Abstract
Background
Inflammation, oxidative stress (OS), atherosclerosis and resistant hypertension (RH) are common features of chronic kidney disease (CKD) leading to a higher risk of death from cardiovascular disease. These effects seem to be modulated by impaired anti-oxidant, anti-inflammatory and reverse cholesterol transport actions of high-density lipoprotein cholesterol (HDL). HDL prevents and reverses monocyte recruitment and activation into the arterial wall and impairs endothelial adhesion molecule expression. Recently, monocyte count to HDL-cholesterol ratio (MHR) has emerged as a potential marker of inflammation and OS, demonstrating to be relevant in CKD. Our research was aimed to assess, for the first time, its reliability in RH.
Methods
We performed a retrospective study on 214 patients with CKD and arterial hypertension who were admitted between January and June 2019 to our Department, 72 of whom were diagnosed with RH.
Results
MHR appeared inversely related to eGFR (ρ = − 0.163; P = 0.0172). MHR was significantly higher among RH patients compared to non-RH ones (12.39 [IQR 10.67–16.05] versus 7.30 [5.49–9.06]; P < 0.0001). Moreover, MHR was significantly different according to the number of anti-hypertensive drugs per patient in the whole study cohort (F = 46.723; P < 0.001) as well as in the non-RH group (F = 14.191; P < 0.001). Moreover, MHR positively correlates with diabetes mellitus (ρ = 0.253; P = 0.0002), white blood cells (ρ = 0.664; P < 0.0001) and C-reactive protein (ρ = 0.563; P < 0.0001).
Conclusions
MHR may be a reliable biomarker due to the connection between HDL and monocytes. Our study suggests that MHR is linked with the use of multiple anti-hypertensive therapy and resistant hypertension in CKD patients, and can be a useful ratio to implement appropriate treatment strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Investigators all over the world are focused on finding an economical, fast and reproducible biomarker to quantify the amount of inflammatory status and oxidative stress (OS) in daily practice.
Patients affected by chronic kidney disease (CKD) are known to be more exposed to atherosclerosis injury and, consequently, to have a higher risk of premature death from cardiovascular disease (CVD) [1,2,3].
These dangerous conditions are clearly associated with a worsening of arterial hypertension and CKD stage as well as adverse cardiovascular outcomes, so it appears fundamental to find a proper strategy to contrast or adequately prevent them.
The link between CKD and atherosclerosis is guided by inflammation, OS and lipid accumulation, which are common features of both conditions. These effects seem to be modulated by an increased endogenous lipid synthesis and with a reduced cellular catabolism of fatty acids and impaired anti-oxidant, anti-inflammatory and reverse cholesterol transport actions of high-density lipoprotein cholesterol (HDL) [4].
HDL has been identified as a protective factor in the setting of atherosclerosis, with additional functional properties beyond its role in lipid regulation [5]. HDL can remove cholesterol from peripheral stores and transport it to the liver for excretion in the biliary system; it also inhibits the oxidative modifications of low-density lipoprotein cholesterol (LDL), reducing its atherogenicity [6]. Moreover, several studies affirmed that physiological serum levels of HDL have beneficial effects on platelet function, thrombolytic balance, cellular reparative mechanisms, anti-apoptotic activities, and normalization of vascular function [7, 8].
Arterial hypertension is a well-known CKD risk factor leading to hypertensive nephrosclerosis, a renal injury characterized by glomerular damage and arterial sclerosis, infiltration of inflammatory cells, interstitial fibrosis and tubular atrophy [9, 10].
As the renal function declines, there is an upregulation of the renin–angiotensin–aldosterone system (RAAS), which stimulates salt and water retention [11].
