Abstract
Deliberate self-harm (DSH) is a public health problem that mainly affects adolescents and young adults. Evidence suggests that multiple methods are used with a self-aggressive intent. The present article focuses on the development and factorial validation of the Inventory of Deliberate Self-harm Behaviours for Portuguese adolescents. This instrument assesses the lifetime frequency of 13 DSH methods, with and without suicidal intent. Study 1 consisted of an exploratory factor analysis with a sample of 131 adolescents with a reported history of DSH. Results revealed a three-factor structure with acceptable internal consistency: High Severity DSH, Mild Severity DSH, and Substance Use DSH. After item reduction, this structure was tested in Study 2 through a confirmatory factor analysis with an independent sample of 109 adolescents also with a history of DSH. Results showed an acceptable model fit. This instrument presents a solid structure and acceptable psychometric properties, allowing its use in further research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deliberate self-harm (DSH) is a significant mental health issue among adolescents and young adults, and it is viewed as the result of a complex interplay of genetic, biological, psychiatric, psychological, social, and cultural factors [1]. The lifetime prevalence rates in population-based studies with adolescents range from 3% to 27.6% [2,3,4,5]. In Portugal, research that used convenience samples of adolescents concluded that DSH presented lifetime prevalence rates between 7.3% and 30% [6,7,8,9,10].
There are some divergences concerning the conceptualization of these behaviours, particularly about the presence of suicidal intent. The term DSH is frequently employed as a broad designation for self-injurious behaviours both with and without suicidal intent that have non-fatal outcomes [11]. Hence, in the present research, we follow this definition of DSH, which is in accordance with the Portuguese National Suicide Prevention Plan [12] and by other studies, namely the Child & Adolescent Self-harm in Europe (CASE) Study [3, 13].
DSH involves a multiplicity of possible methods used with self-aggressive intent. There are differences concerning the prevalence of methods, especially when comparing clinical and community samples. Research with clinical samples has shown that the most common methods include cutting, overdosing, burning, and strangulation [14]; cutting, scratching, and suffocation [15]; and banging/hitting self, cutting, scratching, and burning [16]. Studies that used community samples have concluded that the most frequent methods are cutting and overdosing [3]; cutting, scratching, and banging/hitting self [5, 17]; cutting and skin damaging through other means [2]; biting, scratching, and interfering with wound healing [18]. Some investigations carried out in Portugal concluded that the most common DSH methods are cutting, scratching, biting and banging/hitting self [6, 9, 19].
The methods used for DSH can also be categorized according to its severity. Although this categorization is not consensually described in the literature, the levels of severity are usually defined according to the degree of injury caused to the body tissue (e.g. [20,21,22]). Croyle and Waltz [20] described self-harm without conscious suicidal intent into two groups, namely mildly injurious self-harm behaviours (e.g. interfering with the healing of a wound, or scratching the skin severely enough to cause bleeding or scarring) and moderately injurious self-harm behaviours (e.g. burning or cutting). On the other hand, Whitlock et al. [22] defined three categories for non-suicidal self-injury (NSSI): superficial NSSI (i.e. behaviours with the potential for superficial tissue damage, such as scratching or intentionally preventing wounds from healing); moderate severity NSSI (i.e. behaviours likely to cause bruising or light tissue damage such as punching or banging oneself or other objects); and high severity NSSI (i.e. behaviours with the potential of severe tissue damage such as cutting, burning, or ingesting caustic substances). According to these categorizations, if DSH behaviours are viewed as part of a suicidal continuum [21, 23,24,25], we may consider suicide as the most extreme or severe DSH method.
Research has shown that the diversity and number of methods used for DSH are important factors for the assessment of this phenomenon. Studies concluded that using a large number of methods is associated with a greater psychological maladjustment of the individual [26], is positively correlated with suicidal ideation [27] and suicidal risk [22], and is also a predictor of suicide attempts [28, 29]. Furthermore, some individuals may engage in more lethal behaviours by engaging in increasingly severe DSH over time [23]. Hence, although DSH can be performed simultaneously through multiple self-aggressive methods (e.g. [30]), the categorization according to its severity is an important factor.
Some research also suggests that the DSH methods and their frequency can be associated with specific subgroups or classes of individuals that engage in self-harm [30,31,32,33,34,35,36,37]. According to Walsh [36], these individuals can be classified based on specific characteristics of DSH, including the frequency of the behaviour, methods used, and extent of damage caused by the act. As an example, the investigation conducted by Bjärehed et al. [31] identified three subgroups of adolescents who presented NSSI: (1) a large proportion of adolescents with low-frequency NSSI and little psychological difficulties; (2) a subgroup of adolescents with frequent and multi-faceted NSSI who showed both externalizing and internalizing problems; (3) a subgroup of girls with cutting as the main form of NSSI, and primarily internalizing problems. In another study, You et al. [37] found that repetitive NSSI was associated with more emotional and impulse-control problems than episodic NSSI, and that adolescents with severe NSSI were more impulsive than adolescents with mild NSSI. The types of DSH methods, as well as its association with clinical subgroups of individuals, may imply different psychotherapeutic and treatment approaches [22, 36].
