Abstract
Background
Previous studies suggest that population subgroups have different perceptions of health, as well as different preferences for hypothetical health states.
Objective
To identify determinants of health states preferences elicited using time trade-off (TTO) for the 5-level EQ-5D questionnaire (EQ-5D-5L) in Canada.
Methods
Data were from the Canadian EQ-5D-5L Valuation Study, which took place in Edmonton, Hamilton, Montreal, and Vancouver. Each respondent valued 10 of 86 hypothetical health states during an in-person interview using a computer-based TTO exercise. The TTO scores were the dependent variable and explanatory variables including age, sex, marital status, education, employment, annual household income, ethnicity, country of birth, dwelling, study site, health literacy, number of chronic conditions, previous experience with illness, and self-rated health.
Results
Average [standard deviation (SD)] age of respondents (N = 1209) was 48 (17) years, and 45 % were male. In multivariable linear regression models with random effects, adjusted for severity of health states and inconsistencies in valuations, older age [unstandardized regression coefficient (β) = −0.077], male sex (β = 0.042), being married (β = 0.069), and urban dwelling (β = −0.055) were significantly associated with health states scores. Additionally, participants from Edmonton (β = −0.124) and Vancouver (β = −0.156), but not those from Hamilton, had significantly lower TTO scores than those from Montreal.
Conclusions
Socio-demographic characteristics were the main determinants of preferences for EQ-5D-5L health states in this study. Interestingly, preferences were significantly lower in western Canadian cities compared to eastern ones, bringing into question whether a single preference algorithm is suitable for use in all parts of Canada.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Health utilities represent the strength of individuals’ preferences for particular health states and reflect the belief about the desirability of a health condition, willingness to take risks to gain health benefits, and preference for time [1]. Utilities can be used as a direct outcome measure in clinical research and for calculating quality-adjusted life years (QALYs) in economic evaluations. Several approaches may be used to derive health utilities, including rating scales, standard gamble, and time trade-off (TTO) [2]. Indirect utility measures, such as the EQ-5D, are multiattribute descriptive classification systems that use weighted scoring algorithms based on general population preferences that allow the valuation of a given health state into a single index score, typically anchored at 0 for dead and 1 for full health [3, 4]. There has been an ongoing debate on whose preferences should be used for weighing these measures, particularly for the purposes of economic analyses and resource allocation decisions. This debate is partly due to the conflicting and inconclusive evidence as to whether valuations of hypothetical health states vary by socio-demographic and health-related factors [5–7].
Previous studies have reported that some factors such as age, sex, marital status, and ethnicity contribute to different valuations of hypothetical health states [8–10]. However, there is limited evidence to suggest that education, income, or geographic region influence preferences [10], while evidence on the impact of chronic disease and illness experience has been mixed [9, 11–13]. Although some studies reported small, yet significant, differences in preferences between patients and the general population [13, 14], others noted trivial [9, 11] or no effects [12]. These differences have been attributed to the notion that people who have experienced serious and persistent health conditions report good or excellent quality of life despite their experience, a phenomenon known as the disability paradox [15]. Other factors that might contribute to different health valuations between patients and non-patients include response shift in how people interpret quality of life scales, contrast effects whereby people who experience negative life events become less bothered by less severe negative events, and different vantage points with patients viewing their illness in terms of the benefits that would result from regaining health, while the public views the illness in terms of the costs associated with losing good health [7].
Although variations in health preferences by respondents’ characteristics have led to the question of whose preferences are most valid for use at different levels of decision making in health policy and research, little attention has been paid to understand determinants of preferences in the general population. This may be one of the reasons for discrepancies in the existing literature, which narrowly focused on some factors and overlooked others. For the present study, we intended to identify socio-demographic and health-related factors associated with TTO-based preferences for hypothetical health states in the Canadian EQ-5D-5L valuation study [16]. The increased interest in using the EQ-5D-5L in Canada in economic evaluations to support health policy making and resource allocation, and the publicly funded nature of the Canadian healthcare system make this exploration timely and essential.
