Abstract
Purpose
Anemia persists as a challenge in chronic kidney disease (CKD) patients. Current therapies are the injectable erythropoietin stimulating agents (ESA). Concerns have been raised regarding ESA cardiovascular safety, therefore search for an alternative, convenient and safe therapy is underway. Hypoxia inducible factors-prolyl hydroxylase inhibitors (HIF-PHI) are oral agents with promising results. Numerous small studies reported favorable effects with lack of large, powered studies.
Methods
We conducted a meta-analysis of randomized clinical trials to assess the efficacy and safety of HIF-PHI in non-dialysis-dependent CKD patients. Primary outcome was hemoglobin (Hb) concentration post intervention. Secondary outcomes were all-cause mortality, MACE, and changes in iron metabolism (ferritin, hepcidin). We reported total and serious adverse effects. Data were pooled using a random effect model via RevMan 5.4 software.
Results
We identified 7 trials comprising of 8228 patients (mean age 66.5 ± 13.2 years, 42% were females, 53% used iron replacement) with a mean follow-up of 52 weeks. Compared with the standard of care (ESA), HIF-PHI were non-inferior for treatment of anemia, with comparable effect on mortality and major adverse cardiovascular events. HIF-PHI showed no major safety concerns. Main side effect of HIF-PHI was diarrhea.
Conclusion
HIF-PHI might represent a safe, and convenient alternative to ESA in non-dialysis dependent CKD patients with anemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia remains a challenge in patients with chronic kidney disease (CKD) as it is associated with disease progression, decreased quality of life, and increase in all-cause mortality [1]. Proper management of anemia in these patients is important for overall survival. Currently, erythropoietin stimulating agents (ESAs) such as epoetin and darbepoetin alfa are among the only Food and Drug Administration (FDA) approved drugs for improving hemoglobin in anemic patients with CKD. Due to their increased adverse effects profile and associated high cardiovascular events, especially in patients with hemoglobin > 11 g/dl, the lowest dose sufficient to reduce the need for transfusion of packed red cells is recommended [2]. As a result, search for an alternative to ESA is underway. Oral hypoxia-inducible factor-prolyl hydroxylase inhibitors (HIF-PHIs) are promising therapies for the treatment of anemia in non-dialysis dependent chronic kidney disease (NDD CKD) patients. HIF-PHIs stimulate the production of endogenous erythropoietin through inhibition of the prolyl hydrolase enzymes and increase iron levels in these patients [3, 4]. Randomized controlled trials (RCTs) have evaluated the efficacy and safety of several HIF-PHIs as an oral alternative to parenterally administered epoetin and its derivatives. More recent evidence accumulated suggesting promising results, with lack of large, powered studies. Hence, we conducted a systematic review and meta-analysis of RCTs to compare the efficacy and safety of HIF-PHIs versus ESAs regarding hemoglobin concentration, iron metabolism and adverse effects in anemic patients with NDD CKD.
Methods
Search strategy and eligibility criteria
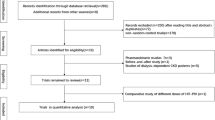
We performed a comprehensive search of multiple electronic databases (PubMed/Medline, Embase, Cochrane, Google scholar), from inception till December/20/2021. We used the following pre-specified search terms (hypoxia-inducible factor-prolyl hydroxylase inhibitors) OR (HIF-PHI) AND (epoetin) OR (erythropoietin) OR (erythropoietin stimulating agent) AND (anemia) OR (low hemoglobin) AND (non-dialysis renal disease) OR (non-dialysis kidney disease) OR (non-dialysis chronic kidney disease). Search was restricted to English language.
We included only RCTs with active comparator reported (ESA). Placebo-controlled trials and observational studies/registries were excluded. CKD was defined as an estimated glomerular filtration rate (GFR) < 60 ml/min/1.73 m2 or CKD stage ≥ 3 per CKD Epidemiology Collaboration (CKD-EPI) formula.
Data extraction/quality assurance
Two investigators (MO, SS) screened the trials abstracts, and if suitable the full manuscript including supplement/appendix and extracted pre-defined variables independently in a pre-designed excel sheet. Data included baseline demographics, intervention, duration of follow-up, clinical outcomes, among others. Quality of studies regarding methods of randomization, concealment of allocation, blinding, and incomplete data were assessed on categorical scale. Disagreement, if any, was resolved by consensus. Units for different variables were standardized using respective calculators and rounded to one decimal.
Outcomes
The primary outcome of interest was hemoglobin concentration (Hb) g/dl post intervention at the longest follow-up duration. Secondary outcomes included all-cause mortality, major adverse cardiovascular events (MACE) (defined as all-cause mortality, non-fatal myocardial infarctions (MI), and non-fatal stroke), and change in iron metabolism in the form change of ferritin and hepcidin. We also reported all, serious, and specific adverse effects (AE).
