Abstract
Purpose
Little is known about health-related quality of life (HRQoL) in patients with chronic hepatitis B virus (CHB) infection in the United States. Our goal is to understand factors associated with HRQoL in this population.
Methods
We conducted a survey to assess HRQoL and behavioral risks among patients with CHB infection from four large U.S. health care systems. Primary outcomes were generated from the SF-8 scale to assess HRQoL, as measured by the mental component scores (MCS) and physical component scores (PCS). The survey also measured socio-demographic information, hepatitis-related behavioral risk factors, treatment exposure/history, stress, and social support. We supplemented survey data with electronic health records data on patient income, insurance, disease severity, and comorbidities. Multivariate analysis was used to estimate and compare adjusted least square means of MCS and PCS, and examine which risk factors were associated with lower MCS and PCS.
Results
Nine hundred sixty-nine patients (44.6%) responded to the survey. Current life stressors and unemployment were associated with both lower MCS and PCS results in multivariate analyses. Lower MCS was also associated with White race and low social support, while lower PCS was also associated with Medicaid insurance.
Conclusions
Stressful life events and unemployment were related to mental and physical health status of CHB patients. Those who have social support have better mental health; White and Medicaid patients are more likely to have poorer mental and physical health, respectively. Management of CHB patients should include stress management, social support, and financial or employment assistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated one million persons in the United States are chronically infected with hepatitis B virus (HBV) [1]. Chronic hepatitis B (CHB) infection can lead to cirrhosis or liver cancer, and the disease can be accompanied by a range of symptoms, including fatigue and loss of appetite. The impact of this disease on patients’ health-related quality of life (HRQoL) [2] is critical to understand in order to effectively manage the condition, since health entails both biomedical and psychosocial well-being [3]. Despite the importance placed on patients’ HRQoL in chronic disease management [4,5,6], such data from CHB patients in the United States remain scarce as most existing studies are on patients outside of the country [7,8,9,10,11]. Since socioeconomic status, health care, culture, and lifestyle affect HRQoL and these factors differ from country to country, understanding predictors of HRQoL in the United States CHB population is important in improving overall care.
In previous work, we identified factors that influence HRQoL of patients with chronic hepatitis C virus (HCV) infection [12]. Predictors of poor mental health, based on the PHQ-8 scale, and poor physical health, based on the SF-8 scale, included male gender, Black race, low education, unemployment, current life stressors, low social support, and high comorbidity. Data for this current study and the previous HCV study were obtained from the CHeCS (Chronic Hepatitis Cohort Study), an observational cohort study that assessed the epidemiology and clinical impact of chronic viral hepatitis in the United States [13, 14]. The study included a patient survey that asked patients about hepatitis-related risk factors, treatment exposures, additional demographic variables such as race, country of origin and education, and key psychosocial measures in the course and outcome of chronic hepatitis disease [15].
The goal of the current study was to identify factors associated with HRQoL among CHB patients living in the United States. HRQoL was measured using the Mental Component Score (MCS) and Physical Component Score (PCS) derived from the Short-Form 8 (SF-8) scale [16, 17]. This study was guided by the psychosocial-stressor model, which relies on the principle that exposure to environmental stressors and the availability of psychosocial resources impact health outcomes [18]. This stress model has been used in previous studies to assess the impact of stressful events on mental health outcomes [19, 20].
Methods
Study design and cohort selection
The study cohort was identified from electronic health records (EHRs) of 2,542,189 patients aged ≥ 18 years who received health care services between January 1, 2006 and December 31, 2011 at one of four sites: Geisinger Clinic, Danville, PA; Henry Ford Health System, Detroit MI; Kaiser Permanente-Northwest, Portland, OR; and Kaiser Permanente-Hawaii, Honolulu, HI. All patients who met a combination of laboratory-based and International Classification of Disease, ninth revision (ICD-9)-based criteria identifying them as having chronic viral hepatitis B virus infection (described elsewhere) [13, 14] were included in the study. Case confirmation was completed by trained medical abstractors, who reviewed EHRs to collect liver biopsy results and outside system laboratory reports. Electronic medical charts flagged by abstractors as missing evidence of CHB infection were reviewed under the supervision of a hepatitis clinician using clinician-developed criteria. Patients who were deceased, incarcerated, living in long-term care institutions, who had invalid addresses or disconnected telephone numbers, or were co-infected with HIV or HCV were excluded from the sample, resulting in a total of 2175 eligible patients.
The CHeCS investigation follows the guidelines of the U.S. Department of Health and Human Services regarding the protection of human subjects. The study protocol was reviewed and approved by an Institutional Review Board at each participating study site.
