Abstract
Purpose
The assessment of the quality of life (QoL) in minilaparotomy cholecystectomy (MC) versus laparoscopic cholecystectomy (LC) with the ultrasonic dissection in both groups has not been addressed earlier.
Methods
Initially, 109 patients with non-complicated symptomatic gallstone disease were randomized to undergo either MC (n = 59) or LC (n = 50). RAND-36 survey was conducted preoperatively and at 4 weeks and 6 months postoperatively. The end point of our study was to determine differences in health status in MC versus LC groups.
Results
QoL improved significantly in both groups, and the recovery was similar in the two groups, except from the higher score in ‘health change’ subscale at 4 weeks in MC group [MC score 75.0 (25.0) vs. LC score 56.5 (23.2), p = 0.008]. The MC and LC groups combined, RAND-36 scores increased significantly in ‘physical functioning’ [combined mean (SD) preoperative score 80.5 (23.9) vs. 6-month postoperative score 86.5 (21.7), p = 0.015], ‘vitality’ [64.5 (19.2) vs. 73.5 (18.3), p = 0.001], ‘health change’ [43.0 (21.6) vs. 74.6 (25.4), p = 0.0001] and ‘bodily pain’ scores [57.7 (26.3) vs. 75.5 (25.5), p = 0.001], respectively. Four RAND-36 domains indicated statistically significant health status differences in comparing the preoperative and postoperative RAND-36 scores in LC and MC groups combined.
Conclusions
Four RAND-36 domains indicated a significant positive change in QoL after cholecystectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic cholecystectomy (LC) is the gold standard for the treatment of symptomatic gallstone disease, although cholecystectomy by minilaparotomy (MC) has shown to have a similar early recovery after surgery [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25]. The classical outcomes for the evaluation of the surgical procedures in the gallstone disease are usually perioperative complications, morbidity, mortality and long-term outcome post-cholecystectomy. However, from the patient’s point of view, the postoperative sick leave duration, patient satisfaction, symptom resolution and quality of life (QoL) are essential. Many QoL scoring tools have been used on patients with cholelithiasis to measure the post-cholecystectomy health status and outcome [2, 3, 7, 17, 26,27,28,29,30]. The disease-specific gastrointestinal QoL index (GIQLI) scoring and the Short Form Health Survey Questionnaire (SF-36) are widely used and easily administered health surveys designed for measuring self-reported physical and mental health status [2, 3, 7, 17, 26,27,28,29,30]. The SF-36 contains a total of eight domains (physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health) and an assessment of perceived health change. In this study, we used the RAND-36 Health Survey Questionnaire [31, 32], which includes the same set of items than SF-36; however, the scoring of the general health and the pain scales is different. To our knowledge, there is no prospective randomized trial available on SF-36 comparing LC and MC techniques.
Most trials on QoL in patients with symptomatic cholelithiasis have involved mainly open cholecystectomy or LC patient cohorts [26,27,28]. Four prospective randomized trials comparing post-cholecystectomy QoL after MC versus LC groups have been previously conducted [2, 3, 7, 17]; however, assessment of QoL in MC versus LC with ultrasonic dissection in both groups has not been addressed. Earlier, we compared LC and MC with ultrasonic dissection (UsD) in both groups and the results indicated a fairly similar perioperative outcome; however, the LC with UsD reported lower pain scores 24 h postoperatively [24, 25]. Therefore, we conducted the present study investigating the health status of MC versus LC patients with RAND-36 questionnaire in prospective randomized study. The study hypothesis was that the post-cholecystectomy health status with RAND-36 in MC versus LC patients is similar.
Materials and methods
The study was approved by the Ethics Committee of Helsinki and Uusimaa University District, Helsinki, Finland (DNRO 120/13/02/02/2010, May 12, 2010), it was registered in the ClinicalTrials.gov database (ClinicalTrials.gov Identifier: NCT01723540, Consort diagram, Fig. 1), and it was conducted in accordance with the Declaration of Helsinki. Participants gave written consent after receiving verbal and written information. Operations were carried out in two hospitals in Finland: Helsinki University Central Hospital, Helsinki (n = 28) and Kuopio University Hospital, Kuopio (n = 81) between March 2013 and May 2015. The flowchart of the study is presented in Fig. 1.
The study design was a prospective, randomized, multicentre clinical trial with two parallel groups. Altogether 109 patients with uncomplicated symptomatic cholelithiasis confirmed by ultrasound were randomized to undergo cholecystectomy with LC, 50 patients, or with MC, 59 patients. The computer-generated randomization was concealed with the sealed envelope method until the patient enrollment, and after randomization, the study was open [18]. The operations were carried out by three consultant-level surgeons (JH, PJ and ME) with extensive experience with both techniques. Only elective patients suitable for day-case surgery with symptomatic gallstones confirmed by ultrasound were included in the study.
