Abstract
Non-suicidal self-injury (NSSI) is an increasingly prevalent phenomenon associated with many detrimental outcomes, ranging from poor academic performance to suicide attempts. Research on self-harming behaviors has identified emotion dysregulation, negative affect, and borderline pathology as strong risk factors of NSSI, whereas the potential protective effects of metacognitive skills such as decentering have not yet been explored. The current study combined ecological momentary assessment (EMA) and self-report measures to explore potential risk and protective factors of NSSI in a clinical group of Borderline Personality Disorder (BPD) patients with NSSI (N = 22), a subclinical group of college students with NSSI (N = 19), and a non-clinical healthy control group (N = 23). Participants completed self-report measures of borderline pathology, emotion dysregulation, decentering ability, and negative emotional symptoms, and they used the Sinjur App (EMA instrument) at least three times a day for 15 days to capture negative affect and NSSI in daily life. A multilevel mixed-effect regression analysis with both self-report and EMA measures was conducted to identify predictors of NSSI. The multilevel analysis showed that only momentary frustration directly predicted NSSI. Momentary guilt and anger only predicted NSSI when interacting with more stable traits of borderline pathology and negative emotional symptoms. Most importantly, greater decentering capacity protected against self-injury and attenuated the association between momentary sadness and NSSI. Findings contribute novel knowledge about NSSI, documenting the protective effects of decentering and highlighting the benefit of interventions that target metacognitive emotion regulation skills.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Non-suicidal self-injury (NSSI) is commonly defined as the deliberate destruction of one’s own body tissue in the absence of conscious suicidal intent [1]. In the past years, the incidence of NSSI among adolescents and young adults has increased at an alarming rate [2,3,4], becoming a major public health concern [5]. In addition, NSSI has been associated with numerous psychiatric and behavioral issues, including academic problems [6], interpersonal difficulties, psychological suffering, and later suicide [7,8,9]. Effectively, NSSI has emerged as a significant psychiatric phenomenon, and it has been included in the last version of the DSM [10] as a “new condition for further study”. The growing prevalence of this phenomenon in both clinical and community populations emphasizes the continued benefit of research to help clarify the factors that confer risk for and protect against self-harm.
Over the past decades, NSSI has emerged as a potential early behavioral symptom in the developmental trajectory to Borderline Personality Disorder (BPD) [11,12,13], a serious mental illness characterized by a pervasive pattern of instability in interpersonal relationships, sense of self, and affective states [14]. Both theory and research suggest that emotion dysregulation, a specific risk factor for NSSI engagement (see for a recent meta-analysis: [15]), lies at the core of BPD [11, 14, 16]. Previous studies show that relative to healthy controls, individuals with BPD exhibit greater reactivity to emotional stimuli [17, 18] and higher negative emotions at baseline [19], which makes them more prone to resort to NSSI to reduce or remove aversive emotional experiences [20].
Previous theoretical work has proposed that NSSI serves to regulate negative emotions and return to emotional baselines [21,22,23,24]. Correspondingly, self-report studies indicate that individuals who engage in NSSI show a tendency to experience more negative emotions [25]. For instance, NSSI has been associated with depressive symptoms and neuroticism [26,27,28], and self-directed negative emotions such as self-derogation, self-criticism, and low self-esteem [29, 30]. In addition, individuals who engage in self-injury retrospectively report that NSSI is commonly preceded by a variety of distressing emotions such as anxiety, anger, sadness, or frustration, which decrease in intensity after NSSI [29, 31,32,33]. Consistent with the affect regulation function of NSSI, a laboratory study showed that after a stress induction, a forearm incision (analogous to NSSI) was able to reduce aversive tension and heart rate in participants with Borderline Personality Disorder (BPD) and NSSI, but not in healthy controls [34]. Using a similar methodology, these researchers also found that the forearm incision in BPD patients with NSSI reduced amygdala activity and normalized its functional connectivity with the superior frontal gyrus [35].
These findings cohere with previous studies that proposed a two-factor model to explain motivations (or functions) for engaging in NSSI. On the one hand, intrapersonal functions involve motivations associated with changes in one’s internal state, such as an emotional state or thoughts (e.g., affect regulation or self-punishment), while on the other hand, interpersonal functions involve motivations associated with changes in the external environment (e.g., revenge) [36, 37]. Self-report studies investigating motivations for NSSI engagement [38] suggest that affect regulation (i.e., an intrapersonal function) is the most commonly reported NSSI function, endorsed by more than 90% individuals [39] (see for a recent meta-analysis: [24]).
Although the motivations for NSSI have been widely studied with self-reports, these studies are limited by their retrospective nature and memory biases [40]. When asked to state the reasons for which they incur to NSSI, individuals who engage in self-injury most commonly report that they do it to alleviate intense negative emotions or thoughts (i.e., intrapersonal function) [41,42,43], while a significant portion of them (27%) report having difficulties with identifying the NSSI-function [41]. Ecological momentary assessment (EMA), a methodology tailored to study real-time NSSI in context [40], may be a more optimal technique which allows researchers to infer NSSI motives by exploring antecedents and consequences surrounding NSSI acts [44], while obviating retrospective bias and maintaining ecological validity [40].
Crucially, although interpersonal conflicts have been identified as common triggers for NSSI in self-report studies [45], only a few EMA studies have directly investigated interpersonal functions in individuals with NSSI [46, 47]. By using experience sampling methods, Snir and colleagues [46] found a discrepancy between explicit and inferred interpersonal motives for NSSI in a sample of patients with BPD and APD (Avoidant Personality Disorder). While participants failed to report explicit endorsement of interpersonal motives for NSSI, experience sampling revealed that these motives do influence NSSI engagement, albeit unconsciously [46]. Specifically, the authors reported that perceived rejection and isolation from others increased prior to NSSI, and decreased post NSSI, indicating interpersonal negative reinforcement as an inferred motive for NSSI. Additionally, Turner and colleagues [47] found that while interpersonal conflict was elevated on the days during which participants with mood, anxiety, or borderline disorder engaged in NSSI, social support also increased on those days, suggesting that NSSI can elicit positive interpersonal reinforcement [48]. Given the dearth of research on the interpersonal functions of NSSI, more EMA work is needed to rigorously test NSSI functions, as such evidence may diverge substantially from self-report findings.
Evidently, EMA studies have brought complementary data to previous findings [44]. To date, the EMA approach to NSSI has mainly focused on affectivity (for exceptions regarding interpersonal and cognitive aspects, see: [45, 49]), identifying affective instability and negative affectivity as significant predictors of NSSI [28, 50]. For example, in examining a sample of young adults with eating disorders, Turner and colleagues [47] found that the days marked by NSSI occurrences were also marked by more intense negative mood. In a nonclinical sample of university students, Victor and Klonsky [25] found that those with NSSI experienced greater negative and less positive emotions than students without NSSI. Collectively, EMA studies provide convergent evidence indicating that NSSI episodes are preceded by increased negative emotions, both in nonclinical [51] and clinical samples [52]. In this regard, two studies in youths with BPD showed that NSSI engagement was associated with the intensity [41] and frequency of simultaneous negative emotions (i.e., complex emotions) experienced prior to NSSI [53].