Data collection methods
Electronic data
We collected prospective and retrospective EHR data on participants, including demographic information, medical encounters, laboratory results, diagnoses, procedures data, and liver biopsy results. Complete observation time was defined as time from first evidence of hepatitis infection in the EHR (including retrospective data prior to January 1, 2006), until either the last known health system encounter or December 31, 2013.
Patient survey data
During 2011 to 2012, we mailed a survey to 2175 CHB CHeCS patients who met study hepatitis B cohort inclusion criteria [13], were known to be alive and not institutionalized, and had valid contact information. The patients could complete and return the mailed paper survey or send back a response card to request a telephone survey. If the paper survey was not received via U.S. mail in a few weeks, up to eight telephone survey attempts were initiated. A nominal recruitment incentive was offered to survey responders to encourage survey response rate.
Outcome variables—health-related quality of life measures
HRQoL was assessed in the paper survey using the Short-Form 8 (SF-8), [16, 17] a measure derived from the Short-Form-36 (SF-36) instrument [21,22,23]. The SF-8 has been used extensively in studies monitoring population health [12, 24]. The SF-8 is composed of a total eight items, four of which assess mental status (vitality (energy/fatigue), social functioning, mental health, and role limitations due to emotional problems) and four that assess physical health status (general health, physical functioning, role limitations due to physical health problems and bodily pain). Each item has a 5- or 6-point response range. The mental component score (MCS) and physical component score (PCS) were calculated by weighting each SF-8 item using a norm-based scoring method given in the instrument guidelines [25]. Higher summary PCS and MCS scores indicate better health [26]. This scale has been normalized in the U.S. population whereby the average population mean is designed to be 50 (higher scores indicate better HRQoL), with a standard deviation of 10. SF-8 variables were treated as continuous variables in the current study, since the racial diversity of the of the sample prevented use of the SF-8 standardized norms for this study, which differ by racial group [25].
Covariates—risk factor measures
From survey
Socio-demographic, substance abuse, and medical data were collected from survey participants. Socio-demographic information included gender, age, race, country of birth, marital status, education level, and employment status. Self-reported substance abuse data were obtained from survey questions on history of injection drug use, history of drug or alcohol abuse treatment, and current cigarette smoking. The survey also collected data on current alcohol abuse using the AUDIT-C scale, a 3-item alcohol screen for hazardous drinkers or alcohol use disorders [27, 28]. The AUDIT-C is scored on a scale of 0–12 (scores of 0 reflect no alcohol use). In men, a score of 4 or more is considered positive; in women, a score of 3 or more is considered positive. Exposure to recent psychological stressors (negative life events) was measured using a validated stressful life events scale adopted from Holmes and Rahe Stress Scale [18], which queried about negative life stressors (death of a spouse/mate, divorce, death of a close family member, marriage, serious injury, family problems work problems or legal problems) within the past year. Patients who denied having any of these stressors were given a score of 0 (“no stress”); those who answered affirmatively to any single item were assigned a score of 1 (“moderate stress”) and those reporting 2 or more of these stressors a score of 2 was assigned (“high stress”). This measure has been used in previous studies [29, 30]. For this study, current social support was based on the sum of four questions about emotional, informational, and instrumental support (e.g., “someone available to help you if confined to a bed,” “someone available to give you good advice about a crisis,” “someone available to get together for relaxation,” “someone available to confide in or talk about your problems,” to which the patient could answer “none of the time,” “some of the time,” “most of the time” or “all of the time.” Points were assigned to each of the answers where no points were given to “none” answer, one point was assigned for each “some” answer, two points for each “most” answer, and three for each “all” answer. The sum of all four questions can range from 0 to 12. The patients were classified as having “low social support” if their total score was 4 or less, “moderate social support” if their score was 5 to 8, and “high social support” for scores 8 to 12. These survey items were based on items used in the Medical Outcomes Study [21, 31] and also used in previous mental health and disaster research [12, 20, 29, 30, 32]. Clinical survey questions included whether the respondent ever visited a liver or hepatitis specialist. To assess if patients were treatment naïve, we asked if they had ever been prescribed hepatitis drugs; those who have were queried about using hepatitis medications in the past 4 weeks and having stopped or changed their medication in the past 12 months.
