Abstract
Purpose
In this study, we aimed to compare the results of split-cuff nipple and modified Lich-Gregoir ureteroneocystostomy, which are the most commonly used techniques in stage ≥ 3 iatrogenic distal ureteral injuries.
Methods
The files of patients who were treated for iatrogenic distal ureteral injuries in our clinic between January 2013 and January 2019 were retrospectively reviewed. A total of 60 patients who underwent either intra-vesical split-cuff nipple ureteroneocystostomy (Group A) or extra-vesical modified Lich-Gregoir ureteroneocystostomy (Group B) operations were included in the study. The success of ureteroneocystostomy was defined as no additional surgery requirement, no progression of hydronephrosis on imaging, and normal contrast transition on imaging.
Results
Thirty-four patients underwent split-cuff nipple and 26 patients underwent modified Lich-Gregoir ureteroneocystostomy. The treatment was successful in 53 (88.3%) patients and failed in seven (11.7%). Complications occurred in 19 (31.7%) patients, of whom 14 (23.3%) had minor and five (8.3%) had major complications. The rate of postoperative complications was significantly higher in Group A than in Group B (p = 0.019). There was no significant difference between Group A and Group B in terms of the success ratio (p = 1), rate of major complications (p = 0.372), and postoperative hospitalization times (p = 0.254).
Conclusion
In this study, a higher complication rate was found in patients with iatrogenic ureteral injuries who underwent ureteroneocystostomy with the split-cuff ureteral nipple technique compared to those who underwent this operation with the modified Lich-Gregoir technique. However, no significant difference was observed between these two techniques in terms of treatment success and major complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ureteral injuries constitute 1–2.5% of urinary system injuries, and 80% of ureteral injuries are due to iatrogenic trauma [1]. Iatrogenic ureteral injuries mostly develop as a result of abdominal and pelvic operations. Rarely, they have also been described after lumbar disk surgery [2]. Iatrogenic ureteral injuries can also occur during open, laparoscopic, robot-assisted laparoscopic, or endoscopic surgery and can lead to complications such as loss of renal function, ureteral stenosis, urinoma, peri-ureteral abscess, sepsis, urinary fistula, and acute kidney failure.
There are no characteristic signs and symptoms of ureteral injuries; therefore, they can sometimes be overlooked [3, 4]. They usually cause hematuria, flank pain, ecchymosis, or hypotension. Hematuria is reported at a rate of 44% [5]. Diagnostic methods that can be used in ureteral injuries include computed tomography (CT) urography, intraoperative intravenous pyelography (IVP), retrograde pyelography (RGP), ureteroscopy, and ureteral exploration. The American Urological Association recommends abdominopelvic CT with an intravenous contrast agent with 10-min delayed images (CT urography) for an accurate evaluation of the ureter [6]. Ureteral injuries should be considered in the presence of contrast extravasation, delayed pyelogram, urinoma, hydronephrosis, and/or contrast transmission distal to the suspected injury site on CT urography [7, 8]. Intraoperative IVP can provide anatomical and functional information about ureteral injuries. For more anatomical information, RGP with intraoperative cystoscopy is helpful. If ureteral damage is suspected during open surgery, direct vision can be obtained by ureteral exploration. The extravasation of substances such as intravenous methylene blue and indigo carmine contributes to the detection of these injuries.
The European Association of Urology guideline recommends immediate repair in complete ureteral injuries if the patient is stable. If the patient is unstable, percutaneous nephrostomy placement is more appropriate than a ureteral double-J stent, since general anesthesia is not required and can be performed outside the operating room. Reconstructive procedures can be postponed until the patient is stable [1]. While 4% of ureteral injuries are managed conservatively, surgical intervention is required in the remaining 96% of cases [9]. According to the classification of the American Association of Trauma Surgery, ureteral injuries are divided into five stages [10]. Stage 1 and 2 ureteral injuries can be repaired with a ureteral double-J catheter or a nephrostomy tube, while surgical repair is recommended in those with stage ≥ 3 injuries [11, 12].