The surgical techniques used were standardized in both groups. The LC is a laparoscopic operation and was performed using the four-trocar technique (two 10-mm and two 5-mm trocars), which needs four small wounds at abdominal wall [total mean (SD) length of skin incisions, 7.8 (2.5) cm]. An optical trocar was used to penetrate into the abdominal cavity, and intra-abdominal pressure was set at 12 mmHg. Ultrasonic scissors (UsD, Harmonic ACE®, Ethicon Endo-Surgery, Cincinnati, OH, USA) were used both in the MC and in LC procedure. The gallbladder was dissected from the liver with UsD scissor, and the cystic artery was sealed with UsD. Two metal clips were inserted to the cystic duct.
The MC technique is open mini-invasive technique with very short wound [mean (SD) length of skin incision, 4.8 (1.0) cm], and the rectus muscle was split, not cut in the MC technique. Cutting the rectus muscle or a skin incision longer than 7 cm was considered as a conversion to a conventional open operation in the MC group [13,14,15,16,17,18]. At the end of the operation, the wounds were infiltrated with local anesthetic (20 ml ropivacaine 7.5 mg/ml) in both groups.
Health-related QoL was assessed pre- and postoperatively using the validated Finnish version of the RAND-36 questionnaire [32]. The preoperative RAND-36 surveys were to be filled and returned by the morning of the surgery. Postoperative RAND-36 questionnaires at 4 weeks and 6 months after the surgery were to be returned by mail with the prepaid envelope. The non-responders were interviewed by phone. The eight health domains were calculated from the 36 questions as instructed by the RAND-36-item health survey [31, 32]. RAND-36 is a generic measure of perceived health status that incorporates behavioral functioning, subjective well-being and perceptions of health by assessing eight health concepts: limitations in physical activities due to health problems, limitations in role activities due to physical health problems, pain, limitations in social activities due to health problems, general mental health, limitations in usual role activities due to emotional problems, vitality (energy and fatigue) and general health perceptions. The questionnaire takes 10–15 min to complete and is easily reproducible. The Finnish version of RAND-36 has been translated, culturally adapted and validated [31].
The study sample size calculation was based on the assumption that the convalescence should be 16 days (SD 4) in the LC group [23]. In order to show a 3-day difference in the convalescence between the two groups, 40 patients per group were required at a study power of 0.9 and two-sided α-level of 0.05 to show a statistically significant difference between the groups.
The data were entered and analyzed with a statistical software program (IBM SPSS Statistics 21.0, IBM, Somers, IL, USA). The results are presented as mean and standard deviation, median and range or as the number of patients when appropriate. For continuous and ordinal data in time-specific groupwise comparisons, the Mann–Whitney U test was used in case of non-normally distributed data, and the independent samples t test in case of normally distributed data. Repeated-measures analysis of variance (ANOVA) was used to evaluate health status differences over time between the two study groups. A two-sided p value of less than 0.05 was considered statistically significant.
Results
Ninety-nine patients of the 109 (91.7%) patients randomized adequately filled the survey preoperatively. In total, 52.5% (52/99) of these patients underwent MC and 47.5% (47/99) LC. Of the 99 patients, 88/99 (88.9%) and 83/99 (83.8%) further returned the survey at 4 weeks and 6 months postoperatively, respectively. The Consort figure of the study is presented in Fig. 1. The study groups did not differ in terms of demographic variables, surgical data, conversions or complications. The demographic characteristics and surgical data are presented in Table 1 with p values.
There were no significant differences in preoperative RAND-36 subscales between the study groups in physical or social functioning, vitality, mental health, role physical, role emotional, bodily pain or general health scores. Postoperatively, the only significant difference between the MC and the LC groups was the higher score in the health change subscale in the MC group at 4 weeks [MC score 75.0 (25.0) vs. LC score 56.5 (23.2), p = 0.008]. Moreover, no significant differences were observed in any of the eight domains of RAND-36 at 6 months after surgery.
