Abstract
The aim of this study was to characterize the phenotypes and genotypes of Staphylococcus aureus isolated from raw bovine milk in Hokkaido, Japan. S. aureus isolates were identified in 135 of 436 milk samples from cows with and without signs of mastitis from three farms in Hokkaido. These clinical isolates were characterized for antimicrobial susceptibility patterns, molecular typing using phage-open-reading frame typing (POT), coagulase gene type, virulence genes, and biofilm-associated genes and were evaluated for biofilm-forming ability. Most isolates were susceptible to the antimicrobial agents tested. The highest rate of resistance was to ampicillin. Molecular typing of all S. aureus isolates indicated a predominance of coagulase type VI and 0–17–34 POT type, and virulence genes were highly prevalent in the isolates from all farms. Moreover, a high percentage of the 0-17–34 POT type isolates showed extensive formation of biofilm. These findings will help veterinarians and farmers to understand the epidemiology of S. aureus so that they can monitor the transmission and spread of this pathogen and control it more effectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bovine mastitis is a disease that causes substantial economic losses worldwide and can be classified as clinical or subclinical. Dairy cows with clinical mastitis show severe clinical signs (abnormal udder size and shape, abnormal milk secretion, and reduced milk production), whereas subclinical mastitis may not show any signs or symptoms and cause no visible changes in the milk (Seegers et al. 2003; Sinha et al. 2014). Staphylococcus aureus is the most common causative organism in bovine mastitis and can produce toxins that affect both animal and human health (Srinivasan et al. 2006). S. aureus produces a number of toxins that have public health implications, such as staphylococcal enterotoxin, which causes food poisoning, and toxic shock syndrome toxin; these toxins are often detected in S. aureus isolated from cows with bovine mastitis (Srinivasan et al. 2006). Such toxins may adversely affect consumers of food that has been contaminated during processing, such as use of raw material contaminated with the enterotoxin or poor hygiene practice.
S. aureus is a leading cause of bovine mastitis and can produce many types of cytolytic toxins, including hemolysin (induced by the hla, hlb, hld, and hlg genes) and leukocidin. Leukocidin can lyse white blood cells, particularly when induced by the LukDE and LukM genes (Vrieling et al. 2016). Virulent, gene-encoding, secreted leukocidin toxins are associated with the neutrophil-killing agent secreted in bovine mastitis and cause tissue necrosis by damaging the mammary epithelial cells in the udder (Vrieling et al. 2016). Moreover, leukocidin is an important toxin in cell-cell interactions and in the formation of an insoluble nucleoprotein matrix during formation of biofilm (Gogoi-Tiwari et al. 2017).
Formation of biofilm is one of the antimicrobial resistance mechanisms used by S. aureus. This is an important characteristic of S. aureus and protects bacteria from the effects of antimicrobial agents, resulting in chronic infection in cows with mastitis. A biofilm is a cluster of bacterial cells that includes the extracellular matrix and water. The extracellular matrix is formed by intercellular adhesion of polysaccharides, which are synthesized at the locus of the ica gene. Other surface proteins that are also crucial in the formation of biofilm include biofilm-associated protein (Bap) (Latasa et al. 2006). Bap and polysaccharides are important in the intercellular adhesion step during formation of biofilm, which leads to increased microbial colonization and enhanced adhesion in the mammary gland (Cucarella et al. 2001).
Administration of an antimicrobial agent is important for the control and treatment of clinical and subclinical bovine mastitis. Therefore, the antimicrobial susceptibility of S. aureus is one of the factors used to determine the appropriate treatment for mastitis. The beta-lactam group of antimicrobials is widely used in the treatment of bovine mastitis. Similarly, penicillin is the drug of choice for treatment of S. aureus in human medicine; however, increased resistance to penicillin is now being reported (Rayner and Munckhof, 2005; Baba et al. 2012; Aslantas and Demir, 2016). Methicillin is a member of the beta-lactam group and is widely used to treat S. aureus, and bacteria that are resistant to methicillin are known as methicillin-resistant S. aureus (MRSA). Bovine mastitis caused by MRSA is resistant to most antimicrobial agents. Previous cases of bovine mastitis caused by MRSA have been of great concern in both human and animal health care systems and caused outbreaks in Japan and elsewhere (Wang et al. 2015; Hata, 2016; Guimaraes et al. 2017). The relationship between biofilm-forming ability and the genotype of S. aureus identified in raw bovine milk has not been well studied in Japan. The purpose of this study was to investigate the prevalence and phenotypic and genotypic characteristics of S. aureus, including MRSA, isolated in milk from cows with and without mastitis in Hokkaido, Japan.