Both EMA and self-report research corroborate the notion that negative affect constitutes a powerful predictor of NSSI. However, elevated negative affect may not invariably lead to NSSI engagement; dispositional moderators may interact with one’s level of negative affect to predict mental health outcomes. Indeed, a recent study reported that decentering, a metacognitive ability to take a detached, observer perspective on one’s internal experiences and the capacity to observe one’s thoughts and emotions as objective, transient events of the mind, rather than personally identifying with them [54, 55], moderates or attenuates the association between negative affect and internalizing symptoms in both cross-sectional and EMA designs [56]. High decentering capacity has also been associated with healthy cognitive, psychological, and social functioning [55], and empirical evidence suggests that changes in decentering temporally precede reductions in worry and anxiety during emotion regulation therapy for generalized anxiety disorder (GAD; [57]). Given its role in regulating emotions, decentering is inversely associated with emotion dysregulation and is involved in cognitive reappraisal, a core emotion regulation strategy [58]. In fact, decentering has been proposed as a putative common mechanism underlying both cognitive reappraisal and mindfulness [59]. Complementarily, while high decentering capacity seems to protect against mental health problems, poor decentering capacity has been associated with a wide range of psychopathology and emotion regulation difficulties [57, 60], and could be considered a transdiagnostic vulnerability factor.
Despite emerging research linking decentering with a wide range of psychopathology, no previous studies specifically address how decentering may be related to NSSI. Innovatively, the current study combined ecological momentary assessment (EMA) and self-report measures to explore whether decentering (assessed by self-reports) would protect against NSSI engagement, and would moderate the association between momentary negative affect (e.g. anger, frustration, guilt, and sadness as captured by EMA) and NSSI. We conducted a multilevel analysis with a combination of self-report and EMA measures to examine potential risk and protective factors of NSSI.
Given the growing prevalence of NSSI in both clinical and community samples, we recruited a clinical group of BPD patients with NSSI and a subclinical group of college students with NSSI, to make results generalizable to both clinical and community populations. We used EMA to capture negative affect and NSSI in daily life and we predicted that momentary negative affect, that is, sadness, anger, frustration, and guilt would precede or predict NSSI episodes, lending support to the affect-regulation (e.g. intrapersonal) function of NSSI. Secondly, we predicted that interpersonal conflicts or discussions with others (captured by EMA) would also predict NSSI episodes, lending support to the interpersonal function of NSSI. Most importantly, we predicted that adaptive metacognitive emotion regulation skills, that is, greater decentering capacity, would protect against NSSI; specifically, we expected that greater decentering (measured with self-reports) would be associated with lower likelihood of NSSI engagement and would attenuate the associations between momentary negative affect and NSSI. Lastly, given the strong co-occurrence of BPD with NSSI and the role of emotion dysregulation in NSSI, we predicted that greater borderline pathology (BPQ), greater emotion dysregulation (DERS), and greater symptoms of anxiety, stress, and depression (DASS-21) would predict NSSI engagement and would exacerbate the association between negative affect and NSSI.
Materials and Methods
Participants
The study sample consisted of 64 young adults (ages between 18 and 33 years), divided into three groups. The first two groups consisted of participants with NSSI (≥ 5 NSSI events in the previous 12 months): (i) a subclinical group of university students recruited from the city of Igualada in Barcelona, Spain (STD group; N = 19) and, (ii) a clinical group of BPD patients (BPD group; N = 22). Students were not receiving any psychological or psychiatric treatment, and they completed the Structured Clinical Interview for Axis II personality disorders (SCID-II; [61]) to ensure that they did not meet criteria for a BPD diagnosis. Patients with BPD were recruited from two specialist BPD units in the region of Barcelona (Spain). Diagnosis of BPD was made by means of the Structured Clinical Interview for Axis II personality disorders (SCID-II; [61]), the DSM-IV, the Diagnostic Interview for Borderlines-Revised [62] and the Mclean Screening Instrument for BPD (MSI-BPD;[63]). The presence of brain injury, psychotic, bipolar or current major depressive disorders and drug abuse were all exclusion criteria for this group. The healthy control group consisted of 23 healthy participants (HC group), who were recruited via local advertisement and did not have any past or current mental disorders. The recruitment of this group was important in order to ensure that STD group was subclinical (see Table S1).
The three groups were matched by sex, such that participants in all groups were mostly females (BPD = 90%, STD = 84.2%, and HC =86.4%). However, the three groups showed differences in age (F (2,60) = 4.82, P < 0.05; BPD: M = 23.62, SD = 5.13; STD: M = 19.74, SD = 1.55; HC: M = 22.65, SD = 4.43), such that participants in the STD group were significantly younger than participants in the BPD and HC groups. Lastly, participants in the three groups did not show differences in education (F (2,54) = 2.51, P = 0.09; BPD: M = 12.82, SD = 1.87; STD: M = 12.89, SD = 1.04; HC: M = 14.14, SD = 2.81) or active employment (χ2 = 1.55, P = 0.45; BPD = 29.4%; STD = 42.1%; HC = 28.6%).
Procedures
The current study is part of a larger project, for which participants received an economic compensation of €45–60. All procedures were approved by the local ethical committee and written informed consent was obtained from all participants.
The STD group resulted from a mass assessment of 180 students. At first, they completed a brief assessment including sociodemographic and clinical data, as well as a screening of NSSI (using the Inventory of Statements about Self-Injury, see supporting information). Then, researchers contacted students who reported more than 5 NSSI acts in the previous 12 months and invited them to take part in the second part of the research (i.e., the current study). Out of the 180 initially recruited students, only 19 qualified for the current study.
All participants (STD, BPD, and HC groups) completed a clinical and self-report assessment in facilities at the Hospital of Igualada. In this session, participants also downloaded the Sinjur App on their phone and were trained in its use. They were instructed to use the App at least three times per day during the next 15 days. As a reminder, participants received three random prompts (in the interval from 8 a.m. to 8 p.m.), and they were instructed to complete the app as soon as they received each prompt. In addition to the three random prompts, they were also instructed to use the app if they engaged in self-injury. Therefore, the sampling scheme was both signal-contingent (3 random prompts per day) and event-contingent (participants self-initiated these prompts to provide a report after an NSSI episode).
Instruments
Self-Reported Measures
Depression, Anxiety and Stress Scale (DASS-21)
DASS-21 was used to assess negative emotional symptoms during the two weeks preceding the study period [64]. These symptoms are grouped in three subscales: (i) depression, (ii) anxiety, and (iii) stress. The Spanish version shows high internal reliability in the three scales (Cronbach’s α = 0.84, 0.70 and 0.82) [54].
