Abstract
Purpose
Utility values are critical for cost-utility analyses that guide healthcare decisions. We aimed to compare the utility values of the 5-level EuroQoL-5Dimension (EQ-5D-5L) health states elicited from members of the general public and patients with heart disease or cancer.
Methods
In face-to-face interviews with 157 heart disease patients, 169 cancer patients, and 169 members from the general population, participants valued 10 EQ-5D-5L health states using a composite Time Trade-Off method.
Results
Pooling utility values for all health states, heart disease patients and cancer patients had mean utility values lower by 0.11 points (P value = 0.014) and 0.06 points (P value = 0.148), respectively, compared to the general population. Adjusting for sociodemographic characteristics, differences in health state utility values between the patient and the general populations were rendered non-significant, except that heart disease patients gave higher utility values (mean difference = 0.08; P value = 0.007) to mild health states than the general population. Difference in utility values, defined as utility value of a better health state minus that of a poorer health state, was higher among heart disease patients compared to the general population, before and after adjusting for sociodemographic characteristics.
Conclusions
Patients may differ from members of the general population in the strength of their preferences for hypothetical health states. Using utility values derived from the general population may under-estimate the comparative effectiveness of healthcare interventions for certain diseases, such as heart diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health state utility values are usually elicited from either the general population or patients [1,2,3]. General population-derived utility values have been recommended for use in cost-effectiveness analysis to inform decisions involving allocation of societal resources [4]. Health utility instruments such as the EuroQol–5Dimensions (EQ-5D) are designed to generate health state utility values based on the health preferences of the general population. Members of the general population, however, may have different health preferences compared to patients, and they may lack understanding of what it means to live in impaired health [5]. Therefore, patient-derived utility values are desirable for effectiveness analysis to inform clinical decision making from a patient-centered perspective.
The issue of whose preferences to use is only important insofar as health preferences differ between the populations. Some studies indicate that there are important differences between patient-derived and general population-derived health state values [6,7,8,9,10]. For example, a meta-analysis found that utility values elicited from patients tend to be higher than those elicited from the general population [8]. However, other studies, including a meta-analysis, report no or minimal difference in the utility values elicited from general and patient populations [9, 11,12,13]. The mixed findings could be due to multiple factors, including type of condition, severity of condition, and valuation method. For example, one study reports that health state values derived using the visual analog scale (VAS) method were similar between individuals with and without arthritis, but were different between individuals with and without heart disease [9]; utility values elicited from patients with arthritis and the general population using the VAS method were similar but values elicited from the two populations using the time trade-off (TTO) method were different [14]. The mixed findings may also be due to the fact that some of the studies were underpowered, poorly designed, or poorly executed [8].
In this study, we investigated the impact of chronic diseases on measurement of the utility of health states defined by the 5-level EuroQoL-5Dimension (EQ-5D-5L) questionnaire [15]. The EQ-5D-5L is a new version of EQ-5D, and has demonstrated better measurement properties than the 3-level EQ-5D (EQ-5D-3L) [16, 17]. The primary objective of this study was to compare two patient populations, heart disease and cancer patients, with the general population. The two diseases were selected because of their high disease burden globally [18, 19]. In all three groups, we elicited utility values for a set of 10 EQ-5D-5L health states using the TTO method. Both TTO and EQ-5D are recommended by the National Institute for Health and Care Excellence (NICE) for generating utility values in economic evaluations of health technologies [20].
Methods
Participants
Heart disease and cancer patients attending outpatient clinics at the National Heart Centre Singapore (NHCS) and the National Cancer Centre Singapore (NCCS), respectively, were invited to participate during their routine visits. The NHCS and NCCS are the largest capacity specialty centers in Singapore for cardiovascular disease and cancer patients, respectively. The main eligibility criterion for the heart disease patients was hospitalization primarily for a heart disease such as coronary heart disease or heart failure treatment in the last 5 years; this criterion was used to screen out patients with mild heart conditions. The main eligibility criterion for the cancer patients was to have histologically confirmed cancer of any type and stage in the last 5 years; this criterion was used to screen out cancer survivors. The study also included a sample from the general population recruited from three shopping malls in Singapore. All participants were between 21 and 80 years old, able to read and communicate in English or Chinese (Mandarin), and well enough for an interview. A quota sampling based on age and gender distributions similar to the Singapore census was used to generate the general population sample.