Ureteral injuries occur more frequently in the distal ureteral segment [13], and for their treatment, many surgical re-implantation methods can be applied [intravesical: split-cuff nipple (SCN), Politano-Leadbetter, and Cohen; extravesical: Lich-Gregoir ureteroneocystostomy). Iatrogenic distal ureteral injuries can lead to renal unit loss and potentially life-threatening complications. However, due to their rarity, there are not sufficient data in the literature concerning which method is more successful and less complicated. Therefore, in our study, we aimed to compare the long-term results of SCN and modified Lich-Gregoir (MLG) ureteroneocystostomy as the most commonly used techniques in stage ≥ 3 distal iatrogenic ureteral injuries. We hypothesized that the two techniques would have comparable complications or outcomes.
Materials and methods
Study design
This study was designed retrospectively and approved by the Institutional Review Board (IRB no: 21263603–604.02.01–161,838, January 7, 2021). Between January 2013 and January 2019, the files of patients with distal ureteral injuries due to abdominal, urologic, or pelvic surgery were reviewed in our clinic. The patients were divided into the two groups as those who underwent intravesical SCN ureteroneocystostomy (Group A) and extravesical MLG ureteroneocystostomy (Group B).
The patients’ demographic characteristics, renal functions before and after repair, time between primary surgery and ureteroneocystostomy, perioperative characteristics (stage of injury and surgical techniques applied), post-operative hospital stay, and perioperative–postoperative complications (using the modified Clavien grading system) were noted. Patients with a follow-up period of less than 24 months, history of urothelial cancer, or ureteral complications due to tumor progression, and those who received postoperative radiotherapy were excluded from the study. Sixty patients aged > 18 years, who had stage ≥ 3 iatrogenic distal ureteral injuries, were included in the study. None of the patients in the study population had bilateral injuries.
Surgical techniques
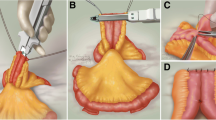
In distal ureteral injuries, debridement was applied to the devascularized-fibrotic ureter segments, especially in thermal injuries. The distal end of the ureter was spatulated. The blood flow to the distal segment restricted by the primarily damaged ureter was managed with ureteral re-implantation (SCN or MLG ureteroneocystostomy).
In intravesical SCN ureteroneocystostomy, 2 cm of the ureter was passed through the neohiatus and taken into the bladder. Seromuscular ureteral tissue was fixed to the neohiatus within the bladder. The most distal of the ureter was reversed and fixed to the urothelium with sutures.
In extravesical MLG ureteroneocystostomy, the bladder was dissected caudally toward the neohiatus. Detrusorrhaphy was applied along the submucosal tunnel, which was planned with sharp dissection. The ureter was anastomosed to the opened window in the mucosa and placed in the submucosal tunnel. The detrusor fibers were closed over the ureter. As a modification, a ureteral anastomosis was performed on the neohiatus.
In all the operations, a 4.8-Fr double-J catheter was inserted into the ureter before the anastomosis was completed. After the anastomosis was completed, a drainage catheter was placed in the operation site. If deemed necessary, the contralateral superior vesical pedicle was ligated to increase bladder mobility. Surgical reconstruction was performed as a tension-free and waterproof anastomosis. Fibrin glue was used both for minor hemorrhages at the trauma site and to strengthen the ureteral anastomosis.
Postoperative evaluation
After surgical repair, the patients were routinely examined at the first, third, and sixth months, and then annually. The ureteral double-J catheter was removed, and vesicoureteral reflux (VUR) was simultaneously evaluated using drip infusion contrast cystourethrography. Physical examination, ultrasonography, and serum urea and creatinine tests were routinely performed at each visit. At the sixth month, the patients were evaluated with CT urography and, if hydroureteronephrosis might persist for a long time in the postoperative period, retrograde pyelography, antegrade nephrostogram, Technetium-99 m diethylene triamine pentaacetate renography or Technetium-99 m mercapto-acetyl-triglycine renography. The success of ureteroneocystostomy was defined as no additional surgery requirement, no progression of hydronephrosis on imaging, and normal contrast transition on imaging.
