Abstract
Irritable bowel syndrome (IBS) is the best studied of the functional gastrointestinal disorders. It is a highly prevalent disorder characterized by symptoms of abdominal pain, bloating, and disordered bowel habits, which may include constipation, diarrhea, or both. IBS has a significant negative impact on patients, both financially and with regard to their quality-of-life. At present, there is no cure for IBS, and while there are a number of pharmacological therapies available to treat IBS symptoms, they are not uniformly effective. For this reason, many patients and providers are turning to dietary interventions in an attempt to ameliorate IBS symptoms. At first glance, this approach appears reasonable as dietary interventions are generally safe and side effects, including potential adverse reactions with medications, are rare. However, although dietary interventions for IBS are frequently recommended, there is a paucity of data to support their use. The goals of this article are to answer key questions about diets currently recommended for the treatment of IBS, using the best available data from the literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
J.S. is a 27-year-old woman sent for a second opinion in gastroenterology for the management of her symptoms of irritable bowel syndrome (IBS). Her symptoms began in college and have slowly progressed over the past 8 years. She has bilateral, lower abdominal pain more days than not that is transiently relieved by having a bowel movement, although sometimes having a bowel movement seems to worsen her underlying pain. She describes significant gas and bloating and feels “like I am pregnant” more days than not. Some days she has to strain to evacuate hard, pellet-like stool, while other days she has 4 to 5 loose, urgent, watery, non-bloody bowel movements. Her weight has remained stable over the last 8 years. Laboratory tests on several occasions have been normal including a complete blood count, a comprehensive metabolic panel, thyroid function tests, and a tissue transglutaminase antibody. A colonoscopy performed for a research study on IBS was normal, including random biopsies. She has tried a number of different medications for IBS without any significant success and would like to try to improve her symptoms using just diet. She works in a chemistry lab and teaches cooking as a part-time job. She asks what diets are available to treat IBS symptoms and wonders what the evidence is to support their use.
The relationship between diet and the symptoms of IBS is not only incredibly complex, but also incompletely understood. Remarkably, over 70 % of patients with IBS attribute their symptoms to food, with the most commonly indicted culprits being high-carbohydrate foods, dairy, beans, foods rich in fats and spice, and lentils among others [1–4]. As a result, there has been increasing interest in evaluating dietary interventions for the treatment of IBS. However, despite the popularity of various IBS diets, data from large randomized controlled trials are limited, leaving clinicians with the challenge of providing patients with reliable guidance based on minimal evidence.
Irritable bowel syndrome is the most prevalent and well-studied functional gastrointestinal disorder worldwide, affecting patients across a broad range of ages, ethnicities, and socioeconomic statuses. The economic impact in the USA of IBS is noteworthy as there are an estimated 3.65 million health care visits annually for IBS, contributing significantly to health care resource utilization [5]. In fact, IBS patients incur average health care costs that are nearly 51 % higher than that of matched controls [6–8]. Numerous pharmacological therapies are available for IBS, but none are curative in nature, and often are unable to ameliorate the most bothersome IBS symptoms such as bloating [9, 10]. Thus, there has been somewhat of a paradigm shift in looking to specialized diets for symptom relief in patients with IBS.
Unsurprisingly, patients with IBS report more food-related trouble than normal subjects [2,4,11]. However, despite the widespread use of various dietary therapies in patients with IBS, diagnostic tests attempting to predict food intolerances and the data supporting these aforementioned dietary interventions have been rather limited. In this review, we aim to highlight the current literature on various diets for IBS, evaluating the strengths and limitations of each study, while proposing recommendations clinicians can provide their patients with IBS based on the evidence.
Does Fiber Supplementation Work for Patients With IBS?
For many years, fiber has been widely recommended to patients with IBS and perhaps in large part, a result of its low cost and availability over-the-counter. While the mechanism of fiber’s benefit is incompletely understood, the presumption is that enhanced colonic metabolism and fermentation or its action as a prebiotic plays a significant role [12, 13]. A 2014 systematic review and meta-analysis by Moayyedi et al. evaluated 14 randomized controlled trials involving dietary fiber supplementation in 906 IBS patients [14•]. Fiber, particularly soluble fiber such as psyllium, was found to be more effective at improving global IBS symptoms as compared to placebo (RR = 0.86; 95 % CI = 0.80–0.94 with an NNT = 10; 95 % CI = 6–33). Only two of the studies used Rome criteria for the diagnosis of IBS, and clinical benefit was not found with insoluble dietary fiber such as bran (RR = 0.90; 95 % CI = 0.79–1.03). Furthermore, there was no evidence of harm from fiber supplementation, albeit bloating often worsens if introduced too swiftly. Thus, there appears to be little downside to using dietary soluble fiber in patients with IBS with some evidence of potential benefit.