Valuation interview
The study design was cross-sectional, and consenting participants were interviewed face-to-face in a computer-assisted interviewing protocol. All interviews were conducted by the same trained interviewer using the EuroQol Valuation Technology (EQ-VT) computer program running from a laptop in either English or Chinese according to participant’s preference [21]. The interviews with the patients were conducted in the hospitals in a quiet waiting area; the general population participants were interviewed in a quiet place of the malls where they were recruited. The study was approved by the SingHealth Centralized Institutional Review Board.
The interviewer followed a standard interviewer script in all interviews [22]. Both the Chinese and English versions of the EQ-VT computer program and the interviewer script were tested among Singaporean general population as well as patient populations in pilot studies. The valuation tasks using the EQ-VT computer program were well understood and accepted by all three major local ethnicities (Chinese, Malay and Indian) in the general and patient populations [21]. The advantages of using a computer program include reduced interviewer burden, inter-interview variation, and errors and violation of interview protocol. The EQ-VT program is designed to collect data on the processes of each interview and upload the data daily to the server. By analyzing the process data, we were able to identify any errors the interviewer made and intervene timely whenever necessary.
The interviews started with some warm-up questions asking the participants to describe their own health using the EQ-5D-5L questionnaire. Subsequently, the TTO-based valuation task was explained to participants using the state of “in a wheelchair” as an example, after which three practice EQ-5D-5L health states were administered to familiarize participants with the task and EQ-5D-5L health states of varying severity. The practice states were followed by TTO valuation of a 10 EQ-5D-5L health states. The interviews ended with some feedback and background questions.
A detailed description of the TTO and the EQ-VT protocol can be found elsewhere [23]. Briefly, the objective of the task was to identify the point of preferential indifference between 10 years of life in the described target state, followed by death, and a shorter life (x ≤ 10 years) in full health, followed by death. With a defined utility value of 1 for 10 years in full health, the utility value of the target state can be calculated as x/10. For states considered to be worse than death (respondent preferred a life of 0–10 years in the target state), a lead-time of 10 years was added to both alternatives in order to elicit a negative utility value for the state. The utility value of a worse than death health state was calculated as (x−10)/10 such that the utility value of each health state is bounded at −1 and 1; 0 represents value for the ‘dead’ state.
In addition to the valuation interview, clinical information was collected from patients by interviewer or directly from their medical records. Clinical information included diagnoses, year of diagnosis, and clinical assessments such as New York Heart Association (NYHA) functional classification and Canadian Cardiovascular Society (CCS) functional classification of angina for heart disease patients; and cancer stage and Eastern Cooperative Oncology Group (ECOG) performance status for cancer patients. All participants were also asked to self-report their current and past chronic diseases.
The EQ-5D-5L health states
In this study, all participants were asked to value the same set of 10 health states, in random order. All health states were defined using the EQ-5D-5L system which contains five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and five functional levels for each dimension (broadly corresponding to no problems, slight problems, moderate problems, severe problems, and extreme problems). EQ-5D-5L health states are conventionally described using a 5-digit index, where the digits represent the functional level of each dimension in the conventional order of presentation (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). For example, the health state ‘11122’ indicates slight problems (level 2 severity) in both pain/discomfort and anxiety/depression and no problems in mobility, self-care, and usual activities. The 10 health states were 11122, 21121, 21222, 21232, 32232, 32333, 22224, 31242, 53343, and 33453. The first three health states (11122, 21121, 21222) with all dimensions at severity level either 1 or 2 were considered as ‘mild’ health states, the last four health states (22224, 31242, 53343, 33453) with at least one dimension at severity level either 4 or 5 were considered as ‘severe’ health states, and the remaining three health states (21232, 32232, 32333) were considered as ‘moderate’ health states.
Statistical analyses
The planned sample size for the study was 525 participants (175 heart disease patients, 175 cancer patients, and 175 participants from the general population). The sample size was estimated to detect a difference of 0.1 standardized effect size in mean value of the 10 elicited health states from a group of patients and general population using a two-sided test for 5% type-I error rate and 80% power, assuming 10% participants may provide logically inconsistent valuation or do not complete the interviews.