Statistical analysis
The normality of the data distribution was evaluated using the Kolmogorov–Smirnov test. Numerical variables that were not normally distributed were expressed using median and range values. The data were analyzed using the Statistical Package for the Social Sciences v. 25 (SPSS Inc, Illinois, USA). The Mann–Whitney U and Fisher’s exact tests were used in the statistical analysis of continuous variables and categorical variables, respectively. A p value of less than 0.05 was considered statistically significant.
Results
Demographic features and preoperative characteristics
Thirty-four patients underwent SCN (Group A) and 26 underwent MLG (Group B) ureteroneocystostomy. The median age of the patients was 55 (24–82) years. Forty-seven (78.3%) patients were female, and 13 (21.7%) were male. Ureteral injuries occurred during gynecologic surgery in 29 (48.3%) patients, abdominal surgery in 27 (45%), and urological surgery in four (6.7%). The primary surgery was non-oncological in 16 (26.7%) patients and oncological in 44 (73.3%). Ureteral injuries occurred in 13 (21.7%) patients due to thermal damage and 47 (78.3%) due to mechanical damage.
Groups A and B did not statistically significantly differ in terms of age (p = 0.154), gender (p = 0.817), side of injury (p = 0.112), preoperative chemotherapy or radiotherapy (p = 0.182), oncological/non-oncological surgical process (p = 0.969), preoperative nephrostomy (p = 0.548), primary surgical department (p = 0.408), mechanism of injury (p = 0.134), degree of injury (p = 0.938), presence of bladder injury (p = 0.122), preoperative hydronephrosis (p = 0.081), preoperative creatinine (p = 0.106), and glomerular filtration rate (p = 0.105). The demographic and preoperative characteristics of the patients are detailed in Table 1.
Perioperative features
The median length of ureteral injury/stricture was 33 (18–50) mm. According to the modified Clavien classification, grade 2 perioperative complications occurred (requiring blood transfusion) occurred in two (2.3%) patients. Groups A and B did not statistically significantly differ in terms of the length of ureteral injury/ stricture (p = 0.532), psoas hitch (p = 0.305), and perioperative complications (p = 0.683) (Table 2).
Postoperative outcomes
The median follow-up period of the patients was 37 (24–87) months. The treatment was successful in 53 (88.3%) patients and failed in seven (11.7%). In Group A, four patients had treatment failure. Re-SCN was (follow-up successful) performed at the 12th month in one patient with ureteral stricture development, and fistula repair was (follow-up successful) performed at the seventh month another patient that developed ureterovaginal fistula. At the 22nd month, one patient was found to have a non-functioning kidney due to VUR aggravation, and simple nephrectomy was performed. In the last patient, the ureteral double-J catheter was removed at the fourth week, and the ureteral double-J catheter was inserted again two weeks later, which provided successful results. In Group B, there were three patients with treatment failure. VUR aggravation occurred in two patients. Endoscopic sub-ureteral injections of dextran were applied to one of these patients (follow-up successful) at the ninth month, and a non-functioning kidney was found in the other at the 18th month (this patient was asymptomatic). In the last patient, the ureteral double-J catheter was removed at the fifth week inserted again a week later with successful results.
Postoperative complications occurred in 17 (28.3%) of the patients. Of the minor complications that occurred in 12 (20%) patients were classified as grade 1 or 2 (UTI, prolonged drainage, and wound-site discharge) according to the modified Clavien classification. Of the major complications that occurred in five (8.3%) patients, two were grade 3a (urinary extravasation requiring a drainage catheter) and three were grade 3b (ileus, ureteral stricture, and ureterovaginal fistula).