The construction of instruments to assess DSH began in the 90’s and its development has accompanied the evolution of the conceptualizations and definitions of these behaviours [38]. There are several instruments which incorporate items that refer to DSH (e.g. [39, 40]) and instruments that focus exclusively on DSH (e.g. [41,42,43]). In Portugal, however, there is a lack of research tools exclusively dedicated to the assessment of DSH. Therefore, the objective of this research is the development of a new instrument entitled Inventory of Deliberate Self-Harm Behaviours (Inventário de Comportamentos Auto-Lesivos, ICAL).
In order to develop the ICAL, we used the first section of the Inventory of Statements About Self-Injury (ISAS, 44) as a basis, since it clearly and succinctly presents 12 methods of DSH, making it appropriate for clinical and investigation settings. Furthermore, this inventory is aimed at adolescents and young adults, has been adapted and validated for the Swedish and Turkish populations [44, 45], and has been used in numerous research that involved diverse samples (e.g. [17, 30, 32, 34, 46,47,48,49,50,51,52]). However, since the ISAS was designed to assess the lifetime frequency of NSSI methods (DSH without suicidal intent), further DSH methods with suicidal intent were added to the inventory. Also, the original response format of the ISAS was modified and a categorization of the answers was added. These procedures are further detailed in the Measures section.
Finally, although research has identified several degrees of severity of DSH, we found no studies that included a factorial analysis of DSH methods. Hence, the current research comprises a first study that consists of an exploratory factorial analysis of the ICAL (Study 1), and a second study, where the factorial structure of the inventory is evaluated with a new independent sample (Study 2). Both studies also tested the internal consistency of the ICAL.
Study 1: Exploratory Factor Analysis
Method
Participants
The participants of the first study consisted of 131 adolescents with a history of DSH, studying in several schools located in the district of Lisbon. These 131 participants were part of an initial sample of 620 adolescents with and without a history of DSH, corresponding to 21.1% of this total. Thus, 42 (32.1%) participants were male and 89 (67.9%) were female. Their ages ranged from 12 to 19 years, with a mean of 16.1 years (SD = 1.8). Table 1 details the socio-demographic data of the participants.
Measures
Our measures consisted of a brief socio-demographic questionnaire and the first version of the ICAL. The socio-demographic questionnaire included questions about the participants’ gender, age, nationality, academic retentions, number of siblings, and the marital status of their parents.
The translation process of the first section of the ISAS [53] was carried out by three experts in the subject with knowledge of the English language. Subsequently, each of these translations was retro-translated into English by three other experts with knowledge of the English language. The final versions were compared with the original instrument and the items considered more similar were selected by the researchers. Afterwards, in order to analyse if the language of the items was easily and accurately understood, facial validation of the instrument was performed with a group of 12 adolescents.
To test the resulting version of the previous procedure, we conducted a pre-test. Results from this pre-test were discussed with researchers in the field of DSH, and some modifications were made. Regarding the original scale, several items were reformulated for better understanding by the adolescents and three items were removed from the inventory (Pinching, Interfering with Wound Healing, and Rubbing Skin Against Rough Surfaces). In order to complement the original ISAS items that focus solely on NSSI, new items were also added to the inventory to incorporate DSH methods with suicidal intent. Therefore, the first version of the instrument comprises 14 items: cutting (original item from the ISAS), biting (original item from the ISAS), burning (original item from the ISAS), carving/engraving symbols or words on the skin (reformulated item from the ISAS), pulling hair (original item from the ISAS), scratching the skin to make a wound (reformulated item from the ISAS), consuming drugs to hurt oneself (new item), sticking self with needles (original item from the ISAS), swallowing dangerous substances to hurt oneself (reformulated item from the ISAS), drinking too much to hurt oneself (new item), banging or hitting self (original item from the ISAS), ingesting medication to hurt oneself (new item), ingesting medication with the intention of dying (new item), attempting suicide (new item).
In addition to these changes, an alternative to the original response format of the ISAS was created. The original response format asked the participant to estimate, in an open question, the number of times he/she had practiced each type of DSH method throughout his/her life. We introduced a four option response format depending on the lifetime prevalence and frequency of these behaviours: “No”; “Yes, one time”; “Yes, 2 to 10 times”; and “Yes, more than 10 times”. This categorization allows the clarification and standardization of results, as well as a quicker response on the part of the participant.
Procedures
Several schools were contacted and informed regarding the goals of the investigation. After receiving the schools’ administration approval, several classes were selected and the researcher delivered the consent forms to the students’ parents/legal guardians, prior to the application of the questionnaire. Data collection was carried out in a single phase, where the students whose parents/legal guardians signed the consent form were asked to complete the questionnaire. The participation of each student was voluntary and their consent was previously requested. Procedures were also followed to ensure the confidentiality of the data and the anonymity of the participants.