Participants who met the following criteria were excluded from the analysis: a) gave the same utility value to all the health states, b) gave negative or zero utility value to all health states (i.e., considered all health states worse than or equal to death). The use of stricter logical inconsistency criteria (i.e., further excluding participants who valued one or more mild states as equal to or lower than any severe states) was explored. It led to exclusion of more participants but had no material impact on results and therefore was not adopted.
We performed ordinary least-square (OLS) regression analysis to compare the mean utility values elicited from the patient groups with those of the general population group. The regression model was performed separately for each of the 10 health states, across 10 health states, the three mild health states (11122, 21121, 21222), the three moderate health states (21232, 32232, 32333), and the four severe health states (22224, 31242, 53343, 33453). Finally, these models were repeated by adjusting for ethnicity, gender, age, marital status, education level, employment status, religion, and household income level because the patient groups and the general population group differed in demographic and socioeconomic characteristics.
Lastly, we compared the differences in utility values between the health states as elicited from members of the general population, heart disease patients, and cancer patients. As the difference in utility values of two health states is usually used to approximate utility gained from transitions between the two health states [24], this comparison helped us to assess whether the different sets of utility values would give similar estimates when used to determine utility gained from health state transitions. First, differences in utility were calculated separately for the heart disease patient group, cancer patient group, and the general population group for 45 pairs of health states where one is no worse than the other in any of the five domains. Second, differences in the differences between a patient group and the general population group were presented using a line graph and tested by OLS regression models. The graph also presented the differences in differences adjusted for participants’ demographic and socioeconomic characteristics, calculated using the regression models performed separately for each pair of health states.
All the models involving more than one utility value per participant used the Eicker–Huber–White robust standard error for cluster data for statistical inference [25]. We also performed both unadjusted and adjusted analysis using mixed-effect models with participant-specific intercepts. The results were very similar to those based on OLS models with robust standard error. Hence, results of only OLS models were presented. All the analyses were carried out using Stata/MP 13.1 for Windows. A minimally important difference of 0.05 points for the utility values was considered to be of practical significance [26].
Results
Of 525 participants who completed the interview, 30 were excluded from analyses: 24 participants assigned the same value to all 10 health states, and six participants valued all the health states worse than or equal to death. There was no systematic difference in demographic and health characteristics between participants included and excluded from the analysis, except that slightly more heart disease patients (n = 18) were excluded compared to the general population participants (n = 6) and cancer patients (n = 6) (Online Appendix Table 1). Table 1 shows the demographic, socioeconomic, and health characteristics of the 495 participants included in the analyses (169 in the general population group, 157 in the heart disease patients group, and 169 in the cancer patients group). Participants in the patient groups were older, had lower education level, and poor self-reported general health compared to participants in the general population group. A total of 62 (37%) participants in the general population group self-reported to have one or more chronic diseases, such as hypertension (15%), hyper/dyslipidemia (12%), and lung diseases (10%). The majority of demographic characteristics of the general population sample were similar to the census population (Online Appendix Table 2) [27].
The majority of the heart disease patients reported no breathlessness with heavy or moderate exertion (95%), and had coronary artery disease (64%), atrial fibrillation (34%), arrhythmias (29%), myocardial infraction (28%), or heart failure (20%). Mean time from the most recent episode of symptom onset to the interview date was 1.2 years (SD 1.5). The majority of the heart disease patients (85%) had other chronic diseases such as hypertension (57%), hyper/dyslipidemia (59%), and diabetes mellitus (29%). Mean time from the most recent hospitalization due to a heart disease problem to the interview date was 1.4 years (SD 2.0). (Online Appendix Table 3).
The majority of the cancer patients reported ECOG performance status 0–1 (99.4%), and had breast cancer (29%), colorectal cancer (21%), or lymphoma (11%). The percentage of patients in cancer stages 0–1, 2–3, and 4 were 21, 42, and 36%, respectively. Mean time from the diagnosis of the most recent cancer to the interview date was 1.9 years (SD 1.4). (Online Appendix Table 4).
Only 5% of patients in the heart disease group self-reported to have had cancer. Similarly, 4% of patients in the cancer group have had heart disease, and less than 5% of participants in the general population group had either heart disease or cancer.
