Abstract
Objectives
To investigate the patient-reported multidimensional gastrointestinal symptoms predictors of generic health-related quality of life (HRQOL) in pediatric patients with functional gastrointestinal disorders (FGIDs).
Methods
The Pediatric Quality of Life Inventory™ (PedsQL™) Gastrointestinal Symptoms Scales and PedsQL™ 4.0 Generic Core Scales were completed in a 9-site study by 259 pediatric patients with functional constipation, functional abdominal pain (FAP), or irritable bowel syndrome (IBS). Gastrointestinal Symptoms Scales measuring stomach pain, stomach discomfort when eating, food and drink limits, trouble swallowing, heartburn and reflux, nausea and vomiting, gas and bloating, constipation, blood in poop, and diarrhea were identified as clinically important symptom differentiators from healthy controls based on prior findings, and subsequently tested for bivariate and multivariate linear associations with overall HRQOL.
Results
Gastrointestinal symptoms were differentially associated with decreased HRQOL in bivariate analyses for the three FGIDs. In predictive models utilizing hierarchical multiple regression analyses controlling for age, gender, and race/ethnicity, gastrointestinal symptoms differentially accounted for an additional 47, 40, and 60 % of the variance in patient-reported HRQOL for functional constipation, FAP, and IBS, respectively, reflecting large effect sizes. Significant individual gastrointestinal symptoms predictors were identified after controlling for the other gastrointestinal symptoms in the FGID-specific predictive models.
Conclusions
Gastrointestinal symptoms represent potentially modifiable predictors of generic HRQOL in pediatric patients with FGIDs. Identifying the condition-specific gastrointestinal symptoms that are the most important predictors from the patient perspective facilitates a patient-centered approach to targeted interventions designed to ameliorate impaired overall HRQOL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional constipation, functional abdominal pain (FAP), and irritable bowel syndrome (IBS) are three of the most common pediatric functional gastrointestinal disorders (FGIDs) internationally [1]. IBS and FAP are abdominal pain predominant FGIDs that adversely affect generic (general or non-disease-specific) health-related quality of life (HRQOL) [2–4]. While patients with IBS or FAP both manifest recurring abdominal pain [5–8], there are also IBS subtypes, with the IBS constipation subtype the most frequent (58.1 %), followed by unsubtyped IBS (34 %), IBS diarrhea subtype (5 %), and the IBS mixed subtype (2 %, includes both constipation and diarrhea) [9]. Pediatric patients with functional constipation generally report infrequent bowel movements, intermittent abdominal pain, feeling bloated, straining throughout bowel movements, and incidences of fecal incontinence as a consequence of rectal fecal impaction, with no identifiable organic etiology [10]. Pediatric functional constipation also adversely affects generic HRQOL [2, 11, 12].
Findings utilizing the Pediatric Quality of Life Inventory™ (PedsQL™) Gastrointestinal Symptoms Scales, a multidimensional gastrointestinal symptom-specific patient-reported outcome (PRO) measurement instrument, suggest a broad gastrointestinal symptoms profile for pediatric patients with functional constipation, FAP, or IBS compared to healthy controls [13, 14]. The identification of specific patient-reported gastrointestinal symptoms predictors of generic HRQOL in pediatric patients with different FGIDs derived from a standardized multidimensional gastrointestinal symptoms profile may facilitate targeted interventions designed to ameliorate impaired overall HRQOL. Nevertheless, to our knowledge, there has been no prior research utilizing pediatric patient self-reported multidimensional gastrointestinal symptoms to identify the most salient predictors of generic HRQOL in pediatric patients with functional constipation, FAP, or IBS.
Consequently, in order to address this significant gap in the pediatric literature, the primary objective of the present study was to investigate the predictive impact of a broad multidimensional gastrointestinal symptoms profile on generic HRQOL from the perspective of pediatric patients with functional constipation, FAP, or IBS. We examined each FGID individually to increase the clinical precision of our multivariate predictive models. Based on the conceptualization of disease-specific symptoms as causal indicators of generic HRQOL [15], and our previous findings which identified significant differences across a broad multidimensional gastrointestinal symptoms profile when comparing pediatric patients with functional constipation, FAP, or IBS to matched healthy controls [13, 14], we expected that individual scales measuring patient-reported gastrointestinal symptoms would be significantly associated with generic HRQOL at the bivariate level of analysis. We further hypothesized that multidimensional gastrointestinal symptoms as a group would explain a significant amount of the variance in generic HRQOL. Given the lack of definitive prior research on the impact of multidimensional gastrointestinal symptoms on generic HRQOL utilizing multivariate statistical methods, a priori hypotheses were not generated regarding the relative significance of the individual gastrointestinal symptoms in the multivariate predictive models tested.
