrition, sarcopenia and inflammation in end-stage renal disease? Eur J Clin Nutr 60(6):718
Furtner J et al (2018) Temporal muscle thickness is an independent prognostic marker in melanoma patients with newly diagnosed brain metastases. J Neurooncol 140(1):173–178
Furtner J et al (2017) Survival prediction using temporal muscle thickness measurements on cranial magnetic resonance images in patients with newly diagnosed brain metastases. Eur Radiol 27(8):3167–3173
Kara E et al (2016) The predictive value of malnutrition-inflammation score on 1-year mortality in Turkish maintenance hemodialysis patients. Clin Nephrol 86(2):94
Kalantar-Zadeh K et al (2001) A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am J Kidny Dis 38(6):1251–1263
Hasegawa Y et al (2019) Temporal muscle thickness as a new indicator of nutritional status in older individuals. Geriatr Gerontol Int 19(2):135–140
Chauveau P et al (2001) Factors influencing survival in hemodialysis patients aged older than 75 years: 2.5-year outcome study. Am J Kidney Dis 37(5):997–1003
Cianciaruso B et al (1995) Nutritional status in the elderly patient with uraemia. Nephrol Dial Transplant 10(supp6):65–68
Owyang C, et al. (1979) Gastrointestinal hormone profile in renal insufficiency. In: Mayo Clinic Proceedings.
Sylvestre LC et al (2007) The malnutrition and inflammation axis in pediatric patients with chronic kidney disease. Pediatr Nephrol 22(6):864–873
Spanner E et al (2003) The impact of quotidian hemodialysis on nutrition. Am J Kidney Dis 42:30–35
Espahbodi F, Khoddad T, Esmaeili L (2014) Evaluation of malnutrition and its association with biochemical parameters in patients with end stage renal disease undergoing hemodialysis using subjective global assessment. Nephro Urol Mon. https://doi.org/10.5812/numonthly.16385
Farrokhi R, Majdzadeh N, Dehghani M (2004) Assessing protein intake through urea production rate in chronic hemodialysis patients of Kerman in 2001. J Kerman Univ Med 11(1):188–196
Bansal S, Cho FME, Beddhu SJU (2018) Assessment of nutritional status in hemodialysis patients. https://www.uptodate.com/contents/assessment-of-nutritional-status-in-patients-on-hemodialysis
Schulman G (2004) Poor nutritional status and inflammation: the dose of dialysis in hemodialysis patients: impact on nutrition. Semin Dial 17:479–488
Charra B et al (1992) Survival as an index of adequacy of dialysis. Kidney Int 41(5):1286–1291
Parker TF et al (1994) Survival of hemodialysis patients in the United States is improved with a greater quantity of dialysis. Am J Kidney Dis 23(5):670–680
Riella MC (2000) Malnutrition in dialysis: malnourishment or uremic inflammatory response? Kidney Int 57(3):1211–1232
Daugirdas JT, Kjellstrand CM (1994) Chronic hemodialysis prescription: a urea kinetic approach. Handbook Dial. 4:146–170
Kalender B, et al (2002) The relationship between nutritional status and adequacy of dialysis in hemodialysis patients. Cerrahpaşa J Med 33(4):223–230
Cano NJ et al (2002) Malnutrition in hemodialysis diabetic patients: evaluation and prognostic influence. Kidney Int 62(2):593–601
Combe C et al (2004) Kidney disease outcomes quality initiative (K/DOQI) and the dialysis outcomes and practice patterns study (DOPPS): nutrition guidelines, indicators, and practices. Am J Kidney Dis 44:39–46
Tapiawala S et al (2006) Subjective global assessment of nutritional status of patients with chronic renal insufficiency and end stage renal disease on dialysis. Japi 54:923–926
Eustace JA et al (2000) Randomized double-blind trial of oral essential amino acids for dialysis-associated hypoalbuminemia. Kidney Int 57(6):2527–2538
Gama-Axelsson T, Heimbürger O, Stenvinkel P, et al (2012) Serum albumin as predictor of nutritional status in patients with ESRD. Clin J Am Soc Nephrol 7(9):1446–1453
Piccoli A (1998) Identification of operational clues to dry weight prescription in hemodialysis using bioimpedance vector analysis. Kidney Int 53(4):1036–1043
Yılmaz E, Arsava EM, Topcuoglu M (2019) Temporal muscle ultrasonographic morphometry: a new measure of sarcopenia in stroke. In: Proceedings 55th National Neurology Congress, Oral presentation (SS-91) p 52, Antalya-Turkey
Campbell KL (2007) Nutritional management in pre-dialysis chronic kidney disease: An investigation of methods for nutritional assessment and intervention in pre-dialysis chronic kidney disease. Queensland University of Technology.
Iorember FM (2018) Malnutrition in chronic kidney disease. Front Pediatr 6:161
Kaysen GA et al (2004) Inflammation and reduced albumin synthesis associated with stable decline in serum albumin in hemodialysis patients. Kidney Int 65(4):1408–1415
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are not any non-financial competing interests we would like to declare in relation to this paper. We have not any other financial competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Demirbaş, S., Demirbaş, Z.A., Beyazal, M. et al. The predictive value of temporal muscle thickness measured by ultrasonography for detecting moderate to severe malnutrition in chronic hemodialysis patients. Int Urol Nephrol 55, 2877–2885 (2023). https://doi.org/10.1007/s11255-023-03577-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03577-2