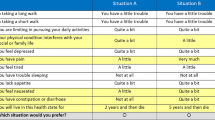
Table 2 summarizes the comparison of utility values between the patient groups and the general population group. Pooling all 10 states, heart disease patients displayed a mean utility value that was lower by 0.11 points (P value = 0.014) than the general population group. Heart disease patients valued moderate and severe health states lower by 0.05 points (P value = 0.353) and 0.25 points (P value <0.001), respectively, than members of the general public. There was no statistically significant difference in mean utility value for mild health states between the two groups (difference = 0.03). After adjusting for demographic and socioeconomic variables in the regression models, the overall difference weakened and became statistically non-significant. However, the mean utility value based on heart disease patients was lower by 0.05 (P value = 0.534) for severe health states, and higher by 0.08 points (P value = 0.007) and 0.09 points (P value = 0.176) for mild and moderate health states, respectively, than that based on the general population members.
Unlike heart disease patients, there was no statistically significant difference in mean utility value for all health states including mild, moderate, and severe health states between cancer patient group and the general population group. After taking the effects of demographic and socioeconomic characteristics into account, the mean differences in utility values between the two groups were smaller than the ones without adjustment and statistically non-significant (Table 2). Among all the covariates adjusted for the analysis, age had strongest association with utility (Wald test P < 0.0001; see Online Appendix Table 5). Older age was associated with lower utility value.
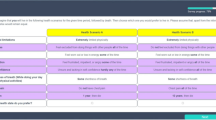
Mean (unadjusted and adjusted) differences in differences between selected health states for the heart disease patients versus the general population group are presented in Fig. 1. It shows that the covariate-adjusted differences in differences were higher than 0.05, a possibly minimally important difference for utility values, for 23 of 45 pairs of health states (51%; P value < 0.05 for 11 pairs), and lower than 0.05 for 13 pairs of health states (29%; P value ≥ 0.05 for 3 pairs) in heart disease patients than the general population group. Similar analysis comparing cancer patients and the general population group (Fig. 2) showed that adjusted differences in differences were greater than 0.05 for 7 of 45 pairs of health states (16%; P value ≥0.05 for all), and lower than 0.05 for 4 pairs (9%; P value ≥0.05 for all).
Discussion
Overall, both heart disease and cancer patients tended to value the utility of EQ-5D-5L defined health states lower than members of the general public. The difference between cancer patients and the general public was consistent across health states of different severity, and disappeared after adjusting for the differences in demographics. In contrast, the difference between heart disease patients and the general public depended on health state severity, and demographics explained the difference in severe states but did not fully account for the difference in mild and moderate states. These results suggest that whether the health preferences of patients and members of the general population differ depends on many factors.
So far two studies, conducted by Pickard et al. [13] and Gandhi et al. [9], compared the valuation of 3-level EQ-5D (EQ-5D-3L) health states between heart disease patients and the general population. Our study is consistent with the two studies; in that heart disease patients give mild and moderate EQ-5D-3L health states higher values compared to the general population, which could be explained by the theory of adaptation or coping. Patients are more likely to have experienced and adapted to mild and moderate health problems defined by EQ-5D-3L than healthy individuals. As a result, patients do not perceive those health states as intolerable or undesirable as the general public. A recent study of patients with type 2 diabetes mellitus reported similar results [6], suggesting that higher valuation of mild health problems may be a common phenomenon in some patient populations. On the other hand, our finding that heart disease patients give lower values to severe health states than the general population was not observed in previous studies. For example, Gandhi et al. [9] found the opposite—heart disease patients valued severe health states higher than the general public, which can be explained by adaptation. However, the adaptation theory could also explain low valuation of severe health problems. If the severe health problems are difficult to adapt to and their detrimental effects are also difficult to imagine, patients who had the experience could perceive them more undesirably than individuals who never had such experience [28]. Coincidentally, a recent study found that, compared to the general population, breast cancer and rheumatoid arthritis patients valued EQ-5D-5L defined mobility and self-care problems less undesirable but pain/discomfort and anxiety/depression more undesirable [29]. In another study, comparing value of depression states between individuals with and without depression has shown that individual with depression valued depression lower than the individual who have not experienced it [30]. These studies might be a good support to the theory we used to explain the low valuation of health problems by patients, considering these two facts: (1) physical problems such as partial paralysis are easier to adapt than sensational problems such as pain and depression if they are persistent; (2) three of the four severe health states we used in our study involved severe or extreme pain/discomfort or anxiety/depression and only one health state involved extreme mobility problems (i.e., unable to walk about). The reasons for not observing this result in previous studies could be due to use of small sample size as well as health states characterized mainly by physical health problems.
