Abstract
Purpose
To evaluate the long-term outcomes of laparoscopic ureteral reimplantation with extracorporeal tailoring and direct nipple ureteroneocystostomy for adult obstructive megaureter and compare the results with the open procedure.
Methods
From January 2007 to July 2013, 22 patients underwent laparoscopic and 28 patients underwent open ureteral reimplantation for adult obstructive megaureter. For laparoscopic group, the dilated ureter was delivered out of through a 12-mm port and the distal end was tailored and formed into an antireflux nipple extracorporeally. The ureteral nipple was intracorporeally reimplanted into the posterolateral wall of the bladder. Demographics, complications and follow-up data were analyzed and compared retrospectively between the groups.
Results
Baseline characteristics including age, gender, body mass index, affected side, age at diagnosis and follow-up time were statistically similar for the groups. All of the surgeries were performed successfully, and no major complications occurred. Comparing with the open group, the use of our novel laparoscopic procedure resulted in less estimated blood loss (50.0 vs. 71.0 ml; P = 0.001), less narcotic analgesic (3.0 vs. 18.0 mg; P = 0.01) and shorter hospital stay (5.1 vs. 7.9 days; P < 0.001). Long-term outcomes including rates of recurrent ureteral stricture (4.5 vs. 0%; P = 0.25), rates of vesicoureteral reflux (9.1 vs. 3.6%, P = 0.42) and success rates (86.4 vs. 96.9%; P = 0.45) did not significantly differ between the two groups.
Conclusion
Laparoscopic ureteral reimplantation with extracorporeal tailoring and direct nipple ureteroneocystostomy is a safe and equally effective as the open surgery for the long-term outcomes of adult obstructive megaureter.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
First recognized in 1923 by Caulk, the megaureter is defined as an abnormally dilated ureter ≥8 mm, with a normal function of the bladder and urethra [1]. Primary megaureter can be classified into four phenotypes, namely obstructive, refluxing, obstructive refluxing and non-obstructive non-refluxing [2, 3]. Primary obstructive megaureter (POM) is considered to be responsible for an aperistaltic juxtavesical segment of ureter, which leads to abnormal ureteral peristalsis and subsequent functional obstruction. As we know, obstructive megaureter is more common among neonates and young children. It can resolve spontaneously in most of the patients with the development of the kidney and ureter [4, 5]. However, in adults, obstructive megaureter can be symptomatic and associated with various complications. Thus, surgical intervention is recommended in most adults to preserve renal function.
Traditionally, open ureteral reimplantation (OUR) is the gold standard treatment for symptomatic obstructive megaureter. Within the past decades, as laparoscopic experience accumulated, the laparoscopic access has been increasingly performed [6, 7]. The key steps in ureteral reimplantation for obstructive megaureter are ureteral tailoring and antireflux management. Correcting the same defect under laparoscopic condition is a challenging procedure that requires skilled surgeons and long operative time. Since August 2010, our technique for laparoscopic ureteral reimplantation (LUR) with extracorporeal tailoring and direct nipple ureteroneocystostomy has evolved so that it mimics the open approach.
Currently, the long-term outcome of OUR for obstructive megaureter has proven to be encouraging [8, 9], but few published data exist about the long-term outcomes of the laparoscopic approach. In the present study, we aim to evaluate the long-term outcome of our modified LUR and compare them with those of the open procedure.
Patients and methods
Patients selection
From January 2007 to June 2013, 22 consecutive patients underwent LUR with ureteral tailoring and nipple ureteroneocystostomy and 28 consecutive patients underwent OUR for adult obstructive megaureter at Peking University First Hospital and Peking University People’s Hospital, Beijing, China. Preoperative radiographic examinations, such as ultrasound, nuclear renography, voiding cystogram and computed tomography urography, were used to confirm the diagnosis of obstructive megaureter. The open surgical procedures were performed by multiple surgeons over the course of the study period, whereas all LURs were performed by two experienced surgeons (XS Li and XJ Ye). Data on the baseline characteristics of the patients were collected retrospectively. The outcome measures included the overall operative time, the estimated blood loss, narcotic analgesic use, surgical complications, hospitalization stay and the follow-up results. Written informed consent was obtained from all the patients included in the study.