Methods
Pediatric patients and settings
Pediatric patients with physician-diagnosed functional constipation, FAP, or IBS were recruited from nine pediatric tertiary care gastroenterology clinical sites across the USA for the PedsQL™ Gastrointestinal Symptoms Module field test study (See “Appendix”) [16]. Participants were identified through medical chart review with ICD-9-CM diagnostic codes 564.1 (irritable bowel syndrome), 789.0 (functional abdominal pain, NOS), or 564.0 (chronic constipation) and met pediatric Rome III criteria for IBS, FAP, or functional constipation [1]. Data collection for the PedsQL™ Gastrointestinal Symptoms Module field test study took place between March 2011 and November 2013 [16]. The present study reports unique statistical analyses of the data from the existing field test study database [2, 13, 14, 16–19]. Specifically, we have not previously reported on multivariate models predicting generic HRQOL utilizing the Gastrointestinal Symptoms Scales in pediatric patients with IBS, FAP, or functional constipation. Written parental informed consent and child assent (when age appropriate) were obtained during the field test study [16]. The research protocol for the field test study was approved by the Institutional Review Board at each participating institution.
Measures
PedsQL™ Gastrointestinal Symptoms Scales
The PedsQL™ Gastrointestinal Symptoms Scales from the PedsQL™ Gastrointestinal Symptoms Module encompass 10 individual scales: (1) Stomach Pain and Hurt Scale (6 items), (2) Stomach Discomfort When Eating Scale (5 items), (3) Food and Drink Limits Scale (6 items), (4) Trouble Swallowing Scale (3 items), (5) Heartburn and Reflux Scale (4 items), (6) Nausea and Vomiting Scale (4 items), (7) Gas and Bloating Scale (7 items), (8) Constipation Scale (14 items), (9) Blood in Poop Scale (2 items), and (10) Diarrhea Scale (7 items). The PedsQL™ Gastrointestinal Symptoms Module items and scales were developed through a literature review of the relevant research, national consultation with pediatric gastroenterologists, as well as focus interviews, cognitive interviews, and pretesting protocols with pediatric patients and their parents [20]. The format, instructions, Likert response scale, and scoring method for the PedsQL™ Gastrointestinal Symptoms Scales are identical to the PedsQL™ 4.0 Generic Core Scales [21], with higher scores indicating better HRQOL and hence lower symptoms [16]. The Scales are comprised of parallel child self-report and parent proxy-report formats for children ages 5–18 years, and a parent proxy-report format for children ages 2–4 years. Child self-report forms are specific for ages 5–7, 8–12, and 13–18 years. For the purposes of the present study, only patient self-report scales are included given the focus on patient-reported outcomes. The instructions ask how much of a problem each item has been during the past 1 month. A 5-point response scale is utilized across child and adolescent self-report for ages 8–18 (0 = never a problem; 1 = almost never a problem; 2 = sometimes a problem; 3 = often a problem; 4 = almost always a problem). To further increase the ease of use for young child self-report (ages 5–7), the response scale is reworded and simplified to a 3-point scale (0 = not at all a problem; 2 = sometimes a problem; 4 = a lot of a problem) and utilizes a faces scale adapted from the Pediatric Pain Questionnaire [22].
Items are reverse-scored and linearly transformed to a 0–100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0), so that lower scores demonstrate more (worse) gastrointestinal symptoms and hence lower (worse) gastrointestinal-specific HRQOL. Scale Scores are computed as the sum of the items divided by the number of items answered (this accounts for missing data). If more than 50 % of the items in the scale are missing, the Scale Score is not computed [23]. Although there are other strategies for imputing missing values, this computation is consistent with previous PedsQL peer-reviewed publications as well as other well-established HRQOL measures [24]. Cronbach’s alpha internal consistency reliability coefficients and known-groups validity for the PedsQL™ Gastrointestinal Symptoms Scales have been previously reported for these pediatric patients with FGIDs [13, 14], as well as young children ages 5–7 years from a broader group of patients with FGIDs and organic gastrointestinal diseases [16].
PedsQL™ 4.0 Generic Core Scales
The 23-item PedsQL™ 4.0 Generic Core Scales encompass: (1) Physical Functioning Scale (8 items), (2) Emotional Functioning Scale (5 items), (3) Social Functioning Scale (5 items), and (4) School Functioning Scale (5 items) [21]. To create the Total Scale Score, the mean is computed as the sum of the items divided by the number of items answered in the Physical, Emotional, Social, and School Functioning Scales. The Total Scale Score measures overall generic HRQOL [21]. Higher scores indicate better HRQOL. Cronbach’s alpha internal consistency reliability coefficients and known-groups validity for the PedsQL™ 4.0 Generic Core Scales have been previously reported for these pediatric patients with FGIDs [2], as well as young children ages 5–7 years from a large group of healthy and ill pediatric participants [25].
PedsQL Family Information Form
Parents completed the PedsQL™ Family Information Form which contains demographic information including the child’s age, gender, and race/ethnicity information [21].
Statistical analysis
PedsQL™ Gastrointestinal Symptoms Scales were selected as potential predictors of generic HRQOL based on previous findings comparing pediatric patients with IBS, FAP, or functional constipation to age, gender, and race/ethnicity matched healthy controls [13, 14]. Specifically, we selected the Gastrointestinal Symptoms Scales that demonstrated medium (0.50) to large (≥0.80) effect size differences between patients with IBS, FAP, or functional constipation versus matched healthy controls [13, 14]. We considered these clinically important differences based on prior evidence [26].