Pickard et al. [13] also compared valuation by cancer patients and the general population. It showed results similar to our study that cancer patients give slightly lower but statistically insignificant values than the general population. A study conducted by Krabbe et al. [14] showed that cancer patients give a higher value to EQ-5D-3L health states than the general population. However, the comparison did not adjust for the effects of demographic and socioeconomic characteristics; the patients were significantly older than the general population group in that study. It can be reasonably postulated that utility values derived from cancer patients and the general population could be similar if the effect of age had been adjusted for in that study. These consistent findings suggest that cancer patients and the general population may have very similar preferences for EQ-5D-5L health states. Therefore, the general population-based EQ-5D-5L value sets could be sufficient for measuring the utility of various health outcomes when the measurement should be based on the preferences of cancer patients such as in clinical decision making.
There are a few possible reasons for why heart disease and cancer patients were different in the valuation of EQ-5D-5L health states compared to the general population. For severe health states, it could be due to different levels of adaptation. It is possible that cancer patients adapt better to such health states than heart disease patients given that most of them have received surgery and/or chemotherapy, both of which have huge impact on patients’ health and quality of life. For mild and moderate health states, cancer patients might focus more on their impact on quality of life than heart disease patients and therefore they are willing to trade a slightly larger portion of their life expectancy (10 years in this study). It is also possible that, compared to members of the general public and heart disease patients of the same age, cancer patients are more likely to perceive their actual life expectancy to be shorter than 10 years and therefore they are more generous in trading the ‘extra’ life years in the given life expectancy. This trading behavior would lead to lower utility values for health states of all severities. It could offset the effect of adaptation and as a result make cancer patients similar to the general population in the valuation of health outcomes using the TTO method. Our finding that older age is associated with lower utility value in this study could be evidence for the effect of self-perceived life expectancy on TTO-based valuation using a standardized time frame. Further studies are needed to test the generalizability of the findings on the population/disease-specific valuation outcomes and ascertain the underlying valuation behaviors.
Our analysis of the differences in differences suggests that utility values derived from the general population will lead to smaller differences than utility values derived from heart disease patients, if those are used to determine utility gained from transitions between the studied health states. This means that the general population-based EQ-5D-5L value sets are less likely under-estimate treatment benefits for heart disease patients if they are used in clinical trials or other longitudinal studies. Therefore, it may be worthwhile to develop a heart disease patient-based EQ-5D-5L value set for use in studies for informing clinical decision making or other decision making in which patients’ health preferences are most relevant. On the other hand, differences in utility between EQ-5D-5L health states based on utility values derived from cancer patients and the general public were found to be quite similar, suggesting that the general population-based EQ-5D-5L value sets may be sufficient for use in clinical decision making for cancer patients. The differing results for heart diseases and cancers in this analysis suggest that patient-based EQ-5D-5L value sets, if needed for evaluating treatments, should be disease specific.
Our finding that older age is associated with lower health state valuation is in concordance with findings of previous studies using a similar valuation method [31, 32]. The effect of age on TTO values could be due to the different life experience and perceived responsibilities of young and old individuals. For young individuals, they may tend to look forward to more life experience and responsibilities in the future and therefore prefer longer life to better quality of life; for old individuals, they are likely to have experienced a lot and fulfilled their responsibilities in past lives and are willing to trade life years for a healthy life. Further studies are needed to test the generalizability of the finding in other patient populations.
Our study has several potential limitations. First, our study sample did not include inpatients. As inpatients are likely to be in worse functional status which was associated with lower utility values in heart disease patients in our study (data not shown), the difference in utility values between the heart disease patients and the general population might be under-estimated. Nevertheless, it would be difficult to conduct the very cognitively demanding valuation tasks with inpatients. Second, our study involved only cardiovascular diseases and cancers. Therefore, our specific study findings may not be generalizable to other patient populations. However, the observation that clinical groups differ in terms of how they value health is likely to be generalizable. Third, our general population sample was recruited from shopping malls. As shopping is generally a pleasant leisure activity which could have an impact on valuation of health, the magnitude of the difference observed between the patient populations and the general population might be different if a more representative general population sample had been used in the study. Fourth, the sample size for the study was powered enough for overall comparison (mean utility of all heath states) between the general population and a patient population. It was not powered for comparison between the populations for mild, moderate, and severe health states separately. Therefore, our study findings should be considered exploratory and need to be confirmed with a bigger study. Furthermore, due to limited number of health states and sample size, it was not possible to evaluate the impact of individual dimensions of EQ-5D-5L on differences in health state preferences. And, finally, the findings reported here are limited to the valuation of hypothetical health states. They may not be generalized to the valuation of experienced health states.
