Abstract
Purpose
No study has investigated the clinical and radiographic risk factors for the deterioration of quality of life (QOL) beyond 6 months after osteoporotic vertebral fractures (OVF). The purpose of this study was to identify the predictors associated with poor QOL improvement after OVF.
Methods
This post hoc analysis included 166 women aged 65–85 years with acute 1-level OVFs. For the patient-reported outcome measures, scores on the European Quality of Life-5 Dimensions (EQ-5D) scale, and visual analogue scale (VAS) for low back pain were used. Lateral radiography at 0, 12, and 48 weeks and magnetic resonance imaging (MRI) at enrollment and at 48 weeks were performed. The associations between baseline variables with change scores for EQ-5D were investigated using a multiple linear regression model.
Results
Univariate analysis showed that time since fracture, EQ-5D score, and VAS for low back pain at 0 week showed significant association with increased EQ-5D score from 0 to 48 weeks. According to the multiple regression analysis, the following equation was obtained: increased EQ-5D score from 0 to 48 weeks = 1.305 – 0.978 × EQ-5D at 0 week – 0.021 × VAS for low back pain at 0 week – 0.006 × age + (fluid-intensity T2-weighted MR image patterns: − 0.037, except for fluid-intensity T2-weighted MR image patterns: + 0.037).
Conclusion
In conclusion, older patients with severe low back pain and fluid-intensity T2-weighted MR image patterns were more likely to have lower QOL improvements after OVFs and may therefore need extra support to improve QOL
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures are the hallmark of osteoporosis and are commonly associated with deterioration in quality of life (QOL) [1]. While most acute vertebral fractures heal with kyphotic deformities and height loss, some vertebral fractures develop non-union [2]. Kyphotic deformities and/or non-union can often lead to reduced mobility and chronic pain, which limit everyday activities [3]. Reduced activities can lead to increased isolation and can cause depression. Several reports have shown that patients with osteoporotic vertebral fractures (OVFs) suffer from a loss of independence [4, 5]. Collectively, these factors arising from OVFs could have a negative impact on the QOL of osteoporotic patients. Indeed, a prospective cohort study concluded that acute OVF was the beginning of a long-lasting severe deterioration of the patient’s health [6].
Regardless of the high prevalence and incidence of OVFs, little is known about the long-term clinical course of acute OVFs. To the best of our knowledge, there are no studies that have investigated the clinical and radiographic risk factors for poor QOL improvement beyond 6 months after OVF. We believe that identifying the risk factors for poor QOL improvement after OVF is essential for implementing preventive measures and improving the clinical outcomes of OVF.
The purpose of this study was to identify the predictors associated with QOL improvement, with a focus on clinical factors, patient-reported outcome measures (PROMs), and radiographic assessments.
Methods
This study involves a post hoc analysis of a previous prospective randomized study that compared the effectiveness of rigid and soft braces for acute thoracolumbar OVFs (UMIN000014876) [7]. Briefly, the original trial enrolled patients with acute thoracolumbar OVF from 71 hospitals; 141 of these patients were randomly assigned to wear rigid braces, and 143 were assigned to wear soft braces. This study was approved by each hospital’s institutional review board, and informed consent was obtained from all participants included in the study. Detailed inclusion and exclusion criteria of this study have been described previously [7].
The original study enrolled 284 patients. Reasons for dropout during the 48-week follow-up period included the following: 2 patients due to changes in osteoporosis medication (bisphosphonate, 1; teriparatide, 1), 6 due to operations (for neurological deficits, 4; for severe pain, 1; for lumbar spinal stenosis, 1), 5 due to their own decision, 2 for dementia progression, 3 because they changed hospitals, 3 because of death, 1 for pneumonia, 29 for missing MRI at enrollment, 33 for missing MRI at 48 weeks, and 34 with no reason given. Finally, 166 patients with 48 weeks of follow-up were included in this study.