From EHR
Survey data were supplemented with data derived from the EHR. Household income was estimated based on recent U.S. Census data corresponding to patients’ geocoded home addresses in the EHR [33]. Patient medical data from the EHR included type of insurance, history of liver transplantation, presence of cirrhosis (compensated or decompensated), and Charlson Comorbidity Score [34]. Charlson Comorbidity Score was calculated from standard diagnosis codes while omitting liver diseases, based on EHR data during this period up to the date of survey. Based on previous research, the score was used to categorize patients into 0, 1, or ≥ 2, where a score of 0 indicates no comorbidities, 1 indicates a single comorbidity that is relatively unlikely to result in mortality within the next year (e.g., diabetes, chronic lung disease), and a score of 2 or higher indicates multiple comorbidities or one or more moderate or severe comorbidities (e.g., diabetes with end-stage organ damage, tumor, etc.) [35]. Liver-related comorbidities were omitted from the Charlson score calculation for these analyses.
Having cirrhosis (compensated or decompensated) was defined as meeting any of these criteria during this same period: (a) FIB-4 score of > 5.17. FIB4 was calculated as [19, 20, 31] /{Platelet count(109/L)*[ALT(U/L)]1/2} from clinical laboratory values measured within 1 week of each other, excluding FIB4 values during hospitalizations, (b) Liver biopsy equivalent to Metavir F-4, (c) Cirrhosis ICD-9-CM (571.2, 571.5), (d) ICD9 codes indicative of hepatic decompensation: Liver failure with hepatorenal syndrome ICD-9-CM (572.4); hepatic encephalopathy ICD-9-CM (572.2); portal hypertension/portal decompression procedures ICD-9-CD and CPT (572.3, 37,140, 37,160, 37,180, 37,181, 37,182, 37,183); esophageal varices complications with bleeding ICD-9-CM and CPT (456.0, 456.20, 42.91, 44.91, 96.06, 43,204, 43,205, 43,243, 43,244, 43,400, 43,401); and ascites/paracentesis procedures ICD-9-CM & CPT (789.5, 789.59, 54.91, 49,080, 49,081). Patients with HIV or HCV-coinfection were excluded from further analysis.
Statistical methods
Descriptive statistics, including means, standard deviations, and proportions, were calculated and summarized in Tables 1 and 2. Statistical independence of categorical variables was tested with Chi-Square test. Outcome variables, MCS and PCS, were used as continuous variables and internal consistency reliability of SF-8 variables and Social Support measures were evaluated using Cronbach’s alpha. Cronbach’s alpha was 0.85 for both MCS and PCS, respectively, and 0.94 for Social Support. Variables with p-values less than 0.2 in bivariate models evaluating the relationship of individual covariates with MCS and PCS were subsequently considered in the multivariate models. We checked for interactions (between age/race, age/gender and gender/race in the MCS model and age/gender in the PCS model) but they were not significant. General Linear Models, adjusting for a priori confounders (age, gender, study site, and disease severity), were used to estimate the independent relationship between predictors and MCS or PCS. The Scheffé test was used for multiple comparison of the adjusted (least squares) means [36]. Statistical analyses were conducted using SAS v. 9.4 (SAS Institute, Cary, NC).
Results
Participation
We received a response rate of 48% (1000 responses from 2175 invited) for the surveys. Of the 1000 surveys, 31 were not included in this analysis due to missing data, yielding a sample of 969 (44.6%). Compared with non-respondents, survey respondents were significantly older (median age 50 years old vs 48 years old), more likely (all p < 0.01) to be: insured by Medicare (21.3% vs 16.9%), not born in the United States or Canada (66.3% vs 100%), and have no history of antiviral therapy at baseline (61.5% vs 73.4%). Race also differed among responders (69.3% Asian/Pacific Islander, 18.9% White, non-Hispanic, 10.2% Black, non-Hispanic, and 1.6% other) vs non-responders (65.4% Asian/Pacific Islander, 14.0% White, non-Hispanic, and 9.7% other), p < 0.001. Among surveyed patients, median time under observation for patients was 5.2 years, for a total of 6963 person-years of observation.
Population characteristics
Table 1 summarizes baseline demographic and clinical characteristics of survey respondents. Mean age was 49.1 ± 13.1 years, most were married (69.4%), and the most common race was Asian/Pacific Islander (70.5%). The majority (69.4%) of respondents were employed, 47.7% were college graduates, 72.1% were privately insured, and 64.5% reported experiencing no major life stressors in the past year (Table 1). Use of injection drugs and psychoactive substances such as alcohol and current cigarette smoking were not common in our study population; only 2.6% of responders reported a history of injection drug use and 3% reported drug abuse treatment. Nearly 12% reported current alcohol abuse and 3.4% reported having ever received treatment for alcohol abuse. Similarly, only 10.7% reported current cigarette smoking. At baseline, a sizeable minority had no history of treatment for HBV (40.3%), while 28.2% had received HBV treatment in the 4 weeks prior to completing the survey. Cirrhosis was rare (1.7%) and most (73.0%) had no medical comorbidities. Mean MCS and PCS were 51.3 ± 8.9 and 51.0 ± 8.6, respectively. The largest group of respondents was born in the United States or Canada (33.3%), followed by Southeast Asia (26.0%), then East Asia (24.7%), as shown in Table 2.