Materials and methods
Sample collection and isolation of S. aureus
A cross-sectional study was performed in 436 raw milk samples collected from cows that were apparently healthy and cows with clinical mastitis on three farms in Hokkaido during 2016–2017. Farm A (n = 124) and farm B (n = 254) were private farms, and farm C (n = 58) was owned by a university. Raw milk samples were collected from more than 80% of the cows on each farm during routine farm service programs run by the Animal Health Laboratory, Department of Health and Environmental Sciences, School of Veterinary Medicine, Rakuno Gakuen University. All milk samples were collected into a sterile tube after cleaning the surface of the udder and teat using cotton swabs soaked in 75% alcohol and kept cool in an ice box while being transported to the laboratory for analysis. At the laboratory, the samples were cultured in tryptic soy broth (with 6% NaCl), incubated overnight at 37 °C, and then streaked onto Baird-Parker agar. After incubation at 37 °C for a second night, typical and suspected colonies of S. aureus were chosen for confirmation using the femA gene (Paule et al. 2004).
Antimicrobial susceptibility testing
An antimicrobial susceptibility test was conducted using the agar dilution method following the guidelines of the Clinical and Laboratory Standard Institute (CLSI, 2015). Briefly, serial twofold dilutions of a number of antibiotic agents were prepared in Mueller-Hinton agar for testing at concentrations of 0.125–512 μg/ml. The following antimicrobial agents sourced from Sigma-Aldrich (St. Louis, MO, USA) were tested: ampicillin (AMP), oxacillin (OXA), cefazolin (CEZ), enrofloxacin (ENR), ciprofloxacin (CIP), gentamicin (GEN), kanamycin (KAN), vancomycin (VAN), and erythromycin (ERY). Tetracycline (TET) was purchased from Wako Pure Chemical Industries (Osaka, Japan). Reference strains of S. aureus (ATCC 25913) and Enterococcus faecalis (ATCC 25212) were used as quality controls. The breakpoints of these antimicrobial agents were determined according to the interpretation criteria of the Clinical and Laboratory Standard Institute (CLSI, 2015).
Molecular analysis
Genotyping by the POT and coagulase gene methods
A commercial multiplex polymerase chain reaction-based POT kit (Cica Geneus Staph POT, Kanto, Tokyo, Japan) was used for genomic characterization of S. aureus. In brief, this POT kit can detect the presence or absence of 22 target genes of S. aureus, and the results of typing are expressed as a triple POT score (Suzuki et al. 2006). The coagulase gene is one of the virulence factors in S. aureus and contributes to its pathogenicity. A coagulase typing (Cica Geneus Staph Coagulase Detection) kit was used for coagulase gene typing to investigate coa polymorphism.
Detection of virulence and biofilm-associated genes
The virulence genes that are important in human and animal health are the classical staphylococcal enterotoxins (sea to see), toxic shock syndrome toxin-1 (TSST-1) (Mehrotra et al. 2000), exfoliative toxin A (ETA; eta), exfoliative toxin B (ETB; etb), and leukocidin (LukDE and LukM) (Jarraud et al. 2002). The presence of these genes and biofilm formation-associated genes (ica and bap), which are associated with increased severity of mastitis (Cucarella et al. 2004), was evaluated by polymerase chain reaction.