Experiences Questionnaire (EQ)
The EQ-Decentering scale [55] was designed to measure a metacognitive skill in the week prior to the study, namely the ability to decenter oneself from undesired internal events and the capacity to observe one’s thoughts and emotions in a detached manner, as if they were transient events of the mind [54]. The Spanish version shows good internal reliability (Cronbach’s α = .89) [60] in the current sample.
Brief Version of the Difficulties in Emotion Regulation Scale (DERS-18)
We used the Spanish translation of DERS-18 to assess the self-perception of long-lasting difficulties in emotion regulation. It consists of six dimensions: (i) lack of emotional awareness, (ii) lack of emotional clarity, (iii) nonacceptance of emotions, (iv) inability to engage in goal-directed behavior when experiencing intense emotional states, (v) engagement in impulsive behavior when feeling emotional, and (vi) inability to access emotion regulation strategies. It is an abbreviated version of the original 36-items measure [65]. The DERS-18 shows a high internal consistency (Cronbach’s α = .91) and the 6 scales present moderate to high internal consistency (Cronbach’s α = .77 to .90) [66]. For the purpose of the current study, we used the total DERS-18 score to measure emotion dysregulation.
Borderline Personality Questionnaire (BPQ)
We used the BPQ to assess BPD traits according to the DSM-IV criteria [67]. BPQ has a total of 80 items with a dichotomous response format (True/False). BPQ shows adequate psychometric properties and has been effective at detecting BPD in young populations [67,68,69]. In the Spanish version, the internal reliability across the 9 scales was moderate to high (Cronbach’s α = .78 to .93) [69]. Here, we used a 3-factor model that includes the 9 scales of BPQ [13, 70]. They were: (i) affective dysregulation (which includes affective instability, abandonment, and intense anger); (ii) disturbed relatedness (including relationship, self-image, emptiness, and quasi-psychotic states); and (iii) behavioral dysregulation (includes impulsivity). The suicidal/self-harm scale (included originally in the behavioral dysregulation factor) was excluded in the current study due to potential confounding effects.
EMA Measures
The Sinjur App was developed to evaluate emotionality and NSSI according to the Experience Sampling Method [71]. The app was designed to assess a variety of emotional states and dysfunctional behaviours (see Supporting Information for more detail), but for the purpose of the current study, we will focus on momentary negative affect, interpersonal conflicts, and NSSI episodes. At each measurement occasion, participants were asked to indicate their momentary negative affect by: (a) choosing from a list of emotions such as anger, guilt, frustration, and sadness (see Table S2), and (b) rating the intensity of these emotions from 0 (lowest) to 100 (highest). They were also asked to indicate: (c) the number of times they engaged in discussions or arguments with others, and (d) whether they engaged in NSSI (yes/no) since the last measurement occasion.
In this latter section, when affirmative, participants were asked about the frequency (how many times they engaged in NSSI since the last assessment), and also about the method and function [72]; see Supporting information].
Data Analysis
Descriptive Analysis
For the analysis, we used R [73] and IBM SPSS v.21 [74]. First, we conducted a descriptive analysis of self-report data (see Table S1). Second, we performed a descriptive analysis of compliance and use of EMA instrument. There were 2131 valid assessment entries across the 64 participants of the sample, and overall compliance was sufficiently high: 79.9% (99.9% in HC, 60.53% in STD group, and 73.7% in BPD group). Importantly, 145 NSSI episodes were recorded during the study period, and the most common NSSI method among patients with BPD was self-cutting (45.5%), followed by banging or burning oneself. Conversely, for STD participants, self-cutting was a less commonly reported NSSI method (17.9%, χ2 = 6.12, P = 0.013), suggesting that students commonly engage in milder forms of NSSI, whereas BPD patients engage in potentially more severe NSSI. Additionally, the majority of participants with NSSI (BPD and STD groups) reported engaging in self-injury with intrapersonal rather than interpersonal motivations (91.8% vs. 8.2%; χ2 = 50.97, P < 0.001).
Multilevel Analysis
Given the nature of the EMA approach, NSSI engagement was determined by factors on four different levels, ranging from the time and day of measurement to the individual (participant) and group level (BPD, STD, HC). Since the relationship between the predictors and the response was measured at different hierarchical levels, we employed a multilevel mixed-effect regression analysis. As suggested by Santangelo et al. [75], the time intervals between the entries may vary between participants and must be accounted for in the model. In our study, time was included as an ordinal random effect to control for potentially varying time intervals between entries on the same day.
A Binary Logistic Generalized Linear Model with Mixed Effects [GLMM] [76] was used to determine the predictive capacity of the variables captured by EMA and self-reports (see Table S2) on NSSI engagement. Models were built and tested using the lme4 package in R [76], starting with a null model including only random effects, and systematically incorporating more predictors until we obtained the best model. Multicollinearity of the predictors was tested in each designed model, using the mer-utils R code [77], and variance explained by each model was estimated using the Pseudo-R-squared for generalized mixed-effect model statistics [78]. Given the nature of the response variable (binominal distribution of responses), a theoretical method of variance was used, included in the MuMIn package in R [79]. Finally, statistical power and effect sizes were estimated using the PowerSIM estimation, in the simr R package [80].
The dataset consisted of both psychometric (e.g., BPQ and DASS-21 scores) and EMA data for each participant. The latter was extracted from the Sinjur App: day, time, and part of day associated with each observation, presence and intensity of negative emotions preceding NSSI (sadness, frustration, sadness, among others), number of discussions or arguments with others, and number of self-injurious behaviours.
To structure the dataset, we defined the time range, the daytime range, and the response variable for each observation. The time range for each observation was 15 min, the daytime range was between 06:00 am until 05:59 am of the next day, and the response for each observation was coded as a binary variable (No self-injury = 0; self-injury = 1). Therefore, the observations structure was defined by subject, day, and time, and the random-effect structure consisted of a four-level model with level 1 = time, level 2 = day, level 3 = subject, and level 4 = group (HC, STD, BPD).
To minimize differences in the measurement scales [76], self-report affectivity and psychometric measures were centred by using the sample average as a common baseline value; since the affective and psychometric variables do not have a natural zero point, they were centred so that the zero point would be the sample average. Therefore, the scores analysed in the model represent the difference between the given observation and the mean of the corresponding variable for the total sample.
In order to extrapolate the results of the aforementioned model, we classified responses as predicted or observed. In order to determine the optimal cut-off point for the appropriate classification, we used the Youden Index [J] method and the balance between specificity and sensitivity [81, 82]; while sensitivity refers to the probability that the model predicts a true positive, specificity refers to the probability that the model predicts a true negative [83, 84]. After computing the sensitivity and specificity indices, we employed the Youden Index (J) formula to estimate the balance of sensitivity and specificity:
According to this index (J), the optimal cut-off for classifying a response as predicted or observed is the one that presents a specificity and sensitivity greater than or equal to 62,5% [85], ideally ≥75%. Alternatively, the optimal cut-off could also be determined by trial-and-error, until we obtain the highest J index that maintains the number of prediction errors low (PE) [81, 83]; the latter is calculated by the following formula:
Results
Multilevel Analysis
Null Model
A GLMM was computed to analyse the binary response variable at the different hierarchical levels of the data (e.g. participant, day, time, group). The null model revealed a significant effect of group on the intercept parameter, as well as variance attributable to the different random effects (see Table 1). Therefore, the initial random effects model was reserved for comparison with the complete model that includes both random and fixed effects, where the latter refers to direct predictors of the response variable and interactions among predictors [86].