The insult of persistent hypertension results in renal interstitial fibrosis, renal fibroblasts’ activation and overproduction of extracellular matrix proteins in both glomeruli and interstitium [12]. These mechanisms cause a deregulation of wound-healing response, leading to glomerulosclerosis, vascular sclerosis, and inflammatory response. Endothelial and mesangial oxidative stress due to hypertension, causes and increases mesangial production of transforming growth factor-β [13], a stimulation of angiotensin II (Ang II) [14], and a disequilibrium in the generation of glomerular nitric oxide, reducing its protective effect in the process of glomerulosclerosis [15]. Ang II also promotes the synthesis of plasminogen activator inhibitor-1, kynurenine pathway [16] and nuclear factor ĸB, contributing to interstitial nephritis through the recruitment and activation of neutrophils, macrophages and T-lymphocytes [17]. This inflammatory mechanism leads to a lesion of the basal membrane and epithelial-mesenchymal transition, as well as an increased production of collagen and alteration of blood vessels and kidney tubules [18].
RAAS inhibition, is associated not only with the regulation of blood volume and systemic vascular resistance, but also with a reduction of urinary albumin excretion and renal function preservation [19].
A proper strategy to prevent vascular damage may be represented by obtaining both the normalization of BP levels and an adequate lipid profile. HDL has been demonstrated to exert favorable effects on inflammatory and oxidative pathways, such as inhibition of lipid peroxidation and cytokine-induced upregulation of pro-inflammatory adhesion molecule and chemokine expression by endothelial cells. At the same time, HDL promotes macrophage phenotype switching from a pro-inflammatory to an anti-inflammatory form [20,21,22,23]. In particular, HDL exerts anti-atherosclerotic effects by suppressing the proliferation-differentiation of monocyte progenitor cells [24] and by suppressing and reverting the activation of monocytes via a decrease in their F-actin content, thereby reducing their CD11b expression. Conversely, HDL decreases the exposure of endothelial adhesion molecules and actively induces vasodilatation by increasing the expression of endothelial nitric oxide synthase [25], thus preventing monocyte recruitment into the arterial wall [26]. HDL also neutralizes the pro-oxidant effects of already active macrophages via inhibiting LDL oxidation, and to maintaining constant efflux of cholesterol from these cells [27].
The central role of macrophages in the kidney is mediated by the monocyte chemoattractant protein (MCP)-1, a chemokine produced by mesangial cells and renal tubular cells that has the responsibility of recruiting macrophages into the kidney [28].
Recently, monocyte count to high-density lipoprotein cholesterol ratio (MHR) has been studied as a new marker of inflammation and OS [24]. Our research aimed to assess, for the first time, the association of MHR with Resistant Hypertension (RH), which represents a fearsome risk factor for CVD and progression to end-stage renal disease (ESRD) in CKD population.
Materials and methods
Data were retrieved through a retrospective scan of the files of 214 hypertensive patients, with different stages of CKD, who were admitted to the Unit of Nephrology and Dialysis of Policlinic G. Martino in Messina, Italy, between January and June 2019. Of them, 72 patients were diagnosed with RH, defined as blood pressure (BP) that remains above 140/90 mmHg despite the use of three different classes of anti-hypertensive medications (one of which must be a diuretic) at the maximum tolerated doses [29]. Participants were advised to avoid caffeinated beverages and exercise for at least 1 h before BP measurement. During the measurement, patients were seated with their arm supported at the level of the heart. The mean of three BP measurements was calculated and used in all analyses. eGFR was calculated according to the CKD-EPI equation [30]. Exclusion criteria were designed to discard any other secondary cause of RH or any condition that might influence monocyte count or HDL serum levels. For these reasons, we excluded: patients receiving corticosteroids or any other immunosuppressant therapy and patients affected by active infections, hematological diseases, intracranial mass, malignant tumors or mental disorders. Written informed consent was obtained from every participant; if disabled, informed consent was acquired from participant’s proxies.
Biochemical assays
After an overnight fast, venous blood samples were collected between 8:00 AM and 9:00 AM through a polyethylene catheter inserted in a forearm vein using BD Vacutainer tubes. All serum creatinine (SCr) measurements were performed at our chemical clinical laboratory using a colorimetric-kinetic Jaffe reaction with a normal range of 0.5–1.4 mg/dl. HDL was analyzed enzymatically on an auto-analyzer, with normal values different for males (> 55 mg/dl) and females (> 65 mg/dl). All the kits’ components were stable and stored tightly closed at 2–8 °C, protected from light and contaminations. All laboratory equipment was calibrated and blinded duplicate samples were used. We calculated MHR as the ratio of the absolute monocyte count to the level of HDL.