The current analysis included patients with 1-level acute thoracolumbar OVF who had received either rigid- or soft-brace treatment. In addition, the patients had undergone lateral radiography at 0, 12, and 48 weeks, and magnetic resonance imaging (MRI) at enrollment and at 48 weeks.
Patient-reported outcome measures
For the PROMs, scores on the European Quality of Life-5 Dimensions (EQ-5D-3L; range − 0.111 to 1, with higher scores indicating a better QOL) instrument [8] and a visual analogue scale (VAS) score for low back pain (range 0–10, with higher scores indicating more severe pain) [9] were used. These PROMs were provided by patients when they visited the hospital at 0, 12, and 48 weeks after brace application.
Radiographic assessment
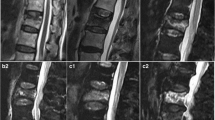
In the radiographic analysis, the anterior vertebral body compression percentage [10], which is defined as the ratio between the vertical height of the compressed anterior section of the injured vertebral body and the posterior vertebral body height at the same level, was measured. For assessment of the MRI findings in the acute phase, we classified the MRI findings into T1 diffuse low-intensity patterns or T1 non-diffuse low-intensity patterns (except for diffuse low-intensity T1-weighted image patterns) and T2 fluid-intensity patterns or T2 non-fluid-intensity patterns (except for fluid-intensity T2-weighted image patterns) according to the previous reports [11, 12]. Non-union was defined as a recognizable gas- or fluid-filled cleft separating the superior and inferior end plates on MRI and radiography at the 48-week follow-up.
Data analysis
An analysis of variance with repeated measures was used as the primary statistical tool to analyze the data over time. When there was a significant main effect of time, we performed paired t test with Bonferroni correction to identify differences between different time points.
The associations between baseline variables with change scores (the difference from 0 to 48 weeks) for EQ-5D were investigated in a multiple linear regression model. First, predictors associated with the dependent variable at a p value ≤ 0.25 in univariate regression analyses were carried forward to the second step of the analysis [13]. Second, the remaining predictors were included in a backward multiple regression analysis along with the baseline equivalent (EQ-5D score at 0 week) of the dependent variable. Including the baseline equivalent is a standard procedure in prediction analysis, because this variable is usually the most important predictor in the regression model [14]. Predictors with a p value > 0.1 were removed.
For all statistical analyses, JMP version 12 (SAS Institute, Cary, NC, USA), EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) and a graphic user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [15, 16] were used. We imputed the missing data measurements with data obtained using the Multiple Imputation by Chained Equations package in R. We chose 20 iterations for multiple imputation. All tests were 2-sided, and p values < 0.05 were considered significant.
Results
Patient demographics
A total of 166 patients were included from the original study. The baseline characteristics of the patients are shown in Table 1.
Patient-reported outcome measures and radiographic assessments
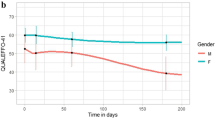
Table 2 shows the differences in PROMs and radiographic assessments during follow-ups. There was a significant main effect of time in EQ-5D (p < 0.001), VAS for low back pain (p < 0.001), and anterior vertebral body compression percentage (p < 0.001). There was a significant difference in EQ-5D between 0 and 12 weeks, 0 week and 48 weeks, and 12 weeks and 48 weeks (p < 0.001, p < 0.001, and p = 0.01, respectively). While there was a significant difference in VAS for low back pain between 0 and 12 weeks, and 0 and 48 weeks (p < 0.001 and p < 0.001), there was no significant difference in VAS for low back pain between 12 and 48 weeks (p > 0.99). There was a significant difference in anterior vertebral body compression percentage between 0 and 12 weeks, 0 week and 48 weeks, and 12 weeks and 48 weeks (p < 0.001, p < 0.001, and p = 0.003, respectively) (Fig. 1).