Final Model of NSSI
The final model selected to predict the response variable (NSSI) is shown in Table 2. The random effects demonstrate the variance explained by time, day, participant, and group, that is, the four hierarchical levels that define the multilevel data structure.
On the other hand, fixed effect analyses show that the intercept for each group is significantly different from zero and different for each group. Specifically, the estimated intercept was −3.245 for the HC group, −3.234 for the STD group, and − 3.195 for the BPD group. Evidently, the BPD group has the highest predisposition to engage in self-injury, while the HC group has the lowest. This finding suggests that predisposition to engage in NSSI varies as a function of the presence or absence of a BPD diagnosis.
Regarding the fixed effects of the momentary emotions measured by EMA, frustration was the only type of negative affect that directly predicted NSSI engagement. Contrary to our hypotheses, momentary emotions of intense guilt and sadness did not present a significant direct effect on NSSI engagement, and momentary emotions of intense anger presented an inverse, that is, a risk-reducing rather than a risk-enhancing effect, on the probability of engaging in NSSI.
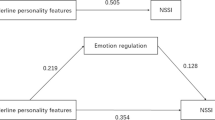
Importantly, as evidenced by the significant interactions between EMA and self-report variables, the effect of each momentary negative emotion on NSSI was moderated by psychometric measures (indicators of more stable affective states) such as symptoms of depression, anxiety, and stress (DASS-21), borderline pathology (BPQ Affective dysregulation), and decentering capacity (EQ). Specifically, the effect of momentary anger on NSSI was moderated by DASS-21, BPQ- Affect dysregulation, and EQ, such that higher scores on these measures facilitated a risk-enhancing effect of momentary anger on NSSI engagement. In addition, the effects of momentary guilt and frustration on NSSI were differentially moderated by DASS-21; while the interaction between momentary emotions of guilt and DASS-21 exerted a risk-enhancing effect on NSSI, the interaction between momentary frustration and DASS-21 exerted a risk-reducing effect on NSSI. Most importantly, the effect of intense, momentary sadness on NSSI was moderated by EQ, consistent with our prediction that greater decentering capacity would attenuate the effects of negative affectivity on NSSI.
Finally, regarding the interpersonal conflicts captured by EMA, the multilevel results revealed a significant risk-enhancing effect of discussions on NSSI engagement, lending support to the interpersonal functions of NSSI.
Utility and Predictive Reliability of the Final Model
To evaluate the utility of the proposed model, we followed two steps of analyses: 1) we compared the model fit parameters between the null and final model, and, 2) we calculated the proportion of explained variance in each model.
Results of the model fit parameters showed that relative to the null model, the final model exhibited significantly better parameters of model fit (AIC = 578.12; F (37, 15) = 135.53, P < 0.001), suggesting that the final model is better adjusted than the null model.
Regarding the proportion of explained variance, we employed the theoretical method of computing the R2 in order to calculate the proportion of variance explained by marginal (only fixed effects) and conditional effects (both fixed and random effects). Correspondingly, results showed that the proportion of variance explained by the marginal estimation (only including the fixed effects) was R2m = 0.056, while the variance explained by the conditional estimation (complete model including both random and fixed effects) was R2c = 0.923. Evidently, the complete model explains more than 92% of the total variance, which suggests that the proposed multilevel model has a high predictive capacity.
To determine the predictive reliability of the final multilevel model, we used a cut-off point to classify predicted and observed values, and we used the Youden Index [J] to estimate the balance between specificity and sensitivity (see Table 3). However, when we used the default cut-off point to classify the data, the sensitivity of the model was below 15%, which suggests that the capacity of the model to predict a true positive was too low. Therefore, we proposed an alternative cut-off point, which is 0.1. Compared to the default cut-off, the new cut-off significantly improved the sensitivity of the model, yielding satisfactory levels of sensitivity and specificity, that is, greater than 62.5% (see Table 3; sensitivity = 67.46%; specificity = 91.24%. In turn, satisfactory levels of sensitivity and specificity yielded a higher Youden Index, and hence, a better balance between accurate predictions (true positives and true negatives) and prediction error.
Discussion
The current study employed a multilevel approach, combining ecological momentary assessment (EMA) and self-report measures to explore potential risk and protective factors of NSSI. Overall, results from the multilevel analysis were partially consistent with our hypotheses. While only intense, momentary frustration directly predicted an increased probability of engaging in NSSI, momentary anger and guilt exerted a risk-enhancing effect when interacting with more stable traits of borderline pathology (BPQ) and symptoms of depression, anxiety, and stress (DASS-21). Importantly, greater decentering ability (EQ) predicted reduced likelihood of NSSI engagement, and momentary sadness exerted a risk-reducing effect when interacting with decentering ability (EQ). By highlighting the protective role of decentering in NSSI and its potential to attenuate the risk-enhancing effects of negative affectivity, the current study contributes novel findings that may have unique implications for NSSI treatment.
In the current sample, momentary frustration was the only type of negative affect that significantly predicted NSSI engagement. This finding is coherent with prior literature reporting that high-arousal negative affect-states (e.g. feeling frustrated) may lead to higher urgency of NSSI, compared to low-arousal negative affect-states (e.g. feeling sad) [39]. Frustration is conceptualized as a negative emotional response triggered after the omission and/or devaluation of an expected reward [87], and it is closely associated with aggression [88]. Prior studies report that feeling “frustrated” is an emotional state that precedes self-injury and diminishes after self-injury [29]. Empirical evidence shows that a painful stimulus (analogue to NSSI) is effective at reducing a state of frustration provoked by a stress induction task in people who self-injure [35]. According to our results, the risk-enhancing effect of frustration on NSSI engagement is attenuated in the context of current emotional distress (i.e., interaction between momentary frustration and DASS-21). This may suggest that participants with low levels of anxiety and depression might be more susceptible to the arousing effects of momentary states of frustration.
Contrary to our hypotheses, momentary anger predicted lower likelihood of NSSI engagement. This protective effect is largely inconsistent with prior research reporting that anger precedes NSSI [31, 42]. Nonetheless, a recent EMA study found that aggressive urges did not predict NSSI behaviour [89] and another study found that trait anger exhibited a negative suppression effect on the frequency of non-hitting NSSI, suggesting that when individuals engage in self-injury to relieve anger, they might choose more violent, hitting forms of NSSI rather than self-cutting [90]. The current sample (both BPD and STD groups) primarily engaged in self-cutting rather than hitting, which might explain the reduced likelihood of NSSI as a function of anger. Importantly, while anger might exert a protective effect against non-hitting NSSI, this effect is mitigated at higher levels of internalizing tendencies (as assessed by the DASS-21). Indeed, the multilevel analysis showed that when momentary anger interacted with the DASS-21, or with trait affective instability (BPQ) or with decentering (EQ), there was an increased probability of engaging in NSSI. Although the latter finding may seem contradictory (anger X EQ interaction), it could reflect that greater decentering capacity may help modulate low-arousal emotions (e.g. sadness) associated with depression [56], but not high-arousal emotions such as anger.