Pearson product–moment correlation analyses were conducted to test the bivariate associations between the hypothesized predictor variables (PedsQL™ Gastrointestinal Symptoms Scales) with generic HRQOL as measured by the PedsQL™ 4.0 Generic Core Scales Total Scale Score (dependent variable). Bivariate correlation effect sizes are designated as small (0.10), medium (0.30), and large (0.50) in magnitude [27]. Only independent variables significantly associate with the dependent variable at the bivariate level of analysis were included as predictor variables in subsequent multivariate analyses. Predictive analytics models utilizing multiple regression analyses were conducted to statistically predict the generic HRQOL criterion variable (Generic Core Scales Total Score) by the Gastrointestinal Symptoms Scales predictor variables after controlling for age, gender, and race/ethnicity demographic variables [28]. Multiple regression analysis is a conservative statistical approach that isolates the effects of a predictor variable on a criterion variable by controlling for the influence of covariates [28]. Hierarchical multiple regression analysis was the statistical procedure for testing the incremental variance accounted for by the set of Gastrointestinal Symptoms Scales predictors.
In the hierarchical multiple regression analyses predicting the generic HRQOL criterion variable, age (continuous variable), gender (coded male = 1, female = 2), and race/ethnicity (dichotomized and coded White non-Hispanic = 1, other race/ethnicity = 0 given the small number of patients identified in some of the race/ethnicity groups) were entered in Step 1 as demographic covariates (statistical control variables). The Gastrointestinal Symptoms Scales previously identified as demonstrating clinically important differences between pediatric patients with IBS, FAP, or functional constipation and matched healthy controls, and significantly associated with generic HRQOL at the bivariate level in the current analyses, were entered as a group in Step 2 in separate hierarchical multiple regression models for each FGID. This sequence of hierarchical steps was intended to control for the age, gender, and race/ethnicity background variables in Step 1 which might influence generic HRQOL, as well as to test the incremental variance accounted for (R 2 change) by the selected gastrointestinal symptoms as a group in Step 2 in predicting generic HRQOL in the statistical models tested. R 2 is the explained variability divided by the total variability around the criterion variable mean. R 2 change is the percentage of variability in the criterion variable (HRQOL mean) explained by the step. In this way, the covariance (shared variance) in the predictor variables and covariates were controlled, facilitating interpretation of incremental variance by the gastrointestinal symptoms predictor variables as a group. Multiple regression effect sizes (R 2) are designated as small (0.02), medium (0.13), and large (0.26) in magnitude [27]. Statistical analyses were conducted using IBM SPSS (Armonk, New York).
Results
Patient characteristics
A total of 259 pediatric patients with FGIDs ages 5–18 years completed all of the PedsQL™ scales included in the present study. For the 108 patients with functional constipation, the average age of the 56 boys (51.9 %) and 52 girls (48.1 %) was 9.65 years (SD = 3.23). With respect to race/ethnicity, the sample contained 68 (63.0 %) White non-Hispanic, 17 (15.7 %) Hispanic, 17 (15.7 %) Black non-Hispanic, 1 (0.9 %) Asian/Pacific Islander, and 5 (4.6 %) Other. For the 113 patients with FAP, the average age of the 32 boys (28.3 %) and 81 girls (71.7 %) was 12.50 years (SD = 3.43). With respect to race/ethnicity, the sample contained 87 (77.0 %) White non-Hispanic, 15 (13.3 %) Hispanic, 3 (2.7 %) Black non-Hispanic, 1 (0.9 %) Asian/Pacific Islander, and 7 (6.2 %) Other. For the 38 patients with IBS, the average age of the 7 boys (18.4 %) and 31 girls (81.6 %) was 13.93 years (SD = 3.49). With respect to race/ethnicity, the sample contained 32 (84.2 %) White non-Hispanic, 5 (13.2 %) Hispanic, and 1 (2.6 %) Black non-Hispanic.
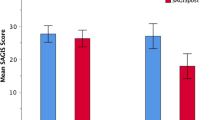
Gastrointestinal Symptoms and Generic Core Scales means and standard deviations
Table 1 contains the means and standard deviations of the Gastrointestinal Symptoms Scales and Generic Core Total Scale Score for each FGID. It is instructive to note that the Generic Core Total Score overall for healthy children has been previously reported as 83.84 (SD = 12.65, N = 5480) [29]. Thus, the Generic Core Total Scores for each of the three FGIDs are approximately 1 SD below (i.e., 71.19) the healthy population benchmark score.