Trends in the study outcomes. European Quality of Life-5 Dimensions (EQ-5D), visual analogue scale (VAS) for low back pain, and anterior vertebral body compression percentage. Shown are the means with 95% confidence intervals at baseline and each follow-up. *p < 0.05; NS not significant, EQ-5D European quality of life-5 dimensions, VAS visual analogue scale
Independent predictors of increased EQ-5D score from 0 to 48 weeks
The associations between baseline variables with change scores (the difference from 0 to 48 weeks) for EQ-5D were investigated in the univariate regression model (Table 3). As a result, time since fracture, EQ-5D score, and VAS for low back pain at 0 week showed significant association with an increase in EQ-5D score from 0 to 48 weeks (Table 3). Then, the independent predictors for increased EQ-5D score from 0 to 48 weeks were evaluated using a multiple regression analysis. Based on the univariate analysis, the dependent variable was defined as the increase in EQ-5D score from 0 to 48 weeks, and the independent variables were age, time since fracture, EQ-5D score at 0 week, VAS for low back pain at 0 week, MRI T1 findings, and MRI T2 findings. As a result, the independent baseline predictors were identified as VAS for low back pain at 0 week (regression coefficient = − 0.021, p < 0.001) and age (regression coefficient = − 0.006, p = 0.03) (Table 4). According to this prediction model, following equation was obtained: increased EQ-5D score from 0 to 48 weeks = 1.305 – 0.978 × EQ-5D at 0 week – 0.021 × VAS for low back pain at 0 week – 0.006 × age + (fluid-intensity T2-weighted MR image patterns: − 0.037, except for fluid-intensity T2-weighted MR image patterns: + 0.037): R2 = 0.71 (Fig. 2). According to the value of the variance inflation factor of each variable, the variables in the final model were controlled for multicollinearity. These results show that patients with a mild low back pain in the acute phase were more likely to improve their QOL, relative to those with a severe low back pain. This prediction model also shows that younger patients were more likely to improve their QOL compared with older patients.
Discussion
This study investigated the predictors of poor QOL improvement after acute OVFs. The EQ-5D score improved over time, but the VAS for low back pain did not differ significantly between 12 and 48 weeks. Univariate analysis showed that time since fracture, EQ-5D score, and VAS for low back pain at 0 week showed significant association with increased EQ-5D score from 0 to 48 weeks. Multiple regression analysis showed that the independent baseline predictors were identified as VAS for low back pain at 0 week and age. According to the prediction model, an increase in EQ-5D score from 0 to 48 weeks = 1.305 – 0.978 × EQ-5D at 0 week – 0.021 × VAS for low back pain at 0 week – 0.006 × age + (fluid-intensity T2-weighted MR image patterns: − 0.037, except for fluid-intensity T2-weighted MR image patterns: + 0.037). To the best of our knowledge, this study is the first to investigate the predictive value of PROMs and radiographic assessments for predicting changes in QOL 48 weeks after acute OVFs.
Univariate analysis showed that time since fracture had significant association with increased EQ-5D score from 0 to 48 weeks. Because this study was a secondary analysis of prospective randomized study examining the effect of brace treatment, patients who had brace treatment interventions early were likely to have better QOL improvement. Indeed, a randomized prospective study showed that brace treatment improved QOL after OVFs [17]. On the other hand, there was no significant difference in the improvement in QOL between the different types of braces in this study. Collectively, it may be better to fit a rigid or soft brace after OVFs as soon as possible. Naturally, future prospective studies should be conducted to determine whether to provide brace treatment for acute OVFs or not.