Conclusions
Patients with chronic diseases may differ from members of the general population in the strength of their preferences for hypothetical health states. The difference may depend on type of the disease, age of patients, and severity of the health states being valued. As a result, using utility values derived from the general population may under-estimate the comparative effectiveness of healthcare interventions for certain type of diseases, such as heart diseases. Larger studies involving more diverse patient groups and a wider range of health states would be required to confirm our study findings.
References
Brazier, J. E., Dixon, S., & Ratcliffe, J. (2009). The role of patient preferences in cost-effectiveness analysis. Pharmacoeconomics, 27(9), 705–712.
Stamuli, E. (2011). Health outcomes in economic evaluation: Who should value health? British Medical Bulletin, 97, 197–210.
Stiggelbout, A. M., & Vogel-Voogt, D. (2008). Health state utilities: A framework for studying the gap between the imagined and the real. Value in Health, 11(1), 76–87.
Drummond, M. F., & McGuire, A. (2001). Economic evaluation in health care: Merging theory with practice. USA: Oxford University Press.
Gandjour, A. (2010). Theoretical foundation of patient v. Population preferences in calculating QALYs. Medical Decision Making, 30(4), E57–E63.
Wang, P., Tai, E., Thumboo, J., Vrijhoef, H. J., & Luo, N. (2014). Does diabetes have an impact on health-state utility? A study of asians in singapore. The Patient, 7(3), 329–337.
Rowen, D., Mulhern, B., Banerjee, S., Tait, R., Watchurst, C., Smith, S. C., et al. (2014). Comparison of general population, patient, and carer utility values for dementia health States. Medical Decision Making, 35(1), 68–80.
Peeters, Y., & Stiggelbout, A. M. (2010). Health state valuations of patients and the general public analytically compared: A meta-analytical comparison of patient and population health state utilities. Value in Health, 13(2), 306–309.
Gandhi, M., Thumboo, J., Luo, N., Wee, H. L., & Cheung, Y. B. (2015). Do chronic disease patients value generic health states differently from individuals with no chronic disease? A case of a multicultural Asian population. Health and quality of life outcomes, 13, 8.
Gerhards, S. A., Evers, S. M., Sabel, P. W., & Huibers, M. J. (2011). Discrepancy in rating health-related quality of life of depression between patient and general population. Quality of Life Research, 20(2), 273–279.
Dolders, M. G., Zeegers, M. P., Groot, W., & Ament, A. (2006). A meta-analysis demonstrates no significant differences between patient and population preferences. Journal of Clinical Epidemiology, 59(7), 653–664.
Mulhern, B., Rowen, D., Snape, D., Jacoby, A., Marson, T., Hughes, D., et al. (2014). Valuations of epilepsy-specific health states: A comparison of patients with epilepsy and the general population. Epilepsy & Behavior, 36, 12–17.
Pickard, A. S., Tawk, R., & Shaw, J. W. (2013). The effect of chronic conditions on stated preferences for health. The European Journal of Health Economics, 14(4), 697–702.
Krabbe, P. F., Tromp, N., Ruers, T. J., & Reil, P. L. (2011). Are patients’ judgments of health status really different from the general population? Health and quality of life outcomes, 9, 31.
Herdman, M., Gudex, C., Lloyd, A., Janssen, M., Kind, P., Parkin, D., et al. (2011). Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research, 20(10), 1727–1736.
Pickard, A. S., De Leon, M. C., Kohlmann, T., Cella, D., & Rosenbloom, S. (2007). Psychometric comparison of the standard EQ-5D to a 5 level version in cancer patients. Medical Care, 45(3), 259–263.
Janssen, M., Pickard, A. S., Golicki, D., Gudex, C., Niewada, M., Scalone, L., et al. (2013). Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: A multi-country study. Quality of Life Research, 22(7), 1717–1727.