Statistical analysis
Kolmogorov–Smirnov test was used to assess data distribution. Normally distributed continuous variables were expressed as mean ± standard deviation (SD), non-normally distributed values as median and interquartile range (IQR), and categorical data as percentage frequency. Differences between groups were examined with Student’s unpaired t-test for normal variables, Mann–Whitney test for non-normally distributed data, and χ2 test for categorical variables. Differences of a variable between the means of several subgroups were evaluated using One-way analysis of variance (ANOVA) test. Correlations between normally distributed variables were determined by assessing Pearson’s correlation coefficient, correlations between non-normal variables through Rank correlation and Spearman’s rho (ρ) coefficient. Independent relationships were investigated by multiple regression analysis. Receiver operating characteristics (ROC) analysis was used to calculate the area under the curve (AUC) for MHR to find the best MHR cut-off value to identify RH. P-values < 0.05 were considered to be statistically significant. Statistical analysis was conducted employing MedCalc® (version 12.7.0.0; MedCalc Software bvba, Belgium) and SPSS® (version 22.0.0.0; IBM Corporation, Armonk, NY) software.
Results
The two groups significantly differed for monocyte, HDL and MHR values and for the number of anti-hypertensive drugs taken whereas differences were not statistically relevant for gender, age and parameters of kidney function.
Demographic, clinical and biochemical parameters of enrolled patients are reported in Table 1.
In the whole cohort of patients, MHR did not correlate with age (ρ = 0.0328; P = 0.6334) but it was inversely related to eGFR (ρ = − 0.163; P = 0.0172) (Fig. 1).
Stratifying subjects according to the presence of RH, MHR values were higher among patients with RH compared to those who had not (12.39 [IQR 10.67–16.05] versus 7.30 [5.49–9.06]; P < 0.0001) (Fig. 2).
Moreover, MHR was significantly different according to the number of anti-hypertensive drugs taken both in the whole study cohort (F = 46.723; P < 0.001) (Fig. 3) and in the group of patients not suffering from RH (F = 14.191; P < 0.001) (Fig. 4), whereas the difference among patients with RH was not statistically significant (F = 2.350; P = 0.103).
At multiple regression analysis, RH and the number of anti-hypertensive drugs resulted to be independent correlates of MHR (Table 2).
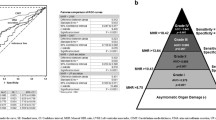
ROC analysis considering RH as status variable showed an AUC for MHR of 0.937 (95% confidence interval [CI], 0.895–0.965). The best MHR cut-off value to predict RH was > 10.11 with a sensitivity of 87.50% (95% CI, 77.6–94.1) and a specificity of 88.03% (95% CI, 81.5–92.9) (Fig. 5).
ROC curve of MHR (monocyte-to-high-density lipoprotein cholesterol ratio) considering RH (resistant hypertension) as status variable. The area under the curve (AUC) for MHR was 0.937 (95% confidence interval [CI], 0.895–0.965). The best MHR cut-off value was > 10.11 with a sensitivity of 87.50% (95% CI, 77.6–94.1) and a specificity of 88.03% (95% CI, 81.5–92.9)
Lastly, MHR values significantly differed according to gender, being higher among males compared to females (9.41 [6.75–12.07] versus 8.02 [5.94–10.57] respectively; P = 0.0463) (Fig. 6).
We analyzed patients according to anti-hypertensive drugs class using Mann–Whitney test. In patients with RH (P = 0.7319) and in patients without RH (P = 0.4365) there was no difference for RAAS versus other anti-hypertensive drugs and MHR.
Moreover, MHR positively correlates with diabetes ellitus (ρ = 0.253; P = 0.0002), white blood cells (ρ = 0.664; P < 0.0001) and C-reactive protein (ρ = 0.563; P < 0.0001) (Fig. 7).
Excluding dialysis patients from statistical analysis, all results were confirmed and remained significant except for the difference in MHR value according to gender (P = 0.0888). Conversely, in the group of dialysis patients the only variable independently related to MHR at the multiple regression analysis was C-reactive protein (P = 0.0028) and the independent relationships with RH and the number of anti-hypertensive drugs were lost (P = 0.1369 and P = 0.3075 respectively).