Biofilm-forming assay
A microtiter plate biofilm assay (Merritt et al. 2005) was used to investigate the biofilm-forming ability of the S. aureus strains isolated from the apparently healthy cows and those with clinical mastitis. In brief, the microtiter plate biofilm assay detects the ability of S. aureus to form a biofilm on a 96-well plate. After incubation overnight, the biofilms are stained using crystal violet dye and measured using spectrophotometry. All isolates were tested four times and the results were averaged. Samples of medium that was not inoculated were used as a negative control. The optical density (OD) of the microplate biofilm assay was measured at 595 nm using a spectrophotometer that reads 96-well plates (Sunrise Rainbow Thermo, Tecan Group Ltd., Männedorf, Switzerland). The cut point for the OD of biofilm production was identified using the classification devised by Christensen et al. (1985). All strains were classified into four categories: ODi ≤ ODC = non-adherent; ODC < ODi ≤ 2 × ODC = weakly adherent; 2 × ODC < ODi ≤ 4 × ODC = moderately adherent; and 4 × ODC < ODi = strongly adherent (Yousefi et al. 2016).
Results
Positive ratio of S. aureus and characterization of antibiotic susceptibility testing
There was a detectable prevalence of S. aureus (28.2%, 123/436) in all samples (farm A, 31.5%, 39/124; farm B, 32.3%, 82/254; farm C, 3.4%, 2/58). One hundred and thirty-five isolates from the 123 positive samples were characterized as antibiotic-susceptible. Most S. aureus isolates were susceptible to the antimicrobial agents tested, and the highest resistance was to AMP (farm A, 76.1%; farm B, 89.7%). The next highest resistance rates were for OXA, CEZ, GEN, KAN, and ENR (2.2%) on farm A and for CEZ (1.1%) on farm B. One isolate showed multiple drug resistance (to AMP, OXA, CEZ, and KAN). No samples of S. aureus from farm C were resistant to antimicrobial agents (Table 1).
Molecular analysis
Results of genotyping by the POT and coagulase gene methods
The POT method could classify all of the S. aureus isolates in this study into six genotypic patterns, with 100% of the 0-17-34 POT type on farms A and C. There were six genotypes of S. aureus isolates on farm B and the POT type on farm B (Table 2). The most frequent type of POT on farm B was 0-17-34, with 52 isolates (59.8%, 52/87), followed by 0-1-0 (26.4%, 23/87) and 6-0-45 (6.9%, 6/87). Only the coa type VI genotype pattern was isolated from all S. aureus isolates on all farms.
Detection of virulence genes
One isolate was positive for the seb gene, and three were positive for the sec gene and co-harboring with the tsst gene. None of the S. aureus isolates from farm A or farm C were positive for the enterotoxin gene. Leukocidin (LukDE and LukM genes) was found in 100% (135/135) and 84.4% (114/135) of samples, respectively. Hemolysins (hla and hld genes) were found in 100% (135/135) and hlb was found in 95.6% (129/135) of the samples. No samples were positive for exfoliative toxin (eta, etb) or the hlg toxin genes. The percentages of toxin gene profile typing of S. aureus isolated from farms A, B, and C are shown in Table 2. No isolates tested were positive for MRSA.
Detection of biofilm-associated ica and bap genes and biofilm-forming assay
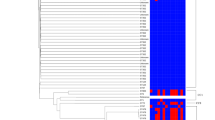
The detection rates for the biofilm-associated ica gene were 100.0% (46/46), 88.5% (77/87), and 100% (2/2) on farms A, B, and C, respectively. The isolates were positive for the ica gene in 92.6% (125/135) of cases and negative in 7.4% (10/135). None of the isolates was positive for the bap gene. S. aureus isolates on farm A were classified as strong biofilm producers (89.1%, 41/46) and those on farm B were classified as strong (16.1%, 14/87), moderate (5.7%, 5/87), weak (27.6%, 24/87), or not (50.6%, 44/87) biofilm producers. Two isolates from farm C were shown not to produce biofilm (100%, 2/2). The characteristics of the POT type are compared according to biofilm formation in all samples in Fig. 1.