Factors associated with lower MCS
In bivariate analyses, many demographic, social, and medical status variables were associated with lower MCS, including younger age, White race (compared to Asians/Pacific Islanders), being born in the United States or Canada, low income, low levels of education, being unemployed, and having Medicaid insurance (compared to those with private insurance). Patients who experienced moderate or high levels of life stressors or had low levels of social support in the past year, reported drug or alcohol abuse, smoking cigarettes, had not taken medication for hepatitis or visited a hepatologist also had significantly lower MCS in bivariate analyses.
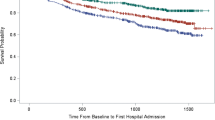
In the fully adjusted model (Table 3), White race had lower MCS than Asian/Pacific Islander, as well as unemployed participants, compared to those who were employed. Participants who had moderate and high stress had lower MCS than those who reported no stress. Similarly, low social support was associated with poorer MCS compared to those who received high social support. Figure 1 compares the adjusted least squares means of MCS for race, employment, stress, and social support. An inverse linear relationship between each stress level and MCS score can be observed in the figure. A similar relationship was observed for level of social support and MCS score although only low vs. high social support was statistically significant.
Adjusted Least Squares (LS) Means* for SF-8 Mental Component Score (N = 952). aModel adjusted for age, gender, current cigarette smoking, cirrhosis, Charlson score 33, and study site. Dots indicate adjusted LS means estimated using general linear model. Error bars indicate 95% confidence interval of the LS mean. Scheffé method comparisons with p < 0.05 are indicated
Factors associated with lower PCS
In bivariate models, race, unemployment, having low income, and having low education were associated with lower PCS. Medicare and Medicaid insurance, stress, and low social support, current cigarette smoking, and drug or alcohol abuse, and had not taken medication for hepatitis or visited a hepatologist were also significant in the bivariate analyses.
In multivariate analyses (Table 3), stressful life events and unemployment, both predictors of lower MCS, were also associated with lower PCS. In addition, lower PCS was significantly associated with receiving Medicare insurance. Figure 2 compares the adjusted least squares means of PCS for employment, stress, and insurance type. Like MCS, both unemployed and unknown employment status had lower PCS than those with full-time or part-time jobs. Patients with private insurance had higher PCS than both Medicaid and Medicare patients. An inverse linear relationship between each stress level and PCS score can be observed in the figure.
Adjusted Least Squares (LS) Means a for SF-8 Physical Component Score (N = 935). aModel adjusted for age, gender, current cigarette smoking, cirrhosis, Charlson score 33, and study site. Dots indicate adjusted LS means estimated using general linear model. Error bars indicate 95% confidence interval of the LS mean. Scheffé method comparisons with p < 0.05 are indicated
Discussion
Using a large survey on CHB patients’ behavioral risks and HRQoL in the United States, we found that stressful life events and unemployment were negatively associated with both MCS and PCS. Other key factors included low social support and White race (for MCS), and being on Medicaid (for PCS). Significant differences in MCS or PCS, even if not clinically significant, can be used to guide future interventions and policy. Use of psychoactive substances, injection drugs, alcohol, and tobacco were not common in our study population and lower than national averages [37,38,39].
Our finding that recent stressful life events were associated with poor mental and physical health is consistent with other findings in the literature [7, 19, 20, 40]. CHB requires life-long monitoring, and when left unmanaged, can lead to cirrhosis and hepatocellular carcinoma. Reactivation of HBV can occur even in patients who have had prolonged periods of undetectable viremia, burdening patients with psychological and economic stress [41]. Patients who are dealing with chronic hepatitis may be more vulnerable to mental health consequences of stressful life events such as the death of a spouse or problems at work. In our population, lower social support is also associated with poorer mental health.
Our study of poor mental and physical health in these patients was guided in part by a “psychosocial-stressor” model [18] used in previous investigations [19, 20]. This model suggests that exposure to psychosocial stressors and/or the availability of psychosocial resources, including socioeconomic resources, are important and can significantly impact health outcomes [29, 42,43,44]. There may be benefits in regularly assessing CHB patients regarding current stressors and HRQoL and using the information to refer patients to additional services, such as stress management and financial assistance, and smoking cessation counseling.