Is There Enough Evidence to Recommend Exclusion Diets for Patients With IBS?
Dietary elimination has long been recommended for gastrointestinal ailments and particularly for IBS. A study from the 1980s showed that a 1-week trial of strict elimination of all foods except distilled or spring water and one meat and one fruit resulted in initial symptom improvement among 14 of 21 IBS patients [15]. However, a recent systematic review by Moayyedi et al. in 2015 evaluated 17 randomized controlled trials involving elimination diets in 1568 IBS patients [16]. Only three of the trials with a total of 230 patients met eligibility criteria and with a wide variety of different approaches to dietary elimination, a meta-analysis could not be performed. Unfortunately, because of limited data and unknown potential adverse effects from long-term food restriction, strict exclusion diets should not be routinely recommended to patients with IBS.
What About a low-Carbohydrate Diet for Patients With IBS?
Carbohydrates are thought to precipitate gastrointestinal symptoms as a result of poor absorption in the small intestine and an increased osmotic load with significant bacterial fermentation in the colon [17]. A 2009 study by Austin et al. evaluated the impact of a low-carbohydrate diet in 17 patients with IBS-D (Rome II criteria) [18]. Only 13 of the 17 patients completed the study, adhering to consuming less than 20 g of carbohydrates per day for 4 weeks. All of the patients were considered responders as they reported relief of symptoms during at least one of the study weeks. Significant improvements were noted in stool frequency and consistency (p < 0.001), abdominal pain (p = 0.007), and quality-of-life measures (p = 0.02). No studies looking at the impact of a low-carbohydrate diet have been performed in IBS-C patients and a frequent symptom associated with low carbohydrate diets is constipation. Given the lack of data on a low-carbohydrate diet, a general recommendation to all IBS patients cannot be made.
What About a low-Fructose Diet for Patients With IBS?
Over the past three decades, the annual amount of fructose consumed has increased dramatically, with the vast majority being in the form of high-fructose corn syrup [19]. Fructose is poorly absorbed in the small intestine and acts as a prebiotic in the colon, increasing colonic gas formation leading to distension and abdominal distress in many patients with IBS [20]. A study published by Shepherd et al. in 2006 evaluated 62 IBS patients (Rome II criteria) with known fructose malabsorption on a fructose-restricted diet [21]. Patients were monitored by telephone for up to 40 months (median of 14 months) with instructions to maintain a diet limiting free-fructose and short-chain fructans and consume foods in which glucose was balanced with the amount of fructose. The authors found that 46 of the 48 patients (77 %) who adhered to the diet achieved at least a 5-point improvement in their gastrointestinal symptoms (i.e., abdominal pain, gas, bloating, nausea, diarrhea, and constipation). Patients who were adherent to a low-fructose diet experienced better symptom response than those who were non-adherent (85 vs. 36 %; p < 0.01). Similarly, a study published in 2008 retrospectively looked at 31 IBS patients (Rome II criteria) with known fructose malabsorption and found IBS symptom improvement with adherence to a fructose-restricted diet [22]. Of the 26 patients (84 %) who participated in a follow-up evaluation (mean of 13 months), 14 (53 %) of them were compliant with a low-fructose diet and reported improvement in abdominal pain, belching, fullness, indigestion, and diarrhea as compared to baseline (p < 0.02). The 12 patients who were non-adherent to the diet experienced no change in their symptoms with the exception of improvement in belching. Poor adherence and challenges with long-term maintenance of a fructose and fructan-restricted diet have limited widespread recommendations to IBS patients.
What About a Gluten-Free Diet for Patients With IBS and Without Celiac Disease?