Bivariate correlations between gastrointestinal symptoms with generic HRQOL
Table 1 demonstrates the bivariate correlations between the Gastrointestinal Symptoms Scales with the Generic Core Total Scale Score for each FGID. All of the Gastrointestinal Symptoms Scales were significantly correlated with generic HRQOL for pediatric patients with functional constipation or FAP (all Ps < 0.001), demonstrating medium to large effect sizes. For pediatric patients with IBS, stomach pain and stomach discomfort when eating demonstrated large effect sizes (P < 0.001), while the other gastrointestinal symptoms demonstrated medium to small effect sizes, with several symptoms not significantly associated with generic HRQOL.
Hierarchical multiple regression analyses predicting generic HRQOL in FGIDs
Table 2 presents the separate hierarchical multiple regression analyses predicting generic HRQOL in pediatric patients with functional constipation, FAP, or IBS. For pediatric patients with functional constipation, after controlling for age, gender, and race/ethnicity in Step 1, the gastrointestinal symptoms as a group in Step 2 significantly accounted for 47 % of the variability in patient-reported generic HRQOL (F (9, 95) = 10.60, P < 0.001), representing a large effect size. Stomach pain (β = 0.32, P < 0.01) and diarrhea (β = 0.22, P < 0.05) were significant individual predictor variables after controlling for the other gastrointestinal symptoms and the demographic variables.
For pediatric patients with FAP, after controlling for age, gender, and race/ethnicity in Step 1, the gastrointestinal symptoms as a group in Step 2 significantly accounted for 40 % of the variability in patient-reported generic HRQOL (F (9, 100) = 7.81, P < 0.001), representing a large effect size. Stomach pain (β = 0.34, P < 0.001) was a significant individual predictor variable after controlling for the other gastrointestinal symptoms and the demographic variables.
For pediatric patients with IBS, after controlling for age, gender, and race/ethnicity in Step 1, the gastrointestinal symptoms as a group in Step 2 significantly accounted for 60 % of the variability in patient-reported generic HRQOL (F (6, 28) = 8.75, P < 0.001), representing a large effect size. Stomach discomfort when eating (β = 0.88, P < 0.001) was a significant individual predictor variables after controlling for the other gastrointestinal symptoms and the demographic variables.
Multicollinearity statistics
Given the significant intercorrelations among the gastrointestinal symptoms predictors (see Appendix Tables 3, 4, 5), multicollinearity statistics were examined to determine whether these intercorrelations might influence the interpretability of the hierarchical multiple regression analyses. Specifically, multicollinearity can be identified using tolerance and the reciprocal variance inflation factor (VIF) statistics. A commonly accepted standard is that a tolerance value of 0.10 or less and a VIF value of 10 or more indicates evidence of problematic multicollinearity [28].
In the hierarchical multiple regression analyses for functional constipation, no gastrointestinal symptoms predictor variable demonstrated problematic multicollinearity, with the lowest tolerance value (0.34) and highest VIF value (2.98) shown for constipation. In the hierarchical multiple regression analyses for FAP, no gastrointestinal symptoms predictor variable demonstrated problematic multicollinearity, with the lowest tolerance value (0.37) and highest VIF value (2.72) shown for gas and bloating. In the hierarchical multiple regression analyses for IBS, no gastrointestinal symptoms predictor variable demonstrated problematic multicollinearity, with the lowest tolerance value (0.26) and highest VIF value (3.82.) shown for stomach upset when eating. However, for IBS, the negative beta weights for food and drink limits, nausea and vomiting, and constipation suggest multicollinearity concerns (i.e., the signs are in the opposite direction to the bivariate correlations for these three variables with generic HRQOL). Nevertheless, the significant predictor variable in the hierarchical multiple regression was stomach discomfort when eating, which demonstrated the largest bivariate correlation with generic HRQOL (r = 0.71, see Table 1). Since stomach discomfort when eating demonstrated the lowest tolerance value and highest VIF value, it is instructive to note that it was highly correlated in the bivariate intercorrelations with stomach pain and hurt (r = 0.68, see Appendix Table 5), and the three predictor variables with negative signs, that is, food and drink limits (r = 0.54), nausea and vomiting (r = 0.50), and constipation (r = 0.57). Thus, the beta weights in the hierarchical multiple regression analyses demonstrate a pattern consistent with the high bivariate correlations between stomach discomfort when eating with generic HRQOL, and the high bivariate intercorrelations of stomach discomfort when eating with stomach pain and hurt, food and drink limits, nausea and vomiting, and constipation.
Discussion
Our findings demonstrate that pediatric patient-reported gastrointestinal symptoms as a group were significant predictors of generic HRQOL in the three FGIDs studied, accounting for 47, 40, and 60 % of the variance in patient-reported generic HRQOL for functional constipation, FAP, and IBS, respectively, reflecting large effect sizes.