Data Analysis
As for data analysis, since we expect factors to be correlated assuming a latent construct (i.e. DSH behaviours), we carried out Exploratory Factor Analysis (EFA), using the Principal Axis Factoring method with oblique rotation (direct oblimin). We considered eigenvalues and scree plots to determine the number of factors, as well as a threshold of .30 for minimum loading coefficient for items in each factor. Finally, we tested the internal consistency of each factor through Cronbach’s alpha. All statistical analyses were carried out using SPSS software v22 (IBM SPSS, Chicago, IL).
Results
Prevalence of DSH
Participants practiced an average of 3.37 DSH methods (SD = 2.23, min. = 1, max. = 10). The most frequent methods were cutting (56.4%), biting (54.2%), and banging or hitting self (38.9%). The less-mentioned methods were ingesting medication to hurt oneself (7.6%), ingesting medication with the intention of dying (7.6%) and consuming drugs to hurt oneself (8.5%). Table 2 presents prevalence and frequency of DSH methods.
Exploratory Factor Analysis (EFA)
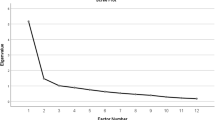
An EFA with the 14 items (KMO = .73, χ2 = 535.85, p < .001) presented a 4-factor model solution with eigenvalues higher than 1. However, after analysing the scree plot, we found that a 3-factor model would better fit these results (Fig. 1). The EFA forced to extract 3 factors which explained 51.64% of variance revealed that item 4 presented very low loadings, failing to load > .30 in any factor. From a theoretical perspective, and taking into account that this item refers to the carving of words or symbols on the skin (i.e. Carving/engraving symbols or words on the skin), we hypothesized that the content of this item could have been considered as a behaviour that does not cause damage to body tissue (such as writing words), or as a behaviour related to body modification practices such as scarification (that are not included in the spectrum of DSH). Therefore, based on these results, we decided to remove item 4 from the inventory.
A second EFA without item 4 was conducted (KMO = .73, χ2 = 528.05, p < .001), where the 3-factor solution explained 55.20% of the variance. Items 13, 12, 14, and 1 loaded >.30 exclusively on factor 1; items 2, 6, 5, 11, and 8 on factor 2; and items 10, 7 on factor 3. Items 3 and 9 presented factor loadings >.30 on both factor 1 (.375 and .361) and factor 2 (.361 and .302), though loadings were higher in the first factor (see Table 3). Therefore, factor 1 explained 27.48% of the variance and includes the following items: item 1 (cutting), item 3 (burning), item 9 (swallowing dangerous substances to hurt oneself), item 12 (ingesting medication to hurt oneself), item 13 (ingesting medication with the intention of dying), and item 14 (attempting suicide). Factor 2 explained 17.97% of the variance and included item 2 (biting), item 5 (pulling hair), item 6 (scratching the skin to make a wound), item 8 (sticking self with needles), and item 11 (banging or hitting self). Finally, factor 3 explained 9.76% of the variance and is composed of item 7 (consuming drugs to hurt oneself) and item 10 (drinking too much to hurt oneself).
An analysis of the internal consistency of the inventory revealed that factor 2 (Mild Severity DSH; α = .72) and factor 3 (Substance Use DSH; α = .74) showed acceptable Cronbach’s alphas, while factor 1 (High Severity DSH; α = .66) showed slightly lower internal consistency.
Study 2: Confirmatory Factor Analysis
Method
Participants
The sample for Study 2 was comprised of 109 adolescents with a history of DSH, from schools located in the district of Leiria, Portugal. These 109 participants integrated an initial sample of 411 adolescents with and without a history of DSH, corresponding to 26.5% of the initial sample. Therefore, 35 (32.1%) participants were male and 74 (67.9%) were female, aged from 12 to 19 years, with an average of 15.4 years (SD = 1.8). As described in Table 4, the socio-demographic data were similar to the sample used in Study 1.
Measures
The measures for this study consisted of a brief socio-demographic questionnaire and the final 13-item version of the ICAL, adapted in Study 1. The socio-demographic questionnaire comprised questions about the participants’ gender, age, nationality, number of academic retentions, number of siblings, and the marital status of their parents.
Procedures
In this study, we followed the same procedures described in Study 1.
Data Analysis
As for data analysis, in Study 2 we developed a Confirmatory Factor Analysis (CFA). Considering that these variables are ordinal and presented a non-normal distribution (kuMult = 176.60), CFA was carried out using the unweighted least squares method [54, 55]. The overall adjustment of the model was estimated through the analysis of factorial weights and several adjustment indicators, namely the Goodness-of-Fit Index (GFI), Adjusted Goodness-of-Fit Index (AGFI), Parsimony Goodness-of-Fit Index (PGFI), Normal Fit Index (NFI) and Root Mean Square Residual (RMR) [56,57,58,59,60]. Internal consistency was estimated through Cronbach’s alpha. All statistical analyses were carried out using SPSS v22 software and Amos Version 22.0 (IBM SPSS, Chicago, IL).