Interestingly, sadness and guilt did not predict NSSI engagement by themselves, but they did so when interacting with other variables. Current results show that levels of emotional distress (assessed by DASS-21) interacted with momentary emotions of guilt to significantly predict NSSI. This finding is consistent with prior literature which suggests that while guilt proneness is not associated with an increased risk for NSSI, this protective effect is attenuated when individuals are overwhelmed by increased internalizing tendencies [91]. Given that individuals who engage in self-injury retrospectively report feeling sadness prior to NSSI [39], the current null finding may initially appear surprising, however, it is somewhat consistent with prior literature which found that sadness interacted with other variables to predict NSSI. For example, Bresin and colleagues [92] found that sadness only predicted self-injurious urges in individuals with high scores in negative urgency (the tendency to engage in risky behaviours during periods of negative affect), but not for individuals scoring low in negative urgency [92].
In the current study, we found that momentary sadness interacted with decentering, such that individuals who experienced frequent and intense sadness were less likely to engage in NSSI if their capacity of decentering was high. These results are congruent with previous EMA studies showing that higher decentering attenuates the association between negative affect and mental health outcomes [56], whereas higher rumination, the conceptual opposite of decentering [93], enhances or exacerbates the effect of negative affectivity on the likelihood of NSSI engagement [94]. In addition to moderating the relationship between momentary sadness and NSSI, decentering also exhibited a risk-reducing or protective effect on NSSI by itself. While this is the first study to directly explore the relationship between decentering and NSSI, our findings are coherent with prior research associating decentering with reduced symptom severity in BPD ([57, 95]. By promoting a detached, observer perspective on one’s internal experiences [54], decentering may encourage disidentification from habitual maladaptive thought patterns, lowering emotional reactivity [96, 97].
In the social field, the multilevel analysis revealed that the number of interpersonal discussions or conflicts significantly predicted NSSI engagement. This finding complements prior diary studies reporting that participants were more likely to engage in self-injurious acts on the days when they experienced interpersonal conflicts with loved ones [47] and it coheres with prior self-report studies identifying interpersonal conflicts as a common trigger for NSSI [13]. While individuals who engage in self-injury may find it difficult to explicitly recognize social motives for engagement in NSSI when using EMA [44, 46, 53], the risk-enhancing effect of interpersonal discussions (captured by EMA) on NSSI engagement may reveal an inferred or implicit interpersonal motive for NSSI, lending support to the interpersonal functions of NSSI (e.g. communicating distress: [24]).
Conversely, disturbed relatedness BPQ-factor, a measure of impaired social cognition in BPD, was negatively associated with NSSI. These findings may be accounted for by prior research suggesting that affective dysregulation is more associated with the intrapersonal functions of NSSI, while disturbed relatedness is more associated with the interpersonal functions of NSSI [13]. Therefore, it is possible that disturbed relatedness was negatively associated with NSSI because most of the current sample reported engaging in NSSI with an intrapersonal rather than an interpersonal motivation.
Strengths and Limitations
Innovatively, we recruited both a clinical group of BPD patients with NSSI and a subclinical group of students with NSSI in order to address the increasing prevalence of NSSI among young adults in community samples [2,3,4,5] and make results generalizable to both clinical and non-clinical populations. By combining a “real-time” measure of NSSI and negative affect with self-report measures, this study identifies reliable risk and protective factors of NSSI and proposes strategies to modify worrisome dysfunction. Most importantly, the current study contributes novel knowledge about NSSI that may help refine prevention and treatment strategies to ameliorate the growing prevalence of self-injury in both clinical and community populations. For the first time to our knowledge, the current study identified decentering, a metacognitive emotion regulation skill, as a protective factor that may attenuate the risk-enhancing effects of negative affectivity on NSSI.
Despite such promising findings, results are limited by several factors that need to be addressed. Firstly, the sample size was relatively small, and participants were not matched by age. Also, females were overrepresented in the current sample, which limits generalization of our results to populations with mixed gender. Secondly, and perhaps more importantly, the within-day sampling frequency in the current study was too low (3 entries/day) and the time interval between entries was too long, compared to recently published EMA studies [49, 75]. Given that NSSI is an impulsive behaviour characterized by short-term action, a higher sampling frequency would have been more optimal to capture short-lived dynamics, that is, the antecedents and consequences surrounding NSSI acts [75]. However, in addition to differences in sampling rate, it may be worth noting that Santangelo et al. [75] explored a wide range of dysfunctional behaviours (e.g. NSSI, binge-eating, promiscuous sex) over a smaller study period (4 days), whereas the current study solely focused on NSSI occurrences over a larger study period (15 days). Narrowing dysfunctional behaviours to NSSI may partly explain the significantly smaller number of observations that limit the conclusions drawn from our study.
In addition, while we instructed participants to respond to the prompts immediately, some participants may have responded in a delayed manner, giving the data a rather retrospective than real-time nature, which may also compromise the accuracy of our results. Lastly, since differentiating emotions is characteristically challenging both for people who engage in self-injury [98] and for adults with BPD [99, 100], findings regarding the role of specific emotions on NSSI are preliminary and should be confirmed by future research. Difficulties with identifying and differentiating emotions may have also interfered with the participants´ ability to answer questions regarding their own emotion regulation difficulties [101], which may partly explain the absence of a significant relationship between emotion dysregulation (measured by DERS-18) and NSSI. Another possible explanation for this null finding is that we used the DERS-18 total score, whereas recent meta-analytic findings suggest that specific dimensions of emotion dysregulation (e.g. lack of emotion regulation strategies and non-acceptance of emotions) may be more robustly associated with NSSI than the other dimensions (e.g. [15, 101].
Conclusions
The current findings have several clinical implications. The predictive model of NSSI may be useful in preventing NSSI in both clinical and non-clinical samples. Given that NSSI has been proposed as an early behavioural indicator of emotion dysregulation in the developmental trajectory to BPD, early interventions with ‘at risk’ young individuals might be considered [11, 12]. Given the protective role of decentering in NSSI, our findings support interventions aimed to improve emotion-regulation and mindfulness skills (e.g., dialectical behavioural therapy) [102], with an emphasis on those improving decentering capacity (i.e., mindfulness-based therapies).