Unemployment was adversely associated with patients’ MCS and PCS in this and previous studies. In HCV [12] and CHB patients [45], unemployment was associated with poorer physical and mental health, and lower medication adherence in CHB patients [46]. Although Medicaid covers many persons with low/no income and fills the insurance coverage gap for those who are not completely covered by Medicare, limited access to covered services and providers, out of pocket cost-sharing for covered services, or caps on the number of medications covered may contribute to poorer physical health scores that Medicare and Medicaid patients had [47]. Financial assistance for these patients may provide some relief and reduce stress and having health navigators to determine barriers to care and provide information to improve access may be beneficial.
Patients of White race are more likely to report lower MCS compared to Asian/Pacific Islanders, perhaps reflecting different routes of viral acquisition (lifestyle vs. perinatal), as well as cultural differences in willingness to report poor mental health [48]. Injection drug use was more common in our cohort among persons of White and Black race compared to other groups [49], and is often associated with depression [50] and poor adherence to long-term therapy [51].
Strengths and limitations
Our study used survey data from four large and geographically and demographically diverse health systems, representing well over 2 million U.S. adults. However, the study was not strictly population-based and has a few limitations that limit the generalizability of the findings. First, our study was composed of mostly Asians and Pacific Islanders, who self-report much lower rates of mental disorders than other racial groups. Members of this population may have been less likely to report problems with mental health or may have reported them differently than non-Asian Americans [52]. However, the large number of Asians and Pacific Islanders in our sample reflects the prevalence of CHB in the United States: this population make up less than 5% of the total U.S. population, but account for more than 40% of the roughly one million chronically infected Americans [53]. Surveillance data from enhanced surveillance sites indicate about one-half of CHB infection cases in the United States are in patients of Asian or Pacific Islander descent. Second, our survey was offered only in English, thus persons without strong English literacy skills may have been unable to respond. This is a critical issue as surveillance data show that 71.3% of CHB infections in the United States are in persons born outside of the country. However, 66.4% of respondents to our survey (641 of 964 who responded to the question) reported being born outside the United States or Canada, suggesting that we successfully captured data from many non-U.S. born CHB patients. Nonetheless, providing the survey in only English likely resulted in some selection bias. Third, more than half of patients who were mailed surveys failed to respond, so it is possible that our sample was not representative of all eligible CHB patients at the participating institutions. EHR data show that survey responders were significantly more likely to be older, of White or Asian/Pacific Islander race, privately insured, born in the United States and treatment naïve at baseline relative to non-responders. Fourth, data are also subject to bias due to self-report and few reported the use of psychoactive substances, injection drugs, alcohol, and tobacco. However, issues of social desirability may bias self-report and self-selection bias is unavoidable in survey research. Concern over length of the survey also limited information we could collect on participants’ smoking status (e.g., past smoking and the use of other tobacco substances). However, the use of a mailed survey allowed us to reach a large number of CHB-infected patients and to obtain sensitive data such as feelings of depression, stressful life events, social support, and reported substance abuse. It is also important to note that due to its cross-sectional design, causal inference was not possible, and our findings could only demonstrate associations between variables. To keep the survey to a reasonable length, we used a modified version of the Medical Outcomes Survey and the Holmes and Rahe Scale for our measurement of social support and life stress, respectively. Although we did not use the full set of questions, these short scales have clear face validity, and in research has been shown to have concurrent, predictive, and discriminant validities and good Cronbach alpha results [12, 19, 20, 29, 30]. Finally, without a comparison group of healthy individuals, we are unable to specifically attribute the determinants of MCS and PCS to CHB.
Conclusions
In the adult population of CHB patients, stressful life events and unemployment were important factors related to both their mental and physical health status. CHB patients who have social support have better mental health and White and Medicaid patients are more likely to have poorer mental and physical health, respectively. Management of CHB patients should include stress management, social support, and financial or employment assistance.
References
Roberts, H., Kruszon-Moran, D., Ly, K. N., Hughes, E., Iqbal, K., Jiles, R. B., et al. (2016). Prevalence of chronic hepatitis B virus (HBV) infection in U.S. households: National Health and Nutrition Examination Survey (NHANES), 1988–2012. Hepatology,63(2), 388–397.
Mayo, N. (Ed.). (2015). Dictionary of quality of life and health outcomes measurement (Mayo, N.). Milwaukee, WI: International Society for Quality of Life Research.
Prince, M., Patel, V., Saxena, S., Maj, M., Maselko, J., Phillips, M. R., et al. (2007). No health without mental health. The Lancet,370(9590), 859–877.