Results
Prevalence of DSH
Results obtained in this second data collection are similar to those found in Study 1 (Table 5). These participants reported an average of 3.30 DSH methods (SD = 2.15, min. = 1, max. = 12). The most mentioned methods were banging or hitting self (57.8%), biting (54.1%) and cutting (45.9%). On the other hand, the less frequent methods were swallowing dangerous substances to hurt oneself (5.5%), ingesting medication with the intention of dying (5.5%), and attempting suicide (7.3%).
Confirmatory Factor Analysis (CFA)
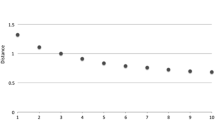
As illustrated in Fig. 2, the CFA for the factorial model developed in Study 1 showed that, with the exception of item 7 (λ = .44), all items presented high factorial weights (> .50). Also, the indices revealed a good model fit (GFI = .954, PGFI = .650, NFI = .857, and RMR = .050). NFI score was slightly lower than usually recommended for a good fit (> .90) but still acceptable [59, 61].
Considering the correlations between the three latent variables (Fig. 2), results showed that Substance Use DSH factor presented a small positive correlation with Mild Severity DSH and a medium positive correlation with High Severity DSH. On the other hand, High Severity DSH and Mild Severity DSH showed a small negative correlation.
Reliability analysis for Study 2 revealed acceptable to good internal consistency for the High Severity DSH factor (α = .76) and Substance Use DSH factor (α = .82). Mild Severity DSH showed slightly lower Cronbach’s alpha (α = .67).
General Discussion
The purpose of the present investigation was to develop and validate the ICAL, an instrument dedicated to the assessment of DSH in Portuguese adolescents. We utilized the first section of the ISAS [53] as a basis for this instrument and complemented the inventory with other DSH methods according to the results of a pre-test, to discussion with experts, and to our conceptual frame. To analyse the factorial structure of the ICAL we conducted two studies: Study 1 consisted of an EFA that also contributed to item reduction, and Study 2 tested the stability of the factorial structure of the inventory through a CFA.
Both studies used independent community samples of adolescents with a history of DSH, which also allowed us to contribute to the understanding of the prevalence of DSH in Portuguese adolescents and to characterize its various methods. In both studies, which involved adolescents aged 12 to 19 years, results revealed that 21.1% (131 participants in Study 1) and 26.5% (109 participants in Study 2) of participants from the initial samples reported having practiced at least one DSH behaviour during their lifetime. These prevalence rates are in line with those previously found in national [6, 9] and international research [2, 11] with identical samples. Focusing on the participants who reported a history of DSH, results showed that the most common methods consisted of cutting (56.4% in Study 1 and 45.9% in Study 2), biting (54.2% in Study 1 and 54.1% in Study 2), and banging or hitting self (38.9% in Study 1 and 57.8% in Study 2). These findings are similar to the results of several investigations that also studied community samples [2, 3, 5, 9, 18].
One of the main goals of this investigation was to analyse the ICAL factorial structure through an EFA and a CFA. The results obtained in the first study presented a three-dimensional structure. This 3-factor arrangement of items seemed to be in agreement with the literature that has proposed a categorization according to the severity of DSH behaviours (e.g. [20,21,22]). Factor 1 is comprised of severe DSH methods (including both items referring to suicide attempts), thus we designated it as High severity DSH. Similarly, items in factor 2 showed mild and moderate forms of DSH. Thus, we assigned the designation of Mild severity DSH to this dimension. Finally, both items in factor 3 refer to the use of psychoactive substances with self-aggressive intent, thus we designated it as Substance use DSH. In Study 2, the CFA tested this factorial structure, revealing an overall good model with a stable three-factor structure. As for the analysis of internal consistency, despite the majority of factors showed acceptable levels of reliability in both studies, the High Severity Self-Harm factor in Study 1 (α = .66) and the Mild Severity Self-Harm in Study 2 (α = .67) showed slightly lower Cronbach’s alpha scores. However, some researchers have pointed out that a threshold as low as .60 can be acceptable in early stages of psychological research (e.g. [62, 63]). Therefore, in general, we can conclude that these studies revealed acceptable values of Cronbach’s alpha for the three factors.