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APD:
-
Avoidant Personality Disorder
- BPD:
-
Borderline Personality Disorder
- BPQ:
-
Borderline Personality Questionnaire
- DASS-21:
-
Depression, Anxiety, and Stress Scale
- DERS:
-
Difficulties in Emotion Regulation Scale
- DSM:
-
Diagnostic and Statistical Manual for Mental Disorders
- EMA:
-
Ecological Momentary Assessment
- EQ:
-
Experiences Questionnaire (constitutes a measure of decentering)
- GLMM:
-
Generalized Linear Model with Mixed Effects
- HC:
-
Healthy Control Group
- NSSI:
-
Non- Suicidal Self-Injury
- STD:
-
Student Group
References
Nock MK. Self-injury. Annu Rev Clin Psychol. 2010;6:339–63.
Lim KS, Wong CH, McIntyre RS, Wang J, Zhang Z, Tran BX, et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health. 2019;16(22):4581.
Vega D, Sintes A, Fernández M, Puntí J, Soler J, Santamarina P, et al. Review and update on non-suicidal self-injury: who, how and why? Actas Españolas Psiquiatr. 2018;46(4):146–55.
Wester K, Trepal H, King K. Nonsuicidal self-injury: increased prevalence in engagement. Suicide Life-Threatening Behav. 2018;48(6):690–8.
Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life-Threatening Behav. 2014;44(3):273–303.
Kiekens G, Claes L, Demyttenaere K, Auerbach RP, Green JG, Kessler RC, et al. Lifetime and 12-month nonsuicidal self-injury and academic performance in college freshmen. Suicide Life Threat Behav. 2016;46(5):563–76.
Bentley KH, Cassiello-Robbins CF, Vittorio L, Sauer-Zavala S, Barlow DH. The association between nonsuicidal self-injury and the emotional disorders: a meta-analytic review. Clin Psychol Rev. 2015;37:72–88.
Klonsky DE, May AM, Glenn CR. The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. J Abnorm Psychol. 2013;122(1):231–7.
Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. 2016;46(2):225–36.
APA. Diagnostic and statistical manual of mental disorders (5th ed.). Author. Washington, DC; 2013.
Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: elaborating and extending linehan’s theory. Psychol Bull. 2009;135(3):495–510.
Ghinea D, Koenig J, Parzer P, Brunner R, Carli V, Hoven CW, et al. Longitudinal development of risk-taking and self-injurious behavior in association with late adolescent borderline personality disorder symptoms. Psychiatry Res. 2019;273:127–33.
Vega D, Torrubia R, Soto À, Ribas J, Soler J, Pascual JC, et al. Exploring the relationship between non suicidal self-injury and borderline personality traits in young adults. Psychiatry Res. 2017 Oct 1;256:403–11.
Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet. 2004;364(9432):453–61.
Wolff JC, Thompson E, Thomas SA, Nesi J, Bettis AH, Ransford B, et al. Emotion dysregulation and non-suicidal self-injury: a systematic review and meta-analysis. Eur Psychiatry. 2019;59:25–36.
Linehan MM. Dialectical behavior therapy for borderline personality disorder: theory and method. Bull Menn Clin. 1987;51(3):261–76.
Dixon-Gordon KL, Chapman AL, Lovasz N, Walters K. Too upset to think: The interplay of borderline personality features, negative emotions, and social problem solving in the laboratory. Personal Disord Theory, Res Treat. 2011;2(4):243.
Ebner-Priemer UW, Badeck S, Beckmann C, Wagner A, Feige B, Weiss I, et al. Affective dysregulation and dissociative experience in female patients with borderline personality disorder: a startle response study. J Psychiatr Res. 2005;39(1):85–92.
Kuo JR, Linehan MM. Disentangling emotion processes in borderline personality disorder: physiological and self-reported assessment of biological vulnerability, baseline intensity, and reactivity to emotionally evocative stimuli. J Abnorm Psychol. 2009;118(3):531–44.
Nock MK, Prinstein MJ. A functional approach to the assessment of self-mutilative behavior. J Consult Clin Psychol. 2004;72(5):885–90.
Hamza CA, Willoughby T. Nonsuicidal self-injury and affect regulation: recent findings from experimental and ecological momentary assessment studies and future directions. J Clin Psychol. 2015 Jun 1;71(6):561–74.
Hasking P, Whitlock J, Voon D, Rose A. A cognitive-emotional model of NSSI: using emotion regulation and cognitive processes to explain why people self-injure. Cogn Emot. 2017 Nov 17;31(8):1543–56.
Klonsky ED. The functions of deliberate self-injury: a review of the evidence. Clin Psychol Rev. 2007;27(2):226–39.
Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, Dickson JM. A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J Affect Disord. 2018;227:759–69.
Victor SE, Klonsky ED. Daily emotion in non-suicidal self-injury. J Clin Psychol. 2014;70(4):364–75.
Allroggen M, Kleinrahm R, Rau TAD, Weninger L, Ludolph AG, Plener PL. Nonsuicidal Self-Injury and Its Relation to Personality Traits in Medical Students. J Nerv Ment Dis. 2014;202(4).
Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate self-harm in a nonclinical population: prevalence and psychological correlates. Am J Psychiatry. 2003 Aug 1;160(8):1501–8.
Selby EA, Franklin J, Carson-Wong A, Rizvi SL. Emotional cascades and self-injury: investigating instability of rumination and negative emotion. J Clin Psychol. 2013;69(12):1213–27.
Laye-Gindhu A, Schonert-Reichl KA. Nonsuicidal self-harm among community adolescents: understanding the “Whats” and “whys” of self-harm. J Youth Adolesc. 2005;34(5):447–57.
St. Germain SA, Hooley JM. Direct and indirect forms of non-suicidal self-injury: evidence for a distinction. Psychiatry Res. 2012;197(1):78–84.
Claes L, Klonsky ED, Muehlenkamp J, Kuppens P, Vandereycken W. The affect-regulation function of nonsuicidal self-injury in eating-disordered patients: which affect states are regulated? Compr Psychiatry. 2010;51(4):386–92.
Kamphuis JH, Ruyling SB, Reijntjes AH. Testing the Emotion Regulation Hypothesis Among Self-Injuring Females: Evidence for Differences Across Mood States. J Nerv Ment Dis, 2007;195(11).
Kleindienst N, Bohus M, Ludäscher P, Limberger MF, Kuenkele K, Ebner-Priemer UW, et al. Motives for Nonsuicidal Self-Injury Among Women With Borderline Personality Disorder. J Nerv Ment Dis. 2008;196(3).
Reitz S, Krause-Utz A, Pogatzki-Zahn EM, Ebner-Priemer U, Bohus M, Schmahl C. Stress regulation and incision in borderline personality disorder—a pilot study modeling cutting behavior. J Personal Disord. 2012;26(4):605–15.
Reitz S, Kluetsch R, Niedtfeld I, Knorz T, Lis S, Paret C, et al. Incision and stress regulation in borderline personality disorder: neurobiological mechanisms of self-injurious behaviour. Br J Psychiatry. 2015;207(2):165–72.