Statistical analysis
Effect estimates were extracted from each study in the form of events or means depending on variable type, directly from the article or calculated indirectly based on the available data from the text. Correspondent authors of respective studies were contacted via email if there was a missing data. We calculated risks ratios (RRs) and weighted mean differences (MDs) with their corresponding 95% confidence intervals (CIs) for dichotomous and continuous data, respectively. Heterogeneity between studies was explored by Cochran Q statistic (P < 0.05) and I-squared (I2) statistic. All statistical tests were two-sided, and P values ≤ 0.05 were considered significant. All analyses were conducted via RevMan 5.4 software using a random-effects model.
Results
We identified 7 RCTs reported in 6 articles [5,6,7,8,9,10] with a total of 8228 patients (HIF-PHI = 4185, ESA = 4043), with a mean age of 66.5 ± 13.2 years, 42% were females and a median follow-up of 52 weeks. Patients with diabetes and hypertension represented 41% and 59%, respectively. The mean Hb and estimated GFR for both groups (HIF-PHI) and (ESA) were 9.8 ± 1.0 g/dl and 20.3 ± 11.5 ml/min/1.73 m2, respectively.
Patients receiving iron replacement represented 53%.
Regarding Hb concentration post intervention, our analysis showed that HIF-PHI and ESA were not statistically different [MD − 0.03, 95% CI (− 0.18, 0.11); P = 0.66] (Fig. 1).
Our analysis also showed no statistical difference between groups regarding all-cause mortality [RR 1.02, 95% CI (0.92, 1.13); P = 0.71] and MACE [RR 1.08; 95% CI (0.99, 1.18); P = 0.08] (Fig. 2).
Regarding iron metabolism, HIF-PHIs showed a significant reduction of ferritin (µg/L) and hepcidin (ng/ml) compared to the ESA group [MD − 18.89, 95% CI (− 29.08, − 8.69); P < 0.001] and [MD − 28.21, 95% CI (− 40.73, − 15.68); P < 0.001], respectively (Fig. 3).
In term of adverse effects (AE) (total AE, serious AE, hypertension, hyperkalemia), we found no statistical difference between HIF-PHI and ESA groups [RR 1.01, 95% CI (0.99, 1.04); P = 0.28], [RR 1.04, 95% CI (0.94, 1.15); P = 0.41], [RR 0.88, 95% CI (0.75, 1.04); P = 0.13], [RR 0.88, 95% CI (0.68, 1.15); P = 0.35], respectively, except diarrhea, which was reported more in the HIF-PHI group compared to ESA, [RR 1.45, 95% CI (1.21, 1.73); P < 0.01], (Fig. 4).
Discussion
Our meta-analysis showed that HIF-PHIs are non-inferior compared to ESA, the current standard of care for treatment of anemia in non-dialysis dependent CKD patients. There were no significant differences between groups in terms of Hb concentration post intervention, all-cause mortality, or MACE. However, HIF-PHIs were associated significant iron metabolism changes in term of lower ferritin, hepcidin. HIF-PHI were also significantly associated with more diarrhea compared with ESAs.
HIF-PHIs as an oral agent are a more attractive and appealing option. This favorable pharmacokinetic property might reduce the need for further outpatient visits required with epoetin/darbepoetin which are given subcutaneously or intravenously. We believe that convenience of administration is vital for patients’ satisfaction and compliance.
Our findings of reduction in ferritin and hepcidin emphasize the role of HIF-PHIs in iron metabolism. HIF-PHI might lead to excessive iron consumption, as reduced levels of hepcidin, might indicate increase in iron absorption and/or utilization, which in turn might necessitate increase in iron supplementation in NDD CKD patients. [11, 12] As the long-term effect of this change in iron metabolism is not yet clear, more studies are needed and awaited.
Our analysis is consistent with current literature. Chen and his colleagues conducted a similar meta-analysis of > 13,000 patients [12]. They studied effect of HIF-PHI in comparison to both active intervention (ESA) and placebo, and they included both dialysis dependent and non-dialysis dependent CKD patients. They reported increase Hb level and iron utilization with good long-term tolerability. In contrast, we included only non-dialysis dependent CKD patients, and active comparison (ESA) arm to maintain homogeneity, but our findings are similar in terms of Hb level, iron utilization, and safety measured as MACE.
Adverse effects analysis was consistent with literature. Gastrointestinal upset is commonly reported in HIF-PHI due to altered epithelial cell metabolism but is usually mild to moderate. We did not find any major safety concerns, which should be reassuring for both potential patients and providers.