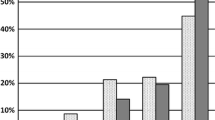
In the analysis of the MC and the LC groups combined, the RAND-36 scores increased significantly in ‘physical functioning’ [combined mean (SD) preoperative score 80.5 (23.9) vs. combined mean (SD) 6-month postoperative score 86.5 (21.7), p = 0.015], ‘vitality’ [64.5 (19.2) vs. 73.5 (18.3), p = 0.001], ‘health change’ [43.0 (21.6) vs. 74.6 (25.4), p = 0.0001] and ‘bodily pain’ scores [57.7 (26.3) vs. 75.5 (25.5), p = 0.001], respectively. Moreover, in the analysis of the MC and the LC groups combined, the ‘health change’ domain increased significantly in the preoperative score versus 4-week postoperative score [43.0 (21.6) vs. 66.0 (25.7), p = 0.0001] and respectively versus 6-month postoperative score [43.0 (21.6) vs. 74.6 (25.4), p = 0.0001]. In the analysis of the MC and the LC groups combined, the only RAND-36 score to significantly decrease was the ‘role physical’ in the preoperative score versus 4-week post-surgery score [67.9 (36.6) vs. 48.0 (39.7), p = 0.01]. However, the ‘role physical’ domain in the preoperative score versus 6-month score increased significantly in both groups (Tables 2, 3). The RAND-36 scores between the MC and the LC with UsD in both groups are presented in Table 2. In the analysis of the MC and the LC groups combined, the RAND-36 scores are presented in Table 3. Figure 2 shows the mean (SD) 6-month postoperative scores of the eight RAND-36 domains between the MC and LC groups compared to age- and gender-adjusted Finnish reference scores.
In a subgroup analysis, no significant differences were shown between the obese and non-obese patients (body mass index <30 vs. >30 kg/m2) or patients with chronic cholecystitis versus no chronic cholecystitis in the time-specific analysis (preoperative vs. 4 weeks vs. 6 months) regarding all eight domains of RAND-36.
Discussion
The duration of sick leave, patient satisfaction, symptom resolution and QoL are essential from the patient’s point of view, and these assessments are increasingly being recognized as an integral factor in surgical decision making. The most often used QoL tools for gallstone disease patients are the GIQLI and SF-36 [2, 3, 7, 17, 26,27,28]. An effective way to investigate the factors that may influence subjective QoL outcomes is to measure the satisfaction rate pre- and post-surgery and repeatedly after surgical treatment.
To our knowledge, there are only four prospective randomized trials on QoL comparing the post-cholecystectomy outcome after MC versus LC patients [2, 5, 7, 17]. Barkun et al. [2] used the Nottingham Health Profile Questionnaire (NHPQ), GIQLI and Visual Analogue Scale (VAS) scores in 70 patients with cholelithiasis randomized to LC (n = 38) and MC (n = 32) groups. The 37/38 (97%) patients in the LC group and 25/32 (78%) in the MC group underwent the allocated procedure and contributed data to the final analysis. There was a significant postoperative improvement in all of the three QoL questionnaires in both groups; however, the LC patients recovered more quickly than did the MC patients. In a study by McMahon et al. [3], SF-36 and the Hospital Anxiety and Depression Scale (HADS) were used, showing higher health status scores after LC at 1 and 4 weeks post-surgically, whereas the scores did not differ at 12 weeks after the surgery. Squirrell et al. [7] randomized a total of 195 patients in the LC (n = 100) versus MC (n = 95) groups, and the NHP questionnaires were completed by a subgroup of 94 of 195 patients (LC = 47 and MC = 47) detecting no statistical significant differences in QoL between the two groups. Keus et al. [17] randomized a total of 257 patients in the LC versus MC groups including the converted procedures. The QoL was analyzed preoperatively and at 1 day, 2 weeks, 6 weeks and 3 months post-cholecystectomy using GIQLI and SF-36 questionnaires, concluding that no significant health status differences between LC and MC patients were observed with the exception of the SF-36 perceived health change subscale at 2 and 6 weeks after surgery in favor of LC group. However, the perceived health change was not reflected in an earlier return to work in the LC group.
The present study population was comparable to the age- and gender-adjusted Finnish reference population [30] in terms of physical and social functioning, vitality, mental health, role emotional and general health scores in the RAND-36 scores preoperatively. In addition, there were no statistically significant differences in the number of analgesic doses during the first 24 h between the LC and MC groups (p = 0.42, Table 1).