Discussion
This study investigated the ratios, antimicrobial susceptibility, and genotypic characteristics of S. aureus in raw bovine milk in Hokkaido, Japan, using POT, the toxin profile, and biofilm-forming ability. The important finding of antimicrobial susceptibility testing in this study was the high rate of resistance to AMP in the samples. AMP is a member of the beta-lactam or penicillin group of antimicrobials, which are the drugs most commonly used to treat bovine mastitis (Pol and Ruegg, 2007). However, several reports from Japan and a number of other countries suggest that members of the penicillin group are the antibiotics most frequently resistant to S. aureus isolated in milk samples from cows with bovine mastitis, and our findings are consistent with these reports (Pitkälä et al. 2004; Rayner and Munckhof, 2005; Baba et al. 2012; Aslantas and Demir, 2016). The results of phenotypic testing in our study suggest that other antimicrobial agents, such as OXA, CEZ, ENR, CIP, GEN, KAN, VAN, ERY, and TET, can be used to control S. aureus infection, which is consistent with another report (Pitkälä et al. 2004). The results of antimicrobial susceptibility testing in this study can be used to predict the likelihood of S. aureus infection being cured in cows with mastitis and to assist veterinarians when selecting antibiotic therapy for this condition. S. aureus isolates detected in routine practice should also be monitored for resistance to beta-lactam agents (Barkema et al. 2006).
In this study, all S. aureus isolates were type VI, which is consistent with previous reports on the coa gene in milk from cows with mastitis in Japan, indicating that type VI is a common causative organism in cases of mastitis (Nagase et al. 2002; Hata, 2016). These studies indicate that coa typing is not sufficient for genomic classification of S. aureus derived from bovine milk in Japan because all isolates showed this type, whereas there were several types of POT. We found that 0–17-34 was the most prevalent type of POT on all farms and showed a high percentage of leukocidin and hemolysin genes and strong formation of biofilm (32.6%). The high prevalence of leukocidin and hemolysin genes in this study is in line with that in a previous study of isolates from bovine and other domestic animals (Yamada et al. 2005). Leukocidin and hemolysin genes are located on a chromosome that potentially makes it easy for horizontal transmission to occur via bacteriophages in S. aureus (Yamada et al. 2005). Moreover, sec-producing strains are frequently found in milk from cows with mastitis in Japan and other countries (Nagase et al. 2002). The present study identified three isolates of POT type 6–0-45 that were sec-producing strains and co-harboring the tsst gene, which is again consistent with previous findings (Nagase et al. 2002). Furthermore, it has been suggested that sec promotes inflammation and chronic infection in the presence of mastitis (Ferens et al. 1998). However, all of the S. aureus-producing enterotoxin and toxic shock syndrome genes came from farm B. This indicates that a critical aspect for controlling the spread of virulent bacteria may be to limit the introduction of animals from high-risk sites. POT is useful in epidemiologic studies because of its rapid and highly discriminatory power (Nada et al. 2009). Moreover, other typing techniques, such as multilocus sequence typing, should also be used in genomic studies in order to understand the evolution and spread of resistant S. aureus strains and their role in buildup of biofilm (Bentley and Parkhill, 2015).
Conclusions
The findings of the present study suggest a considerable prevalence of S. aureus in raw bovine milk in Japan. Generally, different rates of S. aureus infection reflect differences in biosecurity measures, farm practices, and geographic locations. Furthermore, S. aureus strains that produce biofilm may cause mastitis to spread on farms and build up antimicrobial resistance because of treatment failure. In this study, the incidence of S. aureus resistance on farms A and B (both private farms) differed markedly from that on farm C (a university farm). An understanding of the differences in animal husbandry and biosecurity measures in place between privately owned farms, and government-funded farms may provide options for management of mastitis and for preventing its spread.
References
Aslantas, O. and Demir, C., 2016. Investigation of the antibiotic resistance and biofilm-forming ability of Staphylococcus aureus from subclinical bovine mastitis cases. Journal of Dairy Science, 99, 8607–8613.
Baba, K., Ishihara, K., Ozawa, M., Usui, M., Hiki, M., Tamura, Y. and Asai, T., 2012. Prevalence and mechanism of antimicrobial resistance in Staphylococcus aureus isolates from diseased cattle, swine and chickens in Japan. Journal of Veterinary Medical Science, 74, 561–565.