While the prevalence of gluten intolerance in patients without celiac disease is unknown, it is estimated by one study that nearly one in four patients with self-reported non-celiac gluten sensitivity actually carry the diagnosis [23]. While the pathophysiology of gluten ingestion causing gastrointestinal symptoms is unclear, theories include a local immune response, changes in intestinal permeability, and an increased osmotic load in the gastrointestinal tract. In 2011, Biesiekierski et al. published a double-blind, placebo-controlled rechallenge trial in 34 patients (31 females) with IBS (Rome III criteria) in whom celiac disease was excluded [24]. Patients were randomized to receive either gluten (16 g per day) or placebo in addition to being told to maintain a gluten-free diet for 6 weeks. Symptom response was assessed using a visual analogue scale and laboratory testing (serum tissue transglutaminase, gliadin, and endomysial antibody, serum C-reactive protein, fecal lactoferrin, and urine after a lactulose and rhamnose challenge to assess intestinal permeability). Of the 19 patients in the gluten exposure cohort, 13 of them reported poor symptom control as compared to only six patients in the placebo exposure cohort (68 vs. 40 %; p = 0.0001). Using a visual analog scale, those exposed to gluten reported feeling worse within 1 week with symptoms such as abdominal pain (p = 0.016), bloating (p = 0.031), and tiredness (p = 0.001). Interestingly, no differences were observed between the groups in terms of celiac antibodies, C-reactive protein, fecal lactoferrin, and measurements of intestinal permeability.
A study supporting the aforementioned results is a randomized controlled trial that evaluated the effects of a gluten-free diet versus a gluten-containing diet among 45 patients with IBS-D (Rome III criteria) [25]. Celiac disease was excluded in all patients, and measurements of daily bowel function, small intestinal and colonic permeability, and tight junction proteins were performed. Patients randomized to a gluten-free diet had fewer bowel movements per day (p = 0.04) with even greater improvements in those positive for HLA-DQ2 or HLA-DQ8. In this study, however, the authors found that small bowel permeability was increased in the gluten exposure cohort (p = 0.028). The effects were more pronounced in those positive for HLA-DQ2/8, suggesting a potential physiological mechanism of why symptoms may have improved in IBS-D patients on a gluten-free diet.
More recently, Aziz et al. published a prospective study evaluating 41 patients with IBS-D (Rome III criteria) on a 6 week gluten-free diet [26•]. Approximately half of the patients were HLA-DQ2/8 positive, and a clinical response was defined as at least a 50-point decrease in the IBS Symptom Severity Score. After a 6-week gluten-free trial, 29 patients (71 %) were clinical responders with a mean total score decrease from 286 at baseline to 131 after 6 weeks (p < 0.0001). Symptom reduction was similar in both HLA-DQ cohorts. The HLA-DQ2/8 negative group, however, did have greater reductions in abdominal distension (p = 0.04). Twenty-one (72 %) of the 29 clinical responders were followed as far as 18 months after the study with continued symptom improvement on a gluten-free diet. While these results seem promising, data on gluten avoidance continues to remain limited with uncertainty as to long-term effects and how it fares in comparison to other dietary interventions.
Is There Enough Evidence to Recommend a low-FODMAP Diet to all Patients With IBS?
Recently, there has been much enthusiasm about diets low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs). A 2010 study using hydrogen breath testing showed that a diet high in FODMAPs produces intestinal gas and other bothersome gastrointestinal symptoms in both IBS patients and healthy controls [27]. Dr. Peter Gibson was the first to demonstrate an association between a low-FODMAP diet and IBS symptom improvement; however, these initial studies were retrospective in nature and conducted at a single center in Australia [21, 28]. In 2011, an observational study out of the UK evaluated 82 IBS patients who met NICE criteria and randomized them to either a low-FODMAP or standard English diet [29]. More patients in the low-FODMAP cohort reported symptom improvement (86 vs. 54 %; p = 0.038). Significant improvements in bloating (p = 0.02), abdominal pain (p = 0.023), and flatulence (p = 0.001) were seen in the low-FODMAP group as compared to the standard diet group. Sixty-four percent of patients reported strict adherence to a low-FODMAP diet during the 9-month study period. However, limitations of the study included the lack of a standardized diet, different dieticians providing dietary advice, and the lack of control for use of IBS pharmacological therapy.