However, the role physical and the bodily pain scores were lower compared to the reference population and the role physical score further decreased by 4 weeks, indicating the impediment of gallstone disease and post-surgical recovery. Both study groups did significantly improve in bodily pain and role physical scores and finally correlated or outscored the general population in all eight domains of RAND-36 by 6 months. In contrary to the study by Keus et al. [17], in our study, the MC patients had higher scores in the health change subscale both 4 weeks and 6 months after surgery, with a statistically significant difference at 4 weeks (p = 0.008). In the RAND-36 questionnaire, the higher score is better for the health status of the patients; thus, we have no explanation for the MC patients’ prolonged postoperative sick leave due to the lacking correlation between the duration of sick leave days and the health status and the perceived health change post-surgery. In fact, the MC procedure seems to slightly outscore the LC procedure in the bodily pain and the general health subscales at 6 months post-surgery. Moreover, the MC and LC groups combined, the scores increased in four RAND-36 domains: vitality, physical functioning, health change and bodily pain, indicating a significant positive change in QoL postoperatively. Wright et al. [30] found recently that depressed LC patients do worse in recovery and this could be one explanation for patients that have prolonged sick leave when operative successes appear to be good. However, this has not been explored in this study, but could be hypotheses for future research.
In conclusion, four RAND-36 domains indicated statistically significant health status differences in comparing the preoperative and postoperative RAND-36 scores in LC and MC groups combined.
References
Ledet, W. P., Jr. (1990). Ambulatory cholecystectomy without disability. Archives of Surgery, 125, 1434–1435.
Barkun, J. S., Barkun, A. N., Sampalis, J. S., et al. (1992). Randomised controlled trial of laparoscopic versus mini cholecystectomy. The McGill Gallstone Treatment Group. Lancet, 340, 1116–1119.
McMahon, A. J., Russell, I. T., Baxter, J. N., et al. (1994). Laparoscopic versus minilaparotomy cholecystectomy: A randomised trial. Lancet, 343, 135–138.
Tyagi, N. S., Meredith, M. C., Lumb, J. C., et al. (1994). A new minimal invasive technique for cholecystectomy: Subxiphoid “minimal stress triangle” microceliotomy. Annals of Surgery, 220, 617–625.
McGinn, F. P., Miles, A. J., Uqlow, M., et al. (1995). Randomized trial of laparoscopic cholecystectomy and mini-cholecystectomy. British Journal of Surgery, 82, 1374–1377.
Majeed, A. W., Troy, G., Nicholl, J. P., et al. (1996). Randomized, prospective, single-blind comparison of laparoscopic versus small-incision cholecystectomy. Lancet, 347, 989–994.
Squirrell, D. M., Majeed, A. W., Troy, G., et al. (1998). A randomized, prospective, blinded comparison of postoperative pain, metabolic response, and perceived health after laparoscopic and small incision cholecystectomy. Surgery, 123, 485–495.
Seale, A. K., & Ledet, W. P., Jr. (1999). Minicholecystectomy: A safe, cost-effective day surgery procedure. Archives of Surgery, 134, 308–310.
Ros, A., Gustafsson, L., Krook, H., et al. (2001). Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: A prospective, randomized, single-blind study. Annals of Surgery, 234, 741–749.
Srivastava, A., Srinivas, G., Misra, M. C., et al. (2001). Cost-effectiveness analysis of laparoscopic versus minilaparotomy cholecystectomy for gallstone disease. A randomized trial. International Journal of Technology Assessment in Health Care, 17, 497–502.
Thomas, S., Singh, J., Bishnoi, P. K., et al. (2001). Feasibility of day-care open cholecystectomy: Evaluation in an inpatient model. ANZ J Surg, 71, 93–97.
Amjad, N., & Fazal, A. (2002). Mini cholecystectomy now a day stay surgery: Anaesthetic management with multi modal analgesia. J Pak Med Assoc, 52, 291–296.
Harju, J., Juvonen, P., Eskelinen, M., et al. (2006). Minilaparotomy cholecystectomy versus laparoscopic cholecystectomy: A randomized study with special reference to obesity. Surgical Endoscopy, 20, 583–586.
Vagenas, K., Spyrakopoulos, P., Karanikolas, M., et al. (2006). Mini-laparotomy cholecystectomy versus laparoscopic cholecystectomy: Which way to go? Surg Laparosc Endosc Percutan Tech, 16, 321–324.
Harju, J., Pääkkönen, M., & Eskelinen, M. (2007). Minilaparotomy cholecystectomy as a day surgery procedure: A prospective clinical pilot study. Scand J Surg, 96, 206–208.
Harju, J., Pääkkönen, M., & Eskelinen, M. (2007). Comparison of the quality of life after minilaparotomy cholecystectomy versus laparoscopic cholecystectomy: A prospective randomized study. Isr Med Assoc J, 9, 147–148.
Keus, F., de Vries, J., Gooszen, H. G., et al. (2008). Laparoscopic versus small-incision cholecystectomy: Health status in a blind randomised trial. Surgical Endoscopy, 22, 1649–1659.