Surgical technique
Laparoscopic ureteral reimplantation
All patients in the LUR group successfully underwent the surgery without conversion to open surgery. The surgical technique used was the same as previously described [10]. In brief, patients were placed in a supine and head down position with a 30° ipsilateral side tilt. The primary 10-mm port for the camera was placed along the lower lip of the umbilicus in the midline, and two secondary ports (12 and 5 mm) were placed laterally to the ipsilateral rectus muscle and two fingers lower than the camera port. An additional 5-mm port for the assistant was placed 2 cm above the iliac crest.
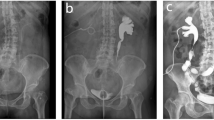
The ureter was exposed and dissected circumferentially to the bladder. The distal ureter was delivered out through the ipsilateral laparoscopic port. Subsequently, a 18F catheter was inserted in the dilated ureter and the redundant wall of the ureter was longitudinally tailored in lateral (Fig. 1a, b). Then, the tailored ureter was closed with a running 3-0 suture (Fig. 1c). The distal end of ureter was formed into a 1.5-cm nipple extracorporeally with the use of interrupted 3-0 Vicryl sutures (Fig. 1d). A double-J stent was then placed in the ureter and fixed to the nipple with 4-0 Monocryl suture. The ureter was replaced in the abdomen. After re-establishment of the pneumoperitoneum, direct nipple ureteroneocystostomy was completed at the posterolateral wall of the bladder (Fig. 1e).
Schematic diagram of the modified laparoscopic ureteral reimplantation for adult obstructive megaureter. a, b The distal ureter was delivered out of the abdomen and longitudinally tailored extracorporeally; c completion of anastomosis of the tailored ureter; d an antireflux nipple was formed and a D-J stent was placed extracorporeally; e the nipple was anastomosed to the posterolateral wall of the bladder intracorporeally
Open ureteral reimplantation
The patient was placed in the supine position, and a midline incision was performed. The ureteral exposure, dissection and tailoring procedures were performed in the same manner as for the laparoscopic approach. Two antireflux methods were applied in the open surgery, namely submucosal tunnel reimplantation and ureteral nipple implantation. For patients undergoing submucosal tunnel ureteroneocystostomy, a submucosal tunnel was created. A mucosa-to-mucosa ureterovesical anastomosis was completed with the use of interrupted 4-0 Vicryl sutures, and the detrusor and serosal layers were closed over the ureter with a running 2-0 Vicryl suture to create the submucosal tunnel. For patients undergoing direct nipple ureteroneocystostomy, the creation of the antireflux nipple, and ureteroneocystostomy were performed as for the laparoscopic technique.
Follow-up
All the patients were followed up at 3, 6 and 12 months after surgery and then at least once a year thereafter. The patients routinely received physical examination, urine routine test, serum creatinine, abdominal ultrasonography, intravenous pyelogram and cystogram at each visit. Computed tomography urography was repeated at 6 months after surgery. The successful outcome was defined as no major complications, resolved symptoms with decreased hydronephrosis, and absence of reflux and stricture during follow-up.
Statistical analysis
Statistical analysis was performed using the SPSS software version 20.0 (SPSS, Chicago, IL, USA). Descriptive data are presented as frequency and percentages. Continuous parametric variables are shown as mean ± SD. Nonparametric variables are expressed as median (interquartile range). The Mann–Whitney U test and Student t test were used to evaluate statistical differences between different groups. A two-sided P < 0.05 was considered to indicate statistically significant differences.
Results
A total of 50 patients who met the inclusion criteria were included in this study, comprising 16 males and 34 females, with mean age of 31.6 years (ranging from 19 to 60 years). Among the 50 patients, the indication for surgery in 24 patients was deterioration of differential renal function, in 20 patients recurrent urinary tract infection and in the remaining six patients recurrent ureteral stricture after balloon dilation. Noteworthy, five patients presented with bilateral megaureter.
The demographic and clinical characteristics of the patients stratified by the surgical approach are listed in Table 1. Among the 50 patients, 22 (44%) underwent the LUR procedure and 28 (56%) underwent the OUR procedure. In the OUR group, ten patients underwent open ureteral tailoring and submucosal tunnel ureteroneocystostomy, while the other 18 patients underwent open ureteral tailoring and nipple ureteroneocystostomy. The baseline characteristics including gender, age, BMI, affected side, age at diagnosis and follow-up time were well balanced between the two groups.