Methods
Data source
Data were taken from the Canadian valuation study, which was conducted to develop a value set and scoring algorithm for the EQ-5D-5L based on Canadian population preferences. Detailed description of the study methods and results were reported elsewhere [16]. Briefly, we used quota sampling to select a sample representative of the Canadian general population in terms of age, sex, and education status. Participants were recruited primarily through random dialling of published landline telephone numbers within each of the recruitment areas and supplemented by publically posted recruitment flyers. English-speaking participants were recruited from the greater metropolitan areas of Edmonton (Alberta “AB”), Hamilton (Ontario “ON”), and Vancouver (British Columbia “BC”), while French-speaking participants were recruited in Montreal (Quebec “QC”). The study involved completing TTO exercises, discrete choice experiment (DCE) questions, and other background questionnaires through face-to-face individual interviews, which were administered by trained interviewers using the EuroQol Valuation Technology [17]. The Health Research Ethics Boards at the Universities of Alberta, McMaster, and British Columbia and the Ethics Board of the Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal approved the data collection protocols and survey instruments, and all participants provided written informed consent.
Dependent variable: EQ-5D-5L health state valuations
The EQ-5D-5L classification system consists of five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, each with five levels: no problems “1,” slight problems “2,” moderate problems “3,”, severe problems “4,” and extreme problems “5” [18]. Each health state is described as a vector of these five dimensions. With five levels for each dimension, the EQ-5D-5L describes 3125 distinct health states, with 11111 being the best health state (full health) and 55555 the worst health state.
For the Canadian valuation study, 86 hypothetical health states of varying severity levels, grouped into 10 blocks with 10 health states per block, were valued using a composite TTO (cTTO) approach. For each health state, cTTO starts with traditional TTO (tTTO), in which the value of a health state (i.e., TTO score) is determined by discerning how much time in full health a respondent is willing to give up in order to avoid undesirable health conditions [19]. If the respondent chooses to give up all years of full health to avoid living in the impaired health state, a 10-year lead-time TTO (LT-TTO) is presented, and the respondent is asked the same question [19, 20]. Each respondent valued 10 health states in one block, which included one of the very mild health states (11112; 11121; 11211; 12111; 21111) and the worst health state (55555). The dependent variable in this analysis was the respondents’ TTO scores (ranging between −1.0 and +1.0) for each of the 10 valued health states, which was used as a continuous variable in all analyses. Participants were considered to have inconsistencies in their TTO valuations if (1) they gave the same or a lower score for the very mild health state compared to 55555 or (2) they gave the same or a lower score for the very mild health state compared to the majority of the health states that are dominated by the very mild health state within the same block [16].
Explanatory variables
Apart from the TTO exercise, each respondent described their current health status by completing the EQ-5D-5L questionnaire and the EuroQol visual analogue scale (EQ-VAS). Socio-demographic data collected included age, sex, marital status [married (including common law); not married (including widowed, separated, divorced, single)], educational level (less than high school; completed high school or equivalent; higher than high school), employment status [employed (part-time or full-time); unemployed (including retired, on disability pension, homemaker, student)], annual household income (≤$75,000; >$75,000; prefer not to respond), ethnicity (White/Caucasian; Aboriginal; other), country of birth (Canada; outside Canada), study site (Edmonton, AB; Hamilton, ON; Montreal, QC; Vancouver, BC), dwelling (rural, urban), and self-reported height and weight. Body mass index (BMI) was calculated (BMI = weight/height2) for each respondent and adjusted for self-report bias using sex-specific adjustment equations (females −0.12 + 1.05*BMI; males −1.08 + 1.08*BMI) [21].
Other measures included health literacy, multimorbidity, and previous experience with illness. Health literacy—the degree to which individuals can obtain, process, understand, and communicate about health-related information needed to make informed health decisions [22]—was assessed using three previously validated screening questions: difficulty in understanding written information; confidence in completing medical forms; and needing help in reading medical information [23]. Each question was scored from 1 to 5 with higher scores indicating lower health literacy and a cut-off point of ≥9.0 for the summative score (range 3–15) indicating inadequate health literacy [23].