Barkema, H.W., Schukken, Y.H. and Zadoks, R.N., 2006. Invited review: the role of cow, pathogen, and treatment regimen in the therapeutic success of bovine Staphylococcus aureus mastitis. Journal of Dairy Science, 89, 1877–1895.
Bentley, S.D. and Parkhill, J., 2015. Genomic perspectives on the evolution and spread of bacterial pathogens. Proceedings of the Royal Society of London. Series B, Biological Sciences, 282, 20150488.
Christensen, G. D., Simpson, W. A., Younger, J. J., Baddour, L. M., Barrett, F. F., Melton, D. M. and Beachey, E. H., 1985. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. Journal of Clinical Microbiology, 22, 996–1006.
Clinical and Laboratory Standards Institute [CLSI], 2015. Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals. VET01S. Clinical and Laboratory Standards Institute. Wayne, PA.
Cucarella, C., Solano, C., Valle, J., Amorena, B., Lasa, I. and Penades, J. R. 2001. Bap, a Staphylococcus aureus surface protein involved in biofilm formation. Journal of Bacteriology 183, 2888–2896.
Cucarella, C., Tormo, M.Á., Úbeda, C., Trotonda, M.P., Monzón, M., Peris, C., Amorena, B., Lasa, Í. and Penadés, J.R., 2004. Role of biofilm-associated protein Bap in the pathogenesis of bovine Staphylococcus aureus. Infection and Immunity, 72, 2177–2185.
Ferens, W.A., Davis, W.C., Hamilton, M.J., Park, Y.H., Deobald, C.F., Fox, L. and Bohach, G., 1998. Activation of bovine lymphocyte subpopulations by staphylococcal enterotoxin C. Infection and Immunity, 66, 573–580.
Gogoi-Tiwari, J., Williams, V., Waryah, C.B., Costantino, P., Al-Salami, H., Mathavan, S., Wells, K., Tiwari, H.K., Hegde, N., Isloor, S., Al-Sallami, H. and Mukkur, T., 2017. Mammary gland pathology subsequent to acute infection with strong versus weak biofilm forming staphylococcus aureus bovine mastitis isolates: A pilot study using non-invasive mouse mastitis model. PLoS One. 12, 1–19.
Guimaraes, F.F., Manzi, M.P., Joaquim, S.F., Richini-Pereira, V.B. and Langoni, H., 2017. Short communication: Outbreak of methicillin-resistant Staphylococcus aureus (MRSA)-associated mastitis in a closed dairy herd. Journal of Dairy Science, 100, 726–730.
Hata, E., 2016. Bovine mastitis outbreak in Japan caused by methicillin-resistant Staphylococcus aureus New York/Japan clone. Journal of Veterinary Diagnostic Investigation 28, 291–298.
Jarraud, S., Mougel, C., Thioulouse, J., Lina, G., Meugnier, H., Forey, F., Etienne, J., Vandenesch, F. and Nesme, X., 2002. Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infection and Immunity, 70, 631–641.
Latasa, C., Solano, C., Penadés, J.R. and Lasa, I., 2006. Biofilm-associated proteins. Comptes Rendus Biologies, 329, 849–857.
Mehrotra, M., Wang, G., Johnson, W.M., 2000. Multiplex PCR for detection of genes for Staphylococcus aureus enterotoxins, exfoliative toxins, toxic shock syndrome toxin 1, and methicillin resistance. Journal of Clinical Microbiology 38, 1032–1035.
Merritt, J. H., Kadouri, D. E. and O'Toole, G. A., 2005. Growing and analyzing static biofilms. Current Protocols in Microbiology. Chapter 1, Unit 1B 1.
Nada, T., Yagi, T., Ohkura, T., Morishita, Y., Baba, H., Ohta, M. and Suzuki, M., 2009. Usefulness of phage open-reading frame typing method in an epidemiological study of an outbreak of methicillin-resistant Staphylococcus aureus infections. Japanese Journal of Infectious Diseases, 62, 386–389.
Nagase, N., Shimizu, A., Kawano, J., Yamashita, K. and Yoshimura, H., 2002. Characterization of Staphylococcus aureus strains isolated from bovine mastitis in Japan. Journal of Veterinary Medical Science, 64, 1169–1172.