The outcomes for patients with obstructive megaureter treated with different approaches (laparoscopic and open) are summarized in Table 2. All the surgeries were successfully performed. No major complications (grade ≥ 3) occurred according to the modified Clavien–Dindo classification [11] in either group. The laparoscopic approach was less invasive, with less blood loss and shorter postoperative hospitalization compared with open surgery. Narcotic analgesic use was considerably less for the LUR group compared to the OUR group (3.0 vs. 18.0 mg; P = 0.01). Postoperative complications (within 90 days after surgery) for the LUR group and OUR group included urinary infection (grade 2, 2 vs. 2), urine leakage (grade 1, 0 vs. 1) and bleeding (grade 1, 0 vs. 1).
The mean postoperative follow-up was 69.3 months (5.8 years). The mean follow-up was 63.4 months for LUR patients and 74.0 months for OUR patients. The longest follow-up extended up to 10 years. During the follow-up, cystogram revealed mild vesicoureteral reflux (asymptomatic with normal renal function) in two patients in the LUR group. In addition, one patient in the LUR group presented recurrent ureter stricture and was managed with ureteral balloon dilation 2 years after surgery. In the OUR group, only one patient developed vesicoureteral reflux; the patient experienced recurrent urinary infection and underwent a second surgical reimplantation to solve the problem. Long-term outcomes, including the rates of recurrent ureteral stricture (P = 0.25), rates of vesicoureteral reflux (P = 0.42) and the success rates (P = 0.45), did not significantly differ between the two groups. At the end of follow-up, the renal function improved or remained stable in all the patients.
Discussion
Regarding adult POM, previous reports suggested that patients were predominantly males with a median age at diagnosis of 30–40 years [12, 13]. In comparison, the age at diagnosis of patients in our study was younger (median age: 25 years), and most of the patients (34, 64%) were female. Several reports had emphasized that adult POM may lead to various complications and damage the renal function if left untreated [14, 15]. Conservative therapy seems to be only appropriate in patients who are asymptomatic with normal renal function, and available for regular lifelong follow-up [15]. In our study, the indications for obstructive megaureter included progressive decrease in the differential renal function <40%, recurrent urinary tract infection associated with obstruction and worsening of the renal pelvic and ureter dilation.
The surgical principle for obstructive megaureter is to remove the non-functioning ureter and construct a non-refluxing and non-obstructive urinary outflow. Even though various surgical approaches have been reported [16,17,18], OUR remains the gold standard treatment for adult obstructive megaureter. Previous studies proved the long-term effectiveness and safety of the open procedure [8, 9]. Ehrlich et al. [19] reported LUR for the first time, proving the feasibility of the procedure in laparoscopic technique. Rassweiler et al. [20] demonstrated that the application of the laparoscopic approach resulted in better short-term outcome with minimal invasion and faster recovery than open surgery. However, few published long-term outcome data on the laparoscopic approach for adult obstructive megaureter are available. Our study is a comparison of the long-term outcomes of the LUR and OUR approaches for the treatment of obstructive megaureter.
Though the laparoscopic approach has emerged as a feasible alternative for obstructive megaureter, it is believed that LUR is technically challenging with intracorporeal tailoring and suturing. To address this issue, Ansari et al. [21] advocated the procedure of extracorporeal tailoring, in which they delivered out the free ureter through the trocar and completed the tailoring extracorporeally. With the application of this procedure, the ureteral tailoring was simple and the learning curve was shortened. Ureteroneocystostomy with antireflux management is another critical but challenging point in the laparoscopic approach, and this is traditionally accomplished by submucosal tunnel ureteroneocystostomy. Tatlisen et al. [22] first introduced the antireflux nipple technique for the treatment of megaureter, achieving a high success rate without ureteral stricture or reflux. Applying the nipple technique by laparoscopy was much easier and less time-consuming compared with submucosal tunnel ureteroneocystostomy. Consequently, since January 2010, we have modified the conventional LUR with extracorporeal tailoring and direct nipple ureteroneocystostomy. The procedures of tailoring, nipple construction and D-J stent placement were all performed extracorporeally. Our previous work demonstrated that the technique could facilitate and speed up the procedure [10]. However, extracorporeal tailoring may lead to undue traction of the ureter and the antireflux nipple is still not a conventional option for megaureter. Besides, there have been concerns regarding the risk of ischemic damage of ureter and postoperative reflux for the technique.