Multimorbidity was defined as the presence of ≥2 of 15 self-reported chronic conditions [24], which included asthma; chronic bronchitis, emphysema, or chronic obstructive pulmonary disease; arthritis; diabetes; heart disease; hypertension; stroke; cancer; intestinal or stomach ulcers; bowel disorders (e.g., Crohn’s disease, ulcerative colitis, irritable bowel syndrome, bowel incontinence); urinary incontinence; migraine headaches; Alzheimer’s disease or any other dementia; mood or anxiety disorders (e.g., depression, bipolar disorder, mania or dysthymia, phobia, obsessive–compulsive disorder or a panic disorder); and obesity (BMI ≥ 25 kg/m2).
Previous experience of illness was defined based on participants’ responses to three questions on experiencing serious illness in them, in caring for a family member or in caring for others. A positive response to one of these questions was indicative of having a previous illness experience.
Statistical analysis
Descriptive statistics were computed for all variables in the overall sample. The associations of each of the explanatory variables with the TTO scores were examined using univariate linear models, adjusted for severity of health states, with random effects to account for multiple valuations by the same respondent. Then, a multivariable random-effects linear regression model, adjusted for severity of health states, was fitted with the TTO score as the dependent variable and including all the explanatory variables. Adjusting for health states severity level was done by including five dimension-specific ordinal variables with five levels each [1–5] to describe the health state vector. Participants considered to have inconsistent valuations, based on the aforementioned criteria, were accounted for using a dummy variable in the overall model. All statistical analyses and data management were performed using STATA 13.0 package.
Results
General characteristics of participants
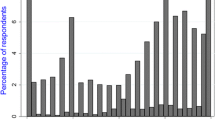
A total of 1209 respondents recruited from the four sites completed the TTO exercises and the socio-demographic and other questionnaires. The average [standard deviation (SD)] age of respondents was 48 (17) years, 45 % were male, 53 % married, 63 % had more than high school education, 50 % were employed, and 29 % had an annual household income >$75,000. The majority of participants (82 %) lived in urban settlements, and 75 % were born in Canada. Few participants (7 %) had inadequate health literacy, 31 % reported having 2 or more comorbid chronic conditions, and 83 % had a previous experience with illness. The mean EQ-VAS score in this sample was 82.3 (SD 14.2) (Table 1).
Almost 11 % (n = 136) of participants had inconsistent valuations; these participants were older, had lower education and less income, and were more likely to be Aboriginal than those without inconsistencies (data not shown). These participants were also much more likely to have inadequate health literacy, more comorbidities, and lower self-rated health than those without inconsistent valuations.
Determinants of TTO scores of health states
In univariate analyses (Table 2), we found that older adults (over 60 years old) had lower scores for all health states compared to young adults. Males, married respondents, those who were employed at the time of the study, respondents born in Canada, and urban dwellers had significantly higher scores for health states than their counterparts. Respondents of ethnic groups other than white or Aboriginals had lower scores for health states than white respondents. Respondents from the two western Canadian cities had lower scores than those from the two eastern cities. Educational level, income, health literacy, multimorbidity, previous experience with illness, and self-rated health were not significantly associated with health states values.
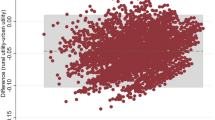
In multivariable linear regression model adjusted for inconsistencies and severity of health states, older age [unstandardized regression coefficient (β) = −0.077; p = 0.004], male sex (β = 0.042; p = 0.025), being married (β = 0.069; p = 0.001), and urban dwelling (β = −0.055; p = 0.035) were significantly associated with health states scores (Table 2). Respondents from Edmonton (β = −0.124; p < 0.001) and Vancouver (β = −0.156; p < 0.001), but not those from Hamilton (β = 0.02; p = 0.451), had significantly lower scores than those from Montreal. Educational level, employment status, annual household income, ethnic background, country of birth, health literacy level, multimorbidity or any of the individual chronic conditions separately (data not shown), previous experience of illness, and self-rated health (based on EQ-VAS) were not significantly associated with health state values.