In the postoperative period, the serum creatinine value of the patients in Group A was significantly lower compared to Group B (p = 0.003). At the same time, the glomerular filtration rate of the patients in Group A was significantly higher compared to Group B (p = 0.002). The rate of postoperative complications was significantly higher in Group A than in Group B (p = 0.019), but there was no significant difference between the two groups in terms of treatment success (p = 1), major complications (p = 0.372), postoperative hydronephrosis (p = 0.962), postoperative follow-up duration (p = 0.879), postoperative ureteral double-J stent removal time (p = 0.412), postoperative drainage catheter removal time (p = 0.139), postoperative urethral catheter removal time (p = 0.268), postoperative VUR (p = 0.358), and postoperative hospitalization time (p = 0.254). The postoperative characteristics of the patients are listed in Table 3.
Discussion
In this study, a higher complication rate was found in patients with iatrogenic distal ureteral injuries who underwent ureteroneocystostomy with the SCN technique compared to those who underwent this operation with the MLG technique. There was no significant difference between the two groups in terms of major complications or treatment success.
There are few studies in the literature comparing the results of SCN and MLG ureteroneocystostomy. However, we found no study comparing the success and complication rates of the treatment of iatrogenic distal ureteral injuries between the SCN and MLG ureteroneocystostomy techniques. In a study conducted with patients that underwent renal transplantation, Baston et al. found a higher complication rate in those who underwent SCN ureteroneocystostomy compared to those who underwent extravesical MLG [14]. Silay et al. reported no difference between the success rates of intravesical (Cohen) and extravesical (Lich-Gregoir) ureteroneocystostomies in the treatment of vesicoureteral reflux in a pediatric population [15]. The European Association of Urology guidelines recommend ureteral re-implantation for the treatment of distal ureter traumas. However, since distal ureteral blood supply is affected in these cases, there is no consensus on whether the refluxing or non-refluxing technique should be used. The non-refluxing technique may disrupt blood flow at that level of the ureter by narrowing the distal end of the ureter. The refluxing technique does not involve this risk but may increase vesicoureteral reflux risk [1]. The results of different repair techniques are reported to be comparable [16]. In our study, the rates of complications and treatment success were consistent with the literature.
Ureteroneocystostomy can be used effectively in the treatment of iatrogenic distal ureteral injuries. In a study by Ambani et al., the success of ureteroneocystostomy in iatrogenic ureteral injuries was 97.1% during a 15-month follow-up [17]. Stearns et al. reported a ureteroneocystostomy success rate of 93% at 12 months [18]. Zhong et al. found the success rate of ureteroneocystostomy to be 90% over a mean follow-up period of 69 months [16]. Witters et al. determined the success rate of ureteroneocystostomy as 89.2% at 12 months in patients with iatrogenic distal ureteral injuries [11]. In our study, the success rate was 88.3% over a median follow-up period of 37 months.
Complications can cause major problems in cases where iatrogenic ureteral injuries are surgically repaired. Kim et al. stated that there were no major complications after ureteroneocystostomy, and the rate of minor complications was 18% [19]. In a study by Manassero et al., there were no major complications after ureteroneocystostomy, and the rate of minor complications was 33.8% [20]. Ambani et al. found the rates of major and minor complications after ureteroneocystostomy as 3 and 37.3%, respectively [17]. Lastly, Ding et al. stated that major complications occurred in 25% of patients after ureteroneocystostomy [21]. In our study, the rate of minor complications was 23.3%, and that of major complications was 8.3%, which is in agreement with the literature. On the other hand, we attributed the difference in the complication rates of the two surgical techniques to the opening of the bladder in intravesical SCN ureteroneocystostomy, which is not undertaken in extravesical MLG ureteroneocystostomy.
Whether the primary surgery is oncological or non-oncological may also affect surgery-related outcomes. In this regard, it is stated in the literature that the frequency of ureteral injuries is higher in oncological operations than in those performed for benign conditions [22]. In a study by Martin et al., ureteral injuries were reported in 7.2% of non-oncological operations and 92.8% of oncological operations [23]. In our study, distal ureter injuries were caused by non-oncological surgery in 26.7% of the patients and oncological surgery in 73.3%. Therefore, we recommend being more careful against possible ureteral injuries in oncological operations.