The three factors are consistent with the existing literature since they group items referring to similar typologies of DSH methods according to its severity [20,21,22]. If we consider DSH to be part of a suicidal continuum that is organized according to the severity of the behaviours [21, 24, 25], it is possible to position Factor 2 (Mild Severity DSH) at the beginning/middle section of this continuum, while Factor 1 (High Severity DSH) can be located at a more extreme point. In addition, the CFA revealed that these factors had a minor negative correlation, which may imply that these two types of DSH methods are independent. Considering that we asked the participants to report their lifetime experience of DSH, we question if the adolescents who reported less severe DSH methods might still be far from engaging in more severe DSH since they are still “positioned” at the beginning of the suicidal continuum.
Factor 3 (Substance Use DSH) encompasses behaviours that can be considered as socially accepted and typical of adolescence (e.g. [64,65,66]). However, in the context of DSH, the consumption of alcohol and other psychoactive substances is characterized by a self-aggressive intent that distinguishes these behaviours from the consumptions considered “normal” during adolescence. Nonetheless, it is difficult to argue where this factor can be positioned on the suicidal continuum in terms of severity. It is known that substance use is associated with DSH (e.g. [10, 67, 68]). Some authors argue that DSH should be viewed within an addictions framework and that, since it has an addictive component, it is understandable that DSH often co-exists with other addictions (e.g. [69, 70]). On the other hand, both DSH and substance use cause physiological damage to the body, so the psychological processes underlying both may be similar [71]. Therefore, since our results revealed positive correlations between this factor and factors 1 and 2, we question if the consumption of psychoactive substances with self-aggressive intent accompanies other DSH methods, if adolescents who engage in DSH consume psychoactive substances during the DSH episodes, or if substance use can act as a “gateway” to other DSH behaviours.
Our findings may have relevant implications for clinical settings, as well as for future research. Firstly, the factorial organization of DSH methods may contribute to create awareness regarding the suicidal continuum in which less severe behaviours may lead to more severe behaviours and, eventually, suicide. The application of the ICAL in clinical settings may, for example, be relevant for the signalling of adolescents at risk of engaging in more severe DSH methods such as suicide attempts, or of adolescents with potential psychopathologies associated with more severe methods [22]. Factor 2, specifically, may also contribute to a new approach concerning the adolescents who present consumptions of psychoactive substances. It might be important to explore if these adolescents’ behaviours have an underlying self-aggressive intent and if they can be situated in the suicidal continuum. In addition, understanding this categorization of DSH methods may be relevant in terms of broad clinical assessment and psychotherapeutic interventions, since different treatment approaches may be required for each DSH typology [22].
In terms of research, the ICAL may be an important tool for the study of DSH in adolescents, mainly because it is a simple tool that assesses multiple DSH methods, categorizes their frequency, and presents three groups/factors of methods. However, although the ICAL has revealed acceptable psychometric properties, some limitations should be noted, including the use of community samples with similar socio-demographic characteristics and the use of self-report measures regarding DSH. Also, the ICAL was not tested regarding its divergent and convergent validity with other variables. These limitations could be overcome with further research that might simultaneously allow more rigorous testing of constructs and of the factorial structure of the inventory.
Overall, we believe that the ICAL can be useful both in research and clinical settings, contributing to subsequent investigations focused on adolescents and for the understanding of the complex phenomenon of DSH.
References
Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379:2373–82. https://doi.org/10.1016/S0140-6736(12)60322-5.
Brunner R, Kaess M, Parzer P, Fischer G, Carli V, Hoven CW, et al. Life-time prevalence and psychosocial correlates of adolescent direct self-injurious behavior: a comparative study of findings in 11 European countries. J Child Psychol Psychiatry. 2014;55(4):337–48. https://doi.org/10.1111/jcpp.12166.
Madge N, Hewitt A, Hawton K, Wilde E, Corcoran P, Fekete S, et al. Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) study. J Child Psychol Psychiatry. 2008;49(6):667–77. https://doi.org/10.1111/j.1469-7610.2008.01879.x.
Moran P, Coffey C, Romaniuk H, Olsson C, Borschmann R, Carlin JB, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet. 2012;379(9812):236–43. https://doi.org/10.1016/S0140-6736(11)61141-0.
Nixon MK, Cloutier P, Jansson M. Nonsuicidal self-harm in youth: a population-based survey. Can Med Assoc J. 2008;178(3):306–12. https://doi.org/10.1503/cmaj.061693.
Carvalho CB, Motta C, Sousa M, Cabral J. Biting myself so I don’t bite the dust: prevalence and predictors of deliberate self-harm and suicide ideation in Azorean youths. Rev Bras Psiquiatr. 2017;39(3):252–62. https://doi.org/10.1590/1516-4446-2016-1923.
Duarte E, Gouveia-Pereira M, Gomes HS, Sampaio D. How do families represent the functions of deliberate self-harm? A comparison between the social representations from adolescents and their parents. Arch Suicide Res. 2019a:1–17. https://doi.org/10.1080/13811118.2018.1545713.
Duarte E, Gouveia-Pereira M, Gomes HS, Sampaio D. Social representations about the functions of deliberate self-harm: construction and validation of a questionnaire for Portuguese adolescents. J Pers Assess. 2019b:1–10. https://doi.org/10.1080/00223891.2018.1557667.