Discussion
This study shows that socio-demographic characteristics, particularly age, sex, marital status, dwelling, and study site (eastern vs. western cities), were the main determinants of TTO scores of hypothetical health states in this study. Other factors including education, income, ethnicity, country of birth, health literacy, multimorbidity, previous experience of illness, and self-rated health had no statistically significant impact on these preferences.
The finding that health preferences vary by socio-demographic characteristics is in accordance with previous literature. For example, a recent large US study reported that women and older adults place a higher value on health states than men, but fewer differences by ethnicity and race were observed [8]. In another large US study, health states’ values were found to significantly vary by ethnicity and marital status, whereby African Americans and married individuals tended to value health states more highly than their counterparts; however, no differences by sex, education, income, or geographic region were noted [10]. To our knowledge, this was the first study to examine the impact of health literacy on valuations of health states. Despite the nonsignificant associations, it is imperative to note that participants who had inadequate health literacy were more likely to have inconsistent responses likely due to lack of understanding the task. This suggests that the true preferences of these participants were not properly elicited, and highlights the need of exploring the impact of health literacy on individuals’ understanding and completion of health preferences elicitation exercises, especially the cognitively challenging such as TTO.
The results of the impact of chronic conditions and previous illness experience on health preferences are consistent with a few studies, however, contradictory to others. For example, two large meta-analyses that summarized the evidence on differences in preferences between patients and the general public had contradictory conclusions [5, 6]. This controversy is also present in more recent literature. One study found that patients with cancer and rheumatoid arthritis tended to assign higher TTO values for hypothetical health states [13], while others reported that chronic conditions have trivial impact on health preferences [9, 11]. These differences among studies could be explained by the varying number and type of chronic diseases in the definition of multimorbidity, the number and severity of health states included, and preference elicitation methods used. Additionally, such differences might arise from the diversity of healthcare systems in countries where these studies were conducted, particularly with respect to the structure and quality of healthcare and its impact on individuals’ perceptions about health and ultimately preferences for certain health states [25].
The most interesting finding in this study was the variation in TTO scores for health states between the two eastern and two western Canadian cities. Although similar approaches of sampling and data collection were employed across all four sites, there were significant differences in all measured characteristics across participants from the four sites (supplemental on-line file 1). There might be other unmeasured factors that might explain these results. Also, one potential explanation could be interviewer effect, which is the distortion of participant response due to differential reactions to the style and personality of interviewers or to their presentation of particular questions. Given the nature of valuation studies’ interviews, which addresses issues of health, life, and death, and where an interviewer is expected to intervene if a respondent appears not to understand the task, interviewers style and personality might impact how participants complete the questions. However, we examined interviewer effect within two of the study sites (AB, BC) and found it insignificant (data not shown). The other sites (QC, ON) had only one interviewer each, and thus this exploration was not possible. Another potential explanation could be the actual variability in healthcare between Canadian provinces that, despite national healthcare legislations, hold the responsibility for planning and funding most publicly insured health services. Previous reports indicated that there is inequity in most healthcare services across Canadian provinces [26] and significant variations in the availability, access and use of resources, in clinical performance and in total healthcare expenditure [27]. Although provincial healthcare variations do exist, they may not fully explain the observed regional (east–west) differences, which need to be further explored given their important implications. Meanwhile, this finding brings into question whether a single utility algorithm is suitable for use in all parts of Canada, or whether region-specific (western, eastern) algorithms estimated from region-specific preferences need to be developed.