Our findings are unique in that we investigated the combined effects on generic HRQOL of a broad multidimensional gastrointestinal symptoms profile individually for each of the FGIDs studied, identifying the relative impact of the symptoms from the patient perspective. Past research with functional constipation, FAP, and IBS has generally investigated the impact of these gastrointestinal disorders on generic HRQOL by simply comparing the generic HRQOL scores between the specific FGID and healthy samples. In contrast, investigating the specific effects of a broad gastrointestinal symptoms profile on generic HRQOL for each FGID potentially identifies more precise treatment targets that may be amenable to tailored interventions to improve overall HRQOL in these patients. The assessment of pediatric patient gastrointestinal symptoms utilizing a standardized multidimensional gastrointestinal symptoms measurement instrument identifies in a systematic way the gastrointestinal symptoms that are most strongly associated with impaired HRQOL from the patient’s perspective. Utilizing multi-item scales to measure these symptom constructs is different than typical clinical practice and provides a more reliable and valid approach than simply asking patients about their symptoms without a standardized measurement instrument.
While our primary objective was to examine the bivariate and multivariate associations of a broad multidimensional gastrointestinal symptoms profile on generic HRQOL in three specific FGIDs, we also explored the relative significance of individual gastrointestinal symptoms in the hierarchical multiple regression analyses. Although the clinical interpretation of the findings must be considered within the constraints of the high intercorrelations among some of the symptoms scores, the hierarchical multiple regression analyses nevertheless provide plausible insights that may contribute important clinical information beyond the bivariate correlations with generic HRQOL. Specifically, for pediatric patients with constipation, stomach pain and diarrhea were the significant individual predictor variables after controlling for the other gastrointestinal symptoms and age, gender, and race/ethnicity. Even though the Constipation Scale demonstrated the lowest scale score (more gastrointestinal symptoms) among the gastrointestinal symptoms profile, followed by the Stomach Pain and Hurt and Gas and Bloating Scales, the Diarrhea Scale nevertheless includes items such as “I have poop accidents in my underwear” that may reflect fecal incontinence or encopresis and/or the effects of laxative treatments for patients with functional constipation [30]. It would be expected that overflow incontinence in one’s clothes would have a significant negative impact on patient-reported daily functioning and overall HRQOL [31, 32]. The findings for FAP are very direct, with stomach pain identified as the significant individual predictor. For IBS, the findings are more complex, in part because of the broader symptoms profile of IBS [13], and the high intercorrelations among several of the individual gastrointestinal symptoms with the resulting multicollinearity issues in the multivariate analyses. Nevertheless, the items in the Stomach Discomfort When Eating Scale, which was the only significant individual predictor variable in the IBS multivariate analyses, would appear to reflect concerns that would have a major impact on daily functioning. Specifically, the scale items such as “When I eat I get sick to my stomach,” and “When I eat my stomach feels bad” may be conceptualized as responses to “trigger foods” that may elicit the worsening of abdominal pain and the initiation of other gastrointestinal symptoms such as gas and bloating, constipation, and diarrhea [33–37]. Thus, stomach discomfort when eating, and the associated elicitation or cascading of other bothersome gastrointestinal symptoms, would logically be expected to negatively impact generic HRQOL and serves as useful patient-reported outcomes for interventions which identify and eliminate trigger foods so as to enhance daily functioning in pediatric patients with IBS. The finding of the importance of stomach discomfort when eating as a salient symptom in pediatric IBS is consistent with the literature, predominantly thus far in adult patients with IBS, highlighting the salience of postprandial worsening of stomach pain and the elicitation of associated gastrointestinal symptoms [38–40], with recommended modified diets to eliminate the purported trigger foods as common non-pharmacological interventions [41–44].
The present study included a relatively large overall sample size for patients with FGIDs, with nationwide representation. Limitations include the lack of information on families who chose not to participate, the sample size for IBS would ideally have been larger, although it is reflective of the low relative prevalence of this disorder compared with functional constipation and FAP, the lack of information on the therapies that the patients were being administered, the potential for shared method variance among the gastrointestinal symptoms scales and generic HRQOL, and the cross-sectional design, which limits assumptions of directionality in statistical prediction. Longitudinal research will be necessary to test the directionality of the variables tested [45].
In conclusion, the findings identified specific gastrointestinal symptoms and their relative impact from the patient perspective that may be important modifiable predictors of overall generic HRQOL in pediatric patients with functional constipation, FAP, and IBS. In developing interventions to ameliorate impaired overall HRQOL in these patients, targeting the potentially modifiable patient-identified gastrointestinal symptoms predictors might be most advantageous in maximizing treatment effectiveness in improving daily functioning and patient well-being.
Abbreviations
- IBS:
-
Irritable bowel disease
- FAP:
-
Functional abdominal pain
- FGID:
-
Functional gastrointestinal disorder
- HRQOL:
-
Health-related quality of life
- PedsQL™:
-
Pediatric Quality of Life Inventory™
- PRO:
-
Patient-reported outcome
References
Rasquin, A., Di Lorenzo, C., Forbes, D., Guiraldes, E., Hyams, J. S., Staiano, A., et al. (2006). Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology, 130, 1527–1537.
Varni, J. W., Bendo, C. B., Nurko, S., Shulman, R. J., Self, M. M., Franciosi, J. P., et al. (2015). Health-related quality of life in pediatric patients with functional and organic gastrointestinal diseases. Journal of Pediatrics, 166, 85–90.