Kendir, C., van den Akker, M., Vos, R., & Metsemakers, J. (2018). Cardiovascular disease patients have increased risk for comorbidity: A cross-sectional study in the Netherlands. European Journal of General Practice,24(1), 45–50.
Bhatti, Z., Salek, M., & Finlay, A. (2011). Chronic diseases influence major life changing decisions: A new domain in quality of life research. Journal of the Royal Society of Medicine,104(6), 241–250.
Bondini, S., Kallman, J., Dan, A., Younoszai, Z., Ramsey, L., Nader, F., et al. (2007). Health-related quality of life in patients with chronic hepatitis B. Liver International,27(8), 1119–1125.
Kim, S. J., Han, K. T., Lee, S. Y., & Park, E. C. (2015). Quality of life correlation with socioeconomic status in Korean hepatitis-B patients: A cross sectional study. Health and Quality of Life Outcomes,13(1), 55–67.
Ferreira, F. A., de Almeida-Neto, C., Teixeira, M. C., & Strauss, E. (2015). Health-related quality of life among blood donors with hepatitis B and hepatitis C: Longitudinal study before and after diagnosis. Revista Brasileira de Hematologia e Hemoterapia,37(6), 381–387.
Abedi, G., Rostami, F., & Nadi, A. (2015). Analyzing the dimensions of the quality of life in hepatitis B patients using confirmatory factor analysis. Global Journal of Health Science,7(7), 22–31.
Woo, G., Tomlinson, G., Yim, C., Lilly, L., Therapondos, G., Wong, D. K., et al. (2012). Health state utilities and quality of life in patients with hepatitis B. Canadian Journal of Gastroenterology and Hepatology,26(7), 445–451.
Zhuang, G., Zhang, M., Liu, Y., Guo, Y., Wu, Q., Zhou, K., et al. (2014). Significant impairment of health-related quality of life in mainland Chinese patients with chronic hepatitis B: A cross-sectional survey with pair-matched healthy controls. Health and Quality of Life Outcomes,12, 101–109.
Boscarino, J. A., Lu, M., Moorman, A. C., Gordon, S. C., Rupp, L. B., Spradling, P. R., et al. (2015). Predictors of poor mental and physical health status among patients with chronic hepatitis C infection: The Chronic Hepatitis Cohort Study (CHeCS). Hepatology,61(3), 802–811.
Moorman, A. C., Gordon, S. C., Rupp, L. B., Spradling, P. R., Teshale, E. H., Lu, M., et al. (2013). Baseline characteristics and mortality among people in care for chronic viral hepatitis: The chronic hepatitis cohort study. Clinical Infectious Diseases,56(1), 40–50.
Spradling, P. R., Rupp, L., Moorman, A. C., Lu, M., Teshale, E. H., & Gordon, S. C., et al. (2012). Hepatitis B and C virus infection among 1.2 million persons with access to care: Factors associated with testing and infection prevalence. Clinical Infectious Diseases,55(8), 1047–1055.
Center for Diseases Control (CDC). (2013). Locations and reasons for initial testing for hepatitis C infection–chronic hepatitis cohort study, United States, 2006–2010. MMWR. Morbidity and Mortality Weekly Report,62(32), 645–648.
Ware, J. E., Jr., Kosinski, M., Bjorner, J. B., Bayliss, M. S., Batenhorst, A., Dahlof, C. G., et al. (2003). Applications of computerized adaptive testing (CAT) to the assessment of headache impact. Quality of Life Research,12(8), 935–952.
Turner-Bowker, D. M., Bayliss, M. S., Ware, J. E., Jr., & Kosinski, M. (2003). Usefulness of the SF-8 Health Survey for comparing the impact of migraine and other conditions. Quality of Life Research,12(8), 1003–1012.
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Psychosomatic Research,11(2), 213–218.
Boscarino, J. A., & Adams, R. E. (2009). PTSD onset and course following the World Trade Center disaster: Findings and implications for future research. Social Psychiatry and Psychiatric Epidemiology,44(10), 887–898.
Boscarino, J. A., Hoffman, S. N., Adams, R. E., Figley, C. R., & Solhkhah, R. (2014). Mental health outcomes among vulnerable residents after Hurricane Sandy: Implications for disaster research and planning. American Journal of Disaster Medicine,9(2), 107–120.
Stewart, A. L., & Ware, J. E. (Eds.). (1992). Measuring functioning and well-being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press.
Stewart, A. L., Greenfield, S., Hays, R. D., Wells, K., Rogers, W. H., & Berry, S. D., et al. (1989). Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA,262(7), 907–913.
Stewart, A. L., Hays, R. D., & Ware, J. E. (1988). The MOS short-form general health survey. Reliability and validity in a patient population. Med Care,26(7), 724–735.