Discussion
The present study shows how MHR value is significantly linked to the number of anti-hypertensive drugs needed in CKD patients and how it is associated with the tendency to develop RH. At multiple regression analysis, RH and the number of anti-hypertensive medication resulted in being independent correlated to MHR.
This close connection between HDL and monocyte has been confirmed in many studies which affirmed that the increased number of monocytes and HDL reduction may contribute to a major risk of plaque formation, progression of atherosclerosis [31, 32] and a consequently increased CVD risk [33,34,35,36].
Sarov-Blat et al. [37] indicated an activated pro-inflammatory state of both monocytes and monocyte-derived macrophages in low HDL subjects that may constitute a novel parameter of risk associated with HDL deficiency. Their study enlightened how several inflammatory cytokine genes including interleukin-1beta, interleukin-8 and tumor necrosis factor-alpha were highly expressed in low HDL subjects. A previous study conducted in dipper and non-dipper hypertensive patients underlined that MHR was significantly higher in the non-dipper hypertension group compared with control (P < 0.001) and dipper hypertension groups (P = 0.03) [38]. In line with these results, in our study, we found out a strong connection between arterial hypertension and MHR and, in particular, an impressive increase of MHR values in patients with RH compared with the remaining cohort. The number of anti-hypertensive drugs was directly proportional to MHR values in the whole study cohort and in the group of patients without RH. Moreover, RH and the number of anti-hypertensive drugs independently correlated with MHR. MHR could thus represent a valid tool to evaluate the efficacy of anti-hypertensive therapy administered in CKD patients by monitoring its trend during follow-up, to improve a tailored therapeutic approach.
MHR may also represent an efficient indicator of hypertensive complications as demonstrated by Aydin et al. [39], who underlined the connection between this ratio and asymptomatic organ damage in patients affected by primary arterial hypertension in terms of increased carotid intima-media thickness, left ventricular mass index, and urinary protein and albumin levels. In this setting, a high MHR value can predict the risk of adverse cardiovascular outcomes, as previously reported by Kanbay et al. [40]. Importantly, we found that MHR can identify patients with RH with high sensibility and specificity. MHR was also inversely related to eGFR in the whole cohort of patients, as previously demonstrated by a large cross-sectional study showing that MHR was independently associated with reduced renal function [41]. In this study, the value of MHR, in patients with normal renal function, was 0.40 ± 0.24.
Moreover, individuals with CKD had low level of apolipoprotein A-I (apoA-I), which exerts a fundamental role in the HDL homeostasis, making HDL more susceptible to catabolism [42].
A higher absolute count of monocytes is linked with a worsening in the biology of kidney disease progression [43], while lower HDL levels could be related to an increased risk for CKD onset and/or its progression [44,45,46].
In our cohort, MHR also positively correlated to C-Reactive Protein, emerging as a potential biomarker of inflammation. This finding confirms that this ratio can reflect the endothelial disfunction and OS at the basis of hypertension.
Furthermore, MHR values were higher in male population with lower levels in female patients. These findings are in line with the results of a study on the sex-specific association of MHR with SYNTAX score in patients with suspected stable coronary artery disease: male population showed a significantly higher MHR (12.2 [8.9–15.5] versus 9.3 [6.2–12.1], P < 0.001) accompanied by a higher prevalence of coronary artery disease (68.1% versus 53.4%, P < 0.001) [47]. This difference between genders could be partially explained by the variability of HDL status in males and females [48]. Gender difference in HDL is partly explained by more elevated estrogen levels that impair macrophages metabolic activity by lipid accumulation, while testosterone promotes it [49].
Conclusions
Our study has some limitations that need to be mentioned to interpret our results accurately. First, the present study is a retrospective, single-center study, including a relatively small number of patients. Secondly, our sample is quite homogeneous, consisting of only Caucasian adults, and then it is unknown whether our findings are also applicable to other racial or ethnic populations.
eGFR in this study is very low, which may reflect the specific pathophysiology of renal failure. Further studies must be performed to verify if the results will be similar to different kind of population. We underlined that a higher need of anti-hypertensive drugs is linked with a major value of MHR: a possibility that must be taken into consideration, is that the higher amounts of drugs can influence the HDL, monocytes and/or MHR status.