Gonçalves SF, Martins C, Rosendo AP, Machado BC, Silva E. Self-injurious behavior in Portuguese adolescents. Psicothema. 2012;24(4):536–41.
Guerreiro DF, Sampaio D, Figueira ML, Madge N. Self-harm in adolescents: a self-report survey in schools from Lisbon, Portugal. Arch Suicide Res. 2017;21(1):83–99. https://doi.org/10.1080/13811118.2015.1004480.
Muehlenkamp JJ, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;6(10). https://doi.org/10.1186/1753-2000-6-10.
Carvalho Á, Peixoto B, Saraiva CB, Sampaio D, Amaro F, Santos JC, et al. Plano Nacional de Prevencão do Suicídio 2013/2017. Lisboa: Direccão Geral da Saúde; 2013.
Madge N, Hawton K, McMahon EM, Corcoran P, De Leo D, De Wilde EJ, et al. Psychological characteristics, stressful life events and deliberate self-harm: findings from the child & adolescent self-harm in Europe (CASE) study. Eur Child Adolesc Psychiatry. 2011;20(10):499–508. https://doi.org/10.1007/s00787-011-0210-4.
Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. 2008;37(2):363–75. https://doi.org/10.1080/15374410801955771.
Zhand N, Matheson K, Courtney D. Self-harm in child and adolescent psychiatric inpatients: a retrospective study. J Can Acad Child Adolesc Psychiatry. 2016;25(3):169–76.
Swannell S, Martin G, Scott J, Gibbons M, Gifford S. Motivations for self-injury in an adolescent inpatient population: development of a self-report measure. Australas Psychiatry. 2008;16(2):98–103. https://doi.org/10.1080/10398560701636955.
Heath NL, Joly M, Carsley D. Coping self-efficacy and mindfulness in non-suicidal self-injury. Mindfulness. 2016;7(5):1132–41. https://doi.org/10.1007/s12671-016-0555-3.
Calvete E, Orue I, Aizpuru L, Brotherton H. Prevalence and functions of non-suicidal self-injury in Spanish adolescents. Psicothema. 2015;27(3):223–8. https://doi.org/10.7334/psicothema2014.262.
Duarte E, Gouveia-Pereira M, Gomes HS, Sampaio D. Social representations about the functions of deliberate self-harm: adolescents and parents. J Adolesc. 2019b;73:113–21. https://doi.org/10.1016/j.adolescence.2019.05.001.
Croyle KL, Waltz J. Subclinical self-harm: range of behaviors, extent, and associated characteristics. Am J Orthopsychiatry. 2007;77(2):332–42. https://doi.org/10.1037/0002-9432.77.2.332.
Skegg K. Self-harm. Lancet. 2005;366(9495):1471–83. https://doi.org/10.1016/S0140-6736(05)67600-3.
Whitlock J, Muehlenkamp J, Eckenrode J. Variation in nonsuicidal self-injury: identification and features of latent classes in a college population of emerging adults. J Clin Child Adolesc Psychol. 2008;37(4):725–35. https://doi.org/10.1080/15374410802359734.
Joiner TE. Why people die by suicide. Cambridge: Harvard University Press; 2006.
Stanley B, Winchel R, Molcho A, Simeon D, Stanley M. Suicide and the self-harm continuum: phenomenological and biological evidence. Int Rev Psychiatry. 1992;4(2):149–55. https://doi.org/10.3109/09540269209066312.
Sun FK. A concept analysis of suicidal behavior. Public Health Nurs. 2011;28(5):458–68. https://doi.org/10.1111/j.1525-1446.2011.00939.x.
Jacobson CM, Gould M. The epidemiology and phenomenology of non-suicidal self-injurious behavior among adolescents: a critical review of the literature. Arch Suicide Res. 2007;11(2):129–47. https://doi.org/10.1080/13811110701247602.
Victor SE, Styer D, Washburn JJ. Characteristics of nonsuicidal self-injury associated with suicidal ideation: evidence from a clinical sample of youth. Child Adolesc Psychiatry Ment Health. 2015;9:1–20. https://doi.org/10.1186/s13034-015-0053-8.
Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144(1):65–72. https://doi.org/10.1016/j.psychres.2006.05.010.
Stewart JG, Esposito EC, Glenn CR, Gilman SE, Pridgen B, Gold J, et al. Adolescent self-injurers: comparing non-ideators, suicide ideators, and suicide attempters. J Psychiatr Res. 2017;84:105–12. https://doi.org/10.1016/j.jpsychires.2016.09.031.
Klonsky ED, Olino T. Identifying clinically distinct subgroups of self-injurers among young adults: a latent class analysis. J Consult Clin Psychol. 2008;76(1):22–7. https://doi.org/10.1037/0022-006X.76.1.22.