Iatrogenic distal ureteral injuries are usually encountered in gynecological and abdominal operations. Kominsky et al. reported that iatrogenic ureteral injuries were caused by gynecological operations in 42.5% of cases and abdominal operations in 33.3% [24]. In another study, Witters et al. stated that the rates of gynecological and abdominal operations as the causes of iatrogenic ureteral injuries were 69.2% and 19.2%, respectively [11]. In our study, distal ureteral injuries were caused by gynecological operation in 48.3% of the patients and abdominal operations in 45%. When these studies are further evaluated, our sample was similar to the sample of Kominsky et al. but differed from that of Witters et al., who reported less gynecological ureteral trauma. This may be due to the differences in the distribution of cases in clinics or different levels of care (secondary or tertiary) in the centers where the studies were conducted. It should also be kept in mind that developing technology and increasing surgical technical knowledge can cause such differences.
The major limitation of our study is the small number of patients due to the rarity of distal iatrogenic ureteral injuries. Although our study was conducted in a single center, our data included the results of more than one surgeon. Another limitation can be considered as the retrospective design. We found no statistically significant difference between the intra-vesical SCN and extra-vesical MLG ureteroneocystostomy techniques in terms of treatment success and major complications, and our results should be confirmed by further randomized prospective studies with larger samples.
Conclusions
In this study, we found that the patients with iatrogenic distal ureteral injuries who underwent intravesical SCN ureteroneocystostomy had more complications than those who underwent extravesical MLG ureteroneocystostomy. However, these two techniques provided similar results in terms of major complications and success rates. We consider that both techniques can be used safely and effectively in the treatment of iatrogenic distal ureteral injuries.
References
Kitrey ND, Djakovic N, Hallscheidt P et al. EAU Guidelines (2021) Edn. presented at the EAU Annual Congress Milan. EAU Guidelines Office, Arnhem, the Netherlands
Baser A, Alkis O, Toktas C (2016) A rare cause of ureteral injuries; simultaneous common iliac artery and ureter injury during posterior lumbar disc surgery. Turk J Urol 42(2):108–110. https://doi.org/10.5152/tud.2016.70105
Arlen AM, Pan S, Colberg JW (2018) Delayed diagnosis of isolated ureteral injury from blunt trauma. Urol Case Rep 19:50–51. https://doi.org/10.1016/j.eucr.2018.04.010
Ditz I, Bizjak J (2019) A rare case report of the use of allium stent in management of a gunshot injury with incomplete tear of the proximal part of the right ureter. J Endourol Case Reports 5(4):154–156
Phillips B, Holzmer S, Turco L et al (2017) Trauma to the bladder and ureter: a review of diagnosis, management, and prognosis. Eur J Trauma Emerg Surg 43(6):763–773. https://doi.org/10.1007/s00068-017-0817-3
Ortega SJ, Netto FS, Hamilton P, Chu P, Tien HC (2008) CT scanning for diagnosing blunt ureteral and ureteropelvic junction injuries. BMC Urol 8(1):3
Bryk DJ, Zhao LC (2016) Guideline of guidelines: a review of urological trauma guidelines. BJU Int 117(2):226–234
Zaid UB, Bayne DB, Harris CR (2015) Penetrating trauma to the ureter, bladder, and urethra. Current Trauma Reports 1(2):119–124
Zou Q, Fu Q (2015) Diagnosis and treatment of acute urogenital and genitalia tract traumas: 10-year clinical experience. Pak J Med Sci 31(4):925
Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Shackford SR, Champion HR, McAninch JW (1995) Organ injury scaling. Surg Clin 75(2):293–303
Witters S, Cornelissen M, Vereecken R (1986) Iatrogenic ureteral injury: aggressive or conservative treatment. Am J Obstet Gynecol 155(3):582–584
Ku JH, Kim ME, Jeon YS, Lee NK, Park YH (2003) Minimally invasive management of ureteral injuries recognized late after obstetric and gynaecologic surgery. Injury 34(7):480–483
Al-Awadi K, Kehinde EO, Al-Hunayan A, Al-Khayat A (2005) Iatrogenic ureteric injuries: incidence, aetiological factors and the effect of early management on subsequent outcome. Int Urol Nephrol 37(2):235–241
Baston C, Gîngu C, Omer A, Margaritis-Guler SS, Manea I, Dudu C, Sinescu I (2016) Split-cuff ureteral nipple versus Lich-Gregoir în transplantul renal de la donatorul în moarte cerebrala-studiu prospectiv al complicatiilor urologice/Split-cuff ureteral nipple versus Lich-Gregoir ureteroneocystostomy in kidney transplantation from deceased donors-a prospective study of urological complications. Roman J Urol 15(2):94
Silay MS, Turan T, Kayalı Y, Basibuyuk I, Gunaydin B, Caskurlu T, Karaman MI (2018) Comparison of intravesical (Cohen) and extravesical (Lich–Gregoir) ureteroneocystostomy in the treatment of unilateral primary vesicoureteric reflux in children. J Pediatric Urol 14(1):65.e1-65.e4. https://doi.org/10.1016/j.jpurol.2017.09.014
Zhong W, Yao L, Cui H, Yang K, Wang G, Xu T, Ye X, Li X, Zhou L (2017) Laparoscopic ureteral reimplantation with extracorporeal tailoring and direct nipple ureteroneocystostomy for adult obstructive megaureter: long-term outcomes and comparison to open procedure. Int Urol Nephrol 49(11):1973–1978. https://doi.org/10.1007/s11255-017-1687-7
Ambani SN, Skupin P, Malaeb BS, Barboglio-Romo P, Stoffel JT (2020) Does early ureteroneocystostomy after iatrogenic ureteral injury jeopardize outcome? Urology 136:245–250
Stearns GL, Tin AL, Benfante NE, Sjoberg DD, Sandhu JS (2021) Outcomes of ureteroneocystostomy in patients with cancer. Urology 158:131–134
Kim TN, Kim JH, Oh CK, Lee W, Nam JK, Lee KS (2021) Three different laparoscopic techniques for the management of iatrogenic ureteral injury: a multi-institutional study with medium-term outcomes. Asian J Surg 44(7):964–968
Manassero F, Mogorovich A, Fiorini G, Di Paola G, De Maria M, Selli C (2012) Ureteral reimplantation with psoas bladder hitch in adults: a contemporary series with long-term followup. Sci World J. https://doi.org/10.1100/2012/379316
Ding G, Li X, Fang D, Hao H, Li X, Zhou L (2021) Etiology and ureteral reconstruction strategy for iatrogenic ureteral injuries: a retrospective single-center experience. Urol Int 105(5–6):470–476
Rock J, Jones A, Howard W (2008) Operative injuries to the ureter: prevention, recognition and management. The Linde’s operative gynecology, 10th edn. Williams & Wilkins, Philadelphia, pp 961–971
Martin A, Wells A, Anderson ML, Chern JY, Rutherford TJ, Shahzad MM, Hoffman MS (2021) Trends in ureteral surgery on an academic gynecologic oncology service. Gynecol Oncol 163(3):552–556
Kominsky HD, Shah NC, Beecroft NJ, Diab D, Crescenze IM, Posid T, Baradaran N (2021) Does timing of diagnosis and management of iatrogenic ureter injuries affect outcomes? Experience from a tertiary center. Urology 149:240–244
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Demirdag, C., Bulbul, E., Gultekin, M.H. et al. Comparison of split-cuff nipple and modified Lich-Gregoir ureteroneocystostomy in iatrogenic distal ureteral injuries: tertiary care center experience. Int Urol Nephrol 55, 605–611 (2023). https://doi.org/10.1007/s11255-022-03449-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03449-1