We found that old age and severe low back pain in the acute phase were significant predictors for low QOL improvement at 48 weeks after OVFs. Moreover, multiple regression analysis revealed that fluid-intensity T2-weighted MR image patterns were included in the prediction model. Therefore, in the presence of fluid-intensity T2-weighted MR image patterns in older patients with severe low back pain after OVFs in the acute phase, it might be better to consider intervention to prevent the acute pain from developing into chronic deterioration of QOL. Regarding surgical interventions, one prospective randomized study showed that percutaneous vertebroplasty did not result in statistically significant greater pain relief, improvement of QOL, and physical functioning than a sham procedure during 12 months’ follow-up among patients with acute OVFs with VAS for back pain > 5 [18]. In contrast, another prospective study reported that early balloon kyphoplasty improved QOL and prevented vertebral body deformities at 6 months after injury more effectively than conservative treatment in patients with acute OVFs with a VAS for back pain > 5 and MRI T2 diffuse low- or fluid-intensity image patterns [19]. Based on the results of this study, when considering surgical interventions for OVFs in the acute phase to improve patient’s QOL, not only VAS scores, but also age and fluid-intensity T2-weighted MR image patterns might be considered to accurately select candidates who really need surgical interventions.
This study has several limitations. First, this study is a post hoc analysis of a subset of patients from the original study. Therefore, it does not represent all patients originally evaluated because not all radiographic assessments and PROMs were available, primarily due to lack of follow-up. Thus, attrition bias might limit the internal validity of this study. Second, we did not perform BMD assessment. Although the severity of osteoporosis might affect QOL, a lower BMD does not necessarily reflect an impaired QOL. Indeed, Albayrak et al. showed that there were no statistical differences between the osteoporosis and normal BMD groups in terms of VAS and QOL Questionnaire of the European Foundation for Osteoporosis total scores [20]. Third, the exclusion criteria in the original study may include factors that may contribute to a poor QOL. Hence, patients with the poorest QOL may be excluded from the study. However, we established this exclusion criterion to focus on the process of recovery from worsening QOL due to fresh OVFs. Lastly, because the patients in the present study were women of an advanced age, it might be difficult to apply these findings to men and younger individuals. Consequently, more studies across sexes and age ranges are warranted.
In conclusion, (a) VAS for low back pain in the acute phase and age contributed significantly to the improvement in the QOL of Japanese women with OVF over the course of a year; (b) the more severe the low back pain and the older the patient, the lesser the improvement in QOL; and (c) MRI T2 non-fluid-intensity patterns might protect QOL. Patients with these risk factors may therefore need extra support to reach a sufficient improvement of QOL. These findings may help physicians select an appropriate treatment strategy to prevent persistent deterioration in QOL after OVF.
References
Rostom, S., Allali, F., Bennani, L., Abouqal, R., & Hajjaj-Hassouni, N. (2012). The prevalence of vertebral fractures and health-related quality of life in postmenopausal women. Rheumatology International, 32(4), 971–980.
Inose, H., Kato, T., Ichimura, S., Nakamura, H., Hoshino, M., Togawa, D., et al. (2020). Risk factors of nonunion after acute osteoporotic vertebral fractures: A prospective multicenter cohort study. Spine (Phila Pa 1976), 45, 895.
Haczynski, J., & Jakimiuk, A. (2001). Vertebral fractures: a hidden problem of osteoporosis. Medical Science Monitor, 7(5), 1108–1117.
Hall, S. E., Criddle, R. A., Comito, T. L., & Prince, R. L. (1999). A case-control study of quality of life and functional impairment in women with long-standing vertebral osteoporotic fracture. Osteoporosis International, 9(6), 508–515.
Paier, G. S. (1996). Specter of the crone: The experience of vertebral fracture. ANS Advances in Nursing Science, 18(3), 27–36.
Suzuki, N., Ogikubo, O., & Hansson, T. (2008). The course of the acute vertebral body fragility fracture: Its effect on pain, disability and quality of life during 12 months. European Spine Journal, 17(10), 1380–1390.
Kato, T., Inose, H., Ichimura, S., Tokuhashi, Y., Nakamura, H., Hoshino, M., et al. (2019). Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: A prospective, randomized, Multicenter Study. J Clin Med, 8(2), 198.