Hypertension is the most common chronic disease in the world and a significant cause of CKD progression. Our study suggests that MHR may be a useful and immediate tool to evaluate OS and inflammatory status in CKD patients affected by RH, to adopt more appropriate treatment strategies. A more efficient control of lipid status and the use of MHR as a predictor of efficacy of anti-hypertensive therapy may show their significant benefits in long-term follow-up trials, but prospective studies are needed to confirm our results.
References
Go AS, Chertow GM, Fan D, McCulloch C, Hsu C (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305
Untersteller K, Meissl S, Trieb M, Emrich IE, Zawada AM, Holzer M, Knuplez E, Fliser D, Heine GH, Marsche G (2018) HDL functionality and cardiovascular outcome among nondialysis chronic kidney disease patients. J Lipid Res 59(7):1256–1265
Balla S, Nusair MB, Alpert MA (2013) Risk factors for atherosclerosis in patients with chronic kidney disease: recognition and management. Curr Opin Pharmacol 13(2):192–199
Vaziri ND, Navab M, Fogelman AM (2010) HDL metabolism and activity in chronic kidney disease. Nat Rev Nephrol 6(5):287–296
Maeda S, Nakanishi S, Yoneda M, Awaya T, Yamane K, Hirano T, Kohno N (2012) Associations between small dense LDL, HDL subfractions (HDL2, HDL3) and risk of atherosclerosis in Japanese-Americans. J Atheroscler Thromb 19(5):444–452
Zwijsen RM, de Haan LH, Kuivenhoven JA, Nusselder IC (1991) Modulation of low-density lipoprotein-induced inhibition of intercellular communication by antioxidants and high-density lipoproteins. Food Chem Toxicol 29(9):615–620
Bandeali S, Farmer J (2012) High-density lipoprotein and atherosclerosis: the role of antioxidant activity. Curr Atheroscler Rep 14(2):101–107
Mackness B, Mackness M (2012) The antioxidant properties of high-density lipoproteins in atherosclerosis. Panminerva Med 54(2):83–90
Conti G, Caccamo D, Siligato R, Gembillo G, Satta E, Pazzano D, Carucci N, Carella A, Campo GD, Salvo A, Santoro D (2019) Association of higher advanced oxidation protein products (AOPPs) levels in patients with diabetic and hypertensive nephropathy. Med (Kaunas) 55(10):7
Gembillo G, Cernaro V, Salvo A, Siligato R, Laudani A, Buemi M, Santoro D (2019) Role of vitamin D status in diabetic patients with renal disease. Med (Kaunas) 55(6):273
Pugh D, Gallacher PJ, Dhaun N (2020) Management of hypertension in chronic kidney disease [published correction appears in Drugs 2020 Aug 25]. Drugs 79(4):365–379. https://doi.org/10.1007/s40265-019-1064-1
Sun HJ (2019) Current opinion for hypertension in renal fibrosis. Adv Exp Med Biol 1165:37–47. https://doi.org/10.1007/978-981-13-8871-2_3
McCarty MF (2006) Adjuvant strategies for prevention of glomerulosclerosis. Med Hypotheses 67(6):1277–1296
Klahr S, Morrissey JJ (2000) The role of vasoactive compounds, growth factors and cytokines in the progression of renal disease. Kidney Int Suppl 7:S7-14
Nogueira A, Pires MJ, Oliveira PA (2017) Pathophysiological mechanisms of renal fibrosis: a review of animal models and therapeutic strategies. In Vivo 31(1):1–22. https://doi.org/10.21873/invivo.11019
Cernaro V, Loddo S, Macaione V et al (2020) RAS inhibition modulates kynurenine levels in a CKD population with and without type 2 diabetes mellitus. Int Urol Nephrol 52(6):1125–1133. https://doi.org/10.1007/s11255-020-02469-z
Remuzzi G, Benigni A, Remuzzi A (2006) Mechanisms of progression and regression of renal lesions of chronic nephropathies and diabetes. J Clin Invest 116(2):288–296