Youssef, N. N., Murphy, T. G., Langseder, A. L., & Rosh, J. R. (2006). Quality of life for children with functional abdominal pain: A comparison study of patients’ and parents’ perceptions. Pediatrics, 117, 54–59.
Varni, J. W., Lane, M., Burwinkle, T., Fontaine, E., Youssef, N., Schwimmer, J., et al. (2006). Health-related quality of life in pediatric patients with irritable bowel syndrome: A comparative analysis. Journal of Developmental and Behavioral Pediatrics, 27, 451–458.
Hyams, J. S., Burke, G., Davis, P. M., Rzepski, B., & Andrulonis, P. A. (1996). Abdominal pain and irritable bowel syndrome in adolescents: A community-based study. Journal of Pediatrics, 129, 220–226.
Mohammad, S., Di Lorenzo, C., Youssef, N. N., Miranda, A., Nurko, S., Hyman, P., et al. (2014). Assessment of abdominal pain through global outcomes and recent FDA recommendations in children: Are we ready for change? Journal of Pediatric Gastroenterology and Nutrition, 58, 46–50.
Chiou, E., & Nurko, S. (2011). Functional abdominal pain and irritable bowel syndrome in children and adolescents. Therapy, 8, 315–331.
Czyzewski, D. I., Lane, M. M., Weidler, E. M., Williams, A. E., Swank, P. R., & Shulman, R. J. (2011). The interpretation of Rome III criteria and method of assessment affect the irritable bowel syndrome classification of children. Alimentary Pharmacology & Therapeutics, 33, 403–411.
Self, M. M., Czyzewski, D. I., Chumpitazi, B. P., Weidler, E. M., & Shulman, R. J. (2014). Subtypes of irritable bowel syndrome in children and adolescents. Clinical Gastroenterology and Hepatology, 12, 1468–1473.
Nurko, S., & Zimmerman, L. A. (2014). Evaluation and treatment of constipation in children and adolescents. American Family Physician, 90, 82–90.
Youssef, N. N., Langseder, A. L., Verga, B. J., Mones, R. L., & Rosh, J. R. (2005). Chronic childhood constipation is associated with impaired quality of life: A case-controlled study. Journal of Pediatric Gastroenterology and Nutrition, 41, 56–60.
Hartman, E. E., Pawaskar, M., Williams, V., McLeod, L., Dubois, D., Benninga, M. A., et al. (2014). Psychometric properties of the PedsQL Generic Core Scales for children with functional constipation in the Netherlands. Journal of Pediatric Gastroenterology and Nutrition, 59, 739–747.
Varni, J. W., Shulman, R. J., Self, M. M., Nurko, S., Saps, M., Saeed, S., et al. (2015). Symptom profiles in patients with irritable bowel syndrome or functional abdominal pain compared to healthy controls. Journal of Pediatric Gastroenterology and Nutrition, 61, 323–329.
Varni, J. W., Nurko, S., Shulman, R. J., Self, M. M., Saps, M., Bendo, C. B., et al. (2015). Pediatric functional constipation gastrointestinal symptom profile compared to healthy controls. Journal of Pediatric Gastroenterology and Nutrition, 61, 424–430.
Fayers, P. M., & Hand, D. J. (1997). Factor analysis, causal indicators and quality of life. Quality of Life Research, 6, 139–150.
Varni, J. W., Bendo, C. B., Denham, J., Shulman, R. J., Self, M. M., Neigut, D. A., et al. (2014). PedsQL™ gastrointestinal symptoms module: Feasibility, reliability, and validity. Journal of Pediatric Gastroenterology and Nutrition, 59, 347–355.
Varni, J. W., Bendo, C. B., Denham, J., Shulman, R. J., Self, M. M., Neigut, D. A., et al. (2015). PedsQL™ Gastrointestinal Symptoms Scales and Gastrointestinal Worry Scales in pediatric patients with functional and organic gastrointestinal diseases in comparison to healthy controls. Quality of Life Research, 24, 363–378.
Varni, J. W., Franciosi, J. P., Shulman, R. J., Saeed, S., Nurko, S., Neigut, D. A., et al. (2015). PedsQL™ Gastrointestinal Symptoms Scales and Gastrointestinal Worry Scales in pediatric patients with inflammatory bowel disease in comparison to healthy controls. Inflammatory Bowel Diseases, 21, 1115–1124.
Varni, J. W., Bendo, C. B., Shulman, R. J., Self, M. M., Nurko, S., Franciosi, J. P., et al. (2015). Interpretability of the PedsQL™ Gastrointestinal Symptoms Scales and Gastrointestinal Worry Scales in pediatric patients with functional and organic gastrointestinal diseases. Journal of Pediatric Psychology, 40, 591–601.
Varni, J. W., Kay, M. T., Limbers, C. A., Franciosi, J. P., & Pohl, J. F. (2012). PedsQL™ Gastrointestinal Symptoms Module item development: Qualitative methods. Journal of Pediatric Gastroenterology and Nutrition, 54, 664–671.