Our meta-analysis is the first to report head-to-head comparison with the current standard of care for anemia in NDD-CKD. The major limitations of our analysis are heterogeneity and relatively short follow-up duration. Further large RCTs with long-term follow-up are needed.
In conclusion, among patients with anemia and NDD CKD, HIF-PHIs are non-inferior to ESAs for treatment of anemia. MACEs were also similar between the two groups. HIF-PHIs are associated with reduced iron metabolism, and more diarrheal episodes.
References
Sato Y, Fujimoto S, Konta T et al (2018) Anemia as a risk factor for all-cause mortality: obscure synergic effect of chronic kidney disease. Clin Exp Nephrol 22(2):388–394. https://doi.org/10.1007/s10157-017-1468-8
Research C for DE and FDA Drug Safety Communication: Modified dosing recommendations to improve the safe use of Erythropoiesis-Stimulating Agents (ESAs) in chronic kidney disease. FDA. Published online January 5 2021. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-modified-dosing-recommendations-improve-safe-use-erythropoiesis. Accessed 9 May 2021
Gupta N, Wish JB (2017) Hypoxia-inducible factor prolyl hydroxylase inhibitors: a potential new treatment for anemia in patients with CKD. Am J Kidney Dis 69(6):815–826. https://doi.org/10.1053/j.ajkd.2016.12.011
Haase VH (2021) Hypoxia-inducible factor-prolyl hydroxylase inhibitors in the treatment of anemia of chronic kidney disease. Kidney Int 11(1):8–25. https://doi.org/10.1016/j.kisu.2020.12.002
Holdstock L, Cizman B, Meadowcroft AM et al (2019) Daprodustat for anemia: a 24-week, open-label, randomized controlled trial in participants with chronic kidney disease. Clin Kidney J 12(1):129–138. https://doi.org/10.1093/ckj/sfy013
Macdougall IC, Akizawa T, Berns JS, Bernhardt T, Krueger T (2019) Effects of Molidustat in the Treatment of Anemia in CKD. Clin J Am Soc Nephrol 14(1):28–39. https://doi.org/10.2215/CJN.02510218
Nangaku M, Kondo K, Kokado Y et al (2021) Phase 3 randomized study comparing vadadustat with darbepoetin alfa for anemia in Japanese patients with nondialysis-dependent CKD. J Am Soc Nephrol. https://doi.org/10.1681/ASN.2020091311 (Published online April 21, 2021:ASN.2020091311)
Chertow GM, Pergola PE, Farag YMK et al (2021) Vadadustat in patients with anemia and non-dialysis-dependent CKD. N Engl J Med 384(17):1589–1600. https://doi.org/10.1056/NEJMoa2035938
Nangaku M, Hamano T, Akizawa T et al (2021) Daprodustat compared with epoetin beta pegol for anemia in Japanese patients not on dialysis: a 52-week randomized open-label phase 3 trial. Am J Nephrol 52(1):26–35. https://doi.org/10.1159/000513103
Singh AK, Carroll K, McMurray JJV et al (2021) Daprodustat for the treatment of anemia in patients not undergoing dialysis. N Engl J Med 385(25):2313–2324. https://doi.org/10.1056/NEJMoa2113380
Akizawa T, Macdougall IC, Berns JS et al (2019) Iron regulation by molidustat, a daily oral hypoxia-inducible factor prolyl hydroxylase inhibitor patients with chronic kidney disease. Nephron 143(4):243–254. https://doi.org/10.1159/000502012
Chen H, Cheng Q, Wang J, Zhao X, Zhu S (2021) Long-term efficacy and safety of hypoxia-inducible factor prolyl hydroxylase inhibitors in anaemia of chronic kidney disease: a meta-analysis including 13,146 patients. J Clin Pharm Ther 46(4):999–1009. https://doi.org/10.1111/jcpt.13385
Author information
Authors and Affiliations
Contributions
Research idea and study design: SS; MM: data acquisition; MO, MM, SS: data analysis/interpretation; MM, AO, MO: editing and review; AO, BK, CN: supervision or mentorship; BK, CN. Each author contributed important intellectual content during manuscript drafting or revision and agrees to be personally accountable for the individual’s own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated, and resolved, including with documentation in the literature if appropriate.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohamed, M.M.G., Oyenuga, M., Shaikh, S. et al. Hypoxia inducible factor-prolyl hydroxylase inhibitors in anemic patients with non-dialysis dependent chronic kidney disease: a meta-analysis of randomized clinical trials. Int Urol Nephrol 55, 167–171 (2023). https://doi.org/10.1007/s11255-022-03300-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03300-7