Group TE. (1990). EuroQol–a new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
McCormack, H. M., Horne, D. J., & Sheather, S. (1988). Clinical applications of visual analogue scales: A critical review. Psychological Medicine, 18(4), 1007–1019.
Keynan, O., Fisher, C. G., Vaccaro, A., Fehlings, M. G., Oner, F. C., Dietz, J., et al. (2006). Radiographic measurement parameters in thoracolumbar fractures: A systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976), 31(5), E156–E165.
Tsujio, T., Nakamura, H., Terai, H., Hoshino, M., Namikawa, T., Matsumura, A., et al. (2011). Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: A prospective multicenter study. Spine (Phila Pa 1976), 36(15), 1229–1235.
Inose, H., Kato, T., Ichimura, S., Nakamura, H., Hoshino, M., Togawa, D., et al. (2020). Predictors of residual low back pain after acute osteoporotic compression fracture. Journal of Orthopaedic Science., S0949–2658(20), 30135–4.
Bursac, Z., Gauss, C. H., Williams, D. K., & Hosmer, D. W. (2008). Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine, 3, 17–17.
Kasl, S. V., & Jones, B. A. (2003). An epidemiological perspective on research design, measurement, and surveillance strategies. Handbook of occupational health psychology (pp. 379–398). Washington: American Psychological Association.
Team RC. (2013). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing.
Kanda, Y. (2013). Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplantation, 48(3), 452–458.
Pfeifer, M., Kohlwey, L., Begerow, B., & Minne, H. W. (2011). Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: A randomized trial. American Journal of Physical Medicine and Rehabilitation, 90(10), 805–815.
Firanescu, C. E., de Vries, J., Lodder, P., Venmans, A., Schoemaker, M. C., Smeets, A. J., et al. (2018). Vertebroplasty versus sham procedure for painful acute osteoporotic vertebral compression fractures (VERTOS IV): randomised sham controlled clinical trial. BMJ, 9(361), k1551.
Hoshino, M., Takahashi, S., Yasuda, H., Terai, H., Watanabe, K., Hayashi, K., et al. (2019). Balloon kyphoplasty versus conservative treatment for acute osteoporotic vertebral fractures with poor prognostic factors: propensity score matched analysis using data from two prospective multicenter studies. Spine (Phila Pa 1976), 44(2), 110–117.
Albayrak, I., Aydogmus, M., Ozerbil, O. M., & Levendoglu, F. (2016). The association between bone mineral density, quality of life, quality of sleep and fatigue. Acta Clinica Belgica, 71(2), 92–98.
Funding
This work was supported by Grants-in-Aid from the Japan Agency for Medical Research and Development (Grant Number 16dk0110008h0003, to AO).
Author information
Authors and Affiliations
Contributions
HI, TK, HN, MH, DT, ToH, YT, TO, HH, TT, KS, YS, MT, KO, SM, KT, MY, TaH, TY, and AO (1) provided substantial contributions to the conception or design of the study or the acquisition, analysis, or interpretation of data; (2) drafted the paper or revised it critically for important intellectual content; (3) provided final approval of the version to be published; and (4) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Hiroyuki Inose, Tsuyoshi Kato, Hiroaki Nakamura, Masatoshi Hoshino, Daisuke Togawa, Toru Hirano, Yasuaki Tokuhashi, Tetsuro Ohba, Hirotaka Haro, Takashi Tsuji, Kimiaki Sato, Yutaka Sasao, Masahiko Takahata, Koji Otani, Suketaka Momoshima, Kunihiko Takahashi, Masato Yuasa, Takashi Hirai, Toshitaka Yoshii, and Atsushi Okawa declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Written informed consent was obtained from the patients for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Inose, H., Kato, T., Nakamura, H. et al. Predictors for quality of life improvement after acute osteoporotic vertebral fracture: results of post hoc analysis of a prospective randomized study. Qual Life Res 30, 129–135 (2021). https://doi.org/10.1007/s11136-020-02629-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02629-9