Klonsky ED, Glenn CR, Styer DM, Olino TM, Washburn JJ. The functions of nonsuicidal self-injury: converging evidence for a two-factor structure. Child Adolesc Psychiatry Ment Health. 2015;9(1):1–9.
Turner BJ, Chapman AL, Layden BK. Intrapersonal and interpersonal functions of non suicidal self-injury: associations with emotional and social functioning. Suicide Life-Threatening Behav. 2012 Feb 1;42(1):36–55.
Klonsky ED. Non-suicidal self-injury: an introduction. J Clin Psychol. 2007 Nov 1;63(11):1039–43.
Klonsky ED. The functions of self-injury in young adults who cut themselves: clarifying the evidence for affect-regulation. Psychiatry Res. 2009;166(2):260–8.
Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32.
Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. Ecological momentary assessment of nonsuicidal self-injury in youth with borderline personality disorder. Personal Disord Theory, Res Treat. 2017;8(4):357.
Nock MK, Prinstein MJ, Sterba SK. Revealing the form and function of self-injurious thoughts and behaviors: a real-time ecological assessment study among adolescents and young adults. J Abnorm Psychol. 2009;118(4):816–27.
Shingleton RM, Eddy KT, Keshaviah A, Franko DL, Swanson SA, Yu JS, et al. Binge/purge thoughts in nonsuicidal self-injurious adolescents: an ecological momentary analysis. Int J Eat Disord. 2013;46(7):684–9.
Rodríguez-Blanco L, Carballo JJ, Baca-García E. Use of ecological momentary assessment (EMA) in non-suicidal self-injury (NSSI): a systematic review. Psychiatry Res. 2018;263:212–9.
Santangelo PS, Koenig J, Funke V, Parzer P, Resch F, Ebner-Priemer UW, et al. Ecological momentary assessment of affective and interpersonal instability in adolescent non-suicidal self-injury. J Abnorm Child Psychol. 2017;45(7):1429–38.
Snir A, Rafaeli E, Gadassi R, Berenson K, Downey G. Explicit and inferred motives for nonsuicidal self-injurious acts and urges in borderline and avoidant personality disorders. Personal Disord. 2015;6(3):267–77.
Turner BJ, Cobb RJ, Gratz KL, Chapman AL. The role of interpersonal conflict and perceived social support in nonsuicidal self-injury in daily life. J Abnorm Psychol. 2016;125(4):588–98.
Hepp J, Carpenter RW, Freeman LK, Vebares TJ, Trull TJ. The environmental, interpersonal, and affective context of nonsuicidal self-injury urges in daily life [published online ahead of print, 2020 Sep 3]. Personal Disord. 2020. https://doi.org/10.1037/per0000456.
Fitzpatrick S, Kranzler A, Fehling K, Lindqvist J, Selby E. Investigating the role of the intensity and duration of self-injury thoughts in self-injury with ecological momentary assessment. Psychiatry Res. 2020;112761.
Anestis MD, Silva C, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, et al. Predicting nonsuicidal self-injury episodes over a discrete period of time in a sample of women diagnosed with bulimia nervosa: an analysis of self-reported trait and ecological momentary assessment based affective lability and previous suicide attempts. Int J Eat Disord. 2012;45(6):808–11.
Armey MF, Crowther JH, Miller IW. Changes in ecological momentary assessment reported affect associated with episodes of nonsuicidal self-injury. Behav Ther. 2011;42(4):579–88.
Muehlenkamp JJ, Engel SG, Wadeson A, Crosby RD, Wonderlich SA, Simonich H, et al. Emotional states preceding and following acts of non-suicidal self-injury in bulimia nervosa patients. Behav Res Ther. 2009;47(1):83–7.
Andrewes HE, Hulbert C, Cotton SM, Betts J, Chanen AM. An ecological momentary assessment investigation of complex and conflicting emotions in youth with borderline personality disorder. Psychiatry Res. 2017;252:102–10.
Safran JD, Segal ZV. Cognitive therapy: an interpersonal process perspective. New York Basic. 1990.
Fresco DM, Moore MT, van Dulmen MHM, Segal ZV, Ma SH, Teasdale JD, et al. Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behav Ther. 2007;38(3):234–46.
Naragon-Gainey K, DeMarree KG. Structure and validity of measures of decentering and defusion. Psychol Assess. 2017;29(7):935–54.
O’Toole MS, Renna ME, Mennin DS, Fresco DM. Changes in decentering and reappraisal temporally precede symptom reduction during emotion regulation therapy for generalized anxiety disorder with and without co-occurring depression. Behav Ther. 2019;50(6):1042–52.
Kobayashi R, Shigematsu J, Miyatani M, Nakao T. Cognitive reappraisal facilitates decentering: a longitudinal cross-lagged analysis study. Front Psychol. 2020;11:103.
Hayes-Skelton S, Graham J. Decentering as a common link among mindfulness, cognitive reappraisal, and social anxiety. Behav Cogn Psychother. 2013;41(3):317–28.
Soler J, Franquesa A, Feliu-Soler A, Cebolla A, García-Campayo J, Tejedor R, et al. Assessing decentering: validation, psychometric properties, and clinical usefulness of the experiences questionnaire in a Spanish sample. Behav Ther. 2014;45(6):863–71.
First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured clinical interview for DSM-IV Axis II personality disorders, (SCID-II). Washington, D.C.: American Psychiatric Press, Inc.; 1997.
Barrachina J, Soler J, Campins MJ, Tejero A, Pascual JC, Alvarez E, et al. Validación de la versión española de la diagnostic interview for borderlines-revised (DIB-R). Actas Esp Psiquiatr. 2004;32(5):293–8.
Soler J, Domínguez-Clavé E, García-Rizo C, Vega D, Elices M, Martín-Blanco A, et al. Validation of the Spanish version of the McLean screening instrument for borderline personality disorder. Rev Psiquiatr y Salud Ment. 2016;9(4):195–202.
Bados A, Solanas A, Andrés R. Psychometric properties of the Spanish version of depression, anxiety and stress scales (DASS). Psicothema. 2005;17(4):679–83.
Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26(1):41–54.
Victor SE, Klonsky ED. Validation of a brief version of the difficulties in emotion regulation scale (DERS-18) in five samples. J Psychopathol Behav Assess. 2016;38(4):582–9.
Poreh AM, Rawlings D, Claridge G, Freeman JL, Faulkner C, Shelton C. The BPQ: a scale for the assessment of borderline personality based on DSM-IV criteria. J Personal Disord. 2006;20(3):247–60.
Chanen AM, Jovev M, Djaja D, McDougall E, Yuen HP, Rawlings D, et al. Screening for borderline personality disorder in outpatient youth. J Personal Disord. 2008;22(4):353–64.
Fonseca-Pedrero E, Paino M, Lemos-Giráldez S, Sierra-Baigrie S, González MPG-P, Bobes J, et al. Borderline personality traits in nonclinical young adults. J Personal Disord. 2011;25(4):542–56.