Bjärehed J, Wångby-Lundh M, Lundh L. Nonsuicidal self-injury in a community sample of adolescents: subgroups, stability, and associations with psychological difficulties. J Res Adolesc. 2012;22:678–93. https://doi.org/10.1111/j.1532-7795.2012.00817.x.
Hamza CA, Willoughby T. Nonsuicidal self-injury and suicidal behavior: a latent class analysis among young adults. PLoS One. 2013;8(3). https://doi.org/10.1371/journal.pone.0059955.
Hargus E, Hawton K, Rodham K. Distinguishing between subgroups of adolescents who self-harm. Suicide Life Threat Behav. 2009;39:518–37. https://doi.org/10.1521/suli.2009.39.5.518.
Somer O, Bildik T, Kabukçu-Başay B, Güngör D, Başay Ö, Farmer RF. Prevalence of non-suicidal self-injury and distinct groups of self-injurers in a community sample of adolescents. Soc Psychiatry Psychiatr Epidemiol. 2015;50(7):1163–71. https://doi.org/10.1007/s00127-015-1060-z.
Stanford S, Jones MP. Psychological subtyping finds pathological, impulsive, and ‘normal’ groups among adolescents who self-harm. J Child Psychol Psychiatry. 2009;50:807–15. https://doi.org/10.1111/j.1469-7610.2009.02067.x.
Walsh BW. Treating self-injury: a practical guide. New York: Guilford; 2006.
You J, Leung F, Fu K, Lai CM. The prevalence of nonsuicidal self-injury and different subgroups of self-injurers in Chinese adolescents. Arch Suicide Res. 2011;15(1):75–86. https://doi.org/10.1080/13811118.2011.540211.
Craigen LM, Healey AC, Walley CT, Byrd R, Schuster J. Assessment and self-injury: implications for counselors. Meas Eval Couns Dev. 2010;43(1):3–15. https://doi.org/10.1177/0748175610362237.
Nock MK, Holmberg EB, Photos VI, Michel BD. Self-injurious thoughts and behaviors interview: development, reliability and validity in an adolescent sample. Psychol Assess. 2007;19(3):309–17. https://doi.org/10.1037/1040-3590.19.3.309.
Vrouva I, Fonagy P, Fearon PRM, Roussow T. The risk-taking and self-harm inventory for adolescents: development and psychometric evaluation. Psychol Assess. 2010;22(4):852–65. https://doi.org/10.1037/a0020583.
Gratz K. Measurement of deliberate self-harm: preliminary data on the deliberate self-harm inventory. J Psychopathol Behav Assess. 2001;23(4):253–63.
Santa Mina EE, Gallop R, Links P. The self-injury questionnaire: evaluation of the psychometric properties in a clinical population. J Psychiatr Ment Health Nurs. 2006;13(2):221–7. https://doi.org/10.1111/j.1365-2850.2006.00944.x.
Whitlock J, Exner-Cortens D, Purington A. Assessment of nonsuicidal self-injury: development and initial validation of the non-suicidal self-injury–assessment tool (NSSI-AT). Psychol Assess. 2014;26(3):935–46. https://doi.org/10.1037/a0036611.
Bildik T, Somer O, Kabukçu-Başay B, Başay Ö, Özbaran B. The validity and reliability of the Turkish version of the inventory of statements about self-injury. Turk J Psychiatry. 2013;24(1):41–9.
Lindholm T, Bjärehed J, Lundh L-G. Functions of nonsuicidal self-injury among young women in residential care: a pilot study with the Swedish version of the inventory of statements about self-injury. Cogn Behav Ther. 2011;40(3):183–9. https://doi.org/10.1080/16506073.2011.565791.
Dickey L, Reisner SL, Lee Juntunen C. Non-suicidal self-injury in a large online sample of transgender adults. Prof Psychol Res Pract. 2015;46(1):3–11. https://doi.org/10.1037/a0038803.
Glenn CR, Klonsky ED. One-year test-retest reliability of the inventory of statements about self-injury (ISAS). Assessment. 2011;18(3):375–8. https://doi.org/10.1177/1073191111411669.
Hamza CA, Willoughby T. A longitudinal person-centered examination of nonsuicidal self-injury among university students. J Youth Adolesc. 2014;43(4):671–85. https://doi.org/10.1007/s10964-013-9991-8.
Klonsky ED, Glenn CR, Styer DM, Olino TM, Washburn JJ. The functions of nonsuicidal self-injury: converging evidence for a two-factor structure. Child Adolesc Psychiatry Ment Health. 2015;9(44):1–9. https://doi.org/10.1186/s13034-015-0073-4.
Kortge R, Meade T, Tennant A. Interpersonal and intrapersonal functions of deliberate self-harm (DSH): a psychometric examination of the inventory of statements about self-injury (ISAS) scale. Behav Chang. 2013;30(1):24–35. https://doi.org/10.1017/bec.2013.3.