Varni, J. W., Seid, M., & Kurtin, P. S. (2001). PedsQL™ 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Medical Care, 39, 800–812.
Varni, J. W., Thompson, K. L., & Hanson, V. (1987). The Varni/Thompson Pediatric Pain Questionnaire: I. Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain, 28, 27–38.
Fairclough, D. L. (2002). Design and analysis of quality of life studies in clinical trials: Interdisciplinary statistics. New York: Chapman & Hall/CRC.
Varni, J. W., & Limbers, C. A. (2009). The Pediatric Quality of Life Inventory™: Measuring pediatric health-related quality of life from the perspective of children and their parents. Pediatric Clinics of North America, 56, 843–863.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). How young can children reliably and validly self-report their health-related quality of life?: An analysis of 8,591 children across age subgroups with the PedsQL™ 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5(1), 1–13.
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care, 41, 582–592.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum.
Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ: Erlbaum.
Varni, J. W., Limbers, C. A., & Burwinkle, T. M. (2007). Impaired health-related quality of life in children and adolescents with chronic conditions: A comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL™ 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5(43), 1–15.
Colombo, J. M., Wassom, M. C., & Rosen, J. M. (2015). Constipation and encopresis in childhood. Pediatrics in Review, 36, 392–401.
Cushing, C. C., Martinez-Leo, B., Bischoff, A., Hall, J., Helmrath, M., Hsi Dickie, B., Levitt, M. A., Peña, A., Zeller, M. H., & Frischer, J. S. (in press). Health related quality of life and parental stress in children with fecal incontinence: A normative comparison. Journal of Pediatric Gastroenterology & Nutrition.
Rajindrajith, S., Devanarayana, N. M., & Benninga, M. A. (2016). Fecal incontinence in adolescents is associated with child abuse, somatization, and poor health-related quality of life. Journal of Pediatric Gastroenterology and Nutrition, 62, 698–703.
Böhn, L., Störsrud, S., Törnblom, H., Bengtsson, U., & Simrén, M. (2013). Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. American Journal of Gastroenterology, 108, 634–641.
Arsie, E., Coletta, M., Cesana, B. M., & Basilisco, G. (2015). Symptom-association probability between meal ingestion and abdominal pain in patients with irritable bowel syndrome. Does somatization play a role? Neurogastroenterology and Motility, 27, 416–422.
Carlson, M. J., Moore, C. E., Tsai, C. M., Shulman, R. J., & Chumpitazi, B. P. (2014). Child and parent perceived food-induced gastrointestinal symptoms and quality of life in children with functional gastrointestinal disorders. Journal of the Academy of Nutrition and Dietetics, 114, 403–413.
Chumpitazi, B. P., Weidler, E. M., Lu, D. Y., Tsai, C. M., & Shulman, R. J. (in press). Self-perceived food intolerances are common and associated with clinical severity in childhood irritable bowel syndrome. Journal of the Academy of Nutrition and Dietetics.
Reed-Knight, B., Squires, M., Chitkara, D. K., & van Tilburg, M. A. (in press). Adolescents with irritable bowel syndrome report increased eating-associated symptoms, changes in dietary composition, and altered eating behaviors: A pilot comparison study to healthy adolescents. Neurogastroenterology & Motility.
Simrén, M., Månsson, A., Langkilde, A. M., Svedlund, J., Abrahamsson, H., Bengtsson, U., et al. (2001). Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion, 63, 108–115.
Le Nevé, B., Brazeilles, R., Derrien, M., Tap, J., Guyonnet, D., Ohman, L., et al. (2016). Lactulose challenge determines visceral sensitivity and severity of symptoms in patients with irritable bowel syndrome. Clinical Gastroenterology and Hepatology, 14, 226–233.
Ragnarsson, G., & Bodemar, G. (1998). Pain is temporally related to eating but not to defaecation in the irritable bowel syndrome (IBS): Patients’ description of diarrhea, constipation and symptom variation during a prospective 6-week study. European Journal of Gastroenterology and Hepatology, 10, 415–421.
Gibson, P. R., Varney, J., Malakar, S., & Muir, J. G. (2015). Food components and irritable bowel syndrome. Gastroenterology, 148, 1158–1174.
Capili, B., Anastasi, J. K., & Chang, M. (2016). Addressing the role of food in irritable bowel syndrome symptom management. Journal for Nurse Practitioners, 12, 324–329.
McKenzie, Y. A., Bowyer, R. K., Leach, H., Gulia, P., Horobin, J., O’Sullivan, N. A., Pettitt, C., Reeves, L. B., Seamark, L., Williams, M., Thompson, J., & Lomer, M. C. E. (in press). British Dietetic Association systematic review and evidence based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). Journal of Human Nutrition and Dietetics.
Shah, S. L., & Lacy, B. E. (2016). Dietary interventions and irritable bowel syndrome: A review of the evidence. Current gastroenterology reports, 18, 41.
Van Oudenhove, L., Törnblom, H., Störsrud, S., Tack, J., & Simrén, M. (2016). Depression and somatization are associated with increased postprandial symptoms in patients with irritable bowel syndrome. Gastroenterology, 150, 866–874.