Sanislow CA, Grilo CM, McGlashan TH. Factor analysis of the DSM-III-R borderline personality disorder criteria in psychiatric inpatients. Am J Psychiatry. 2000;157(10):1629–33.
Larson R, Csikszentmihalyi M. The experience sampling method. In: Flow and the foundations of positive psychology. Springer; 2014. p. 21–34.
Klonsky ED, Glenn CR. Assessing the functions of non-suicidal self-injury: psychometric properties of the inventory of statements about self-injury (ISAS). J Psychopathol Behav Assess. 2009;31(3):215–9.
Team RC. R Foundation for Statistical Computing; Vienna, Austria: 2015. R A Lang Environ Stat Comput. 2018;2013.
IBM. SPSS Inc. PASW Stat Wind Chicago, SPSS Inc ReleasedVersion. 2009;21:18.
Santangelo PS, Holtmann J, Hosoya G, Bohus M, Kockler TD, Koudela-Hamila S, et al. Within- and between-persons effects of self-esteem and affective state as antecedents and consequences of dysfunctional behaviors in the everyday lives of patients with borderline personality disorder. Clin Psychol Sci. 2020;8(3):428–49.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. arXiv Prepr arXiv14065823. 2014.
Nakagawa S, Johnson PCD, Schielzeth H. The coefficient of determination R 2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface. 2017;14(134):20170213.
Barton K. MuMIn: Multi-Model Inference. R package version 1.43. 6. 2019.
Green P, MacLeod CJ. SIMR: an R package for power analysis of generalized linear mixed models by simulation. Methods Ecol Evol. 2016;7(4):493–8.
Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biometrical J J Math Methods Biosci. 2008;50(3):419–30.
Fluss R, Faraggi D, Reiser B. Estimation of the Youden index and its associated cutoff point. Biometrical J J Math Methods Biosci. 2005;47(4):458–72.
Fuentes LE. Methodology for the selection of optimal cutoff point to dichotomize continuous covariates. Rev Cuba Genética Comunitaria. 2013;7(3):36–42.
Dreiseitl S, Ohno-Machado L. Logistic regression and artificial neural network classification models: a methodology review. J Biomed Inform. 2002;35(5–6):352–9.
Rial A, Varela J. Regresión Logística. In Estadística Práctica para la Investigación en Ciencias de la Salud (pp.223–246). Netbiblo; 2008.
Forster M, Sober E. How to tell when simpler, more unified, or less ad hoc theories will provide more accurate predictions. Br J Philos Sci. 1994;45(1):1–35.
Amsel A. Frustration theory: many years later. Psychol Bull. 1992;112(3):396–9.
Dollard J, Miller NE, Doob LW, Mowrer OH, Sears RR. Frustration and aggression: Yale University Press; 1939.
Ammerman BA, Jacobucci R, Kleiman EM, Muehlenkamp JJ, McCloskey MS. Development and validation of empirically derived frequency criteria for NSSI disorder using exploratory data mining. Psychol Assess. 2017;29(2):221–31.
Kleiman EM, Ammerman BA, Kulper DA, Uyeji LL, Jenkins AL, McCloskey MS. Forms of non-suicidal self-injury as a function of trait aggression. Compr Psychiatry. 2015;59:21–7.
VanDerhei S, Rojahn J, Stuewig J, McKnight PE. The effect of shame-proneness, guilt-proneness, and internalizing tendencies on nonsuicidal self-injury. Suicide Life-Threatening Behav. 2014;44(3):317–30.
Bresin K, Carter DL, Gordon KH. The relationship between trait impulsivity, negative affective states, and urge for nonsuicidal self-injury: a daily diary study. Psychiatry Res. 2013;205(3):227–31.
Segal ZV, Teasdale JD, Williams JM, Gemar MC. The mindfulness-based cognitive therapy adherence scale: inter-rater reliability, adherence to protocol and treatment distinctiveness. Clin Psychol Psychother. 2002;9(2):131–8.
Nicolai KA, Wielgus MD, Mezulis A. Identifying risk for self-harm: rumination and negative affectivity in the prospective prediction of nonsuicidal self-injury. Suicide Life-Threatening Behav. 2016;46(2):223–33.
Elices M, Pascual JC, Portella MJ, Feliu-Soler A, Martín-Blanco A, Carmona C, et al. Impact of mindfulness training on borderline personality disorder: a randomized trial. Mindfulness. 2016;7(3):584–95.
Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco DM. Decentering and related constructs: a critical review and metacognitive processes model. Perspect Psychol Sci. 2015;10(5):599–617.
Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62(3):373–86.
Frank A. mer-utils.R. R code. 2011. https://github.com/aufrank/R-hacks/blob/master/mer-utils.R
Bresin K. Five indices of emotion regulation in participants with a history of nonsuicidal self-injury: a daily diary study. Behav Ther. 2014;45(1):56–66.
Suvak MK, Litz BT, Sloan DM, Zanarini MC, Barrett LF, Hofmann SG. Emotional granularity and borderline personality disorder. J Abnorm Psychol. 2011;120(2):414–26.
Zaki LF, Coifman KG, Rafaeli E, Berenson KR, Downey G. Emotion differentiation as a protective factor against nonsuicidal self-injury in borderline personality disorder. Behav Ther. 2013;44(3):529–40.
You J, Ren Y, Zhang X, Wu Z, Xu S, Lin M. Emotional Dysregulation and Nonsuicidal Self-Injury: A Meta-Analytic Review. Neuropsychiatry. 2018;08.
Linehan MM. Cognitive behavioural therapy of borderline personality disorder. New York Guilford. 1993.
Acknowledgments
The authors are grateful to all participants who made this study possible.
Authors´ Contributions
DV designed the study and developed the Sinjur App. JCP, JS and DV recruited patients and evaluated them. LB and DV recruited controls and students and evaluated them. IA, DV, LB, and CS analysed the data, and IA, DV, LB, CS, and SN interpreted the data. All authors contributed to writing the manuscript and all of them read and approved the final manuscript.
Funding
This research was supported by a Spanish government grant to DV (I + D + i fellowship, PSI2016–79980-P). LB, SN and DV were supported by the Catalan government with a PERIS fellowship, reference number SLT006/17/00159. IA and CS are supported by Chilean government by a Becas-Chile fellowship program by the National Agency for Research and Development (ANID), reference numbers 2015–72160105 and 2018–72190624, respectively.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the ethics committee of the Hospital Universitari de Bellvitge, Barcelona (protocol no. PR360/16).
Consent for Publication
Not applicable.
Competing Interests
Authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOC 54 kb)
Rights and permissions
About this article
Cite this article
Briones-Buixassa, L., Alí, Í., Schmidt, C. et al. Predicting Non-Suicidal Self-Injury in Young Adults with and without Borderline Personality Disorder: a Multilevel Approach Combining Ecological Momentary Assessment and Self-Report Measures. Psychiatr Q 92, 1035–1054 (2021). https://doi.org/10.1007/s11126-020-09875-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-020-09875-7