The first prospective, randomized controlled trial to evaluate a low-FODMAP diet was published in 2012 by Staudacher et al. [30]. A total of 41 IBS patients (Rome III criteria) were randomized to either a low-FODMAP or habitual diet during a 4-week study period. Using a validated IBS scoring system, patients in the low-FODMAP cohort reported a greater improvement in overall IBS symptoms as compared to those in the habitual diet cohort (68 vs. 23 %; p < 0.05). Interestingly, there were lower concentrations of bifidobacteria in the low-FODMAP group as compared to the usual diet group when adjusted for baseline (p < 0.001), suggesting a potential impact on the gut microbiome. Limitations of this study, however, included the small sample size as well as the lack of a standardized “habitual” and low-FODMAP diet.
A larger prospective study published in 2013 by De Roest et al. evaluating 90 patients with IBS found that a low-FODMAP diet significantly improved symptoms of abdominal pain, bloating, flatulence, and diarrhea during a mean follow-up of nearly 16 months (p < 0.001 for all) [31••]. Those identified with fructose intolerance via hydrogen breath testing experienced greater symptom improvement than those with a normal breath test. Limitations of this study included the lack of a standardized FODMAP diet, vague IBS criteria, and the lack of a standardized questionnaire.
In 2014, the Australian group led by Halmos et al. published a single-blind, placebo-controlled, cross-over study in 30 patients with IBS (Rome III criteria) [32]. The authors randomly assigned groups to either 21 days of a low-FODMAP (0.5 g of FODMAPs per meal) or typical Australian diet followed by a washout period of at least 21 days before crossing over to the other diet. Using a visual analogue scale, the authors reported a near halving of global IBS symptom scores in the low-FODMAP cohort as compared to those consuming a typical Australian diet (22.8 vs. 44.9; p < 0.01). Abdominal pain, bloating, and passing flatus were also significantly better in the low-FODMAP group. The greatest improvement in symptoms occurred during the first week in most patients with no differences noted among the various IBS subtypes. Albeit a better designed study, the cross-over design, the use of an Australian diet, and the small sample size make it a challenge to apply these results to all patients with IBS.
More recently, a multi-center, parallel, single-blind study of 75 IBS patients (Rome III criteria) was performed with patients randomized to either a low-FODMAP or “frequently recommended” IBS diet (low-fat, avoidance of gas-producing foods, small meals) [33••]. Patients were followed over a 4-week period, and 67 patients (85 %) completed the dietary intervention. The severity of global IBS symptoms, as measured by the IBS Symptom Severity Score, was significantly reduced in both cohorts at the end of 4 weeks (p < 0.0001) with no significant differences in response between the two cohorts (p = 0.62). These findings raise the notion of potentially combining different facets of dietary interventions to trial in patients with IBS.
Undoubtedly, there is a growing body of evidence suggesting the use of a low-FODMAP diet in patients with IBS, and particularly in those with bloating. However, while the diet appears safe for short-term use, long-term data is lacking and studies thus far have had significant limitations, making it a challenge for clinicians to provide an evidence-based recommendation to all patients with IBS. Multicenter, prospective studies of a low-FODMAP diet are greatly needed to better address the aforementioned concerns.
How Does the Low-FODMAP Diet Compare Against Other Diets for Patients With IBS?
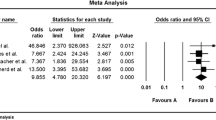
There have been two studies comparing a low-FODMAP diet to other dietary interventions. One randomized, unblinded controlled trial compared a low-FODMAP diet to the probiotic Lactobacillus rhamnosus GG (2 capsules daily), as well as a normal Danish diet in 123 IBS patients (Rome III criteria) [34•]. Over a 6-week treatment period, IBS symptom severity scores were lower in both intervention cohorts as compared to the standard Danish diet cohort (p < 0.01). While quality-of-life was not significantly changed in either of the groups (p = 0.13), a subgroup analysis revealed that patients with IBS-D were more likely to have an improved quality-of-life. This study had significant limitations including the lack of blinding, a placebo capsule, and standardization of meals.