In the application of QALYs in economic evaluations and resource allocation purposes, Dolan suggested addressing three questions: “what is it to be valued; how is it to be valued; and who is to value it?” [28]. In this study, EQ-5D-5L and TTO approach are the answers to the first two questions, respectively, while the third question remains challenging. Although we answered the empirical side of it, there are political and even ideological facets that need to be considered. In Canada, the healthcare system is publicly funded, and these funds are provided at both provincial and federal levels. For that, and given the findings of this study, it might be suitable to have both an overall Canadian population-based preference set and a subgroup preference set based on region (e.g., eastern vs. western) or province, particularly for the application of QALYs in economic evaluations that support health policy making and resource allocation.
The results of this study should be interpreted in light of a few limitations. First, data on chronic conditions were based on self-report and did not include information about the severity or duration of these conditions. Therefore, these results may not be generalizable to more severely ill individuals. Second, we lacked data on other variables such as family status (e.g., having children), religious beliefs, and belief in afterlife that might have affected individuals’ preferences for health. Third, although we used a previously validated measure of health literacy, this measure captures functional, but not critical or communicative aspects of health literacy. Additionally, being able to read was a requirement to participate in this study, so by design, individuals who cannot read or who have reading challenges were not recruited into the study. These factors might have lead to the low prevalence rates of inadequate health literacy observed in this study. Last, the majority of participants were highly educated, lived in urban settings, and generally had adequate health literacy, and so, in these characteristics, they might not represent all Canadians, especially ethnic minorities, and this limits the generalizability of these findings to these populations.
Conclusion
Our study suggests that, at the group level, and irrespective of the severity of the health state, only socio-demographic characteristics have a significant impact on health preferences. It also suggests that utility algorithms for EQ-5D-5L estimated from preferences of the Canadian population would be similar to those estimated from patients with chronic illness or from those who have experienced serious illness. Importantly, health state valuations were significantly lower in western Canadian cities compared to eastern ones. These results bring into question whether an overall preference set is suitable for use in all parts of Canada or region-specific (western, eastern) sets estimated from region-specific preferences need to be developed.
References
Drummond, M. F., O’Brien, B. J., Stoddart, G. L., & Torrance, G. W. (1997). Methods for the economic evaluation of health care programmes (2nd ed.). Oxford: Oxford University Press.
Streiner, D. L., & Norman, G. R. (2003). Health Measurement Scales: A practical guide to their development and use. New York: Oxford University Press.
Feeny, D. (2000). A utility approach to the assessment of health-related quality of life. Medical Care, 38(9), 151–154.
Rabin, R., & de Charro, F. (2001). EQ-5D: A measure of health status from the EuroQol group. Annals of Medicine, 33(5), 337–343.
Dolders, M. G., Zeegers, M. P., Groot, W., & Ament, A. (2006). A meta-analysis demonstrates no significant differences between patient and population preferences. Journal of Clinical Epidemiology, 59(7), 653–664.
Peeters, Y., & Stiggelbout, A. M. (2010). Health state valuations of patients and the general public analytically compared: A meta-analytical comparison of patient and population health state utilities. Value Health, 13(2), 306–309.
Ubel, P. A., Loewenstein, G., & Jepson, C. (2003). Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Quality of Life Research, 12(6), 599–607.
Craig, B. M., Reeve, B. B., Cella, D., Hays, R. D., Pickard, A. S., & Revicki, D. A. (2014). Demographic differences in health preferences in the United States. Medical Care, 52(4), 307–313.
Pickard, A. S., Tawk, R., & Shaw, J. W. (2013). The effect of chronic conditions on stated preferences for health. The European Journal of Health Economics, 14(4), 697–702.
Shaw, J. W., Johnson, J. A., Chen, S., Levin, J. R., & Coons, S. J. (2007). Racial/ethnic differences in preferences for the EQ-5D health states: results from the U.S. valuation study. Journal of Clinical Epidemiology, 60(5), 479–490.
Gandhi, M., Thumboo, J., Luo, N., Wee, H. L., & Cheung, Y. B. (2015). Do chronic disease patients value generic health states differently from individuals with no chronic disease? A case of a multicultural Asian population. Health and Quality of Life Outcomes, 13(1), 1–9.