In the present study, we presented the long-term outcome for 22 patients who underwent treatment with our technique. Regarding the risk of ischemic damage to the ureter, our careful dissection resulted in no urine leakage after surgery. Only one ureteral stricture developed and the patient was successfully managed with ureteral balloon dilation during the follow-up. For postoperative reflux, the direct comparison between submucosal tunnel reimplantation and ureteral nipple implantation in the open group (Supplementary Table 1) demonstrated that ureteral nipple implantation had a comparable postoperative reflux rate compared with submucosal tunnel reimplantation in the long term. In general, the overall success rate in our laparoscopic group was 86.4% during an average follow-up period of 63.4 months. Despite our strict criteria for a successful outcome and the longest average follow-up time, the results with our approach were comparable to those with the other laparoscopic series [7, 10, 23]. During the follow-up, no significant difference was observed in the complications and the long-term successful rate between the two groups. Overall, the laparoscopic approach seems to be safe and equally effective as the open surgery regarding the long-term outcome of adult POM.
Aside from LUR, other minimally invasive surgery options like endoscopic balloon dilation and robotic-assisted LUR have demonstrated satisfactory short-term results for adult POM [16, 17]. Both approaches seem to be less invasive than LUR. We have proposed the endoscopic balloon dilation for megaureter in recent years. However, long-term follow-ups are warranted to confirm the effectiveness and safety of the endoscopic approach.
Admittedly, our study was retrospective with limited sample size, which may reduce the strength of this study. However, despite these limitations, the study evaluates the long-term functional outcome of our modified LUR procedure for adult megaureter, in the largest series of laparoscopic experience to date. Furthermore, to our knowledge, this is the first study that compares the LUR and OUR procedures for adult obstructive megaureter, with a long-term follow-up.
Conclusion
LUR with extracorporeal tailoring and direct nipple ureteroneocystostomy is safe and equally effective as the OUR procedure for the long-term outcome of adult obstructive megaureter. LUR may be recommended as the first line of surgical approach for adult obstructive megaureter in skilled centers. However, a comprehensive, prospective and randomized study is warranted to better delineate the role of LUR in the treatment of adult obstructive megaureter.
References
Im YJ, Jung HJ, Lee YS, Hong CH, Han SW (2013) Impact of ectopic insertion on treatment outcome of primary non-refluxing megaureter. Urology 81(2):402–406. doi:10.1016/j.urology.2012.11.038
King LR (1980) Megaloureter: definition, diagnosis and management. J Urol 123(2):222–223
Fraser L, Khan MH, Ross M, Patterson PJ (2007) Rare case of non-refluxing non-obstructive megaureter in an adult. Int Urol Nephrol 39(2):421–423. doi:10.1007/s11255-006-9054-0
Peters CA, Mandell J, Lebowitz RL, Colodny AH, Bauer SB, Hendren WH, Retik AB (1989) Congenital obstructed megaureters in early infancy: diagnosis and treatment. J Urol 142(2 Pt 2):641–645
Rubenwolf P, Herrmann-Nuber J, Schreckenberger M, Stein R, Beetz R (2016) Primary non-refluxive megaureter in children: single-center experience and follow-up of 212 patients. Int Urol Nephrol 48(11):1743–1749. doi:10.1007/s11255-016-1384-y
He Y, Chen X, Chen Z, Luo YC, Li NN (2012) Treatment of symptomatic primary obstructive megaureter by laparoscopic intracorporeal or extracorporeal ureteral tapering and ureteroneocystostomy: experience on 11 patients. J Endourol 26(11):1454–1457. doi:10.1089/end.2012.0236