Acknowledgments
Dr. Varni holds the copyright and the trademark for the PedsQL™ and receives financial compensation from the Mapi Research Trust, which is a nonprofit research institute that charges distribution fees to for-profit companies that use the Pediatric Quality of Life Inventory™. Dr. Varni received investigator-initiated funding from Takeda Pharmaceuticals North America, Inc. (Deerfield, Illinois) for the previous item generation qualitative methods study. Dr. Pohl received investigator-initiated funding from Takeda Pharmaceuticals North America, Inc. (Deerfield, Illinois) for the previous item generation qualitative methods study. Drs. Varni and Pohl did not receive funding from Takeda Pharmaceuticals North America, Inc. for the current quantitative methods field test study. Dr. Pohl has received the following funding: INSPPIRE to Study Acute Recurrent and Chronic Pancreatitis is Children, Grant # 10987759, National Institutes of Health (NIH), National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Pohl is on the speaker’s bureau for Medical Education Resources, Inc. Dr. Shulman is supported by NIH grants R01 NR013497 and T32 DK007664 and receives research funding from Mead-Johnson and is a consultant for Nutrinia. Dr. Nurko is supported by NIH grant K24DK082792A. Dr Saeed is on the speaker’s bureau for Abbvie, Inc. These grants are not related to the current study. The other authors report no competing interests related to this study. Dr. Saps is now at the Division of Digestive Diseases, Hepatology, and Nutrition, Nationwide Children’s Hospital, Ohio State University, Columbus, OH. Dr. Saeed is now at the Division of Pediatric Gastroenterology, Dayton Children’s Hospital, Wright State University, Dayton, OH. Dr. Vaughan Dark is now at the Division of Pediatric Pulmonology, Children’s Medical Center, Dallas, TX.
Funding
No funding was specifically designated for the PedsQL™ Gastrointestinal Symptoms Module field test study data collection effort or manuscript preparation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Item development for the PedsQL™ Gastrointestinal Symptoms Module was previously supported by Takeda Pharmaceuticals North America, Inc. Data collection for the healthy controls sample was supported by intramural funding from the Texas A&M University Foundation.
Human and animal rights
The research protocol for the field test study was approved by the Institutional Review Board at each participating institution. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committees.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
The Pediatric Quality of Life Inventory™ Gastrointestinal Symptoms Module Testing Study Consortium members are listed in the "Appendix".
Appendix: The Pediatric Quality of Life Inventory™ (PedsQL™) Gastrointestinal Symptoms Module Testing Study Consortium
Appendix: The Pediatric Quality of Life Inventory™ (PedsQL™) Gastrointestinal Symptoms Module Testing Study Consortium
The Pediatric Quality of Life Inventory™ Gastrointestinal Symptoms Module Testing Study Consortium sites include a Network and Statistical Center at the Center for Health Systems & Design, Colleges of Architecture and Medicine, Texas A&M University, College Station, TX (PI: James W. Varni, PhD), and 9 primary research data collection sites: Division of Pediatric Gastroenterology, Nationwide Children’s Hospital, Ohio State University School of Medicine, Columbus, OH (PI: Jolanda Denham, MD); Department of Pediatrics, Baylor College of Medicine, Children’s Nutrition Research Center, Texas Children’s Hospital, Houston, TX (PIs: Robert J. Shulman, MD and Mariella M. Self, PhD); Division of Gastroenterology, Hepatology and Nutrition, Children’s Hospital Colorado, Aurora, CO (PI: Deborah A. Neigut, MD); Center for Motility and Functional Gastrointestinal Disorders, Boston Children’s Hospital, Harvard Medical School, Boston, MA (PI: Samuel Nurko, MD); Division of Pediatric Gastroenterology, Children’s Medical Center of Dallas, University of Texas Southwestern Medical School, Dallas, TX (PI: Ashish S. Patel, MD); Division of Gastroenterology, Hepatology and Nutrition, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH (PIs: James P. Franciosi, MD, Shehzad Saeed, MD, and George M. Zacur, MD); Division of Gastroenterology, Hepatology and Nutrition, Lurie Children’s Hospital of Chicago, Northwestern University Feinberg School of Medicine, Chicago, IL (PI: Miguel Saps, MD); Division of Pediatric Gastroenterology, Hepatology and Nutrition, Goryeb Children’s Hospital, Morristown Medical Center, Morristown, NJ (PI: Barbara Verga, MD); Department of Pediatric Gastroenterology, Primary Children’s Hospital, University of Utah, Salt Lake City, UT (PI: John F. Pohl, MD).
See Appendix Tables 3, 4, and 5.
Rights and permissions
About this article
Cite this article
Varni, J.W., Shulman, R.J., Self, M.M. et al. Gastrointestinal symptoms predictors of health-related quality of life in pediatric patients with functional gastrointestinal disorders. Qual Life Res 26, 1015–1025 (2017). https://doi.org/10.1007/s11136-016-1430-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1430-3