Deaton, C., Froelicher, E. S., Wu, L. H., Ho, C., Shishani, K., & Jaarsma, T. (2011). The global burden of cardiovascular disease. European Journal of Cardiovascular Nursing, 10, S5–S13.
Fitzmaurice, C., Dicker, D., Pain, A., Hamavid, H., Moradi-Lakeh, M., Maclntyre, M. F., et al. (2015). The global burden of cancer 2013. JAMA oncology, 1(4), 505–527.
National Institute for Health and Clinical Excellence. (2013). Guide to the methods of technology appraisal 2013. National Institute for Health and Clinical Excellence. Retrieved March 05, 2017, from https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781.
Luo, N., Li, M., Stolk, E. A., & Devlin, N. J. (2013). The effects of lead time and visual aids in TTO valuation: A study of the EQ-VT framework. The European Journal of Health Economics, 14(Suppl 1), S15–S24.
Oppe, M., Rand-Hendriksen, K., Shah, K., Ramos-Goni, J. M., & Luo, N. (2016). EuroQol protocols for time trade-off valuation of health outcomes. PharmacoEconomics, 34(10), 993–1004.
Oppe, M., Devlin, N. J., van Hout, B., Krabbe, P. F., & de Charro, F. (2014). A program of methodological research to arrive at the new international EQ-5D-5L valuation protocol. Value in Health, 17(4), 445–453.
Sonnenberg, F., & Beck, J. (1993). Markov models in medical decision making: A practical guide. Medical Decision Making, 4, 322–338.
Williams, R. L. (2000). A note on robust variance estimation for cluster-correlated data. Biometrics, 56(2), 645–646.
Nolan, C. M., Longworth, L., Lord, J., Canavan, J. L., Jones, S. E., Kon, S. S., et al. (2016). The EQ-5D-5L health status questionnaire in COPD: Validity, responsiveness and minimum important difference. Thorax, 71(6), 493–500.
Department of Statistics Singapore. Singapore Census of Population 2010. Retrieved 02, June, 2017, from http://www.singstat.gov.sg/publications/publications-and-papers/population#census_of_population.
Mann, R., Brazier, J., & Tsuchiya, A. (2009). A comparison of patient and general population weightings of EQ-5D dimensions. Health Economics, 18(3), 363–372.
Rupel, V. P., & Marko, M. O. (2016). Should patients estimate health related quality of life? The results of empirical study. Value in Health, 19, A480.
Papageorgiou, K., Vermeulen, K., Schroevers, M., Stiggelbout, A., Buskens, E., Krabbe, P., et al. (2015). Do individuals with and without depression value depression differently? And if so, why? Quality of Life Research, 24(11), 2565–2575.
Sayah, F., Bansback, N., Bryan, S., Ohinmaa, A., Poissant, L., Pullenayegum, E., et al. (2016). Determinants of time trade-off valuations for EQ-5D-5L health states: Data from the Canadian EQ-5D-5L valuation study. Quality of Life Research, 25(7), 1679–1685.
Shaw, J., Johnson, J., Chen, S., Levin, J., & Coons, S. (2007). Racial/ethnic differences in preferences for the EQ-5D health states: Results from the U.S. valuation study. Journal of Clinical Epidemiology, 60(6), 479–490.
Acknowledgements
We acknowledge the assistance of Grace Yang and Qu Limin (Debra) in collecting cancer patients’ data. We thank Yeoh Yen Shing for the assistance in data management. The authors appreciate the support of Duke-NUS/SingHealth Academic Research Institute and the medical editing assistance of Serene Ong (Medical writer, Duke-NUS Medical School). The Clinical Trials Research Office, National Heart Centre Singapore has provided administrative support.
Funding
The study was supported in part by the EuroQol Research Foundation (EQ Project 2015220), The Netherlands, and in part by the Duke-NUS Signature Research Program (WBS R-913-200-040) funded by the Agency for Science, Technology and Research (A*STAR), Singapore, and the Ministry of Health, Singapore. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gandhi, M., Tan, R.S., Ng, R. et al. Comparison of health state values derived from patients and individuals from the general population. Qual Life Res 26, 3353–3363 (2017). https://doi.org/10.1007/s11136-017-1683-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-017-1683-5