The other study is a double-blind, cross-over study comparing a low-FODMAP diet to a gluten-free diet in 37 IBS patients (Rome III criteria) [35]. Celiac disease was excluded and all patients had previously reported symptom improvement on a gluten-free diet with at least a 6-week trial. Patients were placed on a low-FODMAP diet for 2 weeks, and then randomized to either a high-gluten (16 g of gluten per day), a low-gluten (2 g of gluten per day), or a placebo diet (16 g of whey protein per day) for 1 week, followed by a washout period of at least 2 weeks. Symptoms were evaluated with a visual analogue scale, and after resolution of symptoms during the 1 week challenge, patients were crossed-over to the second and third dietary arms. In all patients, IBS symptoms significantly improved with the low-FODMAP diet after the 2-week run-in period (p < 0.001). During the 1-week study diet period, symptoms worsened in all three dietary arms (p < 0.001). Bloating and fatigue were worse in the placebo and low-gluten cohorts as compared to the high-gluten cohort. These results are interesting in that patients who previously expressed symptom improvement with a gluten-free diet remained symptomatic upon reintroduction of gluten after being on a low-FODMAP diet for 2 weeks. The notion that there may be a dietary component other than gluten that generates gastrointestinal symptoms in IBS patients is incredibly important for patients to understand.
Conclusions
Given the intricate relationship between IBS symptoms and diet, it has become more important than ever to engage patients in the treatment process. While clinicians routinely scrutinize their patients’ daily dietary intake, the greater challenge is often in distinguishing diet-related symptoms from symptoms related to IBS. Diets have become somewhat of a fad among patients with IBS, but careful advice must be provided to patients given the limited studies and lack of long-term data. A dietary intervention should ideally involve a multidisciplinary team approach with a dietician to help tailor the specific therapy to each individual patient.
We recommend having patients keep a detailed log of daily dietary intake, aiming to identify particular foods that may exacerbate symptoms. An initial trial of an individual dietary intervention should be considered if certain foods appear to be culprits such as fructans or gluten. However, if patients continue to have persistent symptoms despite such a trial or no suspect foods are identified, we suggest a low-FODMAP diet with consultation of a dietician to help patients identify meals that adhere to such a prohibitive diet. A reasonable trial would be 4 weeks as long-term studies have yet to be conducted with unknown untoward consequences such as potential nutritional deficiencies or unfavorable effects on the gut microbiome. Specialty diets have garnered much interest over the past decade, but with limited data on long-term safety and efficacy, there still exists no one-size-fits-all dietary intervention for patients with IBS.
Abbreviations
- FODMAP:
-
Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols
- IBS:
-
Irritable bowel syndrome
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bohn L, Storsrud S, Tornblom H, Bengtsson U, Simren M. Self-reported food-related gastrointestinal symptoms of IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108:634–41.
Locke GR, Zinsmeister AR, Talley NJ, Fett SL, Melton SJ. Risk factors for irritable bowel syndrome: role of analgesics and food sensitivities. Am J Gastroenterol. 2000;95:157–65.
Monsbakken KW, Vandvik PO, Farup PG. Perceived food intolerance in subjects with irritable bowel syndrome—etiology, prevalence and consequences. Eur J Clin Nutr. 2006;60:667–72.
Simren M, Mansson A, Langkilde AM, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63:108–15.
National Ambulatory Medical Care Survey. National Center for Health Statistics: NAMCS Description. Available at: http://www.cdc.gov/nchs/about/major/ahcd/namcsdes.htm.
Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–87.
Longstreth GF, Wilson A, Knight K, Wong J, Chiou CF, Barghout V, et al. Irritable bowel syndrome, health care use, and costs: a U.S. managed care perspective. Am J Gastroenterol. 2003;98:600–7.
Maxion-Bergemann S, Thielecke F, Abel F, Bergemann R. Costs of irritable bowel syndrome in the UK and US. Pharmacoeconomics. 2006;24:21–37.
Chang L, Lembo A, Sultan S. American Gastroenterological Association Institute technical review pharmacological management of irritable bowel syndrome. Gastroenterology. 2014;147:1149–72.
Ford AC, Moayeddi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol. 2014;109 Suppl 1:S2–26.
Chey WD, Olden K, Carter E, et al. Utility of the Rome I and Rome II criteria for irritable bowel syndrome in U.S. women. Am J Gastroenterol. 2002;97:2803–11.
Stephen AM, Cummings JH. Mechanism of action of dietary fibre in the human colon. Nature. 1980;284:283–4.
Eswaran S, Muir J, Chey WD. Fiber and functional gastrointestinal disorders. Am J Gastroenterol. 2013;108:718–27.