Paule, S. M., Pasquariello, A. C., Hacek, D. M., Fisher, A. G., Thomson, R. B., Jr., Kaul, K. L. and Peterson, L. R., 2004. Direct detection of Staphylococcus aureus from adult and neonate nasal swab specimens using real-time polymerase chain reaction. Journal of Molecular Diagnostics, 6, 191–196.
Pol, M. and Ruegg, P.L., 2007. Relationship between antimicrobial drug usage and antimicrobial susceptibility of gram-positive mastitis pathogens. Journal of Dairy Science, 90, 262–273.
Pitkälä, A., Haveri, M., Pyörälä, S., Myllys, V. and Honkanen-Buzalski, T., 2004. Bovine mastitis in Finland 2001—prevalence, distribution of bacteria, and antimicrobial resistance. Journal of Dairy Science, 87, 2433–2441.
Rayner, C. and Munckhof, W.J., 2005. Antibiotics currently used in the treatment of infections caused by Staphylococcus aureus. Internal Medicine Journal, 35, Suppl 2, S3–16.
Seegers, H., Fourichon, C. and Beaudeau, F., 2003. Production effects related to mastitis and mastitis economics in dairy cattle herds. Veterinary Research, 34, 475–491.
Sinha, M.K., Thombare, N.N. and Mondal, B., 2014. Subclinical mastitis in dairy animals: Incidence, economics, and predisposing factors. Scientific World Journal, 2014, 523984.
Srinivasan, V., Sawant, AA., Gillespie, B., Headrick, SJ., Ceasaris, L and, Oliver, S., 2006. Prevalence of enterotoxin and toxic shock syndrome toxin genes in Staphylococcus aureus isolated from milk of cows with mastitis. Foodborne Pathogens and Disease, 3, 274–283.
Suzuki, M., Tawada, Y., Kato, M., Hori, H., Mamiya, N., Hayashi, Y. and Sakae, K. 2006. Development of a rapid strain differentiation method for methicillin-resistant Staphylococcus aureus isolated in Japan by detecting phage-derived open-reading frames. Journal of Applied Microbiology, 101, 938–947.
Vrieling, M., Boerhout, E.M., Van Wigcheren, G.F., Koymans, K.J., Mols-Vorstermans, T.G., De Haas, C.J.C., Aerts, P.C., Daemen, I.J.J.M., Van Kessel, K.P.M., Koets, A.P., Rutten, V.P.M.G., Nuijten, P.J.M., Van Strijp, J.A.G. and Benedictus, L., 2016. LukMF′ is the major secreted leukocidin of bovine Staphylococcus aureus and is produced in vivo during bovine mastitis. Scientific Reports, 6, 1–12.
Wang, D., Wang, Z., Yan, Z., Wu, J., Ali, T., Li, J., Lv, Y. and Han, B., 2015. Bovine mastitis Staphylococcus aureus: Antibiotic susceptibility profile, resistance genes and molecular typing of methicillin-resistant and methicillin-sensitive strains in China. Infection Genetics and Evolution 31, 9–16.
Yamada, T., Tochimaru, N., Nakasuji, S., Hata, E., Kobayashi, H., Eguchi, M., Kaneko, J., Kamio, Y., Kaidoh, T. and Takeuchi, S., 2005. Leukotoxin family genes in Staphylococcus aureus isolated from domestic animals and prevalence of lukM-lukF-PV genes by bacteriophages in bovine isolates. Veterinary Microbiology, 110, 97–103.
Yousefi, M., Pourmand, M. R., Fallah, F., Hashemi, A., Mashhadi, R. and Nazari-Alam, A., 2016. Characterization of Staphylococcus aureus biofilm formation in urinary tract infection. Iranian Journal of Public Health, 45, 485–493.
Funding
This work was financially supported by Rakuno Gakuen University, Hokkaido, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thongratsakul, S., Usui, M., Higuchi, H. et al. Prevalence and characterization of Staphylococcus aureus isolated in raw milk from cows in Hokkaido, Japan. Trop Anim Health Prod 52, 1631–1637 (2020). https://doi.org/10.1007/s11250-019-02169-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11250-019-02169-6