McDonald, S. D., Mickens, M. N., Goldberg-Looney, L. D., Mutchler, B. J., Ellwood, M. S., & Castillo, T. A. (2018). Mental disorder prevalence among U.S. Department of Veterans Affairs outpatients with spinal cord injuries. The Journal of Spinal Cord Medicine,41(6), 1–12.
Ware, J. E., & GlaxoSmithKline, (Eds.). (2001). How to score and interpret single-item health status measures: A manual for users of the of the SF-8 health survey : (with a supplement on the SF-6 health survey). Boston, MA: Lincoln, RI : QualityMetric, Inc.; Boston. MA: Health Assessment Lab.
Ware, J. E., Kosinski, M., Turner-Bowker, D. M., & Gandek, B. (Eds.). (2001). How to score the SF-8 Health Survey. Boston, MA: Health Assessment Lab.
Bradley, K. A., Bush, K. R., McDonell, M. B., Malone, T., & Fihn, S. D. (1998). Screening for problem drinking: Comparison of CAGE and AUDIT. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. J Gen Intern Med,13(6), 379–388.
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine,158(16), 1789–1795.
Adams, R. E., Boscarino, J. A., & Galea, S. (2006). Social and psychological resources and health outcomes after the World Trade Center disaster. Social Science and Medicine,62(1), 176–188.
Freedy, J. R., Kilpatrick, D. G., & Resnick, H. S. (1993). Natural disasters and mental health: Theory, assessment, and intervention. Journal of Social Behavior and Personality,8(5), 49–103.
Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science and Medicine,32(6), 705–714.
Galea, S., Ahern, J., Resnick, H., Kilpatrick, D., Bucuvalas, M., Gold, J., et al. (2002). Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine,346(13), 982–987.
National Center for Health Statistics (2003). U.S. Census 2000 population with bridged categories. (Vol. (PHS) 2003–1335). Hyattsville, MD: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
Deyo, R. A., Cherkin, D. C., & Ciol, M. A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology,45(6), 613–619.
Austin, S. R., Wong, Y. N., Uzzo, R. G., Beck, J. R., & Egleston, B. L. (2013). Why summary comorbidity measures such as the charlson comorbidity index and elixhauser score work. Medical Care,53(9), e65–72.
Scheffé, H. (1953). A method for judging all contrastsin the analysis of variance. Biometrika,40(1–2), 87–110.
Centers for Disease Control and Prevention. (2018). Current cigarette smoking among adults-United States, 2005–2016. Morbidity and Mortality Weekly Report,67(2), 53.
National Institute on Alcohol Abuse and Alcoholism (2017). Alcohol Facts and Statistics. https://pubs.niaaa.nih.gov/publications/AlcoholFacts&Stats/AlcoholFacts&Stats.pdf. Accessed March, 2018.
National Institute on Drug Abuse (2015). Nationwide Trends. https://www.drugabuse.gov/publications/drugfacts/nationwide-trends. Accessed March, 2018.
Bosma, H., Peter, R., Siegrist, J., & Marmot, M. (1988). Two alternative job stress models and the risk of coronary heart disease. American Journal of Public Health,88(1), 68–74.
Atesci, F. C., Cetin, B. C., Oguzhanoglu, N. K., Karadag, F., & Turgut, H. (2005). Psychiatric disorders and functioning in hepatitis B virus carriers. Psychosomatics,46(2), 142–147.
Adams, R. E., & Boscarino, J. A. (2011). A structural equation model of perievent panic and posttraumatic stress disorder after a community disaster. Journal of Traumatic Stress,24(1), 61–69.
Yamashita, J. (2012). A review of psychological assessments for disaster mental health studies. Psychological Trauma,4(6), 560–567.
Slobodin, O., Caspi, Y., Klein, E., Berger, B. D., & Hobfoll, S. E. (2011). Resource loss and posttraumatic responses in Bedouin members of the Israeli Defense Forces. Journal of Traumatic Stress,24(1), 54–60.
Karacaer, Z., Cakir, B., Erdem, H., Ugurlu, K., Durmus, G., Ince, N. K., et al. (2016). Quality of life and related factors among chronic hepatitis B-infected patients: A multi-center study, Turkey. Health and Quality of Life Outcomes,14(1), 153–162.
Tutuncu, E. E., Guner, R., Gurbuz, Y., Kaya Kalem, A., Ozturk, B., Hasanoglu, I., et al. (2017). Adherence to nucleoside/nucleotide analogue treatment in patients with chronic hepatitis B. Balkan Medical Journal,34(6), 540–545.