Saraff PD, Trujillo N, Pepper CM. Functions, consequences, and frequency of non-suicidal self-injury. Psychiatry Q. 2015;86(3):385–93. https://doi.org/10.1007/s11126-015-9338-6.
Victor SE, Glenn CR, Klonsky ED. Is non-suicidal self-injury an "addiction"? A comparison of craving in substance use and non-suicidal self-injury. Psychiatry Res. 2012;197(1–2):73–7. https://doi.org/10.1016/j.psychres.2011.12.011.
Klonsky ED, Glenn CR. Assessing the functions of non-suicidal self-injury: psychometric properties of the inventory of statements about self-injury (ISAS). J Psychopathol Behav Assess. 2009;31(3):215–9. https://doi.org/10.1007/s10862-008-9107-z.
Kogar H, Kogar EY. Comparison of different estimation methods for categorical and ordinal data in confirmatory factor analysis. .Journal of Measurement and Evaluation in Education and Psychology. 2015;6(2):351–64. https://doi.org/10.21031/epod.94857.
Yang-Wallentin F, Jöreskog KG, Luo H. Confirmatory factor analysis of ordinal variables with misspecified models. Struct Equ Model Multidiscip J. 2010;17(3):392–423. https://doi.org/10.1080/10705511.2010.489003.
Arbuckle, J. L. (2013). IBM® SPSS® Amos™ 22 User’s guide. Amos Development Corporation. Retrieved May 10, 2019, from http://www.sussex.ac.uk/its/pdfs/SPSS_Amos_User_Guide_22.pdf.
Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588–606. https://doi.org/10.1037/0033-2909.88.3.588.
Hooper D, Coughlan J, Mullen MR. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6(1):53–60. https://doi.org/10.21427/D7CF7R.
Marôco J. Análise de Equações Estruturais: Fundamentos Teóricos, Software e Aplicações. Pêro Pinheiro: Report Number; 2010.
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online. 2003;8(2):23–74.
Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–46. https://doi.org/10.1037/0033-2909.107.2.238.
Nunnally J. Psychometric theory. New York: McGraw-Hill; 1967.
Aron A, Aron E. Statistics for psychology. 2nd ed. Upper Saddle River: Prentice Hall; 1999.
Degenhardt L, Chiu W-T, Sampson N, Kessler RC, Anthony JC, Angermeyer M, et al. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO world mental health surveys. PLoS Med. 2008;5(7):1053–67. https://doi.org/10.1371/journal.pmed.0050141.
Matos MG, Simões C, Tomé G, Camacho I, Ferreira M, Ramiro L, et al. A Saúde dos Adolescentes Portugueses: Relatório do Estudo HBSC 2010. Lisboa: Centro de Malária e outras Doenças Tropicais/IHMT/UNL; 2012.
Zappe JG, Dell'Agli DD. Variáveis pessoais e contextuais associadas a comportamentos de risco em adolescentes. J Bras Psiquiatr. 2016;65(1):44–52. https://doi.org/10.1590/0047-2085000000102.
Haw C, Hawton K, Casey D, Bale E, Shepherd A. Alcohol dependence, excessive drinking and deliberate self-harm – trends and patterns in Oxford, 1989-2002. Soc Psychiatry Psychiatr Epidemiol. 2005;40:964–71. https://doi.org/10.1007/s00127-005-0981-3.
Hawton K, Hall S, Simkin S, Bale L, Bond A, Codd S, et al. Deliberate self-harm in adolescents: a study of characteristics and trends in Oxford, 1990-2000. J Child Psychol Psychiatry. 2003;44(8):1191–8. https://doi.org/10.1111/1469-7610.00200.
Hasking P, Momeni R, Swannell S, Chia S. The nature and extent of non-suicidal self-injury in a non-clinical sample of young adults. Arch Suicide Res. 2008;12:208–18. https://doi.org/10.1080/13811110802100957.
Mangnall J, Yurkovich E. A literature review of deliberate self-harm. Perspect Psychiatr Care. 2008;44(3):175–84. https://doi.org/10.1111/j.1744-6163.2008.00172.x.
Klonsky ED, Muehlenkamp JJ. Self-injury: a research review for the practitioner. J Clin Psychol In Session. 2007;63(11):1045–56. https://doi.org/10.1002/jclp.20412.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This research was approved by the General Education Directorate of the Ministry of Education and Science from Portugal. All procedures performed in both studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Eva Duarte, Maria Gouveia-Pereira, and Hugo S. Gomes declare that they have no conflict of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duarte, E., Gouveia-Pereira, M. & Gomes, H.S. Development and Factorial Validation of the Inventory of Deliberate Self-Harm Behaviours for Portuguese Adolescents. Psychiatr Q 90, 761–776 (2019). https://doi.org/10.1007/s11126-019-09660-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-019-09660-1