Harju, J., Kokki, H., Pääkkönen, M., et al. (2010). Feasibility of minilaparotomy versus laparoscopic cholecystectomy for day surgery: A prospective randomized study. Scand J Surg, 99, 132–136.
Rosenmuller, M. H., Thoren Örnberg, M., Myrnäs, T., et al. (2013). Expertise-based randomized clinical trial of laparoscopic versus small-incision open cholecystectomy. British Journal of Surgery, 100, 886–894.
Harju, J., Juvonen, P., Kokki, H., et al. (2013). Minilaparotomy cholecystectomy with ultrasonic dissection versus laparoscopic cholecystectomy with electrosurgical energy: A randomized multicenter study. Scandinavian Journal of Gastroenterology, 48, 1317–1323.
Harju, J., Aspinen, S., Juvonen, P., et al. (2013). Ten-year outcome after minilaparotomy versus laparoscopic cholecystectomy: A prospective randomized trial. Surgical Endoscopy, 27, 2512–2516.
Aspinen, S., Harju, J., Juvonen, P., et al. (2014). A prospective, randomized study comparing minilaparotomy and laparoscopic cholecystectomy as a day-surgery procedure: 5-year outcome. Surgical Endoscopy, 28, 827–832.
Aspinen, S., Harju, J., Juvonen, P., et al. (2014). A prospective, randomized multicenter study comparing conventional laparoscopic cholecystectomy versus minilaparotomy cholecystectomy with ultrasonic dissection as day surgery procedure—1-year outcome. Scandinavian Journal of Gastroenterology, 49, 1336–1342.
Aspinen, S., Harju, J., Kinnunen, M., et al. (2016). A randomized multicenter study of minilaparotomy cholecystectomy versus laparoscopic cholecystectomy with ultrasonic dissection in both groups. Scandinavian Journal of Gastroenterology, 51, 354–359.
Aspinen, S., Kinnunen, M., Harju, J., et al. (2016). Inflammatory response to surgical trauma in patients with minilaparotomy cholecystectomy versus laparoscopic cholecystectomy: A randomised multicentre study. Scandinavian Journal of Gastroenterology, 51, 739–744.
Korolija, D., Sauerland, S., Wood-Dauphinée, S., et al. (2004). Evaluation of quality of life after laparoscopic surgery: Evidence-based guidelines of the European Association for Endoscopic Surgery. Surgical Endoscopy, 18, 879–897.
Purkayastha, S., Tilney, H. S., Georgiou, P., et al. (2007). Laparoscopic cholecystectomy versus mini-laparotomy cholecystectomy: A meta-analysis of randomised control trials. Surgical Endoscopy, 21, 1294–1300.
Keus, F., Gooszen, H. G., & van Laarhoven, C. J. (2009). Systematic review: Open, small-incision or laparoscopic cholecystectomy for symptomatic cholecystolithiasis. Alimentary Pharmacology & Therapeutics, 29, 359–378.
Califano, A. D., Angelini, P., et al. (2011). Laparo-endoscopic single site cholecystectomy versus standard laparoscopic cholecystectomy: Results of a pilot randomized trial. American Journal of Surgery, 202, 45–52.
Wright, B., Alexander, D., Aghahoseini, A., et al. (2016). Does preoperative depression and/or serotonin transporter gene polymorphism predict outcome after laparoscopic cholecystectomy? BMJ open, 6, e007969.
Hays, R. D., & Morales, L. S. (2001). The RAND-36 measure of health-related quality of life. Annals of Medicine, 33, 350–357.
Aalto, A.-M., Aro, A. R., & Teperi, J. (1999). Rand-36 as a measure of health-related quality of life. Reliability, construct validity and reference values in the Finnish general population. Helsinki: National Research and Development Center for Welfare and Health. (Research #101 In Finnish, summary in English).
Acknowledgements
The study was funded by the Heikki, Aino and Aarne Korhonen foundation and the EVO funding of the Helsinki University Hospital and Kuopio University Hospital. The authors would like to thank the patients for their participation in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The study was approved by the Ethics Committee of Helsinki and Uusimaa University District, Helsinki, Finland (DNRO 120/13/02/02/2010, May 12, 2010), and it was registered in the ClinicalTrials.gov database (ClinicalTrials.gov Identifier: NCT01723540, Consort diagram, Fig. 1).
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Aspinen, S., Kärkkäinen, J., Harju, J. et al. Improvement in the quality of life following cholecystectomy: a randomized multicenter study of health status (RAND-36) in patients with laparoscopic cholecystectomy versus minilaparotomy cholecystectomy. Qual Life Res 26, 665–671 (2017). https://doi.org/10.1007/s11136-016-1485-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1485-1