Klahr S, Morrissey J (2002) Obstructive nephropathy and renal fibrosis. Am J Physiol Renal Physiol 283(5):F861-875
Mennuni S, Rubattu S, Pierelli G, Tocci G, Fofi C, Volpe M (2014) Hypertension and kidneys: unraveling complex molecular mechanisms underlying hypertensive renal damage. J Hum Hypertens 28:74–79
Nicholls SJ, Dusting GJ, Cutri B, Bao S, Drummond GR, Rye KA, Barter PJ (2005) Reconstituted high-density lipoproteins inhibit the acute pro-oxidant and proinflammatory vascular changes induced by a periarterial collar in normocholesterolemic rabbits. Circulation 111:1543–1550
Tedgui A, Mallat Z (2001) Anti-inflammatory mechanisms in the vascular wall. Circ Res 88:877–887
Xia P, Vadas MA, Rye KA, Barter PJ, Gamble JR (1999) High density lipoproteins (HDL) interrupt the sphingosine kinase signaling pathway. A possible mechanism for protection against atherosclerosis by HDL. J Biol Chem 274:33143–33147
Nicholls SJ, Nelson AJ (2019) HDL and cardiovascular disease. Pathology 51(2):142–147
Ganjali S, Gotto AM Jr, Ruscica M, Atkin SL, Butler AE, Banach M, Sahebkar A (2018) Monocyte-to-HDL-cholesterol ratio as a prognostic marker in cardiovascular diseases. J Cell Physiol 233(12):9237–9246
Kuvin JT, Rämet ME, Patel AR, Pandian NG, Mendelsohn ME, Karas RH (2002) A novel mechanism for the beneficial vascular effects of high-density lipoprotein cholesterol: enhanced vasorelaxation and increased endothelial nitric oxide synthase expression. Am Heart J 144(1):165–172
Linton MRF, Yancey PG, Davies SS et al (2019) The role of lipids and lipoproteins in atherosclerosis. [Updated 2019 Jan 3]. In: Feingold KR, Anawalt B, Boyce A et al (eds) Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK343489/
Canpolat U, Cetin EH, Cetin S, Aydin S, Akboga MK, Yayla C, Turak O, Aras D, Aydogdu S (2016) Association of monocyte-to-HDL cholesterol ratio with slow coronary flow is linked to systemic inflammation. Clin Appl Thromb Hemost 22:476–482. https://doi.org/10.1177/1076029615594002
Viedt C, Orth SR (2002) Monocyte chemoattractant protein-1 (MCP-1) in the kidney: does it more than simply attract monocytes? Nephrol Dial Transplant 17(12):2043–2047. https://doi.org/10.1093/ndt/17.12.2043 (PMID: 12454208)
Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39(33):3021–3104
Levey A, Stevens L, Schmid C, Zhang YL, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Yvan-Charvet L, Pagler T, Gautier EL, Avagyan S, Siry RL, Han S, Welch CL, Wang N, Randolph GJ, Snoeck HW, Tall AR (2010) ATP-binding cassette transporters and HDL suppress hematopoietic stem cell proliferation. Science 328(5986):1689–1693
Patel VK, Williams H, Li SCH, Fletcher JP, Medbury HJ (2017) Monocyte inflammatory profile is specific for individuals and associated with altered blood lipid levels. Atherosclerosis 263:15–23
Karataş MB, Çanga Y, Özcan KS, Ipek G, Güngör B, Onuk T, Durmuş G, Öz A, Karaca M, Bolca O (2016) Monocyte to high-density lipoprotein ratio as a new prognostic marker in patients with STEMI undergoing primary percutaneous coronary intervention. Am J Emerg Med 34(2):240–244
Cetin EHO, Cetin MS, Canpolat U, Aydin S, Topaloglu S, Aras D, Aydogdu S (2015) Monocyte/HDL-cholesterol ratio predicts the definite stent thrombosis after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Biomark Med 9(10):967–977
You S, Zhong C, Zheng D, Xu J, Zhang X, Liu H, Zhang Y, Shi J, Huang Z, Cao Y, Liu CF (2017) Monocyte to HDL cholesterol ratio is associated with discharge and 3- month outcome in patients with acute intracerebral hemorrhage. J Neurol Sci 372:157–161