Eisenberg, J. M., & Power, E. J. (2000). Transforming insurance coverage into quality health care: Voltage drops from potential to delivered quality. JAMA,284(16), 2100–2107.
Margaretten, M., Yelin, E., Imboden, J., Graf, J., Barton, J., Katz, P., et al. (2009). Predictors of depression in a multiethnic cohort of patients with rheumatoid arthritis. Arthritis and Rheumatism,61(11), 1586–1591.
Center for Behavioral Health Statistics and Quality (2015). 2014 National Survey on Drug Use and Health: Detailed Tables. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs2014/NSDUH-DetTabs2014.pdf. Accessed June, 2019.
Ozkan, M., Corapcioglu, A., Balcioglu, I., Ertekin, E., Khan, S., Ozdemir, S., et al. (2006). Psychiatric morbidity and its effect on the quality of life of patients with chronic hepatitis B and hepatitis C. International Journal of Psychiatry in Medicine,36(3), 283–297.
Arnsten, J., Demas, P., Grant, R., Gourevitch, M., Farzadegan, H., Howard, A., et al. (2002). Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. JGIM,17(5), 377–381.
Coleman, K. J., Stewart, C., Waitzfelder, B. E., Zeber, J. E., Morales, L. S., Ahmed, A. T., et al. (2016). Racial-ethnic differences in psychiatric diagnoses and treatment across 11 health care systems in the mental health research network. Psychiatric Services (Washington, D. C.),67(7), 749–757.
Center for Diseases Control (2016). Surveillance for Viral Hepatitis – United States, 2014. https://www.cdc.gov/hepatitis/statistics/2014surveillance/commentary.htm#hepatitisB. Accessed May, 2017.
Acknowledgements
The CHeCS Investigators include the following investigators and sites: Scott D. Holmberg, Eyasu H. Teshale, Philip R. Spradling, Anne C. Moorman, Jian Xing, and Yuna Zhong, Division of Viral Hepatitis; National Centers for HIV, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), Centers for Disease Control and Prevention (CDC), Atlanta, Georgia; Stuart C. Gordon, David R. Nerenz, Mei Lu, Lois Lamerato, Jia Li, Loralee B. Rupp, Nonna Akkerman, Nancy Oja-Tebbe, Talan Zhang, Sheri Trudeau, and Yueren Zhou, Henry Ford Health System, Detroit, Michigan; Joseph A. Boscarino, Zahra S. Daar, and Robert E. Smith, Department of Epidemiology and Health Services Research, Geisinger Clinic, Danville, Pennsylvania; Yihe G. Daida, Connie Mah Trinacty, Jonathan W. Lai, and Carmen P. Wong, Center for Integrated Health Care Research, Kaiser Permanente-Hawaii, Honolulu, Hawaii; Mark A. Schmidt and Judy L. Donald, The Center for Health Research, Kaiser Permanente-Northwest, Portland, OR.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding
This study was funded by the Centers for Disease Control and Prevention and from Gilead Sciences. CHeCS was previously funded through May 2016 by the CDC Foundation, which received grants from AbbVie; Genentech, A Member of the Roche Group; Gilead Sciences; Janssen Pharmaceuticals, Inc. and Vertex Pharmaceuticals; past partial funders include Bristol-Myers Squibb. Granting corporations do not have access to CHeCS data and do not contribute to data analysis or writing of manuscripts.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Stuart C. Gordon receives grant/research support from AbbVie Pharmaceuticals, Conatus, CymaBay, Gilead Sciences, Intercept Pharmaceuticals, and Merck. He is also a consultant/advisor for Dova Pharmaceuticals and Intercept and serves as a speaker/teacher in programs sponsored by Dova. Mei Lu, Joseph A. Boscarino, Mark A. Schmidt, Yihe G. Daida, and Loralee B. Rupp receive research grant support from Gilead Sciences and Intercept Pharmaceuticals. Eyasu H. Teshale, Anne C. Moorman, and Philip R. Spradling have no conflicts of interest to report.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was reviewed and approved by an Institutional Review Board at each participating study site.
Informed consent
The IRB has waived Informed Consent and Authorization for the use of electronic health records in this study. Passive informed consent was obtained from all individual participants who completed the study survey.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
for the Chronic Hepatitis Cohort Study Investigators are listed in “Acknowledgements”.
Rights and permissions
About this article
Cite this article
Daida, Y.G., Boscarino, J.A., Moorman, A.C. et al. Mental and physical health status among chronic hepatitis B patients. Qual Life Res 29, 1567–1577 (2020). https://doi.org/10.1007/s11136-020-02416-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02416-6