Abraham GP, Das K, Ramaswami K, Siddaiah AT, George D, Abraham JJ, Thampan OS (2012) Laparoscopic reconstruction for obstructive megaureter: single institution experience with short- and intermediate-term outcomes. J Endourol 26(9):1187–1191. doi:10.1089/end.2012.0039
Link BA, Slobodov G, Campbell JB, Kropp BP (2007) Radiographic changes following excisional tapering and reimplantation of megaureters in childhood: long-term outcome in 46 renal units. J Urol 178(4 Pt 1):1474–1478. doi:10.1016/j.juro.2007.05.169
Guseinov E (2000) Long-term results of the surgical treatment of primary obstructive megaureter in children. Urologiia 5:35–40
He R, Yu W, Li X, Yao L, He Z, Zhou L (2013) Laparoscopic ureteral reimplantation with extracorporeal tailoring and direct nipple ureteroneocystostomy for adult obstructed megaureter: a novel technique. Urology 82(5):1171–1174. doi:10.1016/j.urology.2013.07.019
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. doi:10.1097/SLA.0b013e3181b13ca2
Pfister RC, Hendren WH (1978) Primary megaureter in children and adults. Clinical and pathophysiologic features of 150 ureters. Urology 12(2):160–176
Hanna MK, Wyatt JK (1975) Primary obstructive megaureter in adults. J Urol 113(3):328–334
Dorairajan LN, Hemal AK, Gupta NP, Wadhwa SN (1999) Primary obstructive megaureter in adults: need for an aggressive management strategy. Int Urol Nephrol 31(5):633–641
Hemal AK, Nayyar R, Rao R (2009) Robotic repair of primary symptomatic obstructive megaureter with intracorporeal or extracorporeal ureteric tapering and ureteroneocystostomy. J Endourol 23(12):2041–2046. doi:10.1089/end.2009.0103
Garcia-Aparicio L, Blazquez-Gomez E, Martin O, Palazon P, Manzanares A, Garcia-Smith N, Bejarano M, de Haro I, Ribo JM (2013) Use of high-pressure balloon dilatation of the ureterovesical junction instead of ureteral reimplantation to treat primary obstructive megaureter: Is it justified? J Pediatr Urol 9(6 Pt B):1229–1233. doi:10.1016/j.jpurol.2013.05.019
Fu W, Zhang X, Zhang X, Zhang P, Gao J, Dong J, Chen G, Xu A, Ma X, Li H, Shi L (2014) Pure laparoscopic and robot-assisted laparoscopic reconstructive surgery in congenital megaureter: a single institution experience. PLOS ONE 9(6):e99777. doi:10.1371/journal.pone.0099777
Hemal AK, Ansari MS, Doddamani D, Gupta NP (2003) Symptomatic and complicated adult and adolescent primary obstructive megaureter–indications for surgery: analysis, outcome, and follow-up. Urology 61(4):703–707
Ehrlich RM, Gershman A, Fuchs G (1994) Laparoscopic vesicoureteroplasty in children: initial case reports. Urology 43(2):255–261
Rassweiler JJ, Gozen AS, Erdogru T, Sugiono M, Teber D (2007) Ureteral reimplantation for management of ureteral strictures: a retrospective comparison of laparoscopic and open techniques. Eur Urol 51(2):512–522. doi:10.1016/j.eururo.2006.08.004
Ansari MS, Mandhani A, Khurana N, Kumar A (2006) Laparoscopic ureteral reimplantation with extracorporeal tailoring for megaureter: a simple technical nuance. J Urol 176(6 Pt 1):2640–2642. doi:10.1016/j.juro.2006.08.025
Tatlisen A, Ekmekcioglu O (2005) Direct nipple ureteroneocystostomy in adults with primary obstructed megaureter. J Urol 173(3):877–880. doi:10.1097/01.ju.0000152533.93716.3c
Bondarenko S (2013) Laparoscopic extravesical transverse ureteral reimplantation in children with obstructive megaureter. J Pediatr Urol 9(4):437–441. doi:10.1016/j.jpurol.2013.01.001
Acknowledgements
The authors are very grateful to the medical illustrator Madam Xinying Ma.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhong, W., Yao, L., Cui, H. et al. Laparoscopic ureteral reimplantation with extracorporeal tailoring and direct nipple ureteroneocystostomy for adult obstructive megaureter: long-term outcomes and comparison to open procedure. Int Urol Nephrol 49, 1973–1978 (2017). https://doi.org/10.1007/s11255-017-1687-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1687-7