Kind, P., & Dolan, P. (1995). The effect of past and present illness experience on the valuations of health states. Medical Care, 33(Suppl. 4), AS255–AS263.
Krabbe, P. F., Tromp, N., Ruers, T. J., & van Riel, P. L. (2011). Are patients’ judgments of health status really different from the general population? Health and Quality of Life Outcomes, 11(9), 31.
Little, M. H., Reitmeir, P., Peters, A., & Leidl, R. (2014). The impact of differences between patient and general population EQ-5D-3L values on the mean tariff scores of different patient groups. Value in Health, 17(4), 364–371.
Albrecht, G. L., & Devlieger, P. J. (1999). The disability paradox: High quality of life against all odds. Social Science and Medicine, 48(8), 977–988.
Xie, F., Pullenayegum, E., Gaebel, K., Bansback, N., Bryan, B., Ohinmaa, A., et al. (2015). A time trade-off-derived value set of EQ-5D-5L for Canada. Medical Care.
Oppe, M., Devlin, N. J., van Hout, B., Krabbe, P. F. M., & de Charro, F. (2014). A programme of methodological research to arrive at the new international EQ-5D-5L valuation protocol. Value in Health, 17(4), 445–453.
Herdman, M., Gudex, C., Lloyd, A., Janssen, M., Kind, P., Parkin, D., et al. (2011). Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research, 20(10), 1727–1736.
Devlin, N. J., Tsuchiya, A., Buckingham, K., & Tilling, C. (2011). A uniform time trade off method for states better and worse than dead: Feasibility study of the ‘lead time’ approach. Health Economics, 20(3), 348–361.
Attema, A. E., Versteegh, M. M., Oppe, M., Brouwer, W. B., & Stolk, E. A. (2013). Lead time TTO: Leading to better health state valuations? Health Economics, 22(4), 376–392.
Gorber, S. C., Shields, M., Tremblay, M. S., & McDowell, I. (2008). The feasibility of establishing correction factors to adjust self-reported estimates of obesity. Health Reports, 19(3), 71–82.
Berkman, N., Terry, D., & McCormack, L. (2010). Health literacy: What is it? Journal of Health Communication, 15(Suppl 2), 9–19.
Chew, L. D., Griffin, J. M., Partin, M. R., Noorbaloochi, S., Grill, J. P., Snyder, A., et al. (2008). Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of General Internal Medicine, 23(5), 561–566.
Fortin, M., Bravo, G., Hudon, C., Vanasse, A., & Lapointe, L. (2005). Prevalence of multimorbidity among adults seen in family practice. The Annals of Family Medicine, 3(3), 223–228.
Soroka, S. N. (2007). Canadian perceptions of the health Care system: A report to the Health Council of Canada. Toronto, ON: Health Council of Canada.
Allin, S. (2008). Does equity in healthcare use vary across Canadian Provinces? Healthcare Policy, 3(4), 83–99.
Barua, B. (2013). Provincial Healthcare Index 2013. Vancouver: Fraser Institute.
Dolan, P. (2011). Thinking about it: Thoughts about health and valuing QALYs. Health Economics, 20(12), 1407–1416.
Acknowledgments
This project was supported by an operating Grant from the Canadian Institutes for Health Research (#MOP 111076) and funding support from the EuroQol Research Foundation. Feng Xie and Eleanor Pullenayegum are supported by Canadian Institutes of Health Research New Investigator Awards (2012–2017). Jeffrey Johnson is a Senior Health Scholar with Alberta Innovates Health Solutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to declare.
Ethical approval
The Health Research Ethics Boards at the Universities of Alberta, McMaster, and British Columbia and the Ethics Board of the Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal approved the data collection protocols and survey instruments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sayah, F.A., Bansback, N., Bryan, S. et al. Determinants of time trade-off valuations for EQ-5D-5L health states: data from the Canadian EQ-5D-5L valuation study. Qual Life Res 25, 1679–1685 (2016). https://doi.org/10.1007/s11136-015-1203-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-1203-4