Moayyedi P, Quigley EMM, Lacy BE, et al. The effect of fiber supplementation on irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1367–74. Systematic review and meta-analysis showing efficacy of dietary soluble fiber supplementation over placebo at improving global IBS symptoms.
Jones VA, Mclaughlan P, Shorthouse M, Workman E, Hunter JO. Food intolerance: a major factor in the pathogenesis of irritable bowel syndrome. Lancet. 1982;2:1115–7.
Moayyedi P, Quigley EM, Lacy BE, et al. The effect of dietary intervention on irritable bowel syndrome: a systematic review. Clin Transl Gastroenterol. 2015;6:e107.
Barrett JS, Gearry RB, Muir JG, et al. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010;31:874–82.
Austin GL, Dalton CB, Hu Y, et al. A very low-carbohydrate diet improves symptoms and quality of life in diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009;7:706–8.
Marriott BP, Cole N, Lee E. National estimates of dietary fructose intake increased from 1977 to 2004 in the United States. J Nutr. 2009;139:1228S–35.
Madsen JL, Linnet J, Rumessen JJ. Effect of nonabsorbed amounts of a fructose-sorbitol mixture on small intestinal transit in healthy volunteers. Dig Dis Sci. 2006;51:147–53.
Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc. 2006;106:1631–9.
Choi YK, Kraft N, Zimmerman B, Jackson M, Rao SSC. Fructose intolerance in IBS and utility of fructose-restricted diet. J Clin Gastroenterol. 2008;42:233–8.
Biesiekierski JR, Newnham ED, Shepherd SJ, Muir JG, Gibson PR. Characterization of adults with a self-diagnosis of nonceliac gluten sensitivity. Nutr Clin Pract. 2014;29:504–9.
Biesiekierski JR, Newnham ED, Irving PM, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011;106:508–14.
Vazquez-Roque MI, Camilleri M, Smyrk T, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013;144:903–11.
Aziz I, Trott N, Briggs R, North JR, Hadjivassiliou M, Sanders DS. Efficacy of a gluten-free diet in subjects with irritable bowel syndrome-diarrhea unaware of their HLA-DQ2/8 genotype. Clin Gastroenterol Hepatol. 2015;14(5):696–703.e1. Prospective study evaluating 41 IBS-D patients on a 6-week gluten-free diet with modest symptom improvement in vast majority of patients.
Ong DK, Mitchell SB, Barrett JS, et al. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010;25:1366–73.
Gearry RB, Irving PM, Barrett JS, Shepherd SJ, Gibson PR. Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease—a pilot study. J Crohns Colitis. 2009;3:8–14.
Staudacher HM, Whelan K, Irving PM, Lomer MCE. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011;24:487–95.
Staudacher HM, Lomer MCE, Anderson JL, et al. Fermentable carbohydrate restriction reduces luminal Bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012;142:1510–8.
De Roest RH, Dobbs BR, Chapman BA, et al. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract. 2013;67:895–903. Prospective study evaluating 90 IBS patients on a low-FODMAP diet with significant improvements in global IBS symptoms.
Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;46:67–75.
Böhn L, Störsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology. 2015;149:1399–407. Multi-center, parallel, single-blind study evaluating 75 IBS patients randomized to either a low-FODMAP or “frequently recommended” IBS diet finding significant reductions in global IBS symptoms in both cohorts.
Pedersen N, Andersen NN, Vegh Z, et al. Ehealth: low FODMAP diet vs. Lactobacillus rhamnosus GG in irritable bowel syndrome. World J Gastroenterol. 2014;20:16215–26. Randomized, unblinded controlled trial evaluating 123 IBS patients with significant IBS symptom improvement in both the low-FODMAP diet and probiotic cohorts as compared to a normal Danish diet cohort.
Biesiekierski JR, Peters SL, Newnham ED, et al. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013;145:320–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
SLS and BEL declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Large Intestine
Rights and permissions
About this article
Cite this article
Shah, S.L., Lacy, B.E. Dietary Interventions and Irritable Bowel Syndrome: A Review of the Evidence. Curr Gastroenterol Rep 18, 41 (2016). https://doi.org/10.1007/s11894-016-0517-x
Published:
DOI: https://doi.org/10.1007/s11894-016-0517-x