Dogan A, Oylumlu M (2017) Increased monocyte-to-HDL cholesterol ratio is related to cardiac syndrome X. Acta Cardiol 72(5):516–521
Sarov-Blat L, Kiss RS, Haidar B, Kavaslar N, Jaye M, Bertiaux M, Steplewski K, Hurle MR, Sprecher D, McPherson R, Marcel YL (2007) Predominance of a proinflammatory phenotype in monocyte-derived macrophages from subjects with low plasma HDL-cholesterol. Arterioscler Thromb Vasc Biol 27(5):1115–1122
Selcuk M, Yildirim E, Saylik F (2019) Comparison of monocyte with high density lipoprotein cholesterol ratio in dipper and nondipper hypertensive patients. Biomark Med 13(15):1289–1296
Aydin E, Ates I, Fettah Arikan M, Yilmaz N, Dede F (2017) The ratio of monocyte frequency to HDL cholesterol level as a predictor of asymptomatic organ damage in patients with primary hypertension. Hypertens Res 40(8):758–764
Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, Karaman M, Oguz Y, Eyileten T, Vural A, Covic A, Goldsmith D, Turak O, Yilmaz MI (2014) Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol 46:1619–1625
Shi WR, Wang HY, Chen S, Guo XF, Li Z, Sun YX (2019) The impact of monocyte to high-density lipoprotein ratio on reduced renal function: insights from a large population. Biomark Med 13(9):773–783
Batista MC, Welty FK, Diffenderfer MR et al (2004) (2004) Apolipoprotein A-I, B-100, and B-48 metabolism in subjects with chronic kidney disease, obesity, and the metabolic syndrome. Metabolism 53(10):1255–1261. https://doi.org/10.1016/j.metabol.2004.05.001
Bowe B, Xie Y, Xian H, Li T, Al-Aly Z (2017) Association between monocyte count and risk of incident CKD and progression to ESRD. Clin J Am Soc Nephrol 12(4):603–613
Cases A, Coll E (2005) Dyslipidemia and the progression of renal disease in chronic renal failure patients. Kidney Int Suppl 99:S87-93
Bae JC, Han JM, Kwon S, Jee JH, Yu TY, Lee MK, Kim JH (2016) LDL-C/apoB and HDL-C/apoA-1 ratios predict incident chronic kidney disease in a large apparently healthy cohort. Atherosclerosis 251:170–176
Bowe B, Xie Y, Xian H, Balasubramanian S, Al-Aly Z (2016) Low levels of high-density lipoprotein cholesterol increase the risk of incident kidney disease and its progression. Kidney Int 89(4):886–896
Xu W, Guan H, Gao D, Pan J, Wang Z, Alam M, Lian J, Zhou J (2019) Sex-specific association of monocyte count to high-density lipoprotein ratio with SYNTAX score in patients with suspected stable coronary artery disease. Med (Baltim). 98(41):e17536
Davis CE, Williams DH, Oganov RG, Tao SC, Rywik SL, Stein Y, Little JA (1996) Sex difference in high density lipoprotein cholesterol in six countries. Am J Epidemiol 143:1100–1106
Rossouw JE (2002) Hormones, genetic factors, and gender differences in cardiovascular disease. Cardiovasc Res 53:550–557
Acknowledgements
We thank the nurse staff of the Unit of Nephrology and Dialysis for their help with the blood sampling and the blood pressure measurement of the patients.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, GG, DS, RS; data curation, RS, GG, AS, AR, GS; formal analysis, VC, VCA and GG; investigation, GG, DS; methodology, GG, GC and DS; supervision, GG, GC and DS; writing—original draft, GG, RS, DS and ES; writing—review & editing, GF, RS, GG and VC. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gembillo, G., Siligato, R., Cernaro, V. et al. Monocyte to HDL ratio: a novel marker of resistant hypertension in CKD patients. Int Urol Nephrol 54, 395–403 (2022). https://doi.org/10.1007/